NPLQ Gen 10 notes
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
100 Terms
what is the chain of survival
1. Early recognition (to prevent cardiac arrest)
2. Early cardiopulmonary resuscitation (to buy time)
3. Early defibrillation (to restart the heart)
4. Post-resusitation caren(to restore quality of life
how do you manage/ treat stomach contents regurgitation of an unconscious causality
1. turn the causality away from you keep them on their side and use your elbow and forearm to balance the causality and to prevent there arm flopping in-front of them
2.Ensure the head is turned towards the floor and their mouth is open, to help the regurgitation to drain away make sure their moth is the lowest point
3. Clear any debris left in the mouth with your fingers and immediately turn them onto their neg and re-establish an airway before beginning cpr.
what is a cardiac arrest
when the heart stops beating blood around the body, this could be from a medical reason or a result of lack of oxygen from asphyxia as an example (drowning). Sometimes seizure like activities make accompany the cardiac arrest. once these have finished check patient for correct breathing
what are the principles of airway management
head tilt chin lift

what is the sequence if an adult CPR
DR ABC
1. check for danger for yourself and any bystanders
2. check the causality and see of they respond- hello are you alright
3a. if the casualty responds then leave them in the same position you found them and find out what is wrong with them and try and assist, reassess the causality frequently
3b. if the causality does not respond then turn casualty on to they back and open their airway
4. check their breathing for no longer than 10 seconds- look for chest movement, listen for breath sounds and feel the air on your cheek. the patient may be taking infrequent or snoring like breaths called atonal gasps, these are an indication to begin CPR immediately
5. call for someone to call an ambulance, explain what has happened, implement EAP, activate the speaker mode, send someone to get a AED (do not leave yourself), start CPR
6. CPR
--> kneel next to the casualty, place hands on chest and complete 30 chest compressions at 5-6cm in the centre of the chest with straight arms, the rate should be between 100-120 times a minute. THEN after 30 compressions pinch the top part of the nose and maintain a chin lift, give two rescue breaths, watch the breaths go in and out.
if the chest does not rise check for a visible obstruction, recheck the head tilt and chin lift but do NOT do more than THE 2 RESCUE BREATHS. return to the 30 chest compressions
7. when the AED arrives switch it on and follow the instructions, you should only stop CPR when a health professional tells you to, you become two exhausted, or if the casualty has definitely woken.
(if the causality is breathing normally then place them in the recovery position, ensure the EAP is implemented, only leave casualty if there is no one else to help, continue to assess and start CPR if needed)
what is the sequence of child CPR
it is rare for a Childs or infants heart to stop so the most likely reason is from drowning, infection, injuries and inhalation if other objects that prevent breathing leading to a cardiac arrest
follow the adult steps but:
1. having asked someone for a ambulance and a AED, give 5 INITIAL RESCUE BREATHS before starting CPR
2. use one hand over the chest if the child is over 1 year, complete the chest compressions and the 2 rescue breaths
3. if you are on your own, perform CPR for approx. 1 min before fetching help
what is the sequence of infant CPR
it is rare for a Childs or infants heart to stop so the most likely reason is from drowning, infection, injuries and inhalation if other objects that prevent breathing leading to a cardiac arrest
follow the adult steps but:
1. having asked someone for a ambulance and a AED, give 5 INITIAL RESCUE BREATHS before starting CPR
2. when performing rescue breaths stabilise the infants head in a neutral position, they may require some extension with a chin lift
3. seal your mouth around their mouth and nose and use the air in your mouth
4. after the 5 rescue breaths move onto chest compressions with two fingers in the middle of the chest
5. if you are on your own, perform CPR for approx. 1 min before fetching help
CPR flow chart
unresponsive and not breathing normally
|
call 999 and ask for ambulance and AED
|
if drowning, child or infant give 5 rescue breaths
|
30 chest compressions
|
2 rescue breaths
|
continue CPR 30:2
|
as soon as AED arrives turn on and follow instructions
what are some problems with CPR
Tracheotomies, Regurgitation, Air in Stomach, Broken ribs, Chest does not rise, Fluid in Airway, Confined space
CPR and tracheostomies
1. remove any stoma cover NOT THE TUBE
2. wipe away any mucus from the stoma or tube
3. Close the casualty's nose and mouth
4. Play your mouth around the opening in the neck
5. Blow into the stoma and watch the chest in the normal rescue breath way
CPR and air in stomach
sometimes extra strength or breaths are needed when there is an obstruction in the airway, this could lead to the air entering the stomach increasing the risk of regurgitation.
1. attempt to improve the casualty's airway by increasing the head tilt and chin lift
2. do not apply pressure over the stomach
3. provided a clear airway the air should leave the stomach
CPR And broken ribs
this can happen especially with the elderly or those with rigid chests and is most often unavoidable. If a rib breaks not action should be carried out or should be during resuscitation which should continue as usual.
CPR and the chest does not rise
1. check the persons mouth and remove any visible obstruction
2. recheck that there is adequate head tilt and chin loft
3. do not attempt more than 2 breaths
CPR And Fluid in the Air Way
in some situations foam or fluid may come out of the mouth, do not attempt to remove this it will keep coming just continue the rescue breaths and the compressions
CPR in a confined space
perform compressions from the head rather than the side
symptoms and treatment of fainting
symptoms:
-nausea
-blurred vision. black spots
-pale face
-sweat on face, neck and hands
-breif unconcuoisness
-cold clammy skin
-shallow breathing
-slow, weak pulse
treatment:
(feeling faint)
1. reassure them and advise to breath deep and slow
2. lay them down and raise their legs
3. ask bystanders to leave and help remain calm
4. once recovered provide sips of water
(full faint)
1. lay down
2. raise legs
3. check airway
4. if they do not come round quickly and they are breathing normally place in recovery and call 999 monitoring breathing
symptoms and treatment of stroke
symptoms:
FAST
(facial weakness, arms can't be raised, speech is slurred and then it is time to call 999)
treatment:
call 999
keep person comfortable, if they are responding lay them down with the head and shoulders slightly raised
reassure them but remember they may not be able to speak well and answer questions
if they become unconscious and are breathing normally place in recovery
symptoms and treatment of poisoning, drugs, alcohol, chemical and gases
drug abuse:
-recreational use of illegal drugs or by accidental or deliberate misuse of prescribed medication
alcohol abuse
-result of excessive consumption of alcohol
release of chemicals or gases:
-a release of these may come from the plant room or store room, follow the EAP and use COSHH to help
symptoms:
difficulty breathing
dizziness
nausea or vomiting
abdominal pains
head ache and confusion
evidence of poisonous substances
unusual smell
pale skin
burns
treatment:
-move to a safe place
-remove cause if possible
-do not induce vomiting
-rinse mouth and give sips of water or milk (swallowed)
-treat injuries e.g burns
-if unconscious and breathing normally place in recovery
-call 999
-use face mask with CPR
-collect info and pass onto emergency services
How can poisons enter the body?
Inhaled, injected, absorbed, ingested
symptoms and treatment of insect bites
symptoms:
complain of pain
swelling in the area around sting or redness
treatment:
-remove sting by brushing it out or using a plastic card, do not use tweezers
-apply a cold compress for 20 mins to relive pain and swelling
-for stings to mouth suck ice and call 999
-for severe and in anaphylaxis call 999 or use epi pen
symptoms and treatment of diabetic emergency
symptoms:
-loss of concuoisness
-rapid pulse
-faintness or dizziness
-trembling or limbs
-confusuon
-could be agressive
-pale skin
-sweating
-shallow breathing
-unconcious
treatment:
(conscious)
-sit them down and give them a sugary drink
-if they respond continue with surgery food or drink and advise them top rest and seek medical advice
-if they do not respond call 999
(unconscious)
-call 999
- place in recovery if they are breathing normally
-monitor airway and breathing
-carry out CPR if need
what is the change of survival
1. early recognition = implement your EAP, call for help and alert the emergency services as soon as you possibly can in order to get professional help
2. early cardiopulmonary resuscitation (CPR) = those who are present when a casualty has a cardiac arrest you should start CPR as soon as possible
3. early defibrillation = applying a controlled electric shock across the chest to re-start the heart
4. post resuscitation care = includes various medical and paramedical procedures such as drugs
what are the priorities when treating a casualty
- emergency CPR
- management of choking
- control of life-threatening bleeding
- care of the unconscious breathing casualty
- treatment for shock
- medical attention
when do you use the recovery position
For a person who is breathing and unresponsive
when is it not appropriate to place someone in the recovery position
when the casualty has suffered significant physical injury, it may not be appropriate to move them unless there airway is in imminent danger from regurgitation or you have to leave them in order to treat other casualties
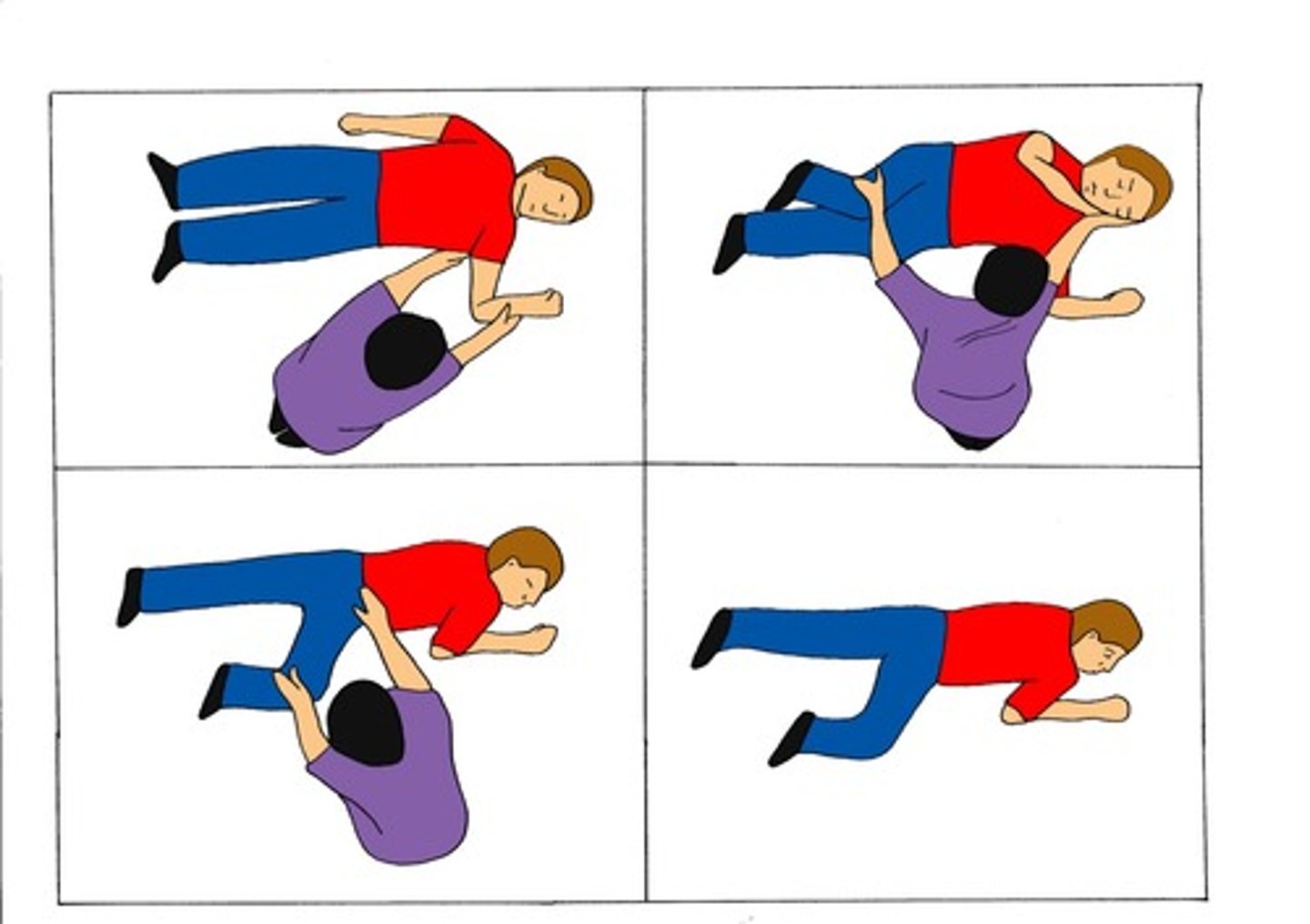
How to place someone in the recovery position
- remove the casualties glasses or goggles
- kneel beside them and make sure both legs are straight and together
- place the arm nearest to you out at a right angle, elbow bent and palm up
- bring the far arm across the chest an hold the back of the hand against the causalities cheek nearest to you
- with your other hand pressed against the cheek, pull on the far leg just above the knee and roll the casualty on their side towards you
- adjust the upper leg so that both the hip and the knee are bent at right angles
- tilt the head back so that the airway remains open
- if necessary adjust the hand under the cheek to keep the head tilted and facing downwards to allow liquid material to drain from the mouth
- check breathing regularly and if it does not remain normal then restart CPR
how long can a casualty remain in the recovery position
they should be kept lying for no longer than 30 minutes on each side to avoid prolonged pressure on the arm and you should stay with them unless absolutely necessary to attend another casualty
What is asphyxia?
also known as suffocation when the body is deprived of oxygen
what can cause asphyxia
tongue blocking the airway of an unconscious person, a foreign object stuck in the throat , strangulation, the mount and nose being covered, drowning
how do you manage the airways
head tilt and chin lift, this will lift the tongue and open the airway
how many breaths are needed for CPR after drowning
5, five rescue breaths before you commence CPR, always do this for children and infants and 5 for a drowning adult but 2 for a non drowning
how do you begin the sequence of CPR in the water following the recovery of the casualty
whilst waiting for assistance to remove the casualty rescue breaths should be performed using the mouth to nose technique.
1. support the casualty with one arm underneath the neck and shoulders and hold onto the poolside
2. If assistance is already available then remove the casualty and begin CPR and reduce breaths on poolside
3. if no assistance is available place ear over mouth and nose and look listen and feel for any signs of breathing, for no longer than 10 seconds using using head tilt chin lift
4. if the casualty is not breathing normally then maintain head tilt chin lift and keep the mouth closed and form a seal around the nose and give rescue breaths
5. continue with these until help arrives
what is drowning
It is the process of experiencing respiratory impairment from submersion/immersion in liquid
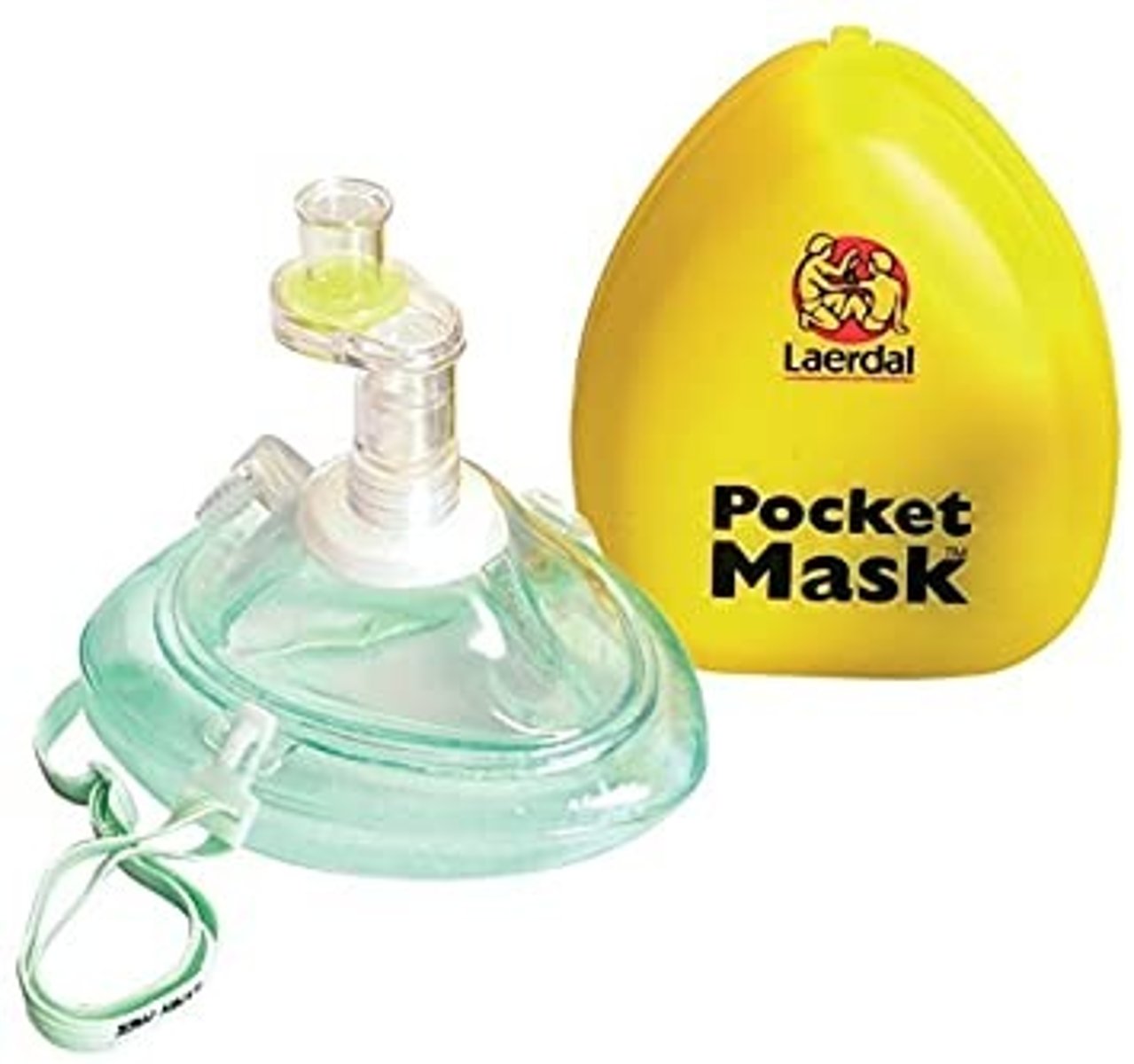
what is a pocket mask
a mask that is placed on the patients face, they minimise the transfer of infection and they can be reused provided that they are cleaned and that the valve is replaced
what problems can there be fore CPR
tracheostomies:
- a tube that is inserted into the lower neck to create an alternative entry for the air leaving an opening in the wind pipe
- remove the cover, wipe any mucus, close the casualties mouth and nose, place your mouth around the tube and blow into the tube watching the chest rise and fall.
air in stomach:
- sometimes when a adequate airway is not prodiuced from head tilt chin lift the air can be forced down into the stomach casing as swelling in the abdomen below the left ribs, affecting the movement of the diaphragm and potentially inducing stomach regurgitation
- if this is seen do not apply pressure etiolated the stomach as this will induce regurgitation, ensure the head tilt and chin lift is efficient and make sure it is maintained to allow the stomach to escape
broken ribs:
- during chest compressions the ribs may be heard to break especially in older casualties with brittle bones or due to incorrect positioning of the hands during CPR. No action can be taken and CPR should be continued but expect the casualty to be in pain after recovery
chest does not rise:
- do not reattempt the 2 breaths, alter the head tilt chin lift and check that there Is nothing blocking the airways
fluid in the airway:
- foam can be created due to the air mixing with the water in the breathing tube, do not attempt to remove this as it will keep going just continue as usual
confined spaces:
- over the head CPR can be used in confined spaces
what should happen with CPR and spinal injuries
particular care should be taken with the head, neck and spine to ensure alignment is maintained. Support will be needed from other member of the team by holding the head steady to prevent any movements and using minimal head tilt and chin lift
what are the signs and symptoms of choking
- Casualty may have been seen to be eating
- A child may have been seen to be put an object in their mouth
- casualty who are chocking will often clutch their throat with one or two hands
- With PARTIAL obstruction the casualty ma be able to speak and cough and breathe but they will be distressed
- With COMPLETE obstruction, the casualty may be unable to speak and cough, they may not be able to breathe, face turning blue and veins standing out of the neck
- Casualty may become unconscious
what is the flow chart of choking
1. assess the severity.
- if its a mild airway obstruction (meaning that they can cough) --> encourage them to cough constantly checking for deterioration and see if the object has been dislodged
- if its severe meaning the cough is ineffective
--> unconscious then start CPR but if that are conscious perform 5 back blows and 5 abdominal thrusts
what is the treatment for an adult choking
breathing = encourage coughing
severe obstruction = stand slightly to the side and behind, support their chest with one hand and lean them forwards so that if the obstruction is dislodged it will exit the mouth
- give up to 5 back blows between the shoulder blades with the heel of your hand, try once check and if needs be try again
- if back blows fail then do 5 abdominal thrusts, stand behind the casualty and place a fist between the umbilicus and the sternum wrapping the arms around the body and pull sharply inwards and upwards. the obstruction should be dislodged and fly out of the mouth
what should you do if a chocking adult becomes unconscious
it may result in the relaxation of the muscles around the throat and allow air to pass down to the lungs. If they become unresponsive begin CPR straight away, support the casualty to the ground, call 999 and begin CPR
what is the treatment for a choking infant and child
support the infant across the knee or lap is seated and ensure that the head is blow the chest so that the dislodged object comes out of the mouth.
- It is dangerous to give infants abdominal thrusts so instead if 5 back blows fail used 5 chest thrusts, on the sternum with sharp and but slower rate thrusts. It is important that infant is on a firm surface such as your thigh and that their head is below their chest
- check the casualties mouth and if the object has not been dislodged call the emergency services ad continue the sequence of back blows and abdominal/ chest thrusts
what should you do differently for a chocking obese or pregnant person
chest thrusts should be used instead of abdominal thrusts if the rescuer cannot encircle the abdomen of the casualty.
what is a AED
Automated External Defibrillator - a portable device that checks the heart rhythm and if needed, can send an electric shock to try and restore a normal rhythm.
what do you do if a AED is not immediately available
start CPR straight away whilst waiting for a AED and when it arrives use it immediately
when do you stop CPR
The rescuer should try not to stop. However, he or she may if:
- he or she becomes so exhausted they cannot continue
- someone of equal or greater training comes to take over
- his or her personal safety is in danger (as in the scene is not safe)
- the victim is pronounced dead by a medical doctor or they are definitely waking up, moving, breathing normally and opening eyes
What are agonal gasps?
Sign of cardiac arrest; not normal breathing; may sound like a snort, snore, or gasp.
where do you place the defibrillation pads
1. Mid-clavicular line just above the right nipple.
2. Mid-axillary line over the 6th left intercostal space.
What are the priorities of first aid
Preserve life
Alleviate suffering
Prevent the situation getting worse
Promote casualty recovery
What should be recorded after a incident
What happened? Where did it happen? When did it happen? What was the casualty doing? How did it happen? Details of injuries person. What was the injury? What first aid was administered? Who administered first aid? What happened next?
What is the NOP
Normal Operation Proceedures
What is in a NOP
What should be in a first aid kit
Guidance leaflet, contents list, large sterile dressing, medium sterile dressing, triangular bandage, safety pins, eye pad sterile dressing, adhesive sterile dressing alcohol free cleaning wipes, adhesive tape, disposable gloves, stair dressing with face shield for your blanket, dressing shoes, conforming bandage
What should not be in a first aid box
Pills, medicine, sprays, creams, sharp scissors, cotton wool, inhalers
What hygiene procedures should be taken
1. Wear gloves and aprons
2. Wash your hands
3. Keep the wound and dressing clean (do not sneeze or cough near one)
4. Clean up after treatment
What is a PSOP?
Pool safety operating procedure
How should you deal with sharps
The details of the procedure will be detailed in the PSOP, many centres will have a sharps bin where the sharps can be placed before being disposed of properly and incinerated. Such as an auto injector
What is the history
What has happened. Find out what happened leading up to the event as witnessed or bystanders. Check for medical factors such as previous medical history, information on a medical bracelet or medication
What are symptoms
How they feel what the casualty tells you. Examples could be stiffness, loss of feelings, tenderness, pain, temperature, thirst, nausea, tingling, dizziness
What are signs
Something you can see, hear or feel. Examples may be bruising, bleeding or joint pain, hear problems with the breathing, swelling, abnormal temperature, alcohol, burning gas and urine
Consent to give first aid must be obtained from every victim who is:
responsive, mentally competent, and of legal age, if they do not allow you to help and they need emergency aid then call 999. If they are unconscious you do not need to get consent
What is the primary survey
Assessing the casualty for life threatening injuries and taking immediate and appropriate action at each stage. DANGER, RESPONSE, AIRWAY, BREATHING, CIRCULATION
What is a second survey
Determines the history and background of the injury, assessing the mechanics of the injury, looking for signs and determine and conducting a thorough examination of the casualty.
What can cause an unconscious casualty
Reduced blood supply, head injury, poison, drugs, extreme temperatures, drowning, seizure or diabetics emergency
symptoms and signs of an unconscious casualty
as the casualty is unconscious they will be unable to tell you any of their symptoms. The level of consciousness can be varied with light drowsiness to completely unresponsive. the best way to decide this is to shake them gently and talk to them, ask if they are aware o you talking to them but be careful not to induce or make worse any injuries
how do you treat a unconscious casualty
start by completing the primary survey and beigninibg CPR if needed, treat any major bleeds if necessary and complete a secondary survey if they are unconscious following an accident. If they are unconscious due to shock etc place them in the recovery position. protect them from the wet and the cold
what is a heart attack
A blockage of blood flow to the heart muscle.
what are symptoms of a heart attack
dizziness, nausea, severe crushing or tightening sensation, pain In chest/ left arm, rapid - weak - irregular pulse, feeling of impending doom, anxiety, blue tinge to skin and lips, sweaty skin, clutching chest or sudden collapse
what is the treatment of a heart attack
- call 999
- assist casualty to sit comfy in a half sitting position
- loosen tight clothing
- ask casualty too take any prescribed medication
- remove any cause of stress
- reassure the casualty
- monitor the casualty
- be prepared to perform CPR
what does the HSE First aid at work regulation says about heart attacks
some casualties may carry their worn medication that they have been prescribed to by a doctor, they should encourage the casualty to take it themselves and should contact the emergency services to help
what is shock
A life-threatening medical condition whereby the body suffers from insufficient blood flow throughout the body as a result of severe injury or illness
what are the symptoms and signs of shock
symptoms: dizziness, confusion, disorientation, thirst and nausea.
Signs result as a lack of oxygen to the body and the body tries to composite this: pale, cold clammy skin, blueness, weak and rapid pulse, shallow breathing.
how does the body compensate for the lack of circulating blood
the body compensates by drawing the remaining blood away from the skin and directing it to more important areas. Increasing the rate of breathing to get as much oxygen as possible into the blood. Speeding up the heat to circulate the blood more rapidly.
what is the treatment of shock
- assist the casualty to lie down, rise the casualty legs where possible injures permit
- loosen tight clothing around the neck, chest and waist
- treat the cause of shock when possible
- reassure the casualty
- monitor the casualty
- keep them warm to prevent heat loss
- do not give them food or drink
- call 999 for help if there is no improvement
why does the body go into shock
- low blood volume
- loss of bodily fluids such as severe vomit or diarrhoea or severe blood loss
- low cardiac output
what is asthma
Constricting of the airway due to inflammation and muscular contraction of the bronchioles. Also called Reactive Airway Disease
can lifeguards look after inhalers or medication
no no no, you cannot accept responsibility for the looking after of any medication or inhalers
what are the symptoms and sings of breathing problems and asthma attack
- breathing difficulties
- wheezy breathlessness
- anxiety (which could have brought on the attack)
- difficulty in speaking
- pale and clammy grey or blue lips
what is the treatment of breathing problems
- reassure the casualty
- sit them in a commutable position
- encourage and assist them to use their prescribed inhaler
- if they have a spacer help them set it up and use it
- use the inhaler again if the attack does not ease
- remove from the cause if known such as a dusty room or fumes
- cold winter airs can make attacks worse so don't take them outside
- call 999 if help is needed in some situations such as if the casualty goes unconscious, medication doesn't not help, lasts longer than normal, distressed or exhausted
what are causes of anaphylaxis
foods such as milk or nuts or egg, medicines, insect bites, latex
what are the symptoms and signs of anaphylaxis
- swollen tongue
- hoarse voice
- difficulty swallowing
- difficulty or noising breathing
- wheeze or persistent cough
- abdominal pain and nausea or vomiting
- anaphylactic shock
- swelling of the hands, feet, face or skin
- red itch rash or raised skin
- anxiety and feeling of terror
what is the treatment of anaphylaxis
- ask the casualty if they have their auto injector with them
- the casualty should administer their own medication as prescribed, adults will generally self medicate and the parent or guardian will most likely medicate a child
- call 999 for emergency help following the use of the first device, even if there is immediate improvement to if further divides are available. The emergency service operator must be told the person is suffering from anaphylaxis and needs to be attended by paramedics
- if they want sit up assist them
- if they feel faint lie them down and raise their legs
- call 999 if they continue to deteriorate, a second dose of medication should be administered if the casualty continues to deteriorate or symptoms return
- be prepared to start CPR if necessary
- if they fall unconscious but are breathing place in the recovery position
can you use a auto injector
only if you have received training, get the casualty to administer them
where does the auto injector go
mid upper outer thigh
what should you say in handover to the emergency team
- casualty name
- what happened
- when and what first aid was administered
- have you used one or two auto injectors
- has the casualty remained conscious throughout
what is hyperventilation
increased rate and depth of breathing following something such as a panic attack or a swimmer thinking it will help them swim underwater or swim faster before a race
what are the symptoms and signs of hyperventilation
dizziness, feeling faint, cramps/ pins and needles in hands and feet, tight chest, panic, rapid pulse, unnaturally fast and deep breathing, flushed skin.
what is the treatment of hyperventilation
Position patient upright, loosen tight clothing, and work with the patient to control breathing, take them to a quiet place and reassure them. Give them water to take small sips off and call 999 if the attack is prolonged
why is a dressing used
it is used to place over a wound to control the bleeding and prevent infection also to absorb any discharge. they should be sterile, absorb and the gauze should be large enough to cover the skin beyond the wound
what are triangular bandages used for
used to make a sling, hold other bandages In place, provide support, restrict movement of or immobilise and injured limb
how do you apply a dressing
always place a dressing straight onto a wound. If the bleeding is under control, clean the wound and surrounding skin first and then apply the dressing. Once a dressing has been applied, particularly the upper limbs, check the circulation to make sure that the dressing is not too tight. Where there is a foreign body protruding the wound apply pressure around the body not ever directly on top and don't ever remove it
where can the body bleed from
capillaries - blood will trickle out seen with small cuts and grazes
veins - the blood will ooze out
artery - the blood will spurt out and can lead to significant and rapid blood loss, leading shock and death
what are types of wounds
bruise, graze, clean cut or slice, laceration (tear or rip), puncture, gun shot
how to treat minor injuries
small cuts:
- irrigate throughly with clean water and remove any dirt
- dry the wound with a sterile dressing and apply an adhesive plaster or sterile dressing
Grazes:
- irrigate thoroughly with clean water to remove any dirt and grit
- dry the wound with a sterile dressing and apply an adhesive plaster or sterile dressing
bruises:
- to reduce swelling use an ice pack wrapped in a clean cloth (triangle bandage can be used)
- apply an ice pack to the bruise for no longer than 20 minutes
what are the symptoms of an external bleed
- pain in the affected area
- shock
-thirst
- weak but rapid pulse
what is the treatment of an external bleed
- wear protective gloves
- lay or sit the casualty in a comfortable position
- call 999 for help in more serious cases
- examine the wound and check for external objects
- apply direct pressure to the wound using a sterile dressing
- treat the casualty for shock
what should you do if the bleeding does not stop
if the bleeding does not stop then re apply a bandage and apply pressure and secure the dressing with a bandage
what symptoms and signs are there for internal bleeding
- skin becoming pale, cold and clammy
- confusion, restlessness that may lead to a collapse and unconsciousness
- bruising and pattern bruising at the point of impact and selling
- shock without any loss of breathing
- thirst
- weak but rapid pulse
what is the treatment of an internal breathing
- call 999
- lie the casualty down
- treat for shock
what is varicose vein
a vein in which blood has pooled due to the one way valve failing and the blood collects behind it. A nock can cause it to be come damages and the blood may squirt and appear quite alarming
what is the treatment of a varicose vein bleed
- help the casualty lay down
- apply firm and direct pressure on the injury using a sterile bandage so the bleeding is under control
- secure another dressing over the first ensuring the pressure is distributed evenly
-call 999
- recheck the limb every 10 minutes