Pathology of Inner Ear
1/90
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
91 Terms
How is vertigo defined?
Either to a sensation of movement when there is no motion or an exaggerated sense of motion in response to movement.
What clinical factors are key to diagnosing vertigo?
Duration of vertigo episodes with associated hearing loss or other neurologic issues.
Is vertigo a diagnosis or a symptom?
Vertigo is a symptom; NOT a diagnosis.
What are the three potential etiologies for vertigo?
Peripheral etiology; central etiology; or both.
What aspects of the medical history are crucial when evaluating dizziness or vertigo?
Duration of episodes of vertigo (seconds; minutes; hours; days);
Associated symptoms (hearing loss; migraine related symptoms);
Triggers (increased salt intake; stress; fatigue; bright lights);
Substance use;
Patient’s medications.
Which categories of medications are relevant when evaluating vertigo?
Anticonvulsants; BP meds; antibiotics; hypnotics; analgesics; tranquilizer medications.
What components should be included in the physical exam of a patient with dizziness/vertigo?
Evaluation of ears; Observation of eye motion and nystagmus in response to head turning; Cranial nerves; Romberg testing.
If balance is fine with eyes open but lost when eyes are closed → positive Romberg sign, meaning proprioceptive or sensory ataxia (problem with dorsal columns or peripheral nerves).
If balance is lost even with eyes open → cerebellar problem.
What is the typical presentation of vertigo caused by peripheral vestibulopathy?
Vertigo of sudden onset; may be so severe that the patient can’t walk or stand; and is often accompanied by Nausea/Vomiting (N/V).
What associated symptoms provide strong support for a peripheral (otologic) origin of vertigo?
Tinnitus and hearing loss.
Describe the typical pattern of nystagmus seen in peripheral lesions.
Usually horizontal with a rotatory component.
What type of nystagmus is characteristic of Benign Paroxysmal Positional Vertigo (BPPV) during the Dix-Hallpike testing?
Fatigable nystagmus.
If nystagmus is non-fatigable, what disease process should be considered?
CNS disease
How does vertigo arising from CNS disease typically progress?
Tends to develop gradually and progressively become more severe and debilitating.
Describe the characteristics of nystagmus in CNS disease.
Not always present but can occur in any direction; may be associated in the two eyes; often non-fatigable; vertical rather than horizontal; without latency; and unsuppressed by visual fixation.
What neuroimaging modality is required if CNS disease is suspected in a patient with vertigo?
MRI of the brain.
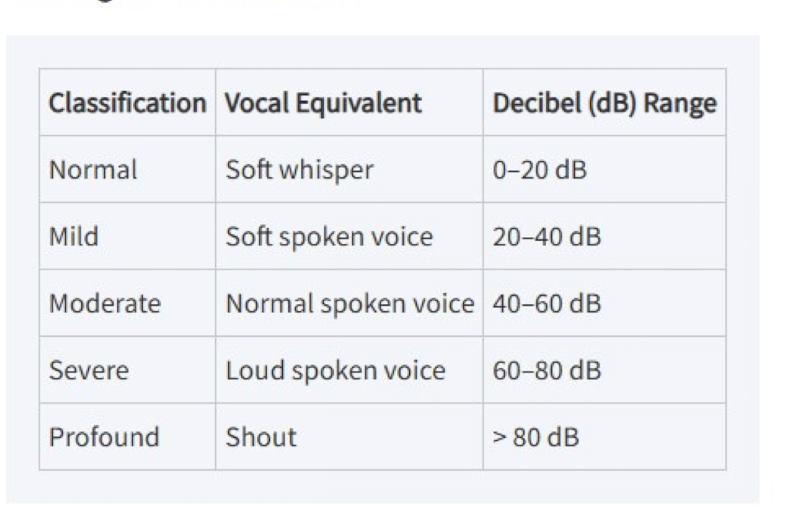
What diagnostic tools help distinguish between central and peripheral lesions causing persistent vertigo?
Audiologic evaluation;
caloric stimulation;
electro- or videonystagmography (ENG or VNG);
vestibular-evoked myogenic potentials (VEMPs); and
MRI
What’s the difference between dizziness and vertigo?
Dizziness is a vague feeling of lightheadedness, unsteadiness, or imbalance that can have many causes (e.g., cardiovascular, metabolic, or anxiety-related).
Vertigo is a specific type of dizziness — a false sense that you or the environment are spinning, usually due to an inner ear or brain disorder.
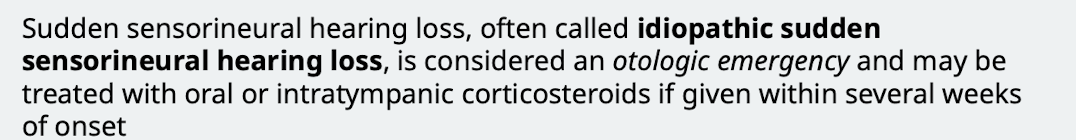
How is hearing loss generally categorized and classified?
Categorized as either conductive or sensorineural; and classified as mild; moderate; severe or profound
How can a normal spoken voice level be quantified?
About 60 decibels.
What is the purpose of using a tuning fork in hearing loss evaluation?
To differentiate conductive from sensorineural hearing loss.
How is the Weber test performed?
The tuning fork is placed directly on the forehead.
How is the Rinne test performed?
The tuning fork is placed alternately on the mastoid bone (bone conduction) and in front of the ear canal (air conduction).
When is immediate audiometric referral necessary for hearing loss?
For patients with idiopathic sudden sensorineural hearing loss (SSNHL) as it requires treatment (corticosteroids) within a limited several-week time period.
anyone who reports hearing loss should be referred though for audiologic evaluation
What is the underlying cause of conductive hearing loss (CHL)?
Results from mechanical disruption of the external auditory canal or middle ear.
List the four mechanical mechanisms that result in impairment of sound vibration passage in CHL.
Obstruction (cerumen impaction);
Mass loading (middle ear effusion);
Stiffness (otosclerosis);
Discontinuity (ossicular disruption).
What are the most common causes of conductive hearing loss in adults?
Cerumen impaction or transient eustachian tube dysfunction from a URI.
What typically causes persistent conductive hearing loss?
Chronic ear infection; trauma; or otosclerosis.
peforartion of TM may also cause conductive hearing loss.
What is the Weber test result in conductive hearing loss?
Sound is heard as louder in the affected ear.
What is the Rinne test result in conductive hearing loss when hearing loss is greater than 25 dB?
Bone conduction sounds are louder than air conduction sounds.
What else may be used in addition to PE to determine the potential cause of conductive hearing loss?
CT
How is conductive hearing loss often treated?
Often correctable with medical (i.e. use of a hearing aid) or surgical (i.e. repair of tympanic membrane and ossicular chain) therapy or both.
What causes sensorineural hearing loss (SNHL)?
Deficits of the inner ear or central (brain) auditory pathway.
What is the physiological cause of most SNHL originating in the inner ear?
Deterioration of the cochlea; usually due to sensory hair cells within the organ of Corti.
What is the most common form of SNHL?
Age-related hearing loss that manifests as a gradually progressive; predominantly high-frequency hearing loss.
If a patient presents with sudden sensorineural hearing loss, how should it be managed?
What surgery can be used to treat severe to proofund sensorineural hearing loss due to deficits of the innear ear
cochlear implantation
SNHL can be due to central auditory pathway deficits involving which structures?
CN VIII; auditory nuclei; ascending tracts; or auditory cortex.
What are examples of central causes of SNHL?
Acoustic neuroma; MS; auditory neuropathy.
Treatment for central causes is aimed at addressing underlying pathology
What is the Weber test result in sensorineural hearing loss?
Sound radiates to the ear that hears better.
What is the Rinne test result in sensorineural hearing loss?
Normal; air conduction will be > bone conduction.
What are the characteristics of Presbycusis?
Age-related hearing loss; the most common cause of SNHL; progressive; predominantly high frequency; and symmetrical.
What is the second most common cause of SNHL?
Noise trauma.
about ___ of people between ages 65-75 and almost ____ of patients over age 75 experience hearing difficulties
25%, 50%
Many patients also have subliclinical hearing loss
What sound exposure criteria are potentially injurious to the cochlea?
Sounds > 85 dB for 8 hours or more.
In noise trauma, where does hearing loss typically begin and progress?
high frequencies and with continuing exposure, progresses to involve speech frequencies
Concussive head trauma has effects on the inner ear similar to what other condition?
Those of severe acoustic trauma.
Some degree of sensory hearing loss may occur following ______and is frequent after ________
concussion , lateral skull base fractures
What are the most common ototoxic medications? What is their prognosis?
Aminoglycosides; loop diuretics; and several antineoplastic agents like cisplatin.
They cause IRREVERSIBLE hearing loss even in therapeutic doses
Why should topical aminoglycosides be avoided if the tympanic membrane (TM) is perforated?
It is possible for these (neomycin; gentamicin) to be absorbed from the middle ear into the inner ear.
How do cochlear implants help patients with severe to profound sensory hearing loss?
The cochlear implant offers socially beneficial auditory rehabilitation; it is an electronic device surgically implanted into the cochlea to stimulate the auditory nerve.
What is the pathophysiology of Meniere’s Disease?
Idiopathic distention of endolymphatic compartment of the inner ear by excess fluid
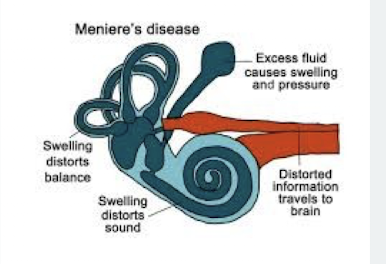
What is the classic syndrome consisting of Meniere’s disease symptoms?
Episodic vertigo lasting minutes to hours; fluctuating low-frequency sensorineural hearing loss; tinnitus; and sensation of unilateral aural pressure.
What is the primary treatment approach for Meniere’s disease?
Symptomatic; decreasing dizzy episodes; usually preventative treatment includes low-salt diet and daily diuretics (to reduce pressure).
What substances should patients with Meniere’s disease avoid because they can increase endolymphatic pressure?
Salt; caffeine; alcohol; chocolate.
What is used for treatment of severe meniere’s disease? what about for the reduction in hearing loss?
Patients may undergo intratympanic corticosteroid or gentamicin injections, endolymphatic sac decompression or surgical or vestibular nerve section
There are no treatments for reduction in hearing loss
What is an Acoustic Neuroma?
Cranial Nerve VIII Schwannoma; the most common intracranial tumor; a benign tumor of Schwann cells.
Acoustic neuromas are usually _______, but on the rare occasion that it isn’t it is associated with ________
unilateral, neurofibromatosis type 2
What clinical finding is considered an acoustic neuroma until proven otherwise?
Unilateral or asymmetric sensorineural hearing loss.
How does vestibular dysfunction present in patients with an acoustic neuroma?
Continuous disequilibrium rather than episodic vertigo.
How is acoustic neuroma diagnosed and monitored?
MRI w/ contrast.
How is acoustic neuroma treated?
observation, microsurgical excision or stereotactic radiotherapy depending on patient age, health, size of tumor, etc
Tumors usually grow slowly and don’t spread throughout the body
What is Vestibular Neuritis?
A viral or postviral inflammatory disorder affecting the vestibular portion of CN VIII.
History of preceding viral illness seen in almost 50% of patients
What is the clinical presentation of Vestibular Neuritis?
Acute; spontaneous; peripheral vestibular ailment characterized by rapid onset of severe vertigo with nausea; vomiting; and gait instability.
What two exam findings are consistent with acute vestibular imbalance in Vestibular Neuritis?
Spontaneous vestibular nystagmus; Positive head impulse test.
What is the treatment for vestibular neuritis?
Symptomatic to reduce vertigo, nausea, and vomiting
antiemetics, antihistamines, anticholinergics
What is Labyrinthitis?
Inflammation of the labyrinth; which is responsible for hearing and balance; cause is unknown.
What are the key symptoms of Labyrinthitis? What happens during the recovery phase? what about hearing?
Acute onset of continuous; usually severe vertigo lasting several days; accompanied by hearing loss and tinnitus.
During a recovery phase, the vertigo gradually improves
Hearing may return to normal or remain permanently impaired in the affected ear
What is the treatment for labyrinthitis
consists of antibiotics (if febrile or sxs of infection), oral corticosteroids and supportive care
Why should vestibular suppressants like diazepam be stopped as soon as possible during recovery from Labyrinthitis?
They help during acute phase but to avoid long-term disequilibrium from inadequate compensation they should be stopped
What is Benign Paroxysmal Positional Vertigo (BPPV)?
Recurrent spells of vertigo; lasting a few seconds per spell; associated with changes in head position.
Movement of the head causes otoliths to be displaced → vertigo
What is the most common cause of vertigo?
BPPV.
How long do acute vertigo spells typically last in BPPV? What can help?
1-60 seconds.
Constant repetition of the positional change leads to habituation
What sign can be used to rule out BPPV?
dizziness that lasts more than a few seconds is NOT BPPV
Some CNS disorders can mimic BPPV however in central lesions there is no…
latent period, fatigability or habituation of signs or symptoms
What maneuver is used to confirm the diagnosis of BPPV?
Dix-Hallpike maneuver.
Perform provoking maneuver and observe symptoms and nystagmus to confirm diagnosis
What are the two main physical therapy protocols used to treat BPPV?
The Epley maneuver and Brandt-Daroff exercises.
Which treatment is considered first line for BPPV and provides more immediate symptom relief? Why is the other not first line? What other treatment is possible?
The Epley maneuver.
Brandt-Daroff exercises focus more on habituation and may take longer for results
Symptomatic treatment also can be provided (i.e. antihistamines, anticholinergics, benzodiazepines)
How is tinnitus defined?
Sensation of sound in the absence of an exogenous sound source.
What does persistent tinnitus indicate?
Presence of hearing loss
What type of tinnitus should be distinguished from tonal tinnitus?
Pulsatile tinnitus; often described by the patient as hearing one’s own heartbeat.
Pulsatile tinnitus may indicate what type of underlying issue?
Vascular abnormality such as glomus tumor; venous sinus stenosis; carotid vaso-occlusive disease; AV malformation or aneurysm.
What type of tinnitus is described as continuous defined frequency sound like ringing or buzzing?
Tonal tinnitus.
What is staccato “clicking” tinnitus, its cause, symptoms, and typical treatment?
Cause: Middle ear muscle spasm or palatal myoclonus
Symptoms: Rapid series of popping noises lasting seconds to minutes, often with a fluttering sensation in the ear
Treatment: Usually surgical
What should be ordered for routine non-pulsatile tinnitus and why?
audiometry to rule out associated hearing loss
If a patient reports unilateral tinnitus associated with hearing loss in the absence of an obvious causative factor? What should be ordered and why?
an MRI to rule out acoustic neuroma
What should you consider ordering for pulsatile tinnitus and why?
MRA, MRV, and temporal bone CT to exclude causative vascular lesion or sigmoid sinus abnormality
What is the mainstay of treatment for routine non-pulsatile tinnitus?
Avoiding exposure to excessive noise; ototoxic agents; and other factors that may cause cochlear damage.
A 45-year-old female presents with recurrent episodes of spinning sensation lasting 45 minutes; associated with a ringing sound and feeling of fullness in her left ear. She reports her hearing has been worsening intermittently. What is the likely diagnosis?
Meniere’s disease; defined by episodic vertigo lasting minutes to hours; fluctuating low-frequency sensorineural hearing loss; tinnitus; and sensation of unilateral aural pressure.
A 68-year-old male is evaluated for gradually worsening hearing loss unilaterally in his right ear. He denies acute spinning episodes but reports continuous unsteadiness (disequilibrium). What diagnosis must be ruled out via MRI w/ contrast?
Acoustic neuroma (CN VIII Schwannoma); which presents with unilateral or asymmetric SNHL until proven otherwise; and continuous disequilibrium.
A 72-year-old patient complains of brief spells of intense vertigo (lasting 10-15 seconds) whenever he rolls over in bed. Physical exam reveals fatigable; horizontal nystagmus upon quickly moving the head backward and to the side. What is the most common cause of vertigo demonstrated by this presentation?
Benign Paroxysmal Positional Vertigo (BPPV); characterized by recurrent spells lasting a few seconds; associated with head position changes; and diagnosed using the Dix-Hallpike maneuver which reveals fatigable nystagmus.
A patient presents with acute onset; continuous; severe vertigo accompanied by nausea and vomiting; which began suddenly three days after recovering from a cold. Physical exam is notable for spontaneous nystagmus and a positive head impulse test. What is the clinical diagnosis?
Vestibular neuritis; understood to be a viral or postviral inflammatory disorder affecting the vestibular portion of CN VIII; characterized by rapid onset of severe vertigo; nausea; vomiting; and gait instability.