Microbio Quiz #3: Chapters 13.4, 2, and 18
1/142
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
143 Terms
Antibiotics
Chemical compounds synthesized by one microbe to selectively kill other microbes and help eliminate pathogens (antibiotics kill pathogens not the host)
Chemotherapeutic agents
A generic term for natural and synthesized antibiotics
Selective toxicity
Paul Ehrlich's production that any successful antimicrobial compound would have to be a “magic bullet” that selectively kills or inhibits the pathogen but not the host
Selectively toxic to bacteria (Magic bullet concept)
Antibiotics are _______ without toxicity to eukaryotic organisms
Cidal agents (EX: bactericidal agents kill bacteria)
Lethal effects!!! An antibiotic is a ____ if kills the target microbe (fungicides, virucides, algicides)
Static agents (EX: bacteriostatic agents inhibit/prevent bacterial growth)
Slow or stop metabolism or reproduction, but are not necessarily lethal (fungistatic, virustatic, algistatic)
Minimum Inhibitory Concentration or MIC (how little is needed to stop growth)
The lowest concentration of the drug that will prevent the growth of an organisms (in vitro tests for antibiotic effectiveness)
Minimal bactericidal concentration or MBC
Requires further plating to determine if any cells survived (in vitro tests for antibiotic effectiveness)
Kirby Bauer Disc Diffusion Test/Assay (clear zones indicate growth inhibition)
A simplified agar diffusion test that can handle 12 antibiotics on one plate makes evaluating antibiotic susceptibility a manageable task. A dispenser deliver up to 12 disks with different antibiotics to the surface of a Mueller-hinton agar plate
0 mm
Kirby Bauer Disc Diffusion Test: No zone around disk is reported as
MIC (measured by serial dilution techniques but can be approximated with the Kirby-Bauer disk diffusion technique)
The diameter of the zone around an antibiotic disk correlates to the WHAT of that antibiotic against the organism tested (measure edge to edge across the zone of inhibition over the center of the disc)
Zone of inhibition
The ____ refers to the measured area around filter-paper disks impregnated with antibiotics
E Test (a strip that contains a gradient of antibiotic/antimicrobial concentration and is placed over a fresh lawn of bacteria spread on an agar plate)
Since tube dilution stake time, this process can reduce processing time by using strip tests which avoids the need for dilutions. While the bacteria are trying to grow, the drug diffuses out of the strip and into the medium
An elliptical zone of inhibition where the antibiotic has stopped bacterial growth (MIC is the point where the zone intersects with the strip)
During an E Test, drug diffusing from the MORE concentrated areas of the strip will achieve and maintain an MIC FARTHER away from the strip resulting in…
Antibiotic is removed from the body via excretion by the kidney or destruction in the liver
The tissue level of a drug over time depends on how quickly the …
Chemotherapeutic index
Ratio of toxic dose to therapeutic dose (ideally the therapeutic dose is much lower than the toxic dose
Chemotherapeutic index = toxic dose/therapeutic dose = how much body can tolerate/how much needed to stop bacteria
What is the chemotherapeutic index equation?
Higher, safer
The _____ the chemotherapeutic index, the _____ the drug
Therapeutic dose
Minimum dose per kilogram of body weight that stops pathogen growth
Toxic dose
Maximum dose the patient can tolerate
Synergistic or antagonistic
Combinations of antibiotics can be…
Synergistic drugs (EX: Amino-glycosides inhibit protein synthesis and vancomycin inhibits cell wall synthesis; work poorly on their own but when combined they work well)
Have a greater effectiveness when used together (each drug alone works poorly but the drugs can work well if combined)
Antagonistic drugs (EX: Penicillin and macrolides)
Their mechanism of action interfere with each other and decrease effectiveness (can occur when a bacteriostatic agent is combined with a bactericidal agent
Metabolic, protein synthesis (50S ribosome subunit), DNA replication, RNA polymerase and cell wall inhibitors (*also cell membrane damage)
What are examples of inhibitors or different antimicrobial (antibiotic) drugs that work to kill or stop the group of bacteria (Diagram shows a bacterial cell and where different antibiotics act within it)
Microbiota (human)
The collection of all microbes (bacteria, archaea and eukaryotic) on the human body
Colonization
The ability of the microbe to stay attached to the body surface and replicate (grow in a place to increase # of organisms)
Adhesins
Proteins on their surface that enable the microbiota to attach to host cells and colonize epithelial cells lining mucous membranes
Parasites
Microbes that cause harm-inducing infections
Ectoparasites, endoparasites
Parasites on the body surface (fleas or lice), parasites inside host body (helminth/tapeworms)
Pathogen
Any bacterium, virus, fungus, protozoan, or worm (helminth) that causes disease in humans
Pathogenicity
The ability of the organism to cause disease
Infection (MOST infections do not cause symptoms and go unnoticed)
Occurs when a pathogen or parasite enters and begins to grow on the host
Disease (infection with a microbe does not always lead to disease)
Occurs when the patient develops symptoms after an infection
Acute infection (EX: common cold)
Symptoms develop and resolve rapidly
Chronic infection (EX: tubercuolosis)
Symptoms that develop gradually and resolve slowly
Primary pathogens
Likely to cause disease after infection in a healthy host, rapidly reproduce/increase in number (ex: influenza virus), and are moderate to high virulence
Opportunistic pathogens
Less likely to cause disease in a healthy host, low virulence, in immunocompromised patients
Latent (pathogen is present in host but its inactive and causing no symptoms)
Some pathogens have a ____ state where the pathogen cannot be found in culture (explains why some microbes cannot be located in the body that cause disease)
Virulence (how deadly or harmful a pathogen is)
Describes the level of harm caused by a pathogen following infection
Lethal dose 50% (LD50) (Lower LD50 = more lethal/harmful)
Virulence can be measured by _____, the number of bacteria or virus particles (virions) required to kill 50% of an experimental group of animal hosts (mice/guinea pigs)
Infectious dose 50% (ID50) (Lower ID50 = more contagious)
Virulence can be measured by _____, the number of microbes required to cause disease symptoms in half of an experimental group of hosts
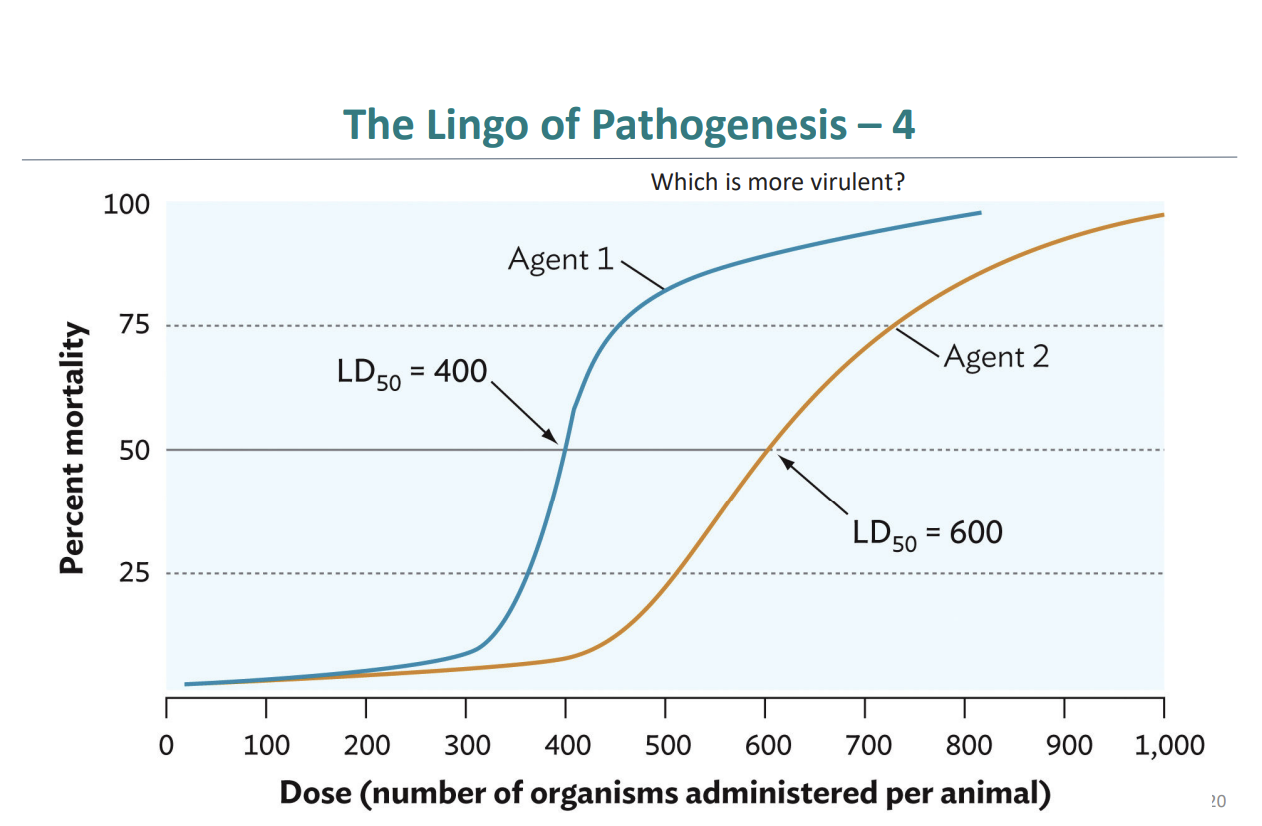
Agent 1 is more virulent because it has a lower LD50 (400) compared to Agent 2 (600) (This means that fewer organisms are needed to kill 50% of the animals)
This graph compares Agent 1 and Agent 2: Which is more virulent? Agent 1 has an LD50 of 400 (kills 50% of the animals at a dose of 400 organisms) whereas Agent 2 has an LD50 of 600 (takes more organisms to kill 50% of the animals)
Invasion (EX: Mercy west doctors invading Seattle Grace!)
One aspect of a pathogen that contribute to virulence defined as the entry of a pathogen INTO A LIVING CELL where it then lives
Invasiveness
One aspect of a pathogen that contribute to virulence defined as the ability of a bacterial pathogen to SPREAD RAPIDLY THROUGH TISSUES
Disease (identified by characteristic signs and symptoms)
A disruption of the normal structure or function of any body part, organ, or system that can be recognized by a characteristic set of symptoms and signs
Infectious disease
A disease caused by a pathogen (bacterial, viral, or parasitic) that can be transferred from one host to another
Signs (examples include fluid filled rash, fever of 102)
Can be observed by examination, objective marker of disease
Symptoms (examples include pain and fatigue)
Experienced by the person, subjective indicator of disease
Syndrome
A collection of signs and symptoms that occur together and collectively characterize a condition
Immunopathology
Many of the signs and symptoms of disease are caused by the hosts response to the infection (cells damage nearby host tissue when killing the microbe)
Sequelae (complication or condition following a prior illness or disease)
After a disease resolves, pathological consequences called ___ may develop. For example, the immune response to strep throat can cause heart damage weeks after the infection has resolved (bodies immune response to the infection mistakenly attacks the heart valves)
Host range
How readily a pathogen can infect different animals
Incubation, prodromal, illness, decline, convalescence phase, long term
What are the 6 characteristic stages of an acute infectious disease?
Incubation phase
Stage of an infectious disease, where an organism begins to grow but symptoms have not developed, both number of microbes and immune response are low
Prodromal phase
Stage of an infectious disease, which can be unapparent or show vague symptoms, number of microbes is increasing and higher than immune response
Illness phase
Stage of an infectious disease, when signs and symptoms are apparent and the immune system is fighting the disease, high number of microbes than immune response
Decline phase
Stage of an infectious disease, when the number of pathogens decrease and symptoms abate/become less intense, higher immune response than number of microbes
Convalescence phase
Stage of an infectious disease, when symptoms are gone the patient recovers, high immune response and low number of microbes
Morbidity
A measure of how many people are sick from an infectious disease, rate of illness due to a disease
Mortality (CDC publishes the Morbidity and Mortality Weekly Report)
A measure of how many died, rate of death due to a disease
Infection cycle
The route of transmission from one person or animal to another
Horizontal transmission
Occurs when the infectious agent is transferred from one person or animal to the next
Vertical transmission
Occurs when the infectious agent is transferred from parent to offspring
Direct contact transmission
Cycles of infection can be simple or complex: organisms may spread directly from person to person (EX: kissing, touching or sex)
Indirect Transmission
Pathogens may spread indirectly through an intermediary, which may be living or nonliving (EXAMPLES: airborne transmission, fomites (inanimate objects), vechiles such as food, water, or air, vectors such as ticks or mosquitos)
Reservoir (do not necessarily exhibit disease)
An animal (including humans) or an environment that normally harbors the pathogen. These are crucial for the survival of a pathogen and serve as a source of infection
Asymptomatic carrier
Harbors the potential disease agent but does not have the disease (EX: Neisseria meningitides is an important cause of meningitis but it has no animal reservoir and is maintained in the human population by these hosts)
Endemic (always present in an area, usually in small numbers)
Disease is one that is always present in a community at a low rate, often in an animal reservoir
Epidemic (the number of victims suddenly rises above endemic levels)
Disease is one in which the number of cases increases in a community in a short time
Pandemic
Disease is an epidemic that spreads worldwide (EX: Influenza, HIV, Covid-19)
Portals (routes) of entry/exit (how microbes get into your body)
Pathogens use _____ ___ ______ best suited to their mechanisms of pathogenesis to gain access to the body from one host to the next
Fecal-oral
The portal is the mucosa of the GI tract (pathogenies can be INGESTED)
Skin
The portal is the skin epithelium (Skin can be colonized by some pathogens and PENETRATED by others, WOUNDS offer pathogens access to body’s interior)
Respiratory
The portal is the mucosa of the respiratory tract (AIRBORNE pathogens can be inhaled)
Urogenital
The portal is the mucosa of the genital and urinary tracts (Pathogens can enter via direct contact with GENITAL MUCOSA or SEXUAL TRANSMISSION)
Parenteral
The portal is through breaks in the skin (Pathogens can be injected into the BLOODSTREAM)
Entry via the eye
The portal is conjunctiva
Standard Precautions (regulations designed by the CDC to protect medical personnel)
Proper hand hygiene, use PPE, respiratory and cough hygiene, safe injection practices, handle sharps safely, practice patient isolation precautions, serialize instruments and clean and disinfect environmental surfaces are all various levels of protective measures used for handling potentially infectious biological materials
Four (levels correlate the hazard potential of an infectious agent with the level of containment and precaution necessary to work safely with each)
In the lab, ____ levels of agent contaminant are employed depending on the biosafety level (BSL) of the infectious agent
BSL 1
Low risk, basic precautions
BSL 2
Human pathogens causing mild disease, barrier precautions
BSL 3
Human pathogens causing serious illness, separate rooms, work done in a biosafety cabinet (BSC)
BSL 4
High virulence pathogens where exposure can be lethal, separate facilities, may require use of a positive-pressure suit must wear earplugs to protect hearing
More
The more microbes that get in, the _____ likely they can cause infection
True (For example a burglar needs to get through the door and stay inside)
T/F: The microbes must stick to your body’s cells before they can cause harm known as ADHERENCE
Trick or fight off your body’s defenses
In order to survive, microbes need to ______ (avoid immune system)
Capsules, cell wall components, enzymes, antigenic variation
What are some ways microbes avoid the immune system
Toxins (Exotoxins are released by microbes and Endotoxins are part of the microbes outer layer)
Microbes release _______ which are poisons
Viruses changing cells to make them more harmful, destroys cells directly
Lysogenic conversion vs direct damage
Breathing out, sneezing, feces, open wounds (microbes usually leave the same way they came in so they can spread to others)
Examples of portals of exit (how microbes leave your body)
Enter the body, stick to cells, avoid immune defense, cause damage, then leave to infect someone else
Mechanisms of Pathogenicity diagram in a simple sentence starting with microbes ___ (Ellis see Alex, Cristina then Lexie)
Example of virulence factors (allow microbial pathogens to cause disease)
Pili (help attachment), enzymes that harm the host or prevent detection, proteins that disrupt normal cellular function, capsule, enzymes that inactive antibiotics
Pathogenicity island
A genomic island that contains virulence factors
Genomic island, horizontal gene transfer
A region of the bacterial chromosome that has altered GC (guanine/cytosine) content and segments of phages or plasmid DNA that mark it as different from the rest of the genome. Entire genomic island can be acquired via _____
Conjugation, transduction, transformation
What are the three components of horizontal gene transfer?
Conjugation
A donor cell directly transfers genetic materiel, often in the form of a plasmid, to a recipient cell, sometimes via a specialized tube called a sex pillus
Transduction
A virus (bacteriophage) mistakenly picks up a fragment of host DNA during its replication and then transfers it to a new host cell when it infects it
Transformation
Bacteria take up naked DNA fragments from their enviorment and integrate them into their own genome
If the transferred island INCREASES the fitness of a microorganism (pathogen) during interaction with a host (new emerging pathogens evolve this way)
How to spot a pathogenicity island?
Adhesion (types include pili also called fimbriae and nonpilus adhesions)
The human body has mechanisms to exclude pathogens, pathogens must evade these mechanisms in our to attach. For pathogen attachment, an _____ is any microbial factor that promotes attachment