ch 11- schizophrenia
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
schizophrenia
chronic, debilitating psychological disorder that touches every facet of the person’s life → characterized by a break with reality that typically takes the form of hallucinations and delusions and by a pattern of aberrant behavior
hallucinations: sensory distortions such as hearing voices or seeing things
delusions: fixed, false beliefs
course of development of schizophrenia
typically begins during late adolescence or early adulthood
same cases onset can occur suddenly
prodromal phase
residual phase
its a chronic disorder but 1/2- 2/3 patients improve significantly overtime with medication and therapy
prodromal phase
gradual deterioration; characterized by subtle symptoms involving unusual thoughts or abnormal perceptions, as well as waning interest in social activities, difficulty meeting responsibilities of daily living; and impaired cognitive functioning involving problems with memory and attention, use of language, and ability to plan and organize one’s activities
one of first signs of prodrome is lack of attention to one’s appearance
over time behavior gets odd, speech becomes vague
changes in personality may be so gradual that they may raise little concern among family and friends at firs
residual phase
after acute psychotic episodes, behavior returns to the level of the prodromal phase
flagrant psychotic behaviors are absent but person is still impaired by significant cognitive, social and emotional deficits , and difficulties thinking or speaking clearly and holding unusual ideas
key features of schizophrenia
acute episodes of schizophrenia involve break in reality
marked by delusions, hallucinations, illogical thinking, incoherent speech, and bizarre behavior
in between episodes may have lingering deficits
40% of patients have long periods of remission that last a year or longer
prevelence of schizophrenia
0.25-0.64 % of population of americans
men have higher risk and develop disorder earlier
peak period of life when psychotic symptoms first appear are middle 20s for men late 20s for women
features of schizophrenia cont
differences in men and women suggest they develop different forms of schizophrenia or it affects different areas of the brain
men have more cognitive impairment, greater behavior deficits, and poorer response to drug therapy than women
women have higher level of functioning before the onset of the disorder and have less severe course of illness than men
schizophrenia occurs universally across cultures but some particular symptoms that emerge may vary from culture to culture
visual hallucinations are more common in non-Western culture
dsm 5 criteria schizophrenia
A) two or more of the following, each present for a significant portion of time during a 1 month period (or less if successfully treated) at least one of these must be (1), (2), or (3)
delusions (1)
hallucinations (2)
disorganized speech (3)
grossly disorganized or catatonic behavior
negative symptoms
(B) for a significant portion of time since the onset of the disturbance, level of functioning in one or more major areas, such as work, interpersonal relations, or self care, is markedly below the level achieved prior to the onset (or when the onset is in childhood or adolescence, there is failure to achieve expected level of interpersonal, academic, or occupational functioning)
(C) continuous signs of the disturbance persist for at least 6 months. during this period must include at least 1 month of symptoms that meet criterion A, and must include periods of prodromal or residual symptoms. during these prodromal or residual periods, the signs of the disturbance may be manifested by only negative symptoms or by two or more symptoms listed in criterion A present in an attenuated for (odd beliefs, unusual perceptual experiences)
(D) schizoaffective disorder, depressive or bipolar disorder with psychotic features have been ruled out(E) disturbance is not attributable to the physiological effects of a substance or another medical condition
(F) if there is a history of autism spectrum disorder or a communication disorder of childhood onset, the additional diagnosis of schizophrenia is made only if prominent delusions or hallucinations, in addition to other required symptoms of schizophrenia, are also present for a least one month
positive and negative symptoms of schizophrenia
positive symptoms: atypical excesses of behavior involving a break with reality, including hallucinations and delusional thinking
negative symptoms: behavioral deficits or absences of typical behaviors and emotions that affect a person’s ability to function in daily life
includes lack of emotional responses, loss of motivation, loss of pleasure, lack of social relationships, limited verbal expression
Aberrant content of thought (disturbed thoughts and speech)
delusions involve disturbed content of thought in form of false beliefs that remain fixed despite their illogical bases
delusions of persecution or paranoia
delusions of reference
delusions of being controlled
delusions of grandeur
thought broadcasting
thought insertion
thought withdrawal
aberrant forms of thought (disturbed thought and speech)
people with schizophrenia tend to think in a disorganized, illogical fashion
thought disorder: positive symptom of schizophrenia involving a breakdown in the organization, processing, and control of thoughts
looseness of associations is sign of disorder
poverty of speech is another sign of disorder
less common signs: neologisms (made up words), perseveration (inappropriate but persistent repetition of same words), clanging (stringing together of words), and blocking (involuntary, abrupt interruption of speech of thought)
attentional deficiencies
core feature of schizophrenia is sensory deficit that makes it difficult to filter out irrelevant stimuli → makes it difficult to organize thoughts and focus attention
hypervigilent
eye movement dysfunction
abnormal event related potentials
hypervigilant
acutely sensitive to extraneous sounds, especially during early stages
of the disorder
eye movement dysfunction
difficulty tracking slow moving targets across their field of vision, fall back then catch up in jerky movement
common in people with schizophrenia and in first degree relatives → suggests its a biomarker (associated with genes linked to schizophrenia
abnormal event related potentials
event related potentials: brain wave patterns which occur in response to external stimuli such as sounds and flashes of light
normally sensory gating mechanism in the brain suppresses event related potentials to a repeated stimulus occurring within the first hundredth of a second after stimulus is presented → people with schizophrenia doesn’t work effectively leading to sensory overload
hallucinations (perceptual disturbances)
auditory hallucinations is most common symptom of schizophrenia → 70% of schizophrenia patients have auditory hallucinations
most voices are critical
5% of general population have experienced temporary hallucinations, does not mean they have schizophrenia
causes of hallucinations
unknown, but speculations
dopamine is thought to have an effect → anti psychotics block dopamine activity which reduces hallucinations
auditory cortex becomes active during hallucinations even when there is no sound → scientists speculate auditory hallucinations might be form of internal speech which for unknown reasons becomes attributed to external sources rather than one’s own thoughts
brain mechanisms involved with hallucinations involve number of interconnected symptoms → abnormalities in connections among neurons in the brain may disrupt brain circuits that allow us to distinguish reality from fantasy
emotional disturbances
schizophrenia patients tend to have more negative and fewer positive emotions than healthy individuals
flat affect: loss of normal emotional expression, may speak in monotone and maintain an expressionless face
may also display positive symptoms which involve exaggerated or inappropriate affect; example laughing for no reason or giggling at bad news
even when not showing emotion, most schizophrenia patients internal emotions are like healthy people
lack capacity to express emotions outwardly
other types of impairments
confused about personal identities
ego boundaries: failing to recognize themselves as unique individuals and be unclear about how much of what they experience is part of themselves
difficulty perceiving emotions in others
disturbances of volition
seen in residual or chronic state
characterized by apathy, which is loss of motivation or initiative to pursue goal directed activities
other types of impairments cont
catatonia: unaware of the environment and maintain a fixed or rigid posture
waxy flexibility: adopting a fixed posture into which they have been positioned by others
significant impairment to interpersonal relationships
withdraw from social interactions
psychodynamic perspective on schizo
schizophrenia represents the overwhelming of the ego by primitive sexual or aggressive drives or impulses arising from the id
impulses threaten ego and give rise to intense intrapsychic conflict
under such threat, the person regresses to an early period in the oral stage, referred to as primary narcissism
input from id causes fantasies to become mistaken for reality
psychodynamic harry sullivan perspective
placed more emphasis on interpersonal than intrapsychic factors
emphasized that impaired mother-child relationships can set the stage for gradual withdrawal from other people
early childhood anxious and hostile interactions between the child and the parent lead the child to take refuge in a private fantasy world → cycle continues into adulthood, increasing demands causes person to become overhelmed and withdraw completely into world of fantasy
critics point out that schizophrenic behavior and infantile behavior are different, so schizophrenia cannot be explained by regression
learning based perspective
development of some forms of schizophrenic behavior can be understood in terms of conditioning and observational learning
case study: Haughton and Ayllon
conditioned 54 yr old chronic schizophrenia patient to cling to broom using cigarette as reinforcement
after pattern was repeated, the woman would not let go of the broom
social cognitive theorists
modeling of schizophrenic behavior can occur within the mental hospital
biological perspectives
genetic factors
first degree relatives have 10x greater risk of developing schizophrenia than average population
concordance rates
48% for identical twins
17% for fraternal twins
genetic and environmental factors contribute
cross fostering study: compares incidence of schizophrenia among children whose biological parents either had or didn’t have schizophrenia and who were reared by adoptive parents who either had or didnt have schizophrenia
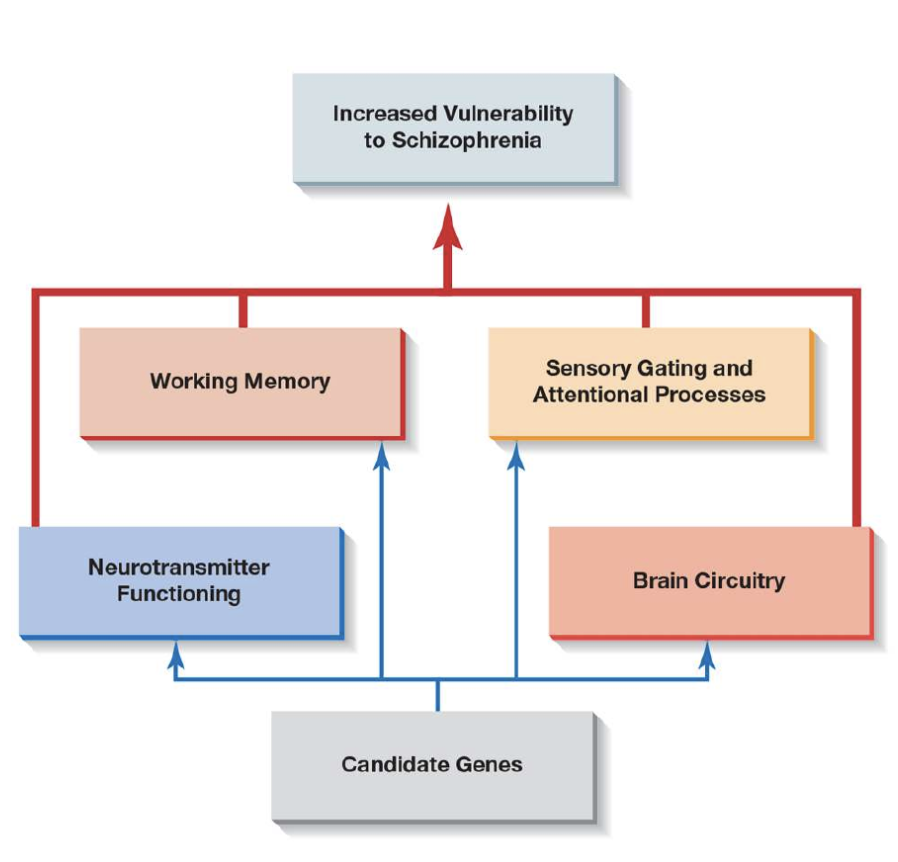
presently, investigators are now zeroing in on particular genes linked to schizophrenia
no single gene responsible for schizophrenia → many different genes contribute to the development of brain abnormalities that, together with stressful environmental influences, lead to schizophrenia
older fathers stand increased risk of developing schizophrenia and autism
dopomine hypothesis
overactivity of dopamine transmission of brain
source of evidence is found in effects of antipsychotic drugs called neuroleptics
first generation of neuroleptics are called phenothiazines
thorazine, mellaril, and prolixin
neuroleptic drugs act like a dam against dopamine → help stop delusions and hallucinations
biochemical factors
dopamine hypothesis
amphetamines can mimic paranoid schizophrenia in normal people
evidence points to irregularities in neural pathways that utilize dopamine in brains of people with schizophrenia
another theory is decreased dopamine may help explain development of negative symptoms
glutamate and GABA may also be involved
viral infections and vitamin d deficiency in prenatal development
schizophrenia is more likely in people who are born in winter in northern hemisphere, time of year associated with the flu
sweden suggests risk posed by prenatal infections may be limited to offspring whose mothers had psychiatric disorders
children born with vitamin D deficiency had 44% higher risk of later developing schizophrenia
brain abnormalities
loss or thinning of brain tissue (gray matter)
clearest signs of deterioration of brain tissue are abnromally enlarged ventricles
brain may have been damaged or failed to develop normally during prenatal development or early childhood as result of genetic factors or environmental influences
not all cases involve structural damage to brain tissue
evidence linking genetic variations in schizophrenia to a thinning or pruning of synaptic connections in the prefrontal cortex of people with schizophrenia
prefrontal abnormalities may explain why people with schizophrenia have problems with working memory
people with schizophrenia may have relatively few pathways (think of them as roadways) in the prefrontal cortex for information to pass from one neuron to another → results in messages becoming bottled up in the veritable “traffic jam” in the brain → results in confused and disorganized thinking
evidence also points to abnormalities in brain circutry connecting the prefrontal cortex and lower brain structures including the thalamus and parts of limbic system involved in regulating emotions and memory
communication deviance (role of family)
pattern of unclear, vague, disruptive, or fragmented communication that is often found among parents and family members of people with schizophrenia
high communication deviance parents often have difficulty focusing on what their children are saying, and verbally attack them rather than offering constructive criticism
parents with high communication deviance stand higher than average risk of having children with schizophrenia spectrum disorders
expressed emotion (role of family)
pattern of responding to the family member with schizophrenia in hostile, critical, and unsupportive ways
people who live in high EE family environments have more than twice the risk of suffering a relapse as those from low EE families
high EE relatives show less empathy, tolerance, and flexibility than low EE relatives and tend to believe that their relatives with schizophrenia can exercise greater control over their disturbed behavior
cultural differences in both the frequency of EE in family members of patients with schizophrenia and the effects these behaviors have on the patients
chinese families with high levels of EE are more likely than low EE families to view the psychotic behavior of a family member with schizophrenia as within the persons control
high EE families are more common in industrialized countries such as US and China vs developing countries such as India
high EE in african american families were associated with better outcomes → critical comments may be perceived as signs of caring and concern rather than rejection
nervios: cultural label attached to wide range of troubling behaviors including anxiety, schizophrenia, depression and one that carries less stigma and more positive expectations than the label of schizophrenia
diathesis stress model

biomedical approaches
antipsychotic drugs help control flagrant behavior patterns such as delusional thinking, hallucinations and reduces need for long term hospitalization
first generation antipsychotics phenothiazines
chlorpromazine (thorazine)
thioridazine (mellaril)
trifluoperazine (stelazine)
fluphenazine (prolixin)
- haloperidol (hadol) similar but chemically different from phenothiazines
- block dopamine receptors in the brain which reduce symptoms such as hallucinations and delusions
effectiveness has been repeatedly demonstrated in double blind placebo controlled studies
tardive dyskinesia
side effect from long term use of neuroleptics
can take different forms
frequent eye blinking
involuntary chewing and eye movements
lip smacking or puckering
facial grimacing
involuntary movements of the limbs and trunk
most common among older people and women
second generation antipsychotics referred to as atypical antipsychotics
same level of effectiveness as first gen antipsychotics but carry fewer side effects and lower risk of tardive dyskinesia
clozapine (clozaril)
risperidone (risperdal)
olanzapine (zyprexa)
side effects
cardiac death
susbtantial weight gain
seizures
metabolic disorders-
lethal disorder where body does not produce enough white blood cells
sociocultural factors in biomedical treatment
asians and hispanics require lower doses than european americans
asians experience more side effects
african americans were less likely to recieve new generation of atypical antipsychotics
psychosocial approaches
psychoanalysis
learning based therapies
CBT
psychosocial rehabilitation
family intervention programs
combined approaches
psychoanalysis
harry sullivan and frieda fromm-reichmann adapted techiques for schizophrenia
learning based therapies
selective reinforcement behavior: providing attention for appropriate behavior and extinguishing bizarre verbalizations through withdrawal of attention
token economy: individuals in inpatient units are rewarded for appropriate behavior with tokens, such as plastic chips, that can be exchanged for tangible reinforcers
social skills training: clients are taught conversational skills and other appropriate social behaviors through coaching, modeling, behavioral rehearsal and feedback
CBT
focuses on changing thinking patterns to help patients with schizophrenia control their hallucinations by means of reattributing their voices to their internal voice or self
help patients avoid cognitive errors such as jumping to conclusions, replace delusional beliefs, combat negative symptoms
Aaron Beck proposes the types of cognitive biases we see in depression patients also play role in accounting for both positive and negative symptoms in schizophrenia patients
psychosocial rehabilitation
help patients strengthen cognitive skills such as attention and memory
self help clubs (clubhouses) and rehabilitation centers have popped up to help patients find a place in society
provides members with social support and help finding educational opportunities and employment
family intervention programs
works with families to help them cope with burden of care and assist them in developing more cooperative, less confrontational ways of relating to others
combined approaches
drug therapy combined with psychological approaches is most effective
brief psychotic disorder
applies to psychotic disorder that lasts from a day to a month and is characteried by at least one of the following features
delusions
hallucinations
disorganized speech
grossly disorganized or catatonic behavior
eventually there is a full return of functioning
Schizophreniform Disorder
consists of abnormal behavior identical to those in schizophrenia that have persisted for at least one month but fewer than six months
usually reclassified as schizophrenia or schizoaffective disorder
delusional disorder
applies to people who hold persistent, clearly delusional beliefs, often involving paranoid themes
affects an estimated 20 people in 10,000 during their lifetime
apart from delusion, the individual’s behavior may not show evidence of obviously bizarre or odd behavior
Schizoaffective Disorder
refers to mood disorder in which one experiences a major mood disorder and psychotic features associated with schizophrenia
in terms of severity of disturbed behavior, schizoaffective is on low end and schizophrenia on the higher end
Schizoaffective Disorder prevelance
0.3% prevalence
chronic and responds well to anti-psychotics
schizoaffective disorder and schizophrenia appear to share genetic link