Leukocyte Development and Immune Functions
1/217
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
218 Terms
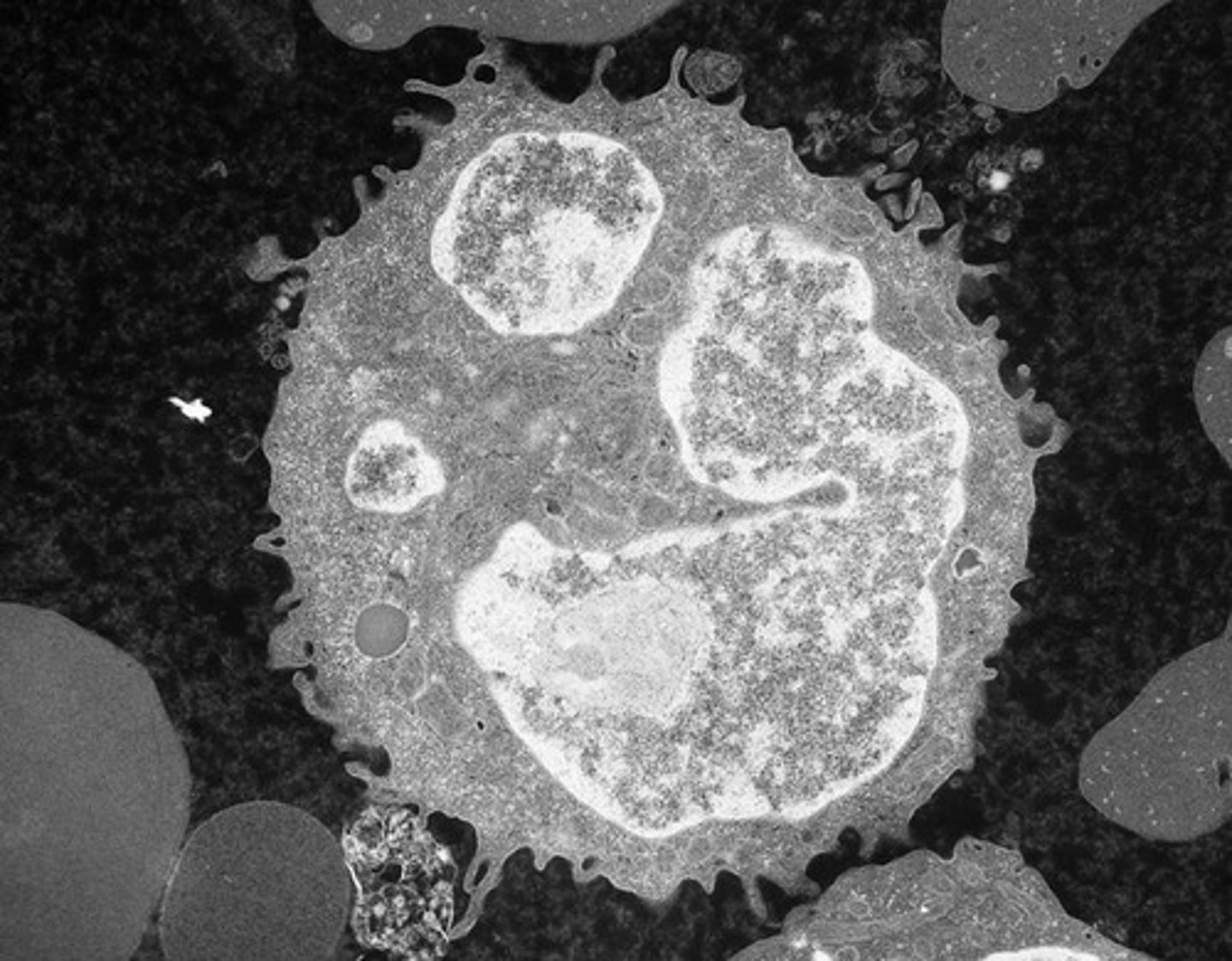
Leukocytes
White blood cells involved in immune response.

Hematopoietic Stem Cell
Stem cell that gives rise to all blood cells.
Granulocytes
Leukocytes with granules in their cytoplasm.
Mononuclear Cells
Leukocytes with a single, non-segmented nucleus.
Neutrophils
Most abundant leukocytes, involved in phagocytosis.
Eosinophils
Leukocytes that combat parasitic infections.
Basophils
Leukocytes involved in allergic reactions.
Monocytes
Leukocytes that differentiate into macrophages.
Lymphocytes
Key players in adaptive immunity.
Cytokines
Signaling molecules that mediate immune responses.
G-CSF
Granulocyte colony-stimulating factor, stimulates neutrophil production.
Kinetics
Movement of cells through developmental stages.
Promonocytes
Precursor cells that develop into monocytes.
Myeloblasts
Immature cells that develop into granulocytes.
Promyelocytes
Stage in neutrophil development with basophilic granules.
Myelocytes
Stage in neutrophil development with distinct granules.
Metamyelocytes
Mature stage of neutrophil development before band cells.
Band Neutrophils
Immature neutrophils with band-shaped nuclei.
Segmented Neutrophils
Mature neutrophils with lobulated nuclei.
Hematogones
Immature B cells found in bone marrow.
Natural Killer Cells
Lymphocytes that attack virus-infected cells.
Plasma Cells
B cells that produce antibodies.
Mast Cells
Cells involved in allergic responses and inflammation.
Immune Response
Body's defense mechanism against pathogens.
Flow Cytometry
Technique to identify leukocyte types via surface antigens.
Romanowsky Stain
Staining technique for visualizing blood cells.
Reference Interval
Normal range for leukocyte counts in blood.
Acute Myeloid Leukemia
Cancer characterized by rapid growth of myeloblasts.
HSCs
Hematopoietic stem cells, origin of blood cells.
CMPs
Common myeloid progenitors, precursors to myeloid cells.
GMPs
Granulocyte-monocyte progenitors, lead to granulocytes.
Type I Myeloblast
High N:C ratio, no visible granules.
Type II Myeloblast
Contains few azure granules, larger than Type I.
Type III Myeloblast
More heterochromatin, nucleoli absent.
Myelocyte
Final mitotic stage, produces secondary granules.
Metamyelocyte
Indented nucleus, no division capability.
Band Neutrophil
9% to 32% of marrow cells, indented nucleus.
Segmented Neutrophil
7% to 30% of marrow cells, lobed nucleus.
Proliferation Pool
Stage where cell division occurs.
Maturation Pool
Stage for storage of mature cells.
Stem Cell Pool
Reservoir of hematopoietic stem cells.
IL-3
Interleukin-3, stimulates hematopoiesis.
GM-CSF
Granulocyte-macrophage colony-stimulating factor.
Primary Granules
Formed during promyelocyte stage, last to release.
Secondary Granules
Formed during myelocyte stage, contain specific proteins.
Tertiary Granules
Formed during metamyelocyte stage, second to release.
Secretory Granules
First to release, contain surface proteins.
Neutrophil
Most abundant leukocyte, fights infection.
Cytoplasmic Basophilia
Presence of RNA, indicates cell maturity.
Nucleus-to-Cytoplasm Ratio
Indicator of cell maturity, varies by cell type.
Dawn of Neutrophilia
Early myelocyte stage, secondary granules appear.
Clinical Utility of Band Counts
Controversial, often included in neutrophil counts.
Pediatric Neutrophil Values
Differ significantly from adult values.
Pediatric leukocyte values
Leukocyte percentages differ significantly in children.
Circulating Neutrophil Pool (CNP)
Neutrophils freely circulate in the bloodstream.
Marginated Neutrophil Pool (MNP)
Neutrophils loosely adhere to capillary walls.
Neutrophil half-life
Neutrophils survive approximately 7 hours in blood.
Neutrophil production rate
Production is 0.9 to 1.0 x 10^9 cells/kg/day.
Proliferative pool
Contains about 2.1 x 10^9 neutrophils.
Maturation pool
Holds roughly 5.6 x 10^9 neutrophils.
Diapedesis
Process for neutrophils to exit blood into tissues.
Apoptosis
Programmed cell death of neutrophils.
Bcl-2 family
Regulates neutrophil apoptosis via pro- and anti-apoptotic signals.
Neutrophil rolling
Transient adhesion to endothelial cells during migration.
Chemokines
Facilitate neutrophil activation and rolling on endothelium.
Integrins
Molecules that stabilize neutrophil adhesion.
Transmigration
Neutrophils move through endothelial cells to tissues.
Phagocytosis
Process of engulfing and destroying pathogens.
Surface receptors
Recognize pathogens or opsonic molecules for phagocytosis.
Pseudopodia
Extensions of neutrophils that surround pathogens.
Phagosome
Vesicle formed around engulfed particles in neutrophils.
Respiratory burst
Activation of NADPH oxidase producing reactive oxygen species.
Oxygen-independent killing
Digestive enzymes function in neutral pH phagosome.
Neutrophil Extracellular Traps (NETs)
DNA and enzymes expelled to trap pathogens.
Chemotaxis
Movement of neutrophils towards chemical signals.
Eosinophil characteristics
Large reddish-orange granules in eosinophil myelocytes.
Reactive oxygen species
Molecules generated to kill pathogens during phagocytosis.
Myeloperoxidase (MPO)
Enzyme that converts hydrogen peroxide to hypochlorite.
Primary lysosomes
Contain hydrolytic enzymes for pathogen digestion.
Secondary lysosomes
Fuse with phagosomes to release bactericidal molecules.
Bilobed nucleus
Characteristic nuclear shape of mature eosinophils.
Secondary granules
Granules that increase in number during maturation.
Secretory granule
Granule type involved in secretion processes.
Tertiary granules
Granules that degrade extracellular matrix.
NETs
Extracellular traps formed by dying neutrophils.
NETosis
Neutrophil death resulting in NET formation.
Transcobalamin I
Protein necessary for vitamin B12 absorption.
Eosinophil kinetics
Study of eosinophil development and turnover.
Myelocyte division time
3.5 days from myelocyte to mature eosinophil.
Eosinophil turnover rate
Approximately 2.2 x 10^8 cells/kg per day.
Storage pool
9 to 14 x 10^8 eosinophils/kg in marrow.
Primary granules
Contain Charcot-Leyden crystal protein.
Degranulation
Process of eosinophils releasing granule contents.
Classical exocytosis
Granules fuse with plasma membrane to release contents.
Compound exocytosis
Granules fuse together before membrane fusion.
Piecemeal degranulation
Selective release of specific proteins from granules.
Cytolysis
Release of intact granules during cell lysis.
Eosinophil lifespan
Circulating half-life is approximately 18 hours.
Tissue survival time
Eosinophils survive 2 to 5 days in tissues.
Eosinophil functions
Roles include immune regulation and inflammation.