Anatomy Lesson 4 - Cartilage and Bone Tissue
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
describe the composition, function and distribution of fibrocartilage
composition: thickest out of all three cartilage; contains thick collagen fibers hence little ground substance; parallel collagen fibers; no perichondrium(dense irregular connective tissue layer that surrounds cartilage)
function: shock absorber (not elastic nor flexible so it’s a shock absorber)
location: intervertebral discs, pubic symphysis, menisci of knee, articular discs of jaw
describe the function and distribution of hyaline cartilage
most prevalent in our body
function: supports soft tissue; flexible but resilient
location: respiratory system (larynx, trachea, bronchi), costal cartialge, nose, articular cartilage, epiphyseal plate, fetal skeleton(most of fetus is cartilage not bone)
(**to remember which are hyaline cartilage, memorize fibrocartilage and elastic cartilage and the rest of the cartilage are hyaline cartilage)
describe the composition, function and distribution of elastic cartilage
composition: small amount of ECM; elastic fibers form weblike mesh around lacunae which…(continue to functions)
function: thinnest cartilage allows elasticity and flexibility
location: epiglottis (covers respiratory tract when we swallow food/water), external ear
(**to memorize, realize that Elastic, Epiglottis, and Ear all starts with the letter E)
which connective tissue is cartilage a part of?
supportive connective tissue
list the cartilages from thickest to thinnest
fibrocartilage > hyaline cartilage > elastic cartilage
What are the components of (general) cartilage? Define them
chondroblasts: cells that produce cartilage matrix
lacunae: “cave“ where chondrocytes live
chrondrocytes: mature cartilage cells that reside in lacunae
ECM: protein fibers and ground substance
perichondrium: dense irregular connective tissue
what are the functions of cartilage
support soft tissues
provide articular/gliding surface for joints
provide a model for endochondrial
bone formation (cartilage serves as a rough draft for bone tissue)
what are the characteristics of cartilage
semirigid, weaker than bone
flexible & resilient due to elastic fibers and water content
avascular, therefore receives nutrients via diffusion
what are the functions of bone
support & protect: creates framework of body and protects vital organs from injury
movement: bone serves as attachment sites for muscles
hemopoiesis or hematopoiesis (same thing): makes RBCs from red bone marrow
storage of minerals and energy reserves: calcium phosphate and yellow bone marrow(as humans mature, red bone marrow degenerates to become yellow BM and w/in the yellow BM of shaft and long bones is potential energy stored as lipids)
identify the characteristics of long bone and classify them
long bones are longer than wide, they include…
humerus
radius and ulna
metacarpals and metatarsals
phalanges (hands and feet)
femur
tibia and fibula
classify short bones
carpels, tarsals, sesamoid bone on the patella (knee bone)
classify flat bones
skull, scapulae, sternum and ribs(*ribs are tricky bc one might think they’re long bones but in reality they are curved but flat)
classify irregular bones
vertebrae, sacrum, coccyx, os coxa, thmoid and sphenoid
what is another name(s) for compact bone
cortical bone
what is another name(s) for spongy bone
cancellous or trabecular
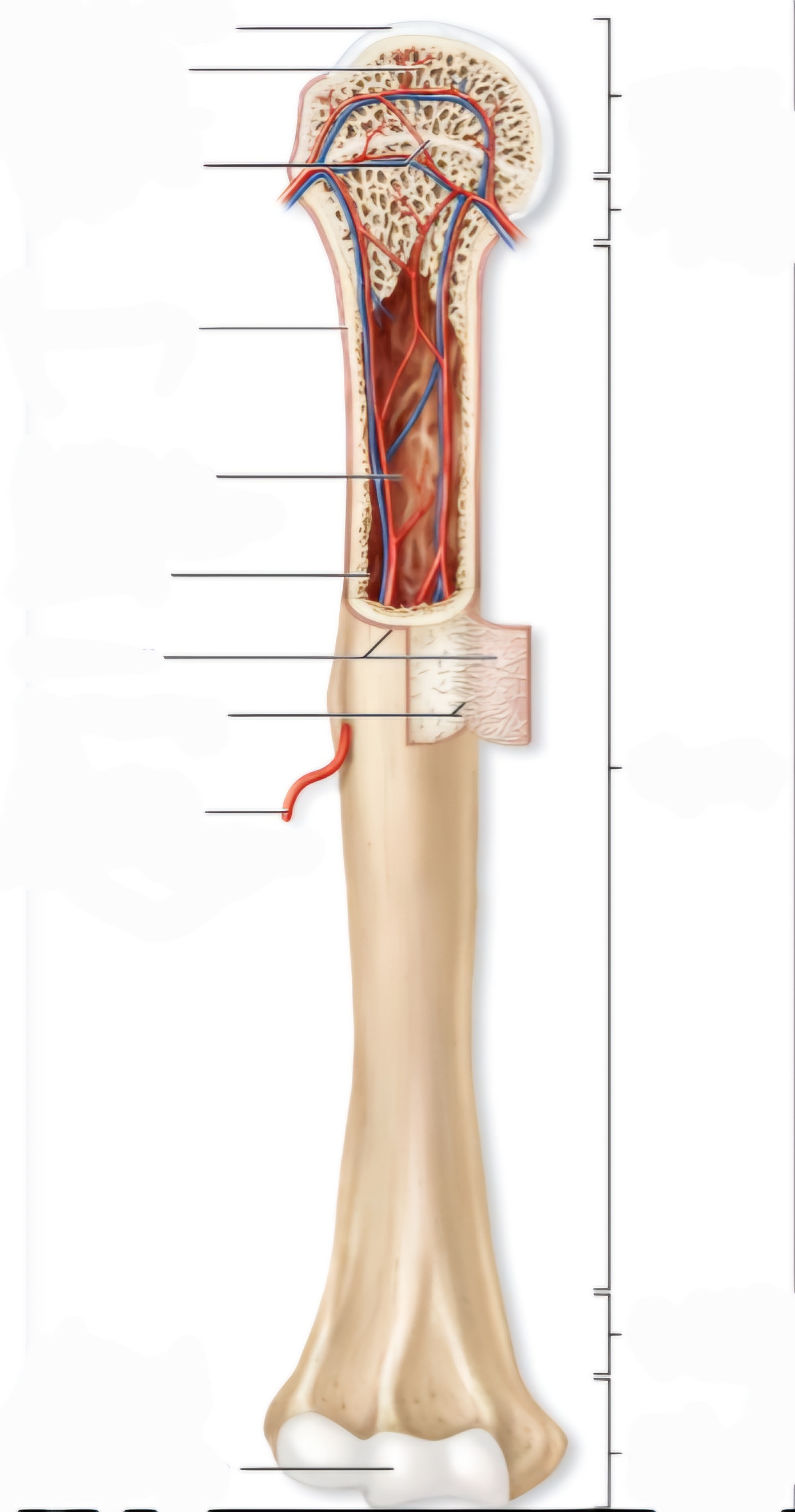
label the structures of long bone
define: medullary cavity, endosteum, periosteum, perforating fibers
epiphyseal plate/line is found within the metaphysis
epiphyseal plate is made of cartilage in children, it’s a growth plate
epiphyseal line is in adults, and it is NOT made of cartilage
medullary cavity: inside of bone (cortex is on the outside of the bone)
contains yellow bone marrow in adults and red in children
endosteum: membrane(not bone); layer of cells lining the spongy bone and medullary cavity
periosteum: membrane(not bone); dense regular CT, outer covering of diaphysis of long bone; lines the compact bone on the outside
provides stem cells for bone growth and fracture repair
perforating fibers: what holds the periosteum to the bone
list in order of superficial to deep the layers of bone
(superficial) periosteum, compact bone, spongy bone, endosteum (deep)
differentiate between osteoprogenitor cells, osteoblasts, osteocytes, and osteoclasts in terms of function and location
osteoprogenitor cells: stem cells of bone
osteoblasts: ones that build bone by secreting osteoid(bone matrix)
osteocytes: mature bone cells that maintain bone matrix; osteocytes are encased in matrix called lacunae
osteoclasts: consumes bone (bone resorption)
describe the lifecycle of an osteoprogenitor cell
either mesenchyme or osteoprogenitor cell becomes osteoblast which then becomes osteocyte
what is bone matrix (aka bone extracellar matrix) made of? Which component is organic and which is inorganic?
made up of osteoid (collagen), which is secreted by osteoblasts, and calcium phosphate
Osteoid is organic and calcium phosphate is inorganic so we need it from our diet
[**way to remember] Osteoid is Organic (both starts with “O”s)
describe the structure of a typical flat bone
(think of it like a sandwhich) Periosteum > compact bone > spongy bone > compact bone > periosteum
compact bone and spongy bone are both lined with periosteum
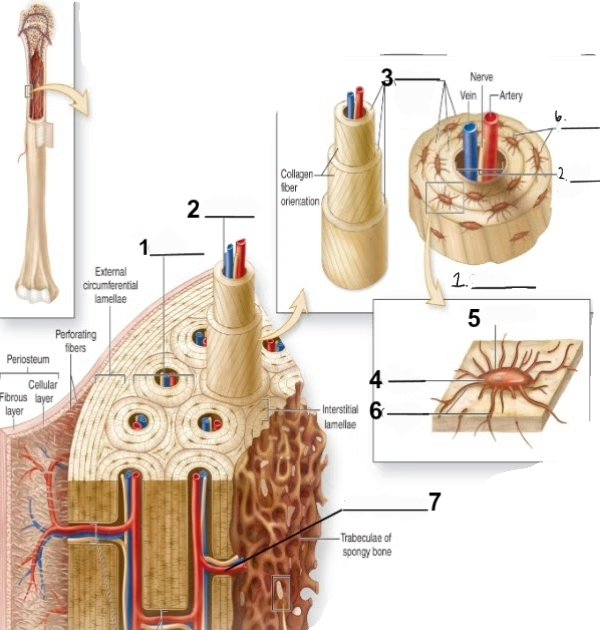
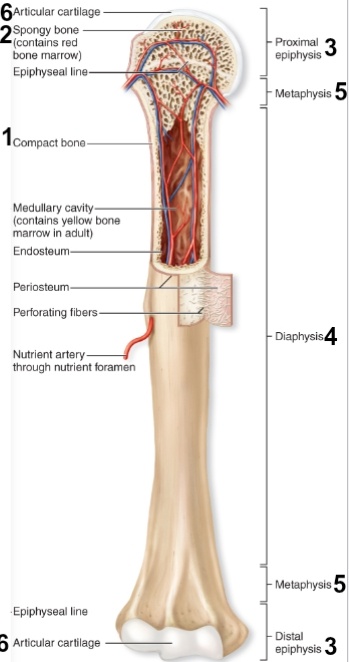
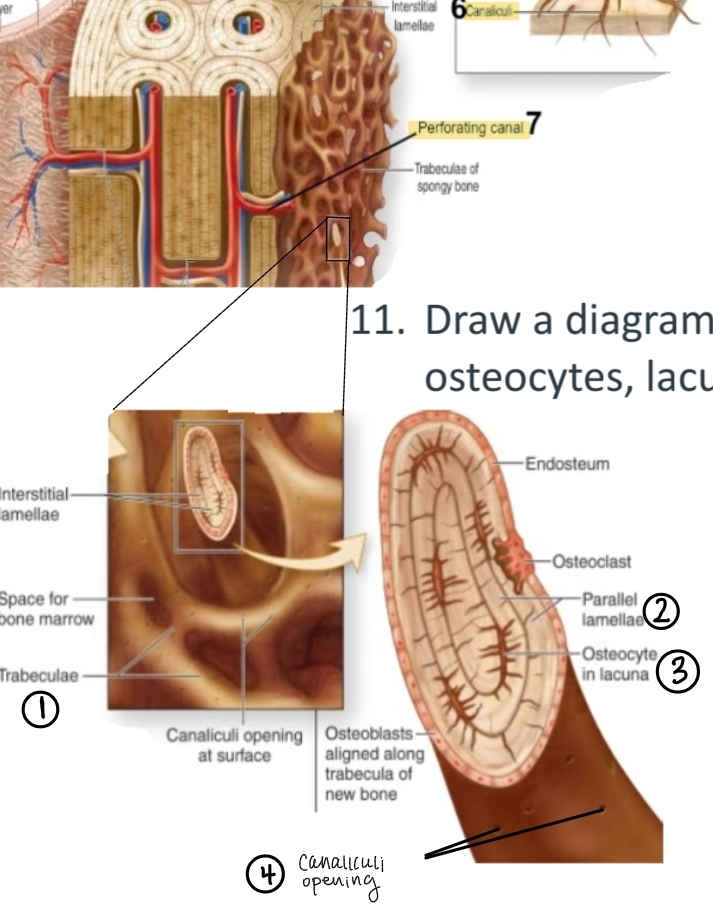
label the cross section of a compact bone
What is an osteon of compact bone and what’s its alternative name
aka Haversion system; basic functional/structural unit of mature compact bone
what is a central canal of compact bone and what is the alternative name
aka Haversian canal; cylindrical channel that lies in the center of osteon; blood vessels and nerves run w/in the canal and supplies the bone
what is a concentric lamellae of compact bone
rings of bone connective tissue that surround central canal and form the bulk of osteon
where is osteocyte located in a compact bone
housed in lacunae and occur b/t adjacent concentric lamellae
what is a canaliculi
tiny channels/passageway b/t central canal and osteocytes allowing minerals, nutrients, gases and wastes to travel to supply nutrients to osteocytes
what is a perforating canal and what is its alternative name
aka volkmann’s canal; runs perpendicular to central canals and help connect multiple central canals creating a vascular innervation connection among the multiple osteons; contains blood vessels and nerves
[**way to remember: you take a volkswagon bug across perforating caval b/t central canals]
how is a spongy bone different from a compact bone
it has tribeculae (crisscrossing bars and plates between compact bone that provide resistance to stress coming from all directions and distributes stress throughout framework)
it has parallel lamellae, osteocytes, and canaliculi but NO osteon or perforating canal bc there are no central canals like there is in compact bone
summarize the process of intramembranous ossification and the bones formed from it
aka dermal ossification; growth within a membrane that forms bones from clavicle and up
Process: mesenchymal cells become osteoblasts, which then secretes osteoid which then goes thru calcification when it comes in contact with calcium phostphates and forms a calcified matrix which traps some osteoids which then becomes osteocytes
(**specifics of the process is not really important to know for this course but know general process)
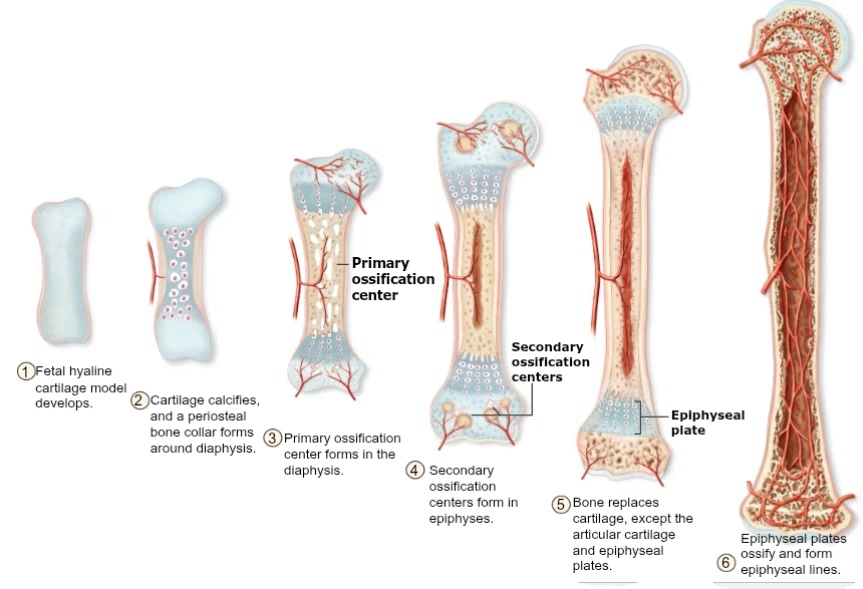
summarize the process of endochondral ossification and the bones formed from it
bone growth within a cartilage; turns fetal framework of hyaline cartilage into bone, formation of most bones but specifically bones from clavicle down (NOT including the clavicle)
Process:
Fetal hyaline cartilage model develops
cartilage calcifies and periosteal bone collar forms around diaphysis
primary ossification center forms in the diaphysis
secondary ossification centers form in epiphyses
bone replaces cartilage, except the articular cartilage and epiphyseal plate
epiphyseal plate ossifies and becomes epiphyseal line
(**specifics of the process is not really important to know for this course but know general process)
how does bone grow in length, what is it called?
interstitial growth:
occurs at the epiphyseal plate
Process: chondrocytes at the epiphyseal plate go thru cell division
this division pushes the zone of resting cartilage toward the epiphysis (flexible matrix of hyaline cartilage permits this growth)
this hyaline cartilage is later replaced w/ bone (endochondral ossification)
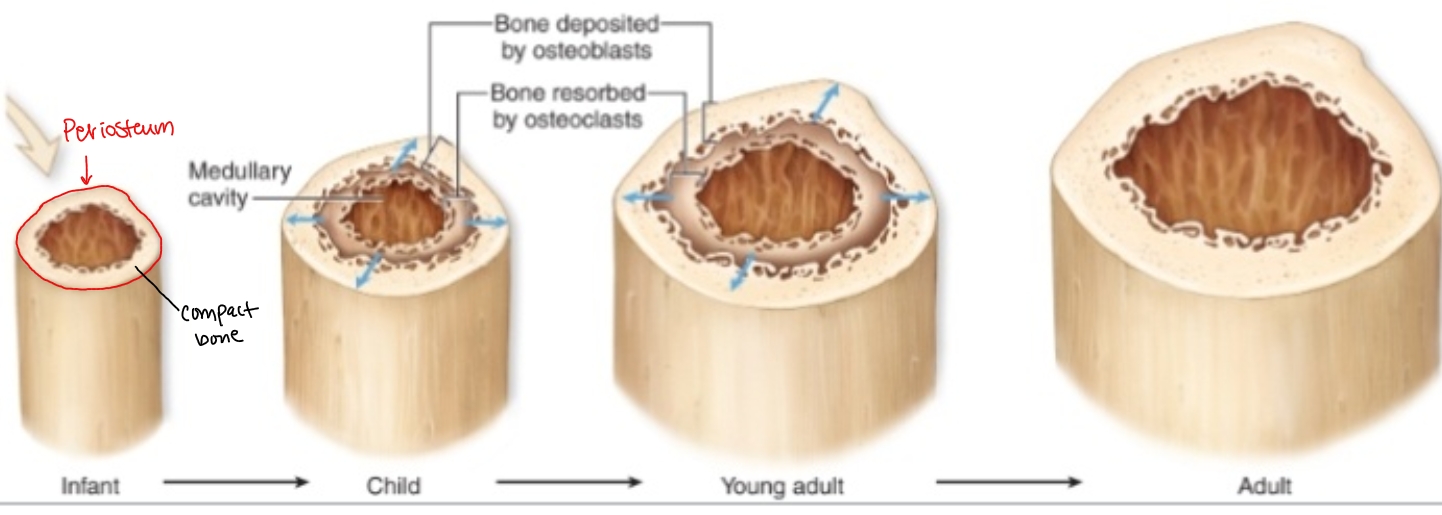
how does bone grow in thickness (width), what is it called?
appositional growth: occurs at the periosteum and endosteum
Process: osteoclasts in the inner cellular layer of the periosteum lay down bone matrix in layers
as the number of these layers increase, the structure widens. as new bone is being laid down, osteoclasts along the medullary (inside) cavity resorbs bone matrix, making an expanded, wider hollow medullary cavity
what are the four different types of bone fractures? Define them
simple fractures: bone doesn’t pierce skin
open/compound fracture: bone pierces skin
stress fracture: think break from repetitive loads
pathologic fracture: disease weakens bones (such as osteoporosis)
explain how bone fractures are repaired
fracture hematoma forms where blood pools in the area where the bone fracture teared the blood vessels
fibrocartilage (soft) callus forms and produce collagen fibers that help connect broken ends of bones
hard (bony) callus forms: osteoprogenitor cells next to soft callus becomes osteoblasts and make trabeculae of primary bone. Soft callus is replaced by bone which forms hard callus
bone is remodeled: osteoclasts remove excess bony material and primary bone is replaced with compact bone
*periosteum provides stem cells for bone growth and fracture repair
Bone Disorder: osteomalacia
called rickets in children > soft bones which leads to bowed legs
Possible causes: vit D deficiency, calcium deficiency
Bone Disorder: osteoporosis
excessive bone resorption due to aging and post-menopause
Bone Disorder: osteitis deformans
aka Paget’s disease
excessive osteoclast and osteoblast function
bone is unstable and immature, so it’s more susceptible to fractures and deformation
most common in os coxa, skull, vertebrae, femur and tibia
ossification begins in the embryo (T/F)
TRUE
vitamin A activates
osteoblasts
vitamin C is required for
normal synthesis of collagen
vit D stimulates
absorption and transport of calcium and phosphate ions into blood > basically strengthens bone