Pleural Diseases
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
24 Terms
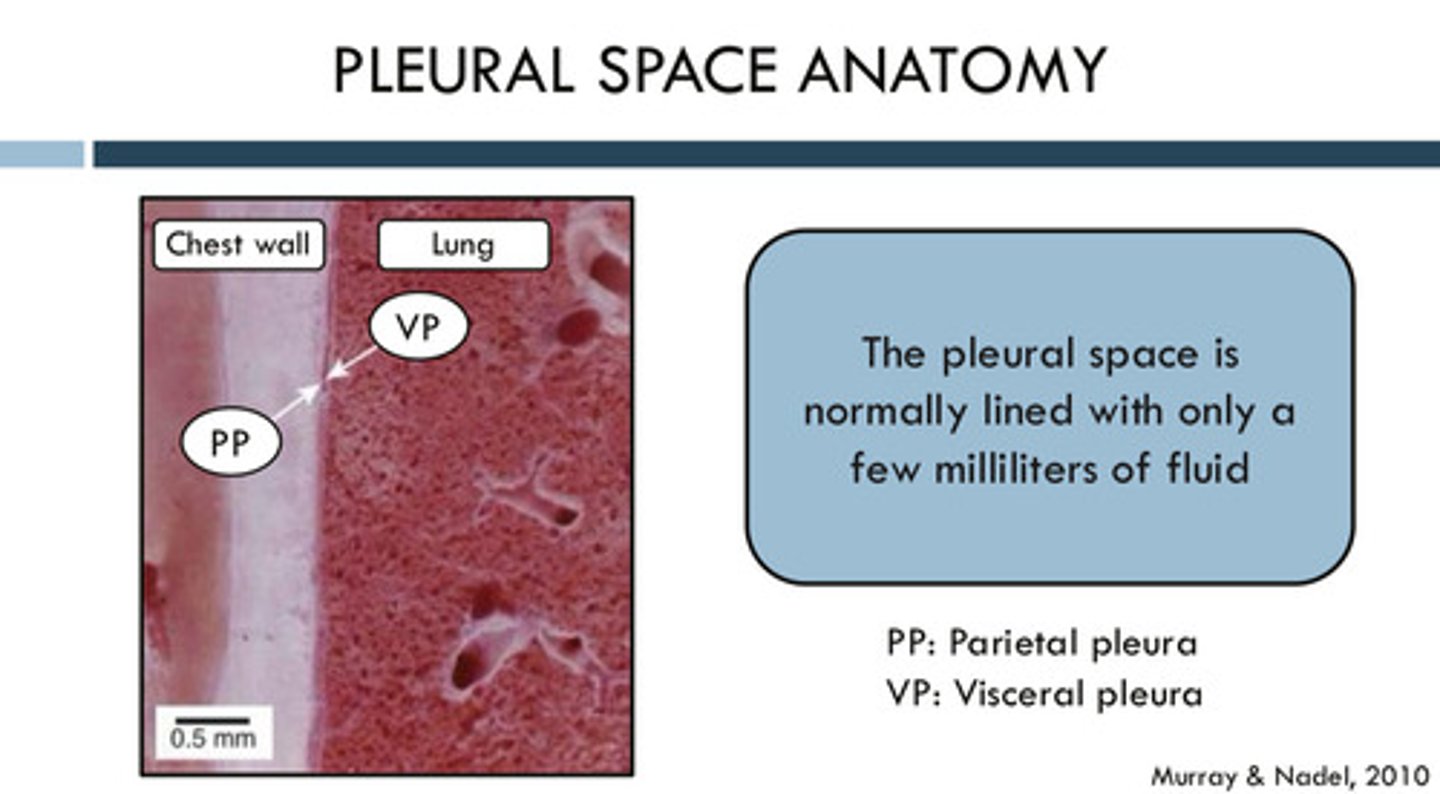
what are the parietal and visceral pleura
parietal pleura: outermost pleura which connects to the inside of the chest wall
visceral pleura: innermost pleura, which connects to the outside of the lungs
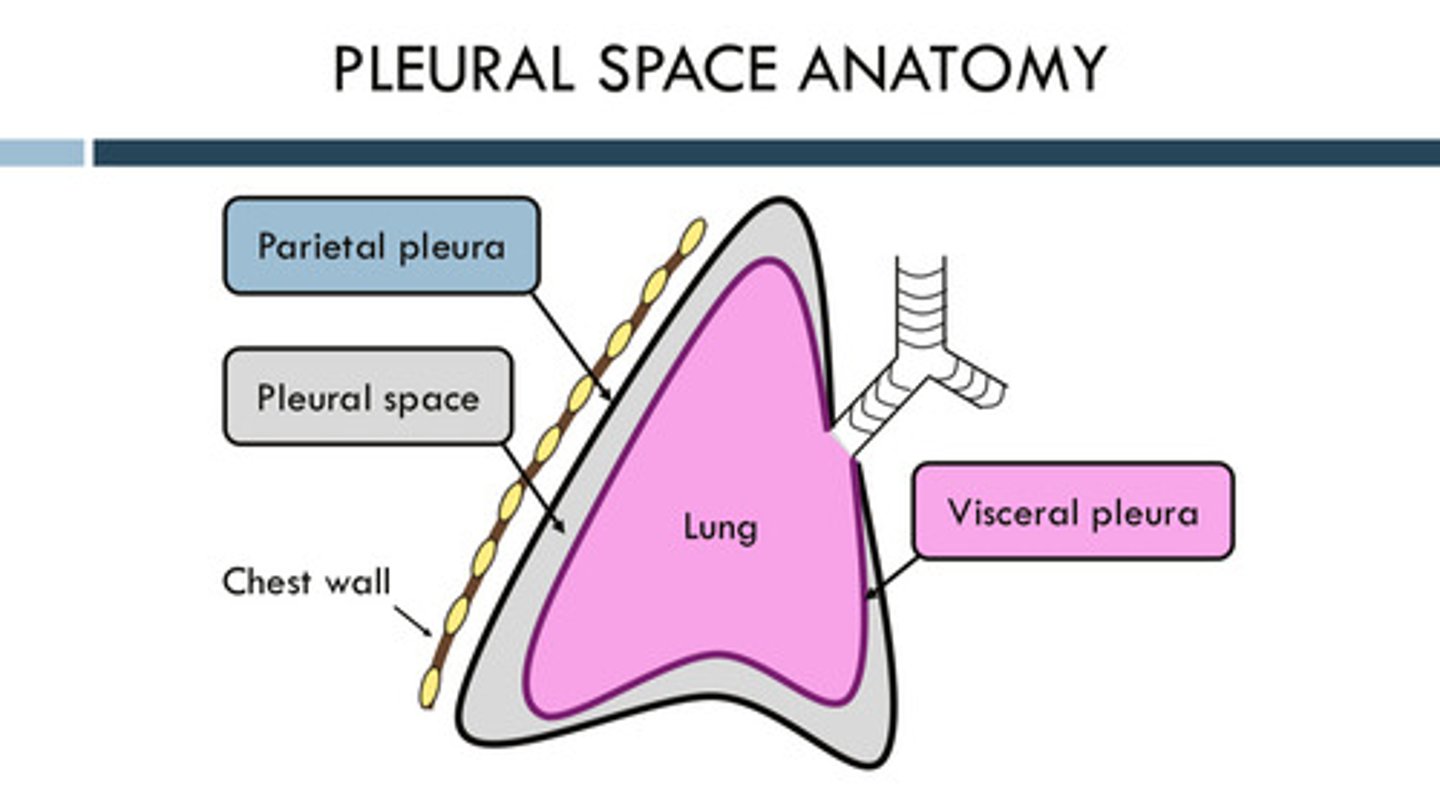
what is the pleural space
the space between the parietal and visceral pleura; this space is inside the chest wall, but outside of the lungs
where does the fluid that accumulates in the pleural space come from?
comes from the blood vessels in the partial pleura (intercostal arteries) and visceral pleura (bronchial arteries); although the fluid comes from both sides, the fluid comes primarily from the parietal pleura
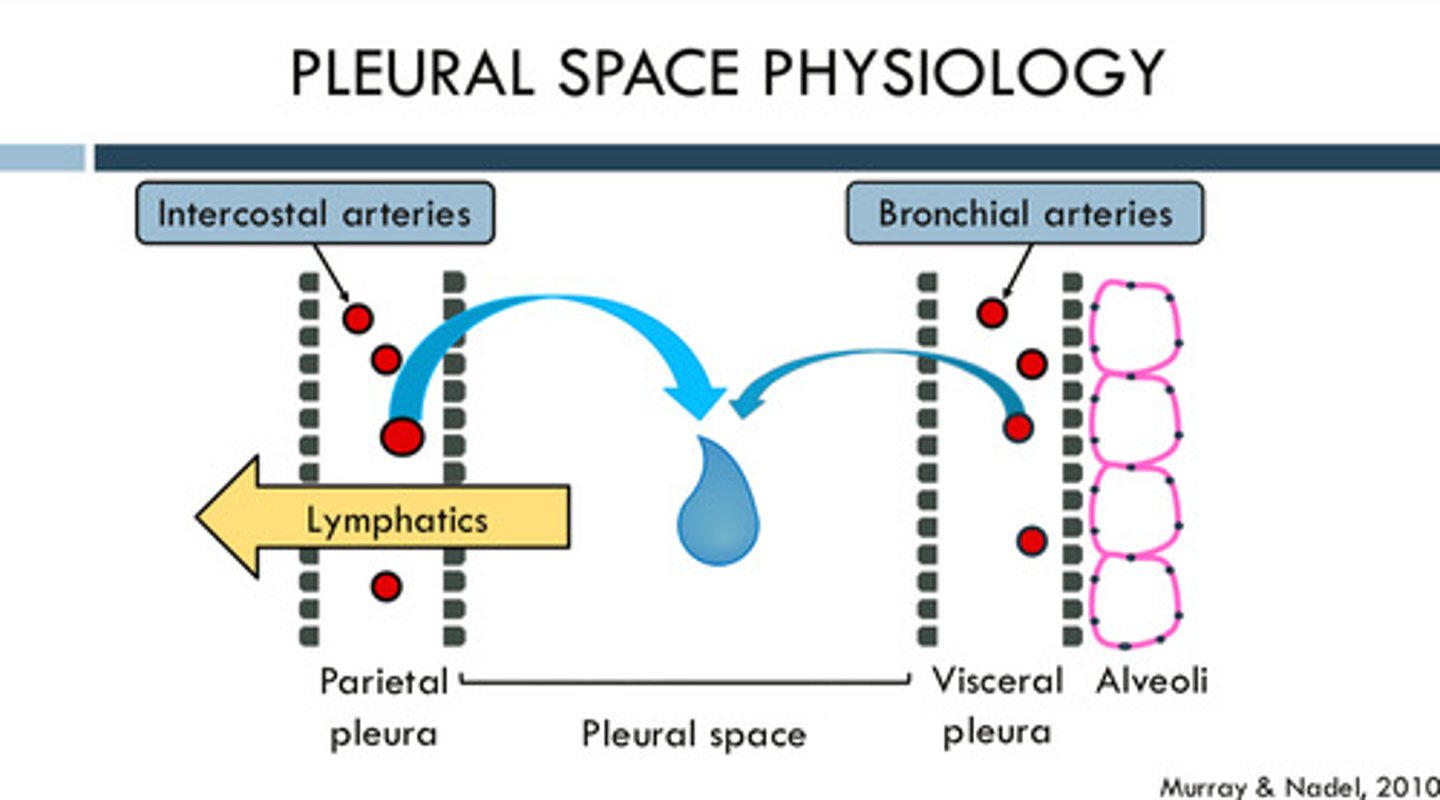
how does the fluid in the pleural space leave?
through lymphatics
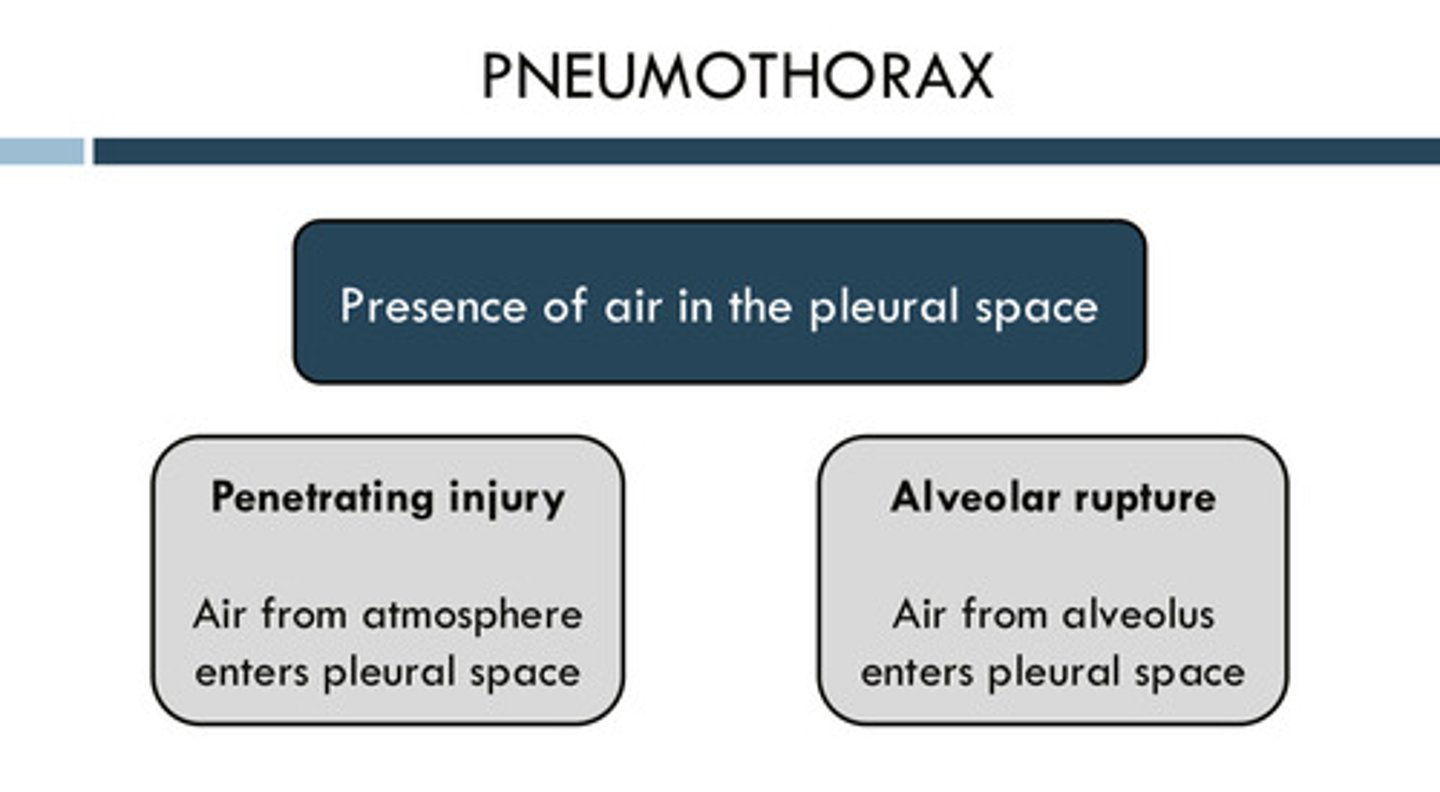
what is pneumothorax? what are some potential causes?
the presence of air in the pleural space
may be from a penetrating injury in which air from the atmosphere enters the pleural space OR may be from an alveolar rupture in which air from the alveolus enters the pleural space
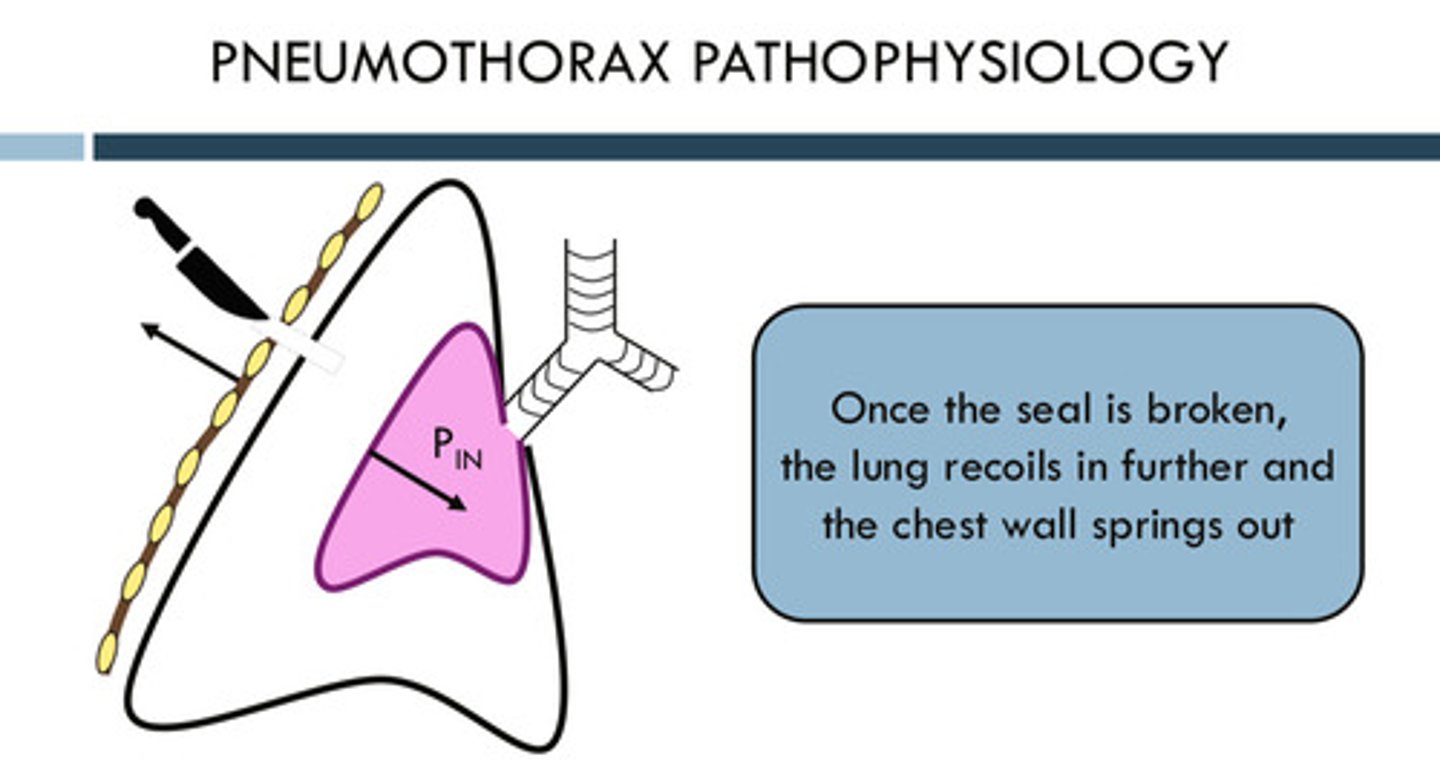
why might you see a collapsed lung in pneumothorax?
once the seal between the lung and the chest wall (the pleural space) is broken due to some reason, the lung recoils IN further (collapses) and the chest wall springs out (the inward recoil of the lung is no longer balanced with the outward recoil of the chest wall)
what are the signs and symptoms of pneumothorax
symptoms: acute onset dyspnea, pleuritic chest pain
signs: hypoxemia, hyperresonance to percussion, diminished breath sounds
what is "pleuritic chest pain"
a sharp, stabbing pain in the chest that worsens with breathing, coughing, or movement; mostly caused by the inflammation of the pleura
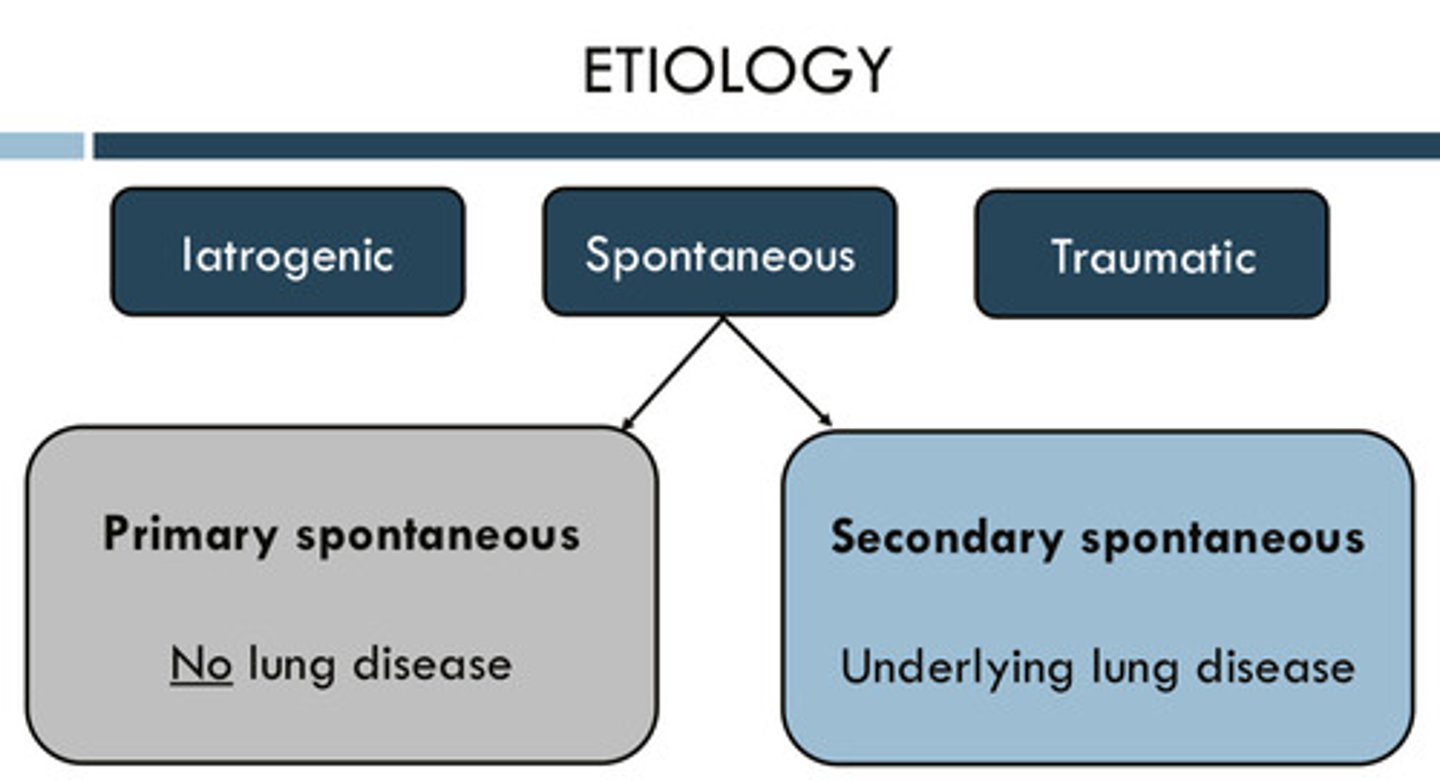
what are some etiologies of pneumothorax?
1) iatrogenic (caused by medical exam or tx)
2) traumatic
3) spontaneous: primary spontaneous —> happens with NO underlying lung disease & secondary spontaneous —> happens with underlying lung disease
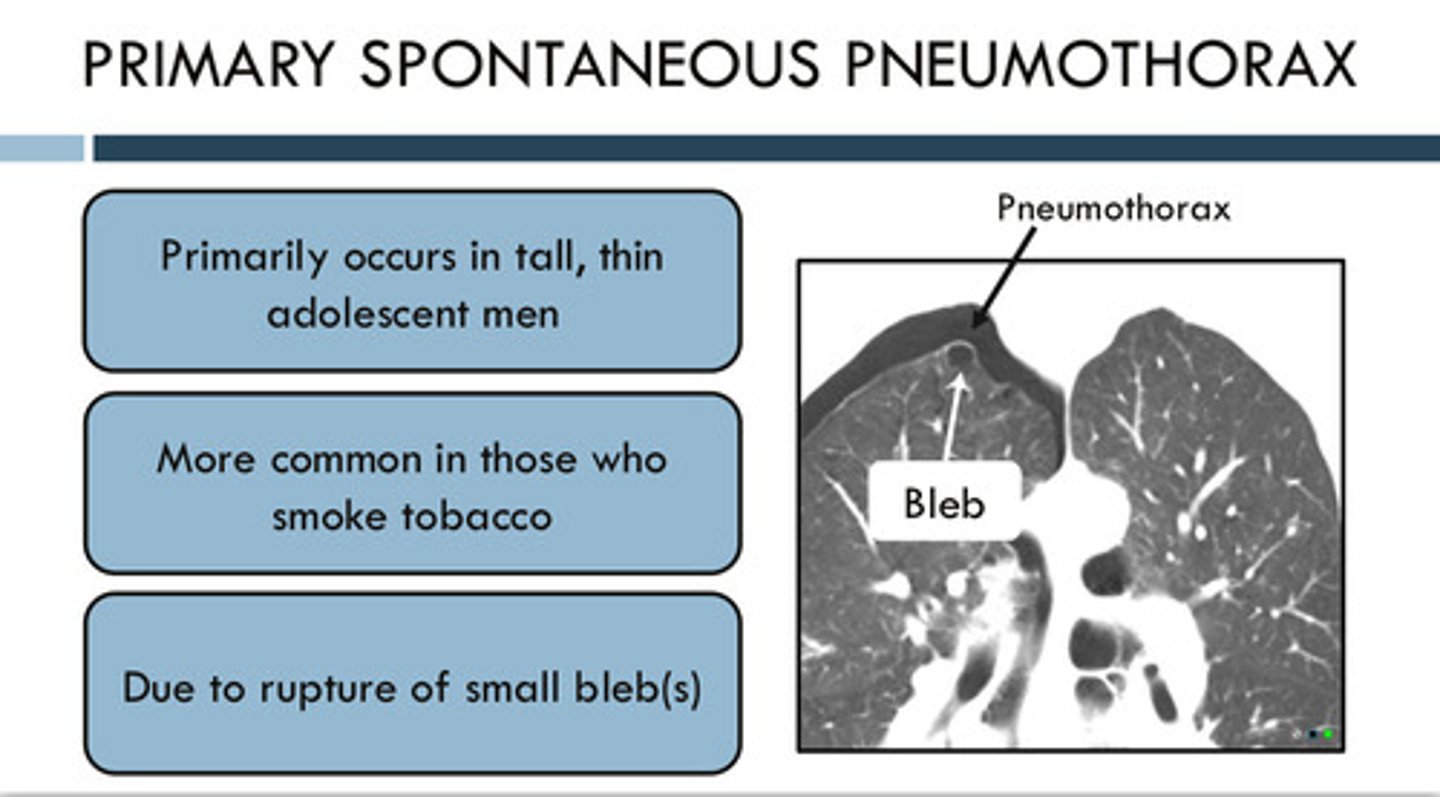
what demographic gets primary spontaneous pneumothorax?
1) primarily occurs in tall, thin adolescent men
2) more common in those who smoke tobacco
3) caused due to the rupture of small bleb(s): no presence of lung disease
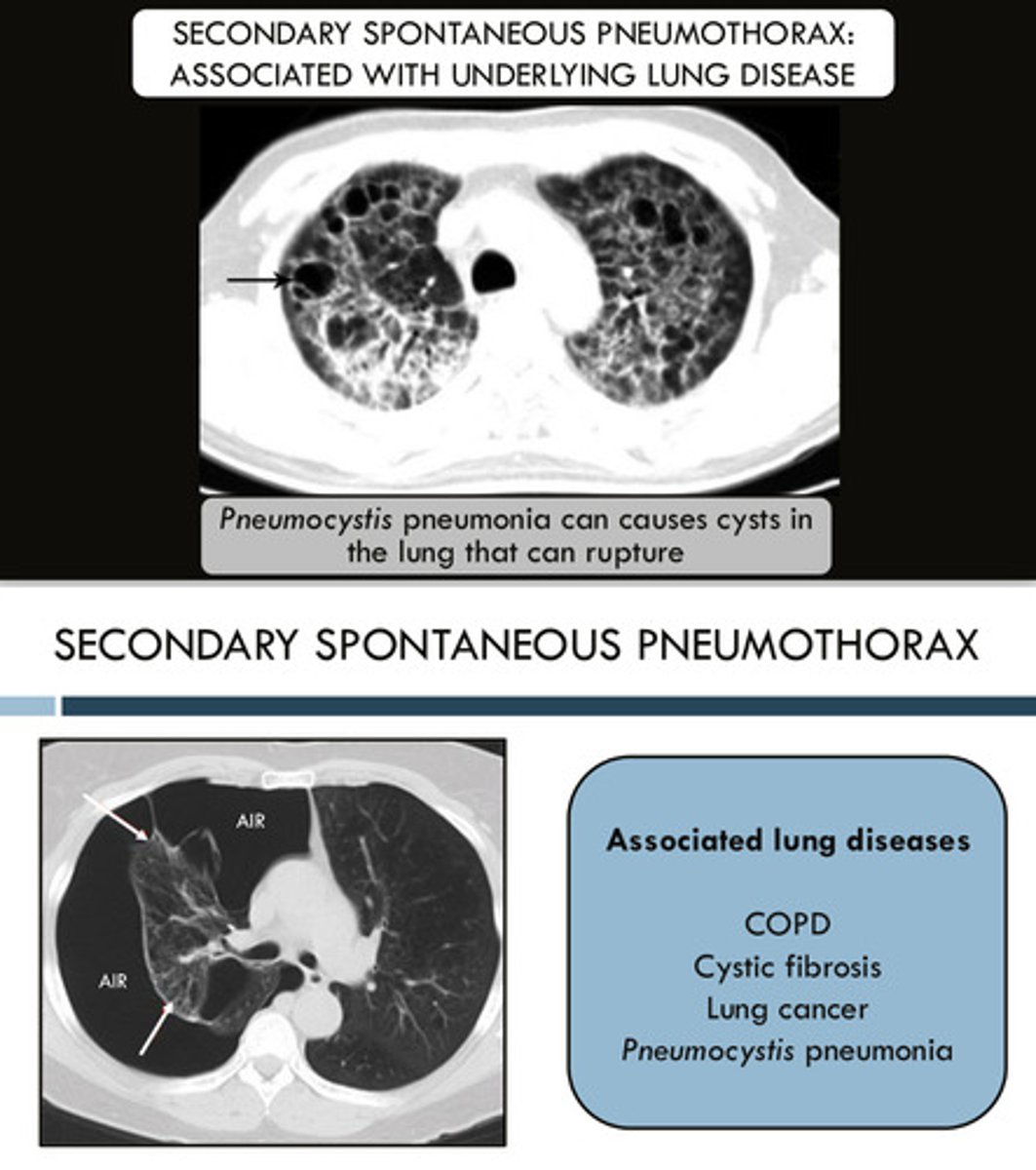
what are some causes of secondary spontaneous pneumothorax?
1) COPD
2) cystic fibrosis
3) lung cancer
4) Pneumocystis pneumonia: this can cause cysts in the lungs that can rupture
what is atelectasis or an atelectatic lung?
a condition where the alveoli in the lungs collapse or fail to inflate properly, leading to a partial or complete collapse of a lung or part of a lung
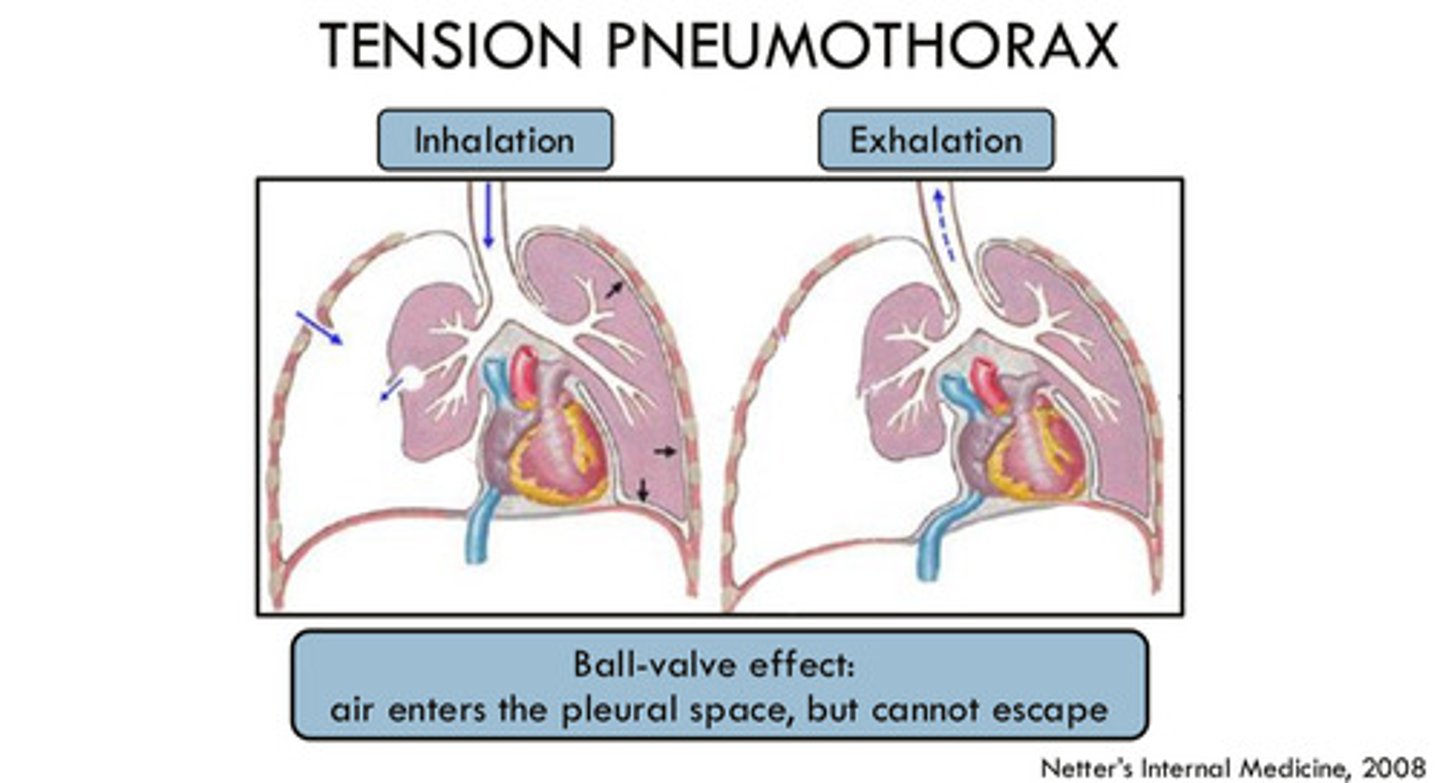
what is a tension pneumothorax?
pneumothorax with rapid accumulation of air in the pleural space (this air cannot escape) that can increase intrathoracic pressure —> results in compression of the lung on the affected side and pressure on the heart and great vessels, pushing them away from the affected side; a medical emergency!!!
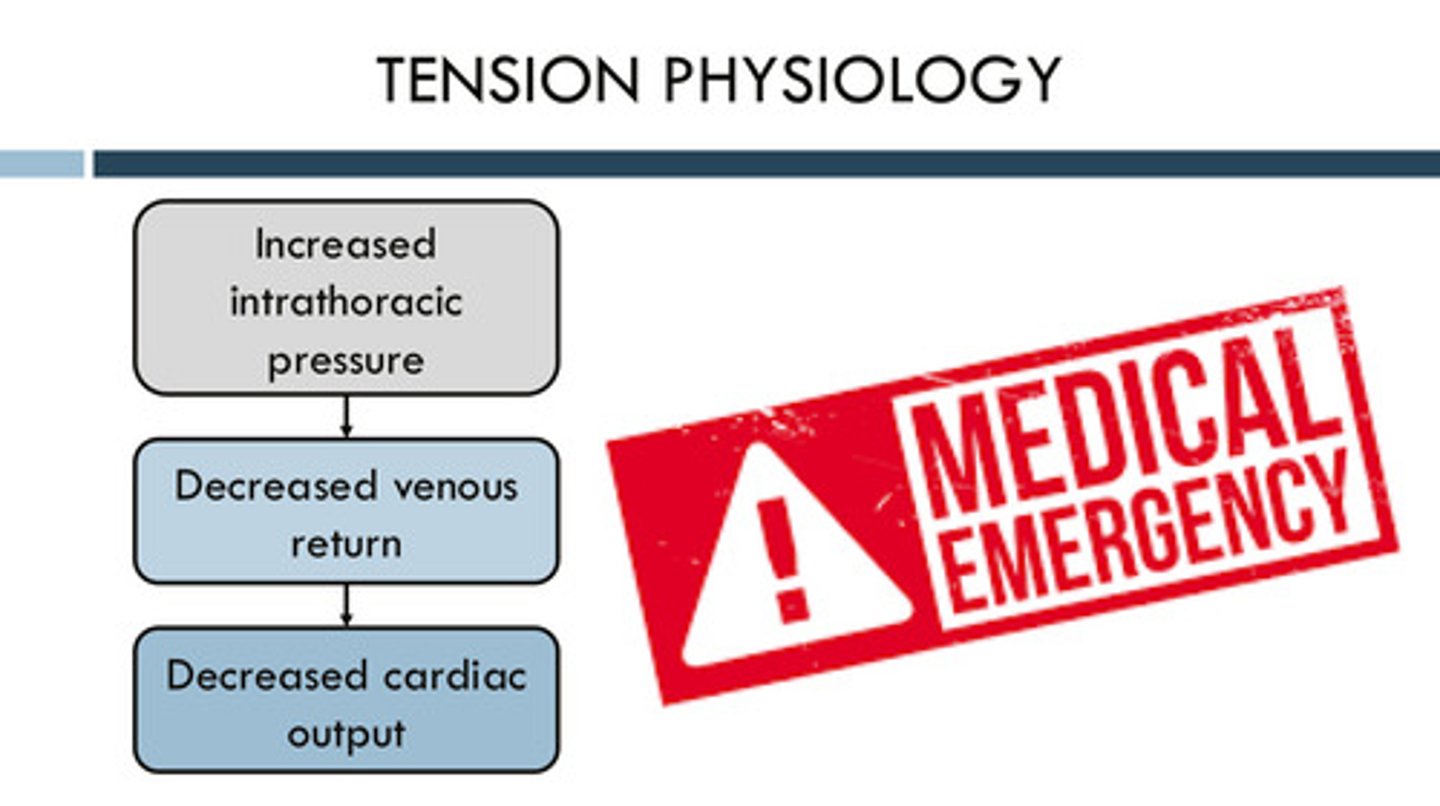
when the pressure is increasing in the thorax due to tension pneumothorax, what happens to the cardiac output?
as the intrathoracic pressure increases —> venous return is decreased —> cardiac output is also decreased
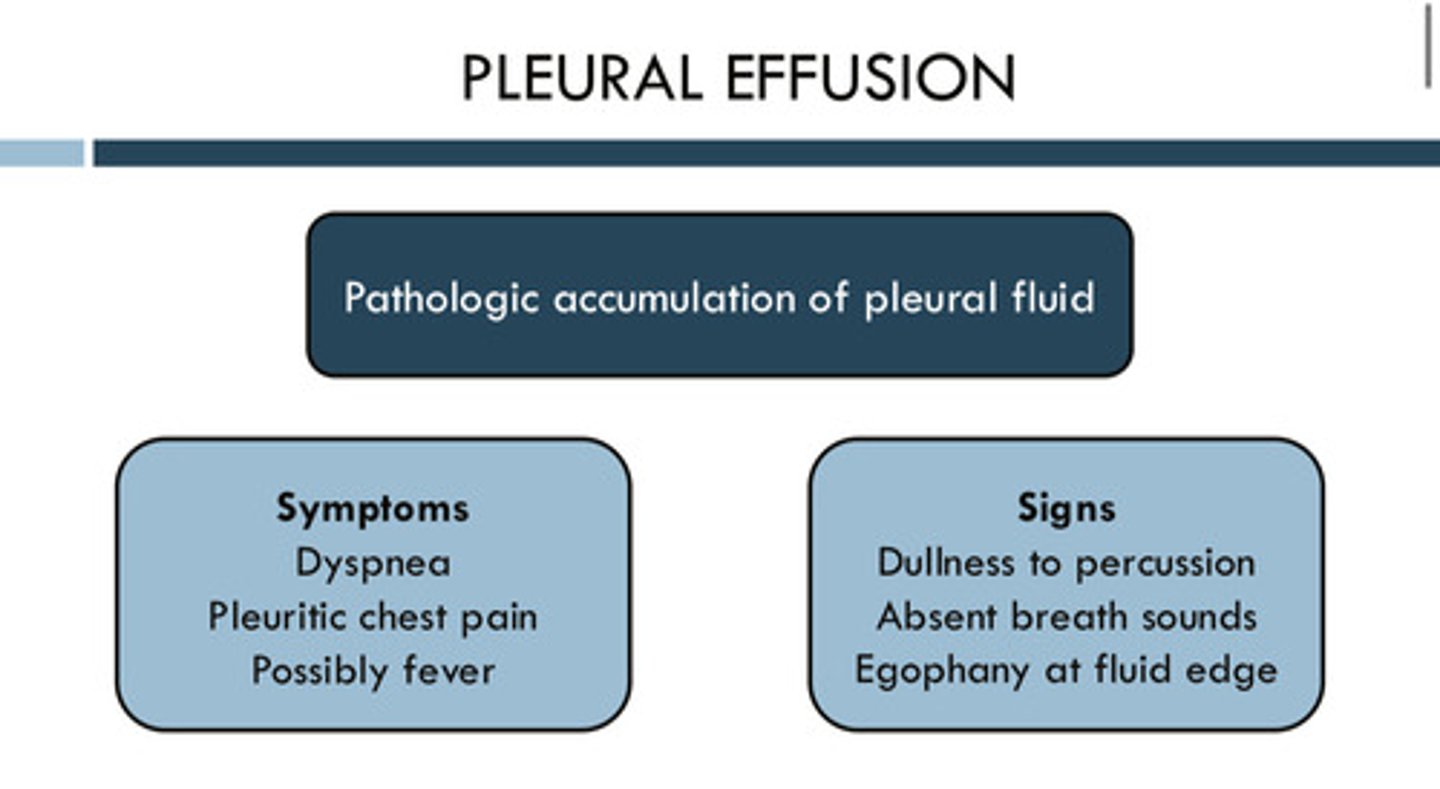
what is pleural effusion
pathologic accumulation of pleural fluid in the pleural space
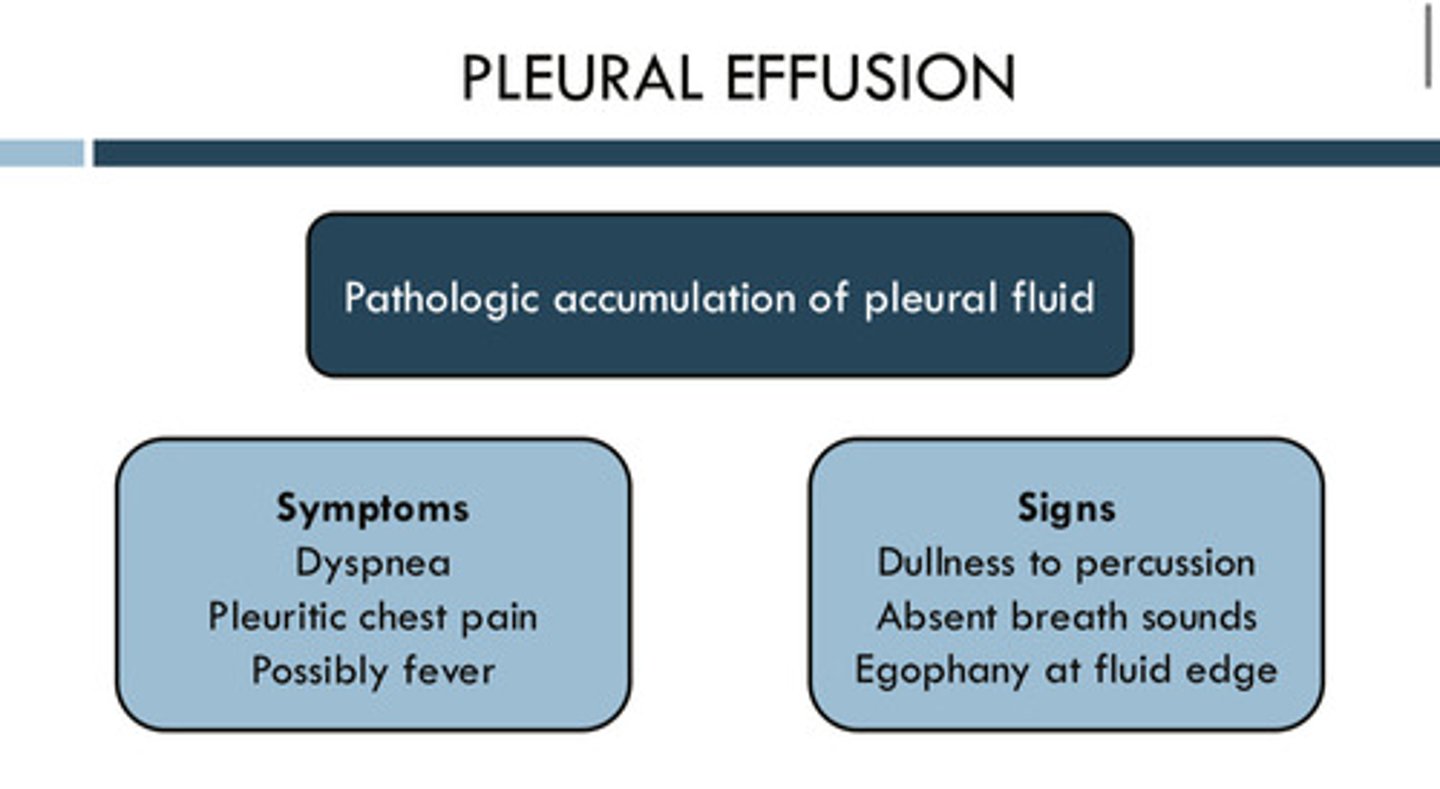
what are the signs and symptoms of pleural effusion
symptoms: dyspnea, pleuritic chest pain, possibly fever
signs: dullness to percussion, absent breath sounds, egophany (abnormal lung sound characterized by a nasal, bleating quality) at fluid edge
what is the name of the procedure to drain or sample the pleural fluid
thoracentesis
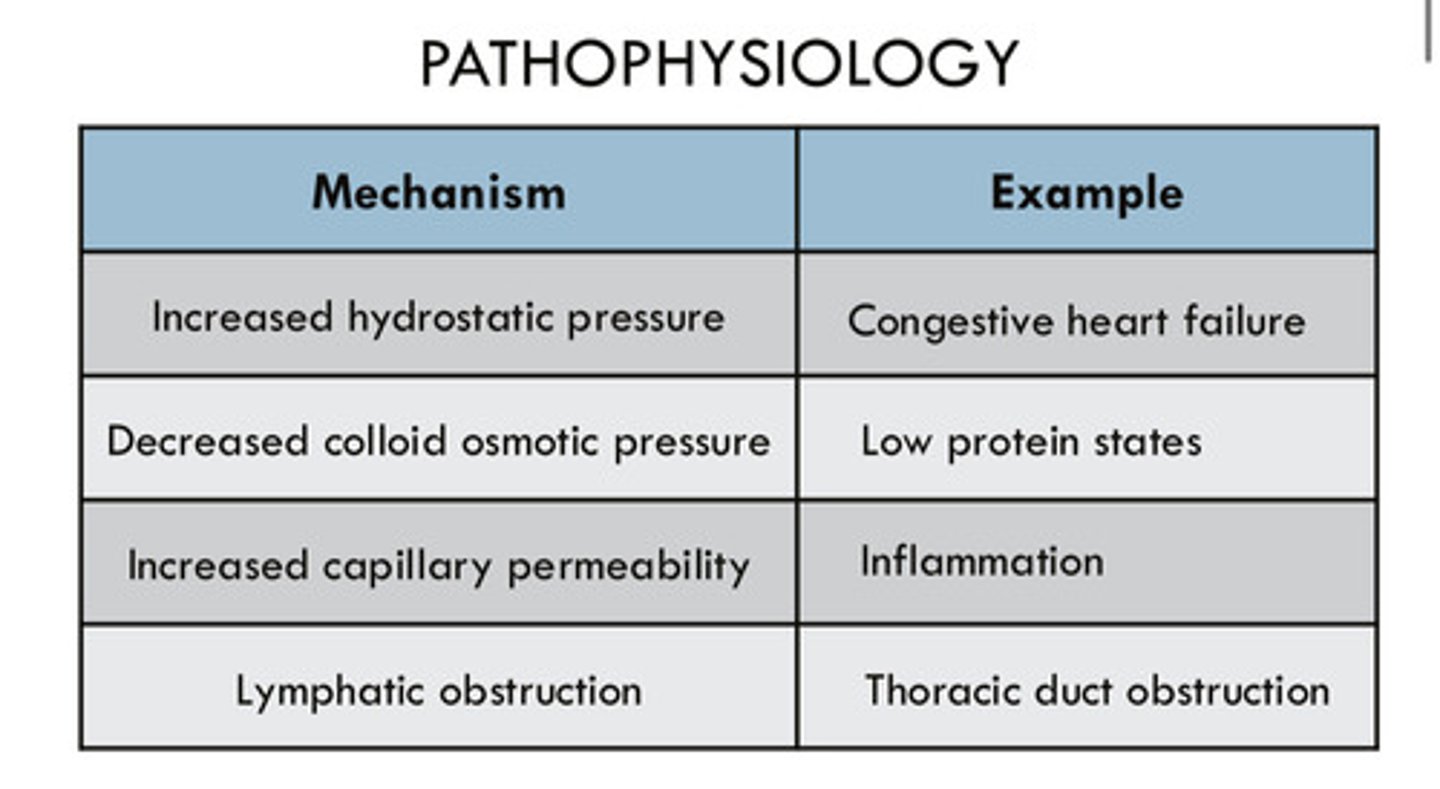
what are the 4 mechanisms of a pleural effusion? (causes of pleural effusion use different combinations of these mechanisms, so knowing these mechanisms help guide the tx or sometimes help figure out the cause)
1) increased hydrostatic pressure (ex: congestive heart failure)
2) decreased colloid osmotic pressure (ex: low protein states)
3) increased capillary permeability (ex: inflammation)
4) lymphatic obstruction (ex: thoracic duct obstruction)
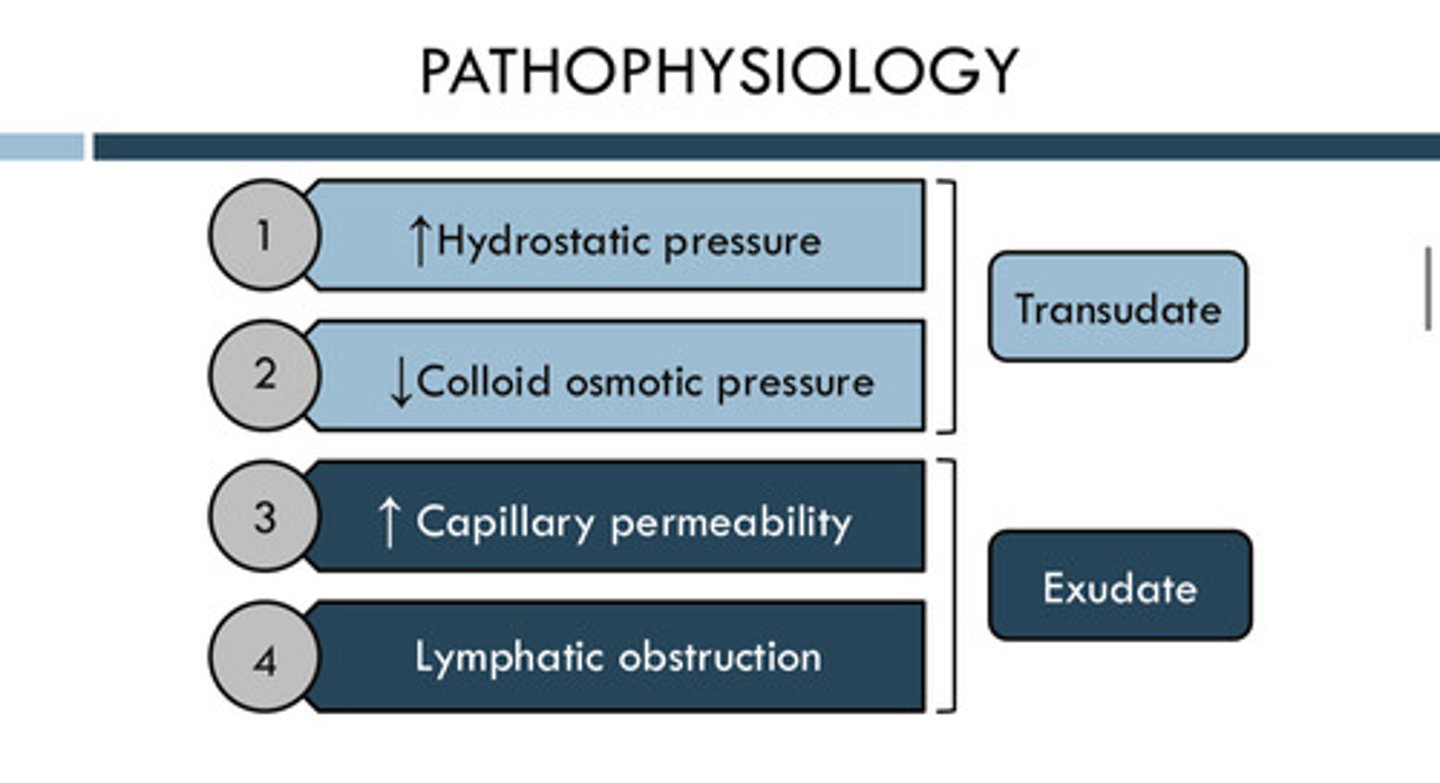
describe fluid that is a transudate
a fluid that results from increased hydrostatic pressure and/or decreased colloid osmotic pressure; in other words: a very bland, simple fluid without a lot of other content such as proteins/cells
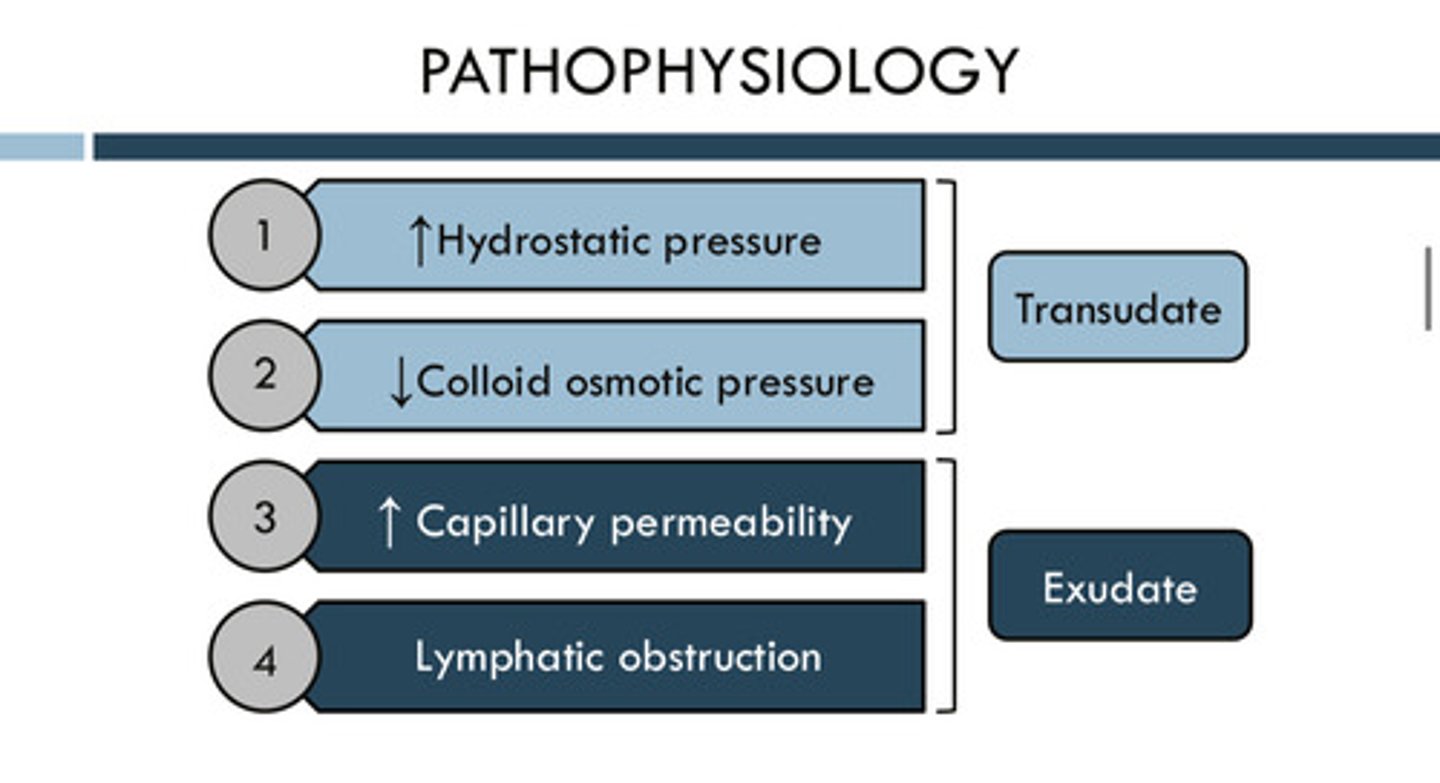
describe fluid that is an exudate
a fluid that results from increased capillary permeability and lymphatic obstruction; a fluid that has a lot of protein and cells in it
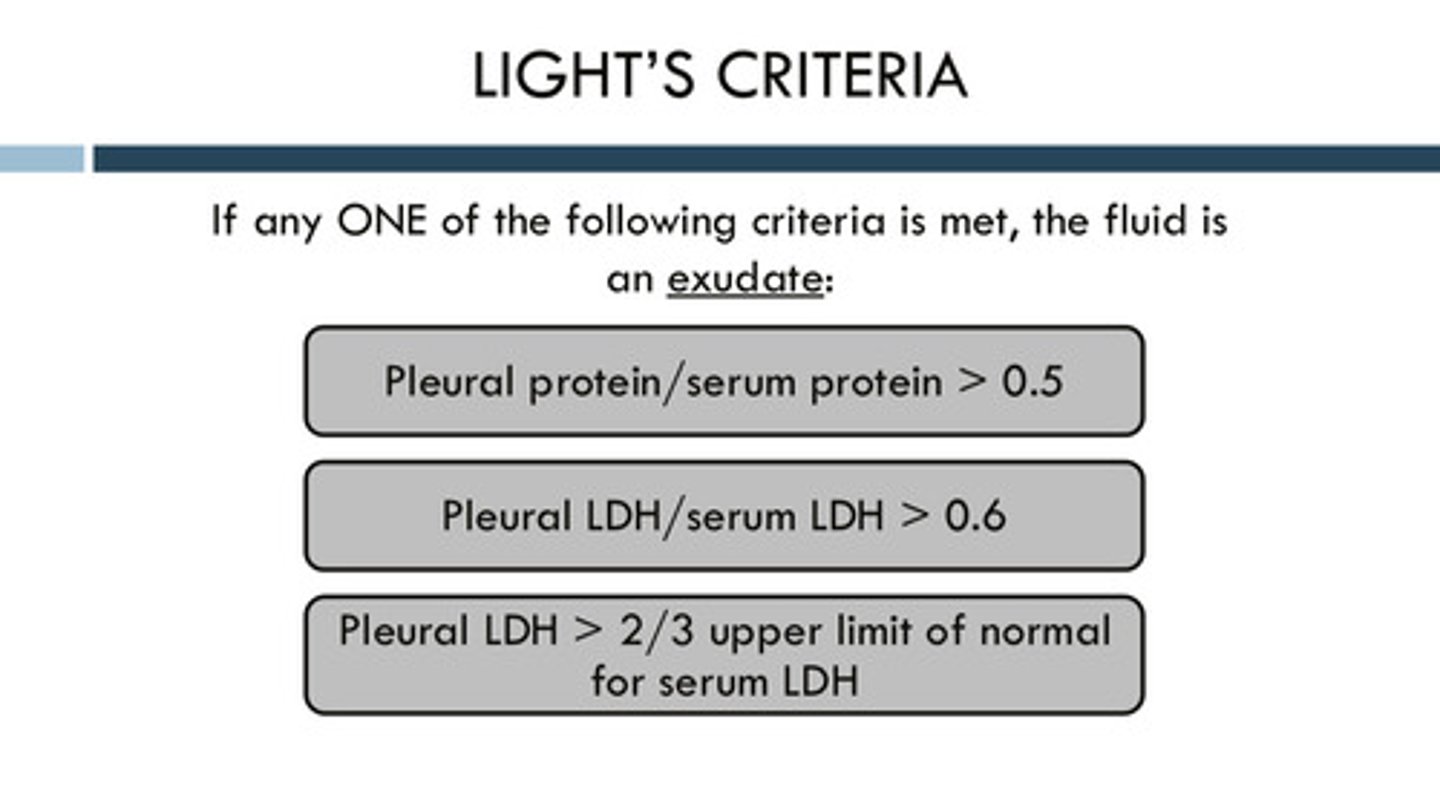
what are the criteria used to determine whether the fluid is a transudate or an exudate?
light's criteria: you do not need to memorize the criteria, but know that the difference between the two is mostly due to presence of proteins/cells/content
LDH means lactate dehydrogenase
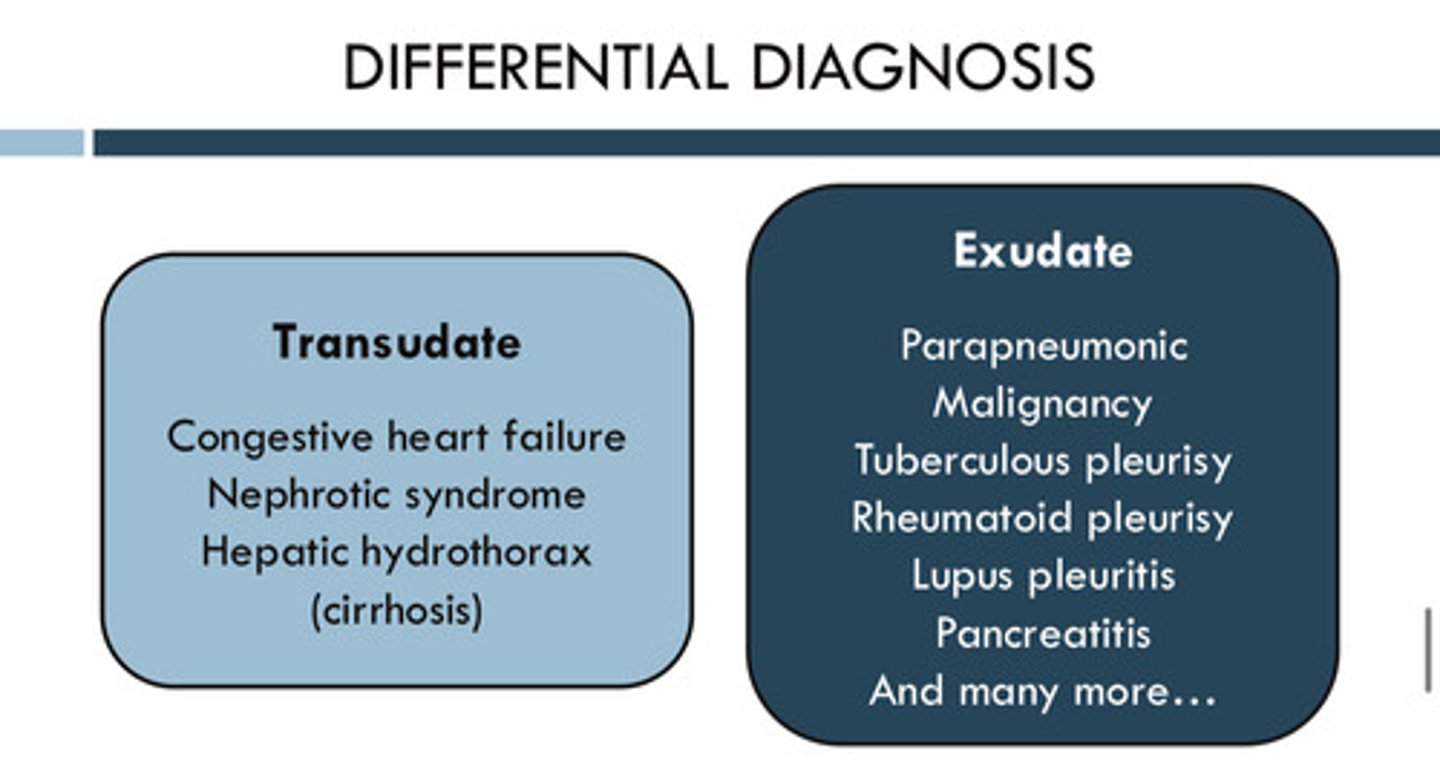
what are the causes of a transudate pleural effusion?
1) congestive heart failure
2) nephrotic syndrome (leaking albumin out through the kidneys)
3) hepatic hydrothorax (cirrhosis)
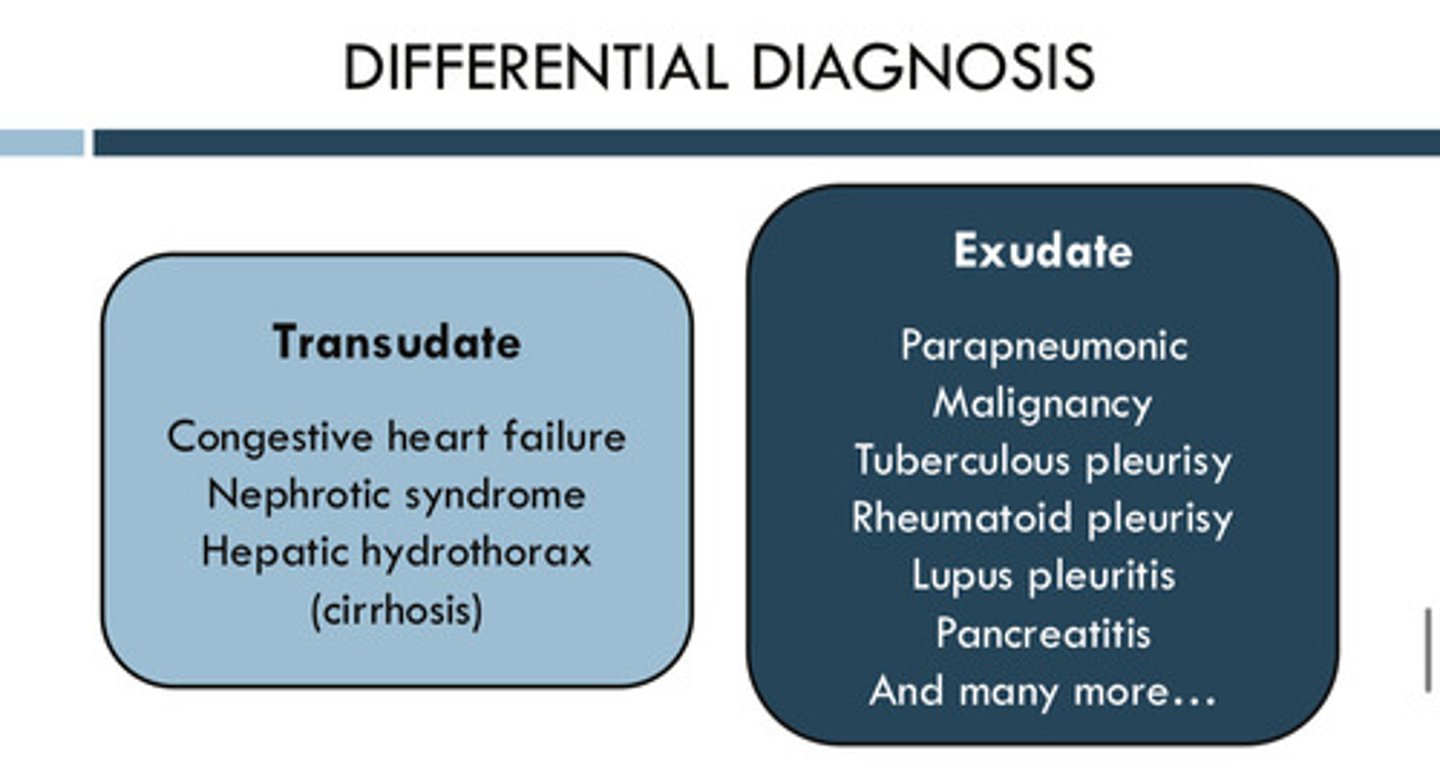
if a pleural effusion is exudative, you should know that it is not caused by the 3 diseases that cause a transudate pleural effusion, but instead by something else. what are some causes of an exudate pleural effusion?
1) parapneumonic
2) malignancy
3) tuberculous pleurisy
4) lupus pleuritis
5) pancreatitis
so many more!
key points