Renal 4 - Renal Processes/Tubular Secretion + Reabsorption
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
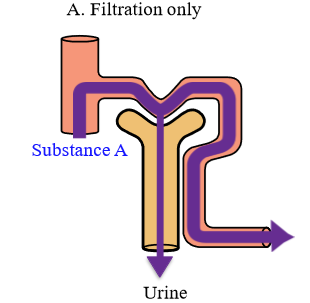
How does the kidney handle Inulin or creatinine?
The substance is filtered in bowman's space, and there is no extra secretion or reabsorption. Whatever is filtered is excreted
What is inulin
Polysaccharide found in some vegetables and plants
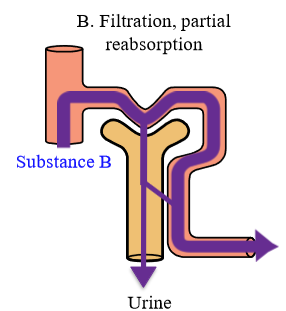
How does the kidney handle electrolytes?
Substance is filtered at the glomerulus, and is then partially reabsorbed into the peritubular capillaries. Some gets excreted
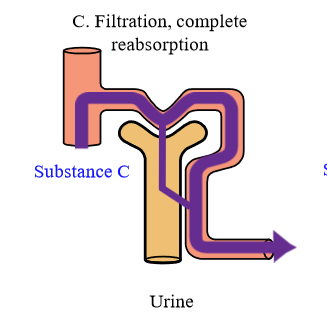
How does the Kidney handle glucose + amino acids
Substance is fileted at the glomerulus, and is then completely reabsorbed back into the peritubular capillaries. Under normal circumstances, no glucose or protein is excreted
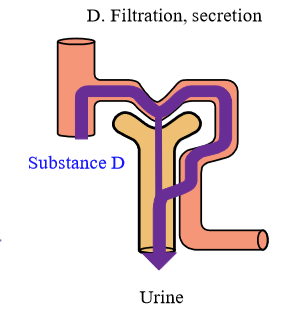
How does the kidney handle organic acids (like para-aminohippuric acid) and bases?
Substance is filtered at the glomerulus, and is then completely secreted from the peritubular capillaries into the tubules. Whole amount of substance is excreted
How much water is filtered, excreted, and % reabsorbed per day?
180 L is filtered per day, with only 1.8L being excreted. 99% of water is reabsorbed
How much sodium is fitered, excreted, and % reabsorbed per day?
630 g is filtered per day, with only 3.2 g being excreted. 99.5% of sodium is reabsobred
How much glucose is filtered, excreted, and reabsorbed per day?
180 g is filtered per day, with 0 g being excreted. 100% is reabsorbed
How much urea is filtered, excreted, and reabsorbed per day?
54 g is filtered per day, with 30 g being excreted. 44% is reabsorbed. This makes sense (low reabsorption) as urea is a waste product
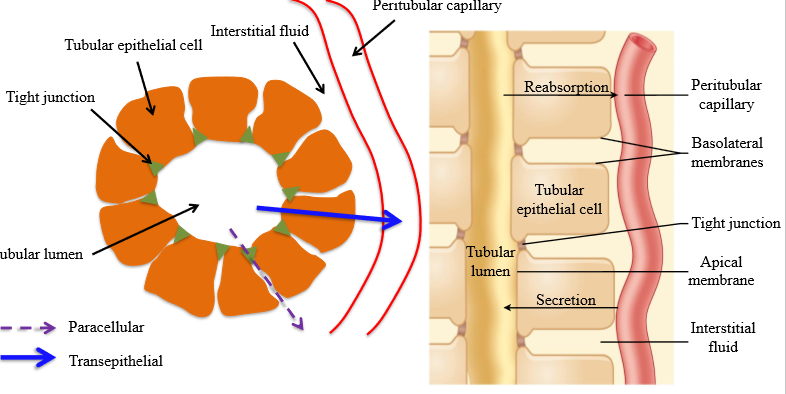
What are the 2 mechanisms that mediate tubular reabsorption
1. Diffusion across the tight junction (paracellular): minor part
2. Carrier mediated transport (transepithelial): major part
What is the importance of Sodium reabsorption in the kidney?
The reabsorption of other molecules (glucose, urea) depends on the reabsorption of sodium
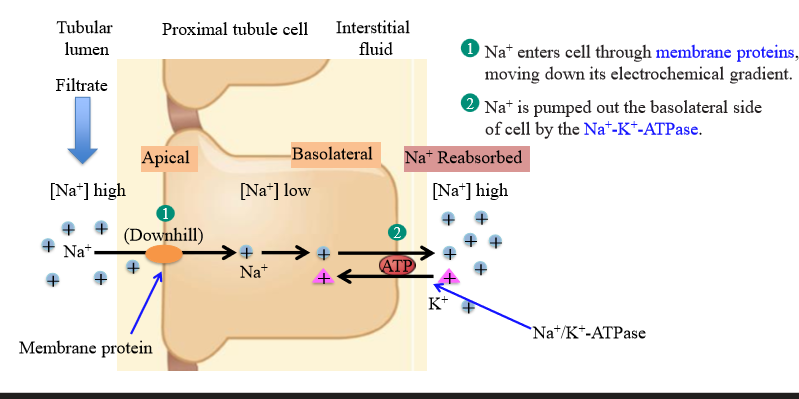
Steps of sodium reabsorption from the tubular lumen to the peritubular capillary
1. Sodium moves into luminal/apical surface via passive diffusion (carrier mediated via transport protein)
2. Sodium moves out of the tubular epithelial cell via the Na+/K+ ATPase (3Na out, 2K in) into the interstitial fluid. Utilizes ATP to pump
3. Sodium enters the peritubular capillary via bulk flow
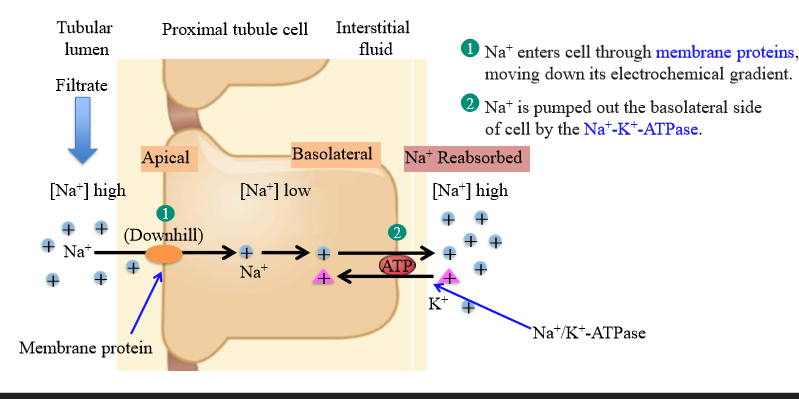
What allows sodium to flow into the tubule epithelial cell via passive diffusion
The Na+/K+ ATPase maintains the concentration gradient, so that there is a low intracellular concentration of sodium
At normal plasma glucose concentration, the clearance of glucose is ....
Zero. All filtered glucose is reasbsobred
What happens when glucose is above the renal threshold?
Glucose will appear in urine
Steps of glucose reabsorption in the proximal tubule
1. Na+ moves down electrochemical gradient using SGLT protein, which allows glucose to move into the cell up its concentration gradient (secondary active transport)
2. Glucose diffuses out of the basolateral side of the cell via GLUT protein (carrier-mediated facilitated diffusion)
3. Na+ is pymped out of the cell via Na+/K+ ATPase to create concentration gradient for glucose to diffuse into cell
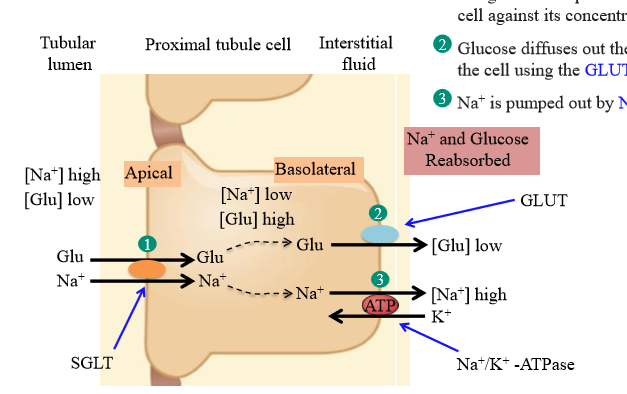
Main differences between glucose and Na+ reabsorption in PCT
Glucose: movement across the apical surface is active transport (sodium is passive). Movement across the basolateral surface is passive transport (sodium is active)
Apical surface protein for glucose reabsorption
SGLT transporter
Basolateral surface protein for glucose reabsorption
GLUT transporter
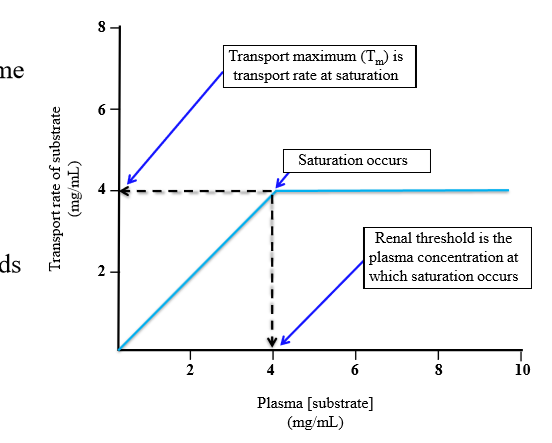
Transport maximum
Limit of substance that can be transported per unit time. It is the maximum reabsorption rate of glucose
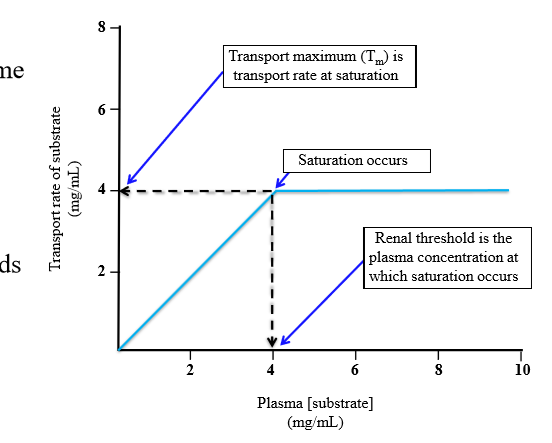
What causes the transport maximum to occur
Binding sites of transport proteins becomes saturated - filtered load exceeds limit of reabsorption (finite number of transport proteins on finite number of cells)
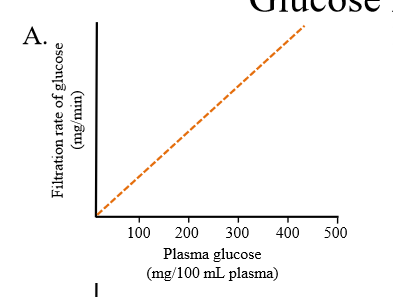
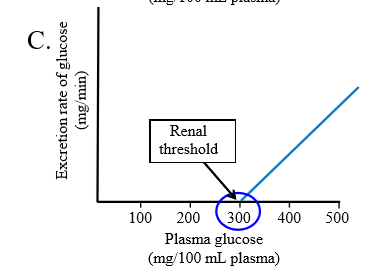
Relationship between Filtration rate of glucose and plasma glucose
Linear relationship. The more glucose in the blood, the more glucose gets filtered at the glomerulus
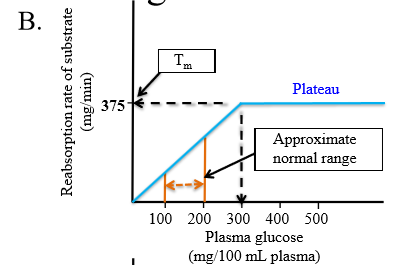
Relationship between reabsorption rate of glucose and plasma glucose concentration
Linear up to 300 mg/100mL of glucose. Then the reabsorption rate plateaus (transport maximum)
Relationship between rate of glucose excretion and plasma glucose
Linear. The more plasma glucose you have, the more glucose is excreted. The graph begins at the renal threshold: 300 mg/100mL
Two causes of glucose appearance in blood
Diabetes mellitus, Renal Glucosuria (benign glucosuria or familial renal glucosuria)
Diabetes mellitus
Capacity to reabsorb glucose is normal, but filtered load is greatly increased and beyond threshold level to reabsorb (but SGLT transporter is functioning)
What causes diabetes mellitus
Insulin resistance, no insulin production
Renal glucosuria
Genetic mutation of SGLT transporter that mediates reabsorption of glucose into proximal tubules
Is urea freely filtered?
Yes. Whatever urea is found in plasma will be filtered into Bowman's space
How does urea get reabsorbed
Diffusion dependent on water reabsorption (follows water)
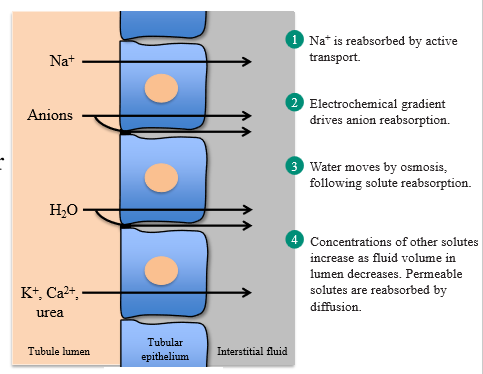
Steps of urea reabsorption
1. Na+ is reabsorbed by active transport
2. Electrochemical gradient drives anion reabsorption (down gradient)
3. Interstitial fluid is more concentrated, so water moves into interstitial fluid via osmosis, following electrolytes
4. Concentration of tubular solutes increases as fluid volume decreases. Solutes (urea) will move via diffusion
What is tubular secretion
Movement of substances from the peritubular capillaries into the tubules
Common substances that are secreted into the tubules
H+, K+, Choline, Creatinine, Penicillin
Method of tubular secretion
Involves active transport, and is often coupled to Na+ reabsorption
Renal clearance
A way of quantifying kidney function in removing substances from plasma. It measures the volume of plasma from which a substance is completely removed by the kidney per unit time
How to calculate renal clearance
C= U x V / P
U is urine [ ]x
V is urine flow rate (mL/min)
P is plasma [ ]x
What is the renal clearance of inulin if urine concentration is 300 mg/L, urine flow rate is 0.1L/h, and plasma concentration is 4mg/L
C = (300 mg/L x 0.1L/hr) / 4 mg/L = 7.5L/hr = 180 L/day
What is the special case of Inulin renal clearance
Normal inulin renal clearance is equal to the glomerular filtration rate. Acts as an excellent way to assess kidney function
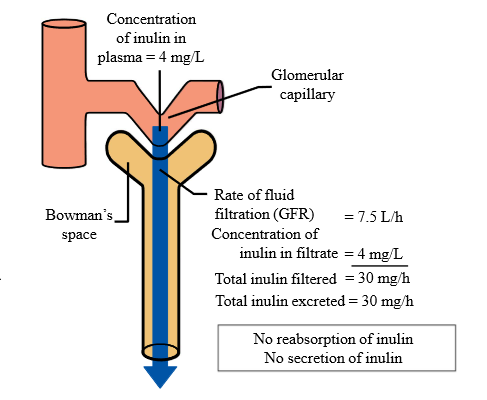
Is inulin reabsorbed or secreted in the kidney?
No. It is only filtered. That is why renal clearance can calculated GFR
Use of creatinine to measure GFR
Creatinine is filtered, not reabsorbed, but undergoes slight secretion. Creatinine clearance will slightly overestimate GFR, but it can be used clinically to assess kidney function
What is creatinine
Product of muscle metabolism
If clearance of a substance is > GFR, this means that the substance undergoes...
Secretion into tubules from peritubular capillaries
Example of a compound where clearance > GFR
Para-aminohippuric acid, or any other organic acid/base
If clearance of a substance is
Reabsorption from tubules into peritubular capillaries
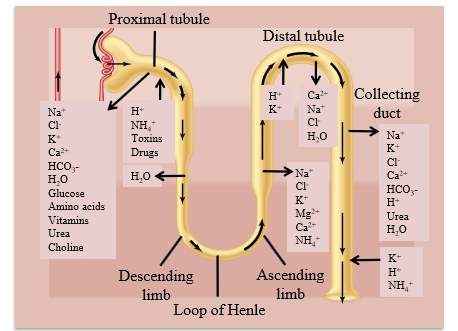
Ion transport in the nephron
- Na+ is actively reabsorbed
- Cl- is transported passively when Na+ is pumped out of the cell
- K+ is secreted into tubules by cells of DCT and collecting ducts
Role of PCT in nephron
Reabsorbs most water and non-waste plasma solutes. Also acts as major site of solute secretion (except for K+)
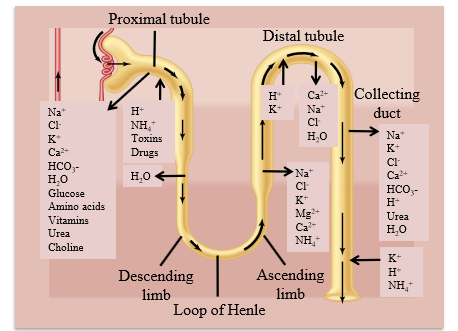
Role of loop of henle in nephron
Creates osmotic gradient - reabsorbs large amounts of ions and less amounts of water
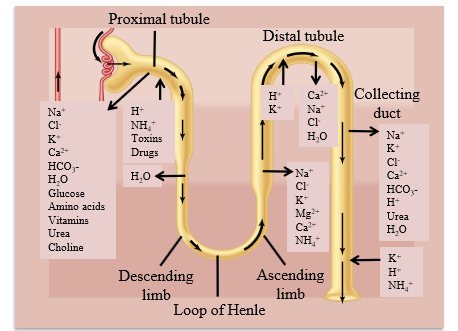
Role of DCT in nephron
Major homeostatic mechanisms of fine control of water and solute to produce urine
What percent of PCT activity is resorptive
80%
What % of DCT activity is reabsorptive
12-15%