Effect of environment of skin
1/12
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
13 Terms
The Skin: Vital Organ
The skin is the interface between the body and the external environment, constantly exposed to physical, chemical, and biological stresses
It is a vital organ essential for survival
Consequences of extensive skin damage (epidermal ± dermal)
Can occur in severe burns or rare drug reactions
May be fatal due to:
Dehydration and shock
Infection
Heat loss and hypothermia (or hyperthermia from impaired thermoregulation)
Protein loss, electrolyte imbalance
High-output cardiac failure
Renal failure
Toxic epidermal necrolysis (TEN)
Rare, severe adverse drug reaction
Characterised by detachment of the epidermis
Often preceded by flu-like symptoms
Rapid development of painful erythematous rash and desquamation of skin and mucous membranes
High mortality, highlighting the critical protective role of skin
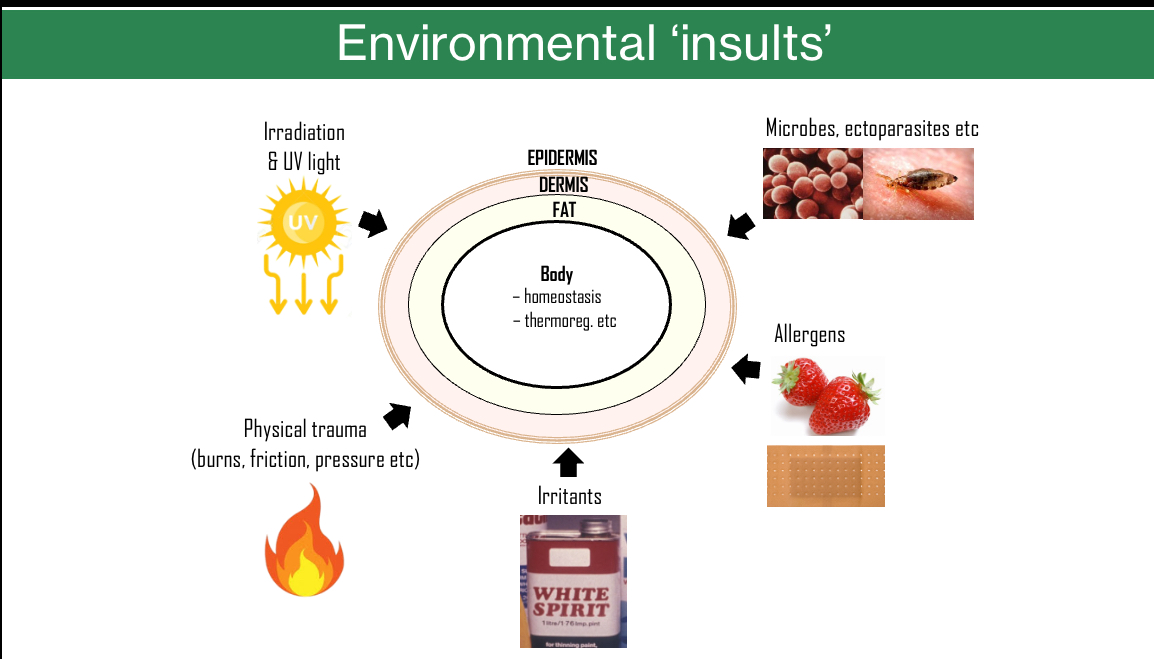
Environmental Insults
The skin protects the body from multiple external challenges while maintaining homeostasis and thermoregulation
Major environmental insults include:
UV radiation and irradiation
Microbes and ectoparasites
Physical trauma (burns, friction, pressure)
Chemical irritants
Allergens
Damage or breach of the skin barrier compromises protection and disrupts normal body function
Protective features of Skin
Prevents drying: waterproof epidermis plus sebum from sebaceous glands
Resists friction and impact:
Thick, regenerating, keratinised epidermis
Nails
Basement membrane anchoring epidermis to dermis with a wavy interface to resist shear
Strong collagen fibres in the dermis arranged in multiple directions
Heat regulation: sweating and vasodilation
Cold protection: subcutaneous fat, adjustable blood supply, and hair (especially on the head)
Protection from burns and injury: thick, regenerating epidermis
Protection from radiation/sunlight: thick epidermis and melanin
Defense against infection: impervious epidermal barrier and resident immune cells
Normal Skin Adaptations to the Environment
Temperature regulation
Sweating and vasodilation in heat
Vasoconstriction in cold
Rapid response (minutes)
Hyperkeratosis (callus formation)
Thickening of the stratum corneum in response to repeated rubbing or pressure (e.g. feet, fingers)
Can also occur mildly after UV exposure
Slow response (weeks)
Tanning
Increased melanin production by melanocytes after UV exposure
Protective response to radiation
Slow response (days)
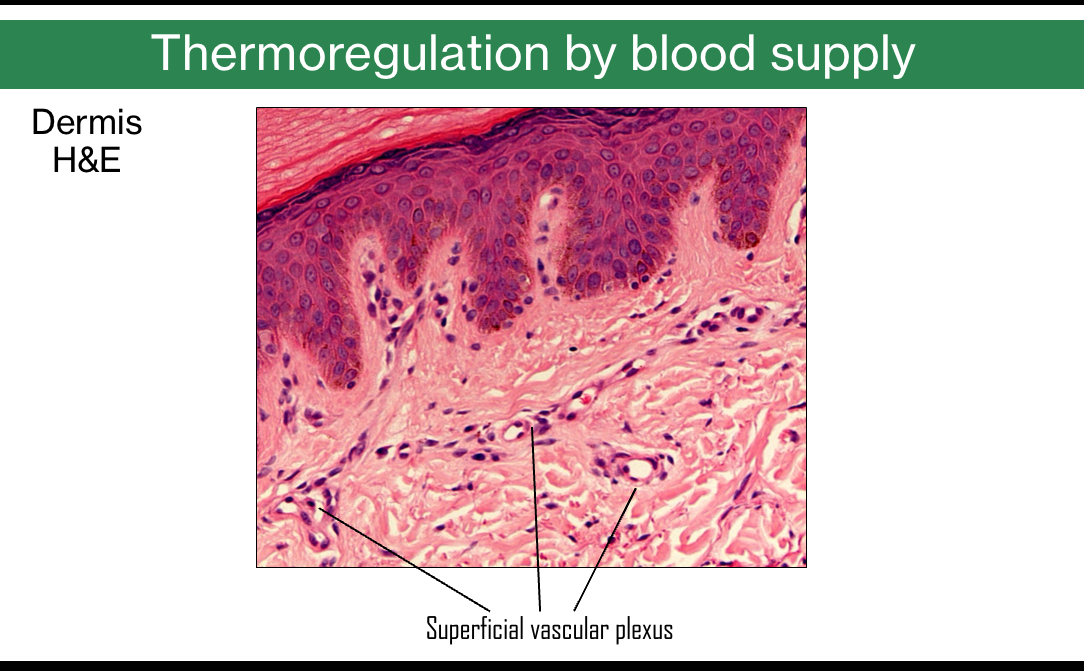
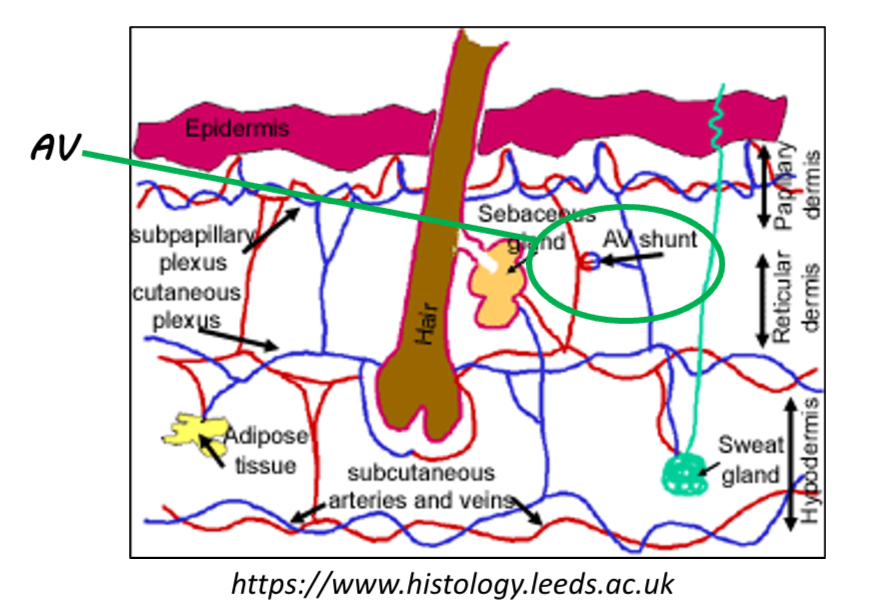
Thermoregulation by blood supply
Skin temperature is regulated by arteriovenous (AV) shunts in the dermis
AV shunts connect arterioles and venules and are abundant in the dermis
They respond to skin thermoreceptors detecting heat or cold
Shunts open → increased blood flow to the superficial vascular plexus in the papillary dermis
More heat loss
Skin appears redder
Shunts close → reduced superficial blood flow
Heat conserved
Skin appears pale or blue
Facial blood flow can also change due to emotional or sympathetic nervous system activity (blushing)
Prolonged shunt closure can cause tissue damage, e.g. frostbit
UV protection: Epidermal melanin
Skin colour
Determined mainly by melanin (darker skin) and haemoglobin (lighter skin)
Large normal genetic variation in melanin production (many genes involved)
Role of melanin
Absorbs UV radiation and protects DNA from damage
Reduces risk of skin cancer
Darker skin has significantly lower skin cancer incidence than lighter skin
Melanocytes
Located in the epidermis
Produce melanin in melanosomes
Transfer melanosomes mainly to basal keratinocytes
Keratinocytes position melanin over the nucleus to shield DNA
Tanning
UV exposure increases melanocyte activity
More melanin synthesis and transfer to keratinocytes
Provides partial protection against further UV damage
Accompanied by epidermal thickening, adding extra protection
Mechanism of suntanning
UV causes DNA damage signalling in basal keratinocytes
Keratinocytes release MSH (melanocyte-stimulating hormone)
MSH binds MC1R on melanocytes
Activates cAMP signalling → increased transcription
Results in increased melanin synthesis, transfer, and melanocyte activity
Melanin synthesis pathway
Tyrosine → L-DOPA → DOPAquinone (via tyrosinase)
Produces:
Eumelanin (brown–black)
Pheomelanin (yellow–red)
Protection against microorganisms
Langerhans cells are key immune cells in the epidermis
Located mainly in the non-basal layers of the skin
Are dendritic cells
Function as antigen-presenting cells, similar to macrophages
Form an immune surveillance network within the epidermis
Act as part of the skin’s immune defence against microorganisms
Abnormal effects of the environment: Damage by ‘insults’
Environmental insults include friction/scratching, ultraviolet radiation, burns, irritants, allergens, and microbes
Chronic or excessive exposure leads to structural damage, inflammation, abnormal growth, and malignancy
Friction and scratching
Can cause lichenification: a severe form of hyperkeratosis
Skin becomes thickened, rough, and accentuated in skin markings due to repeated rubbing or scratching
Ultraviolet (UV) radiation effects
UVA (longer wavelength): penetrates deeper, contributes to photoaging and wrinkles
UVB: causes direct DNA damage, sunburn, and increases cancer risk
UVC is filtered out by the ozone layer
Sunburn
A radiation burn caused by UV exposure
Leads to inflammation, blistering, and keratinocyte cell death due to DNA damage
History of sunburn significantly increases skin cancer risk
Use of UV sunbeds before age 35 markedly increases melanoma risk
Polymorphic light eruption
Immune-mediated “sun allergy” triggered by UV exposure
Causes itchy red papules or plaques on sun-exposed skin
Photoaging (solar elastosis)
Chronic UV exposure damages elastic fibres in the dermis
Results in wrinkles, loss of skin elasticity, and leathery appearance
Pigmentary changes related to UV
Freckles (ephelides):
Genetically influenced, linked to MC1R variants and fair/red hair
Increased melanin production without increased melanocyte number
Appear on sun-exposed skin
Naevi (moles):
Benign proliferation of melanocytes
Numerous or large naevi increase melanoma risk
Solar lentigos (liver/age spots)
Benign, flat brown lesions caused by chronic UV exposure
Age-related and found on sun-exposed areas
Due to increased melanin, not increased melanocyte number
Solar keratoses (actinic keratoses)
UV-induced dysplastic growth of keratinocytes
Rough, scaly premalignant lesions on sun-exposed skin
Can progress to squamous cell carcinoma
Skin cancer (UV-related)
Results from cumulative UV-induced DNA damage
Two major categories:
Melanoma: arises from melanocytes, least common but most dangerous
Non-melanoma skin cancers (keratinocyte-derived, more common):
Squamous cell carcinoma
Basal cell carcinoma (most common, least aggressive)
UV – beneficial effects
UV exposure is required for vitamin D₃ synthesis in the skin
~15 minutes of summer sunlight on face and arms is usually sufficient for light skin
Longer exposure is needed for darker skin
Vitamin D can also be obtained via supplements
Therapeutic UV (phototherapy) is used clinically to treat certain skin conditions
Examples: vitiligo and psoriasis
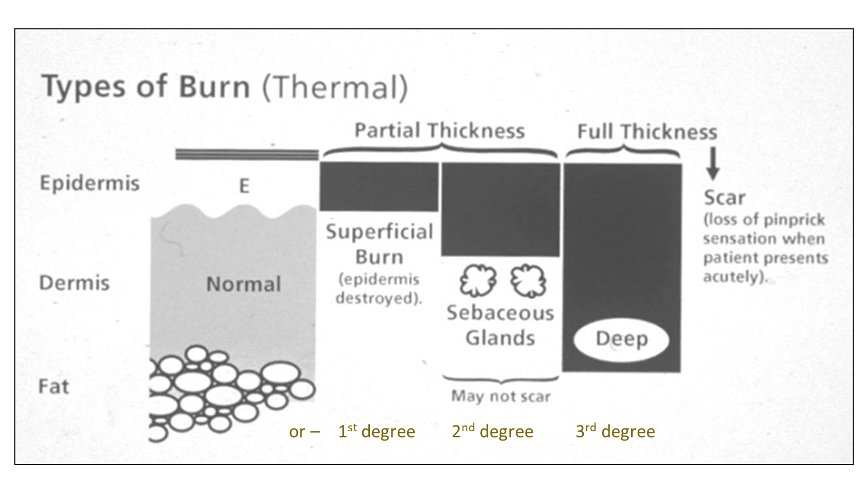
Burns
Superficial burn (1st degree)
Damage limited to the epidermis
Epidermis destroyed only
Heals without scarring
Partial thickness burn (2nd degree)
Damage to epidermis + part of dermis
Sebaceous glands may remain intact
May blister
May heal without scarring if dermal structures survive
Full thickness burn (3rd degree)
Destruction of epidermis, dermis, and deeper tissues
Loss of skin appendages and nerve endings
Results in scarring
Often associated with loss of pinprick sensation initially
Irritants: Irritant Contact Dermatitis
Caused by excessive exposure to an irritating substance (dose-dependent, not immune-mediated)
Sensitivity varies between individuals
Condition often improves by reducing exposure rather than complete avoidance
Typical features include redness, itching, swelling, blistering, and/or scaling
Allergens: Allergen Contact Dermatitis
Immune-mediated allergy to a substance contacting the skin
Very small amounts of allergen can trigger a reaction
Sensitivity varies widely; can develop after short or prolonged exposure
Symptoms include redness, itching, swelling, blistering, and/or weeping
Management: strict avoidance of the allergen
Key comparison & mechanism (allergens vs irritants)
Irritant contact dermatitis:
Common
Dose-dependent, non-immune
Allergic contact dermatitis:
Relatively uncommon (e.g. nickel)
Requires sensitisation first: Langerhans cells present antigen to lymphocytes
Delayed (type IV) hypersensitivity on re-exposure via memory T cells
Microbes(Fungi, Bacteria, Viruses)
Paronychia
Infection of the nail fold
Can be bacterial or fungal
Often associated with damaged skin around the nail
Fungal – Tinea capitis
Scalp ringworm
Patchy hair loss with scaling
Caused by dermatophyte fungi
Bacterial – Impetigo
Superficial bacterial skin infection
Crusting lesions, commonly in children
Often caused by Staphylococcus aureus or Streptococcus
Bacterial – Cellulitis
Deeper skin infection (dermis/subcutis)
Red, hot, swollen, painful skin
Commonly caused by Streptococcus
Enters via breaks in the epidermis
Viral – Human papillomavirus (HPV)
Causes warts
Hyperkeratotic, rough surface lesions
Key infection principles
Portal of entry
Microbes enter through breaches in the epidermis
Impaired immunity increases risk
Examples: HIV, widespread viral warts
Eczema herpeticum: herpes simplex virus infecting eczematous skin