Block 1C - H+N Cancers (Laryngeal, Nasal Cavity, Paranasal Sinuses)
1/133
Earn XP
Description and Tags
ONCOL 310 - Clinical Oncology II. University of Alberta
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
134 Terms
what is the most common H+N tumor?
laryngeal cancer
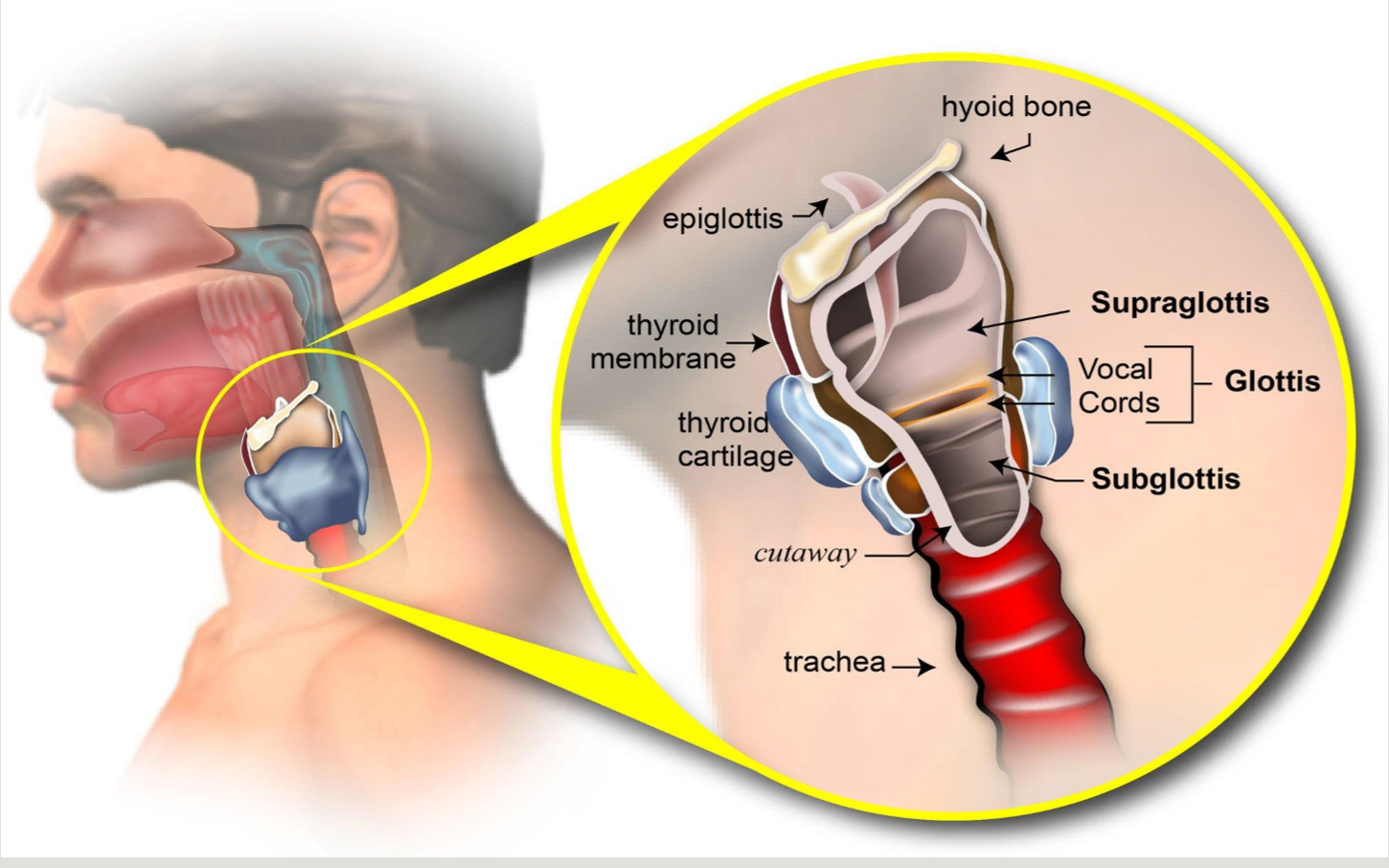
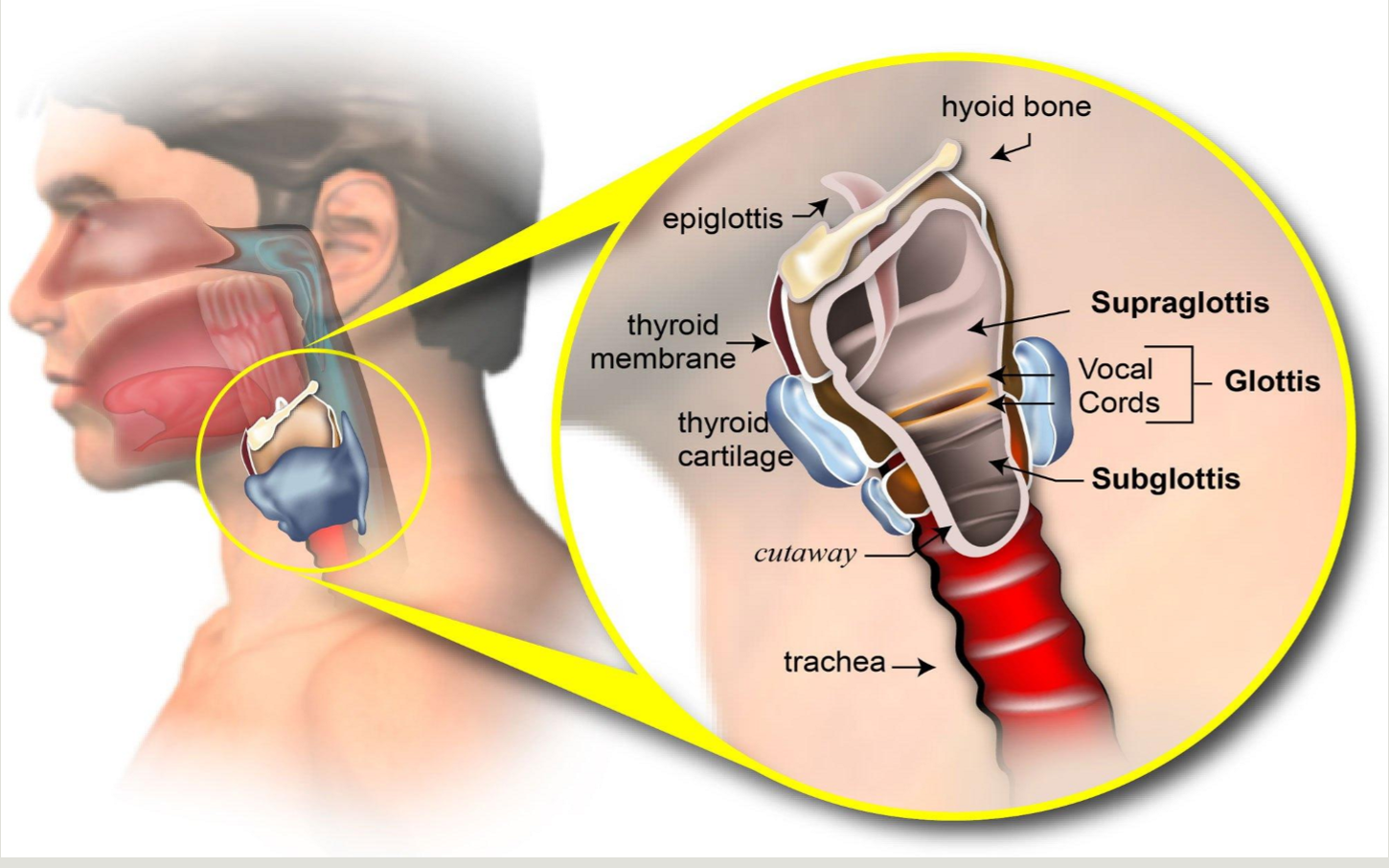
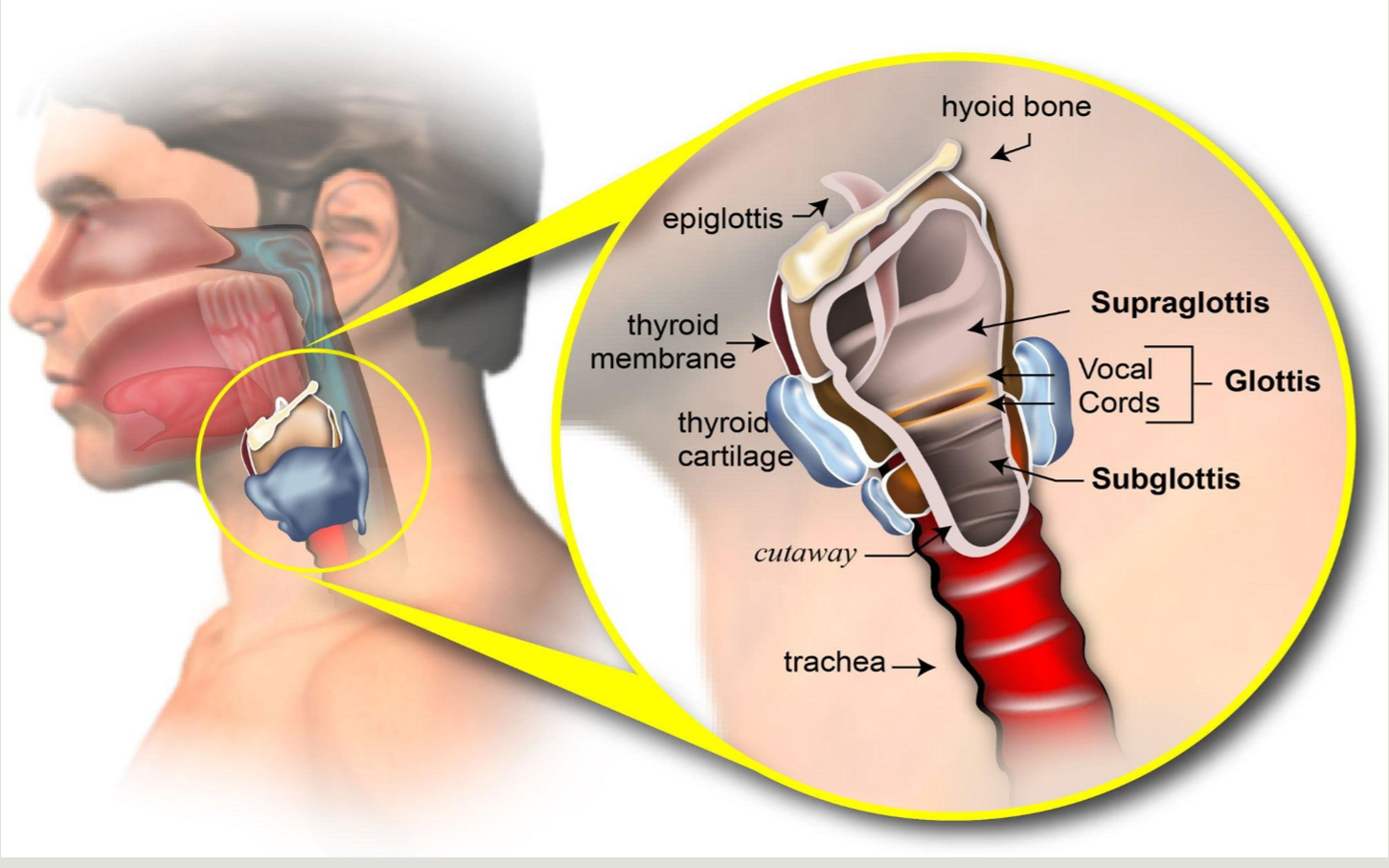
what are the three anatomical regions of the larynx
supraglottic larynx
glottic larynx
subglottic larynx
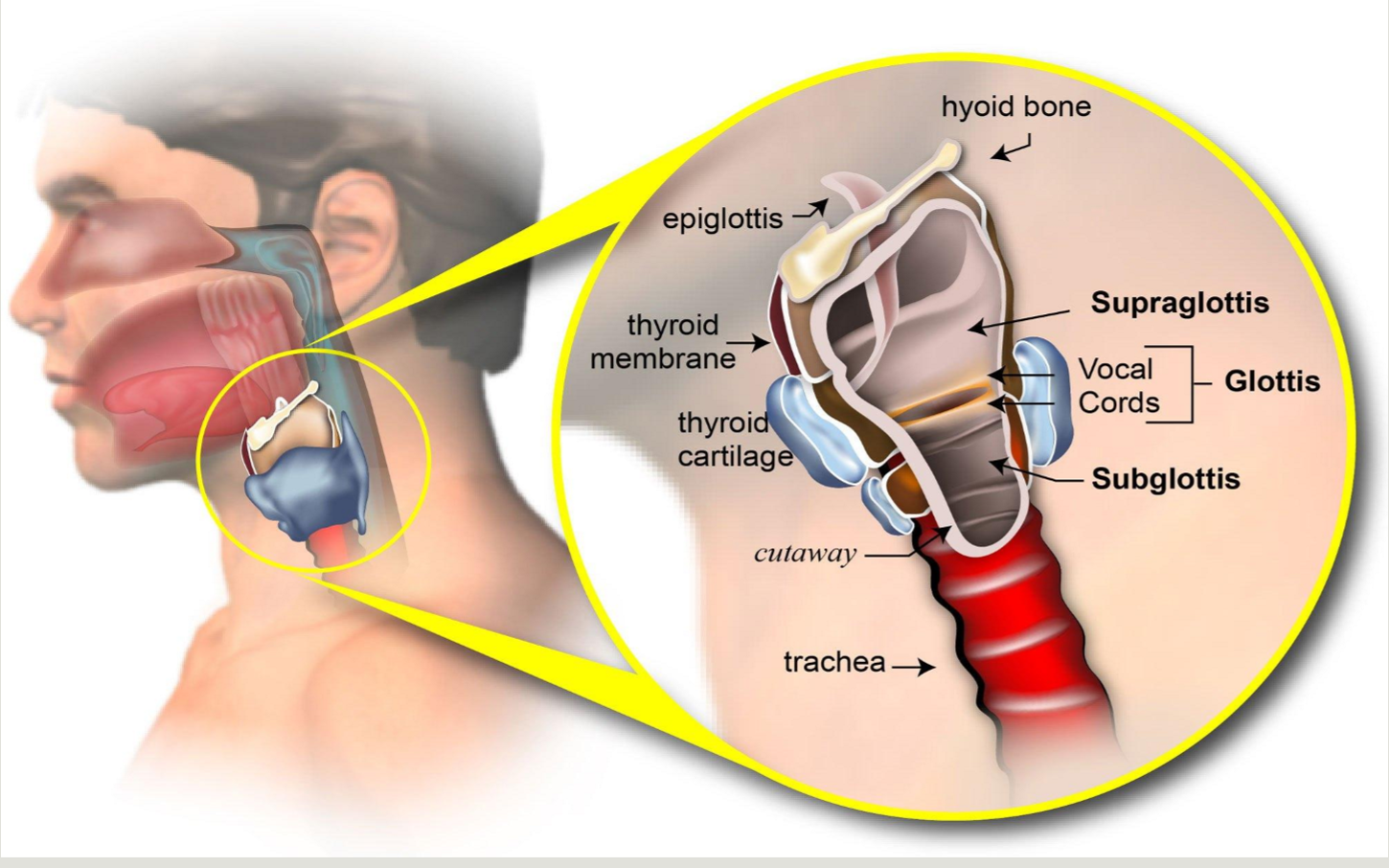
what is contained in the supraglottic larynx
epiglottis, false vocal cords, ventricles, aryepiglottic folds, arytenoids
why does the supraglottic larynx have the most risk of spread?
there is rich lymphatic drainage from the jugulodigastric and mid-jugular
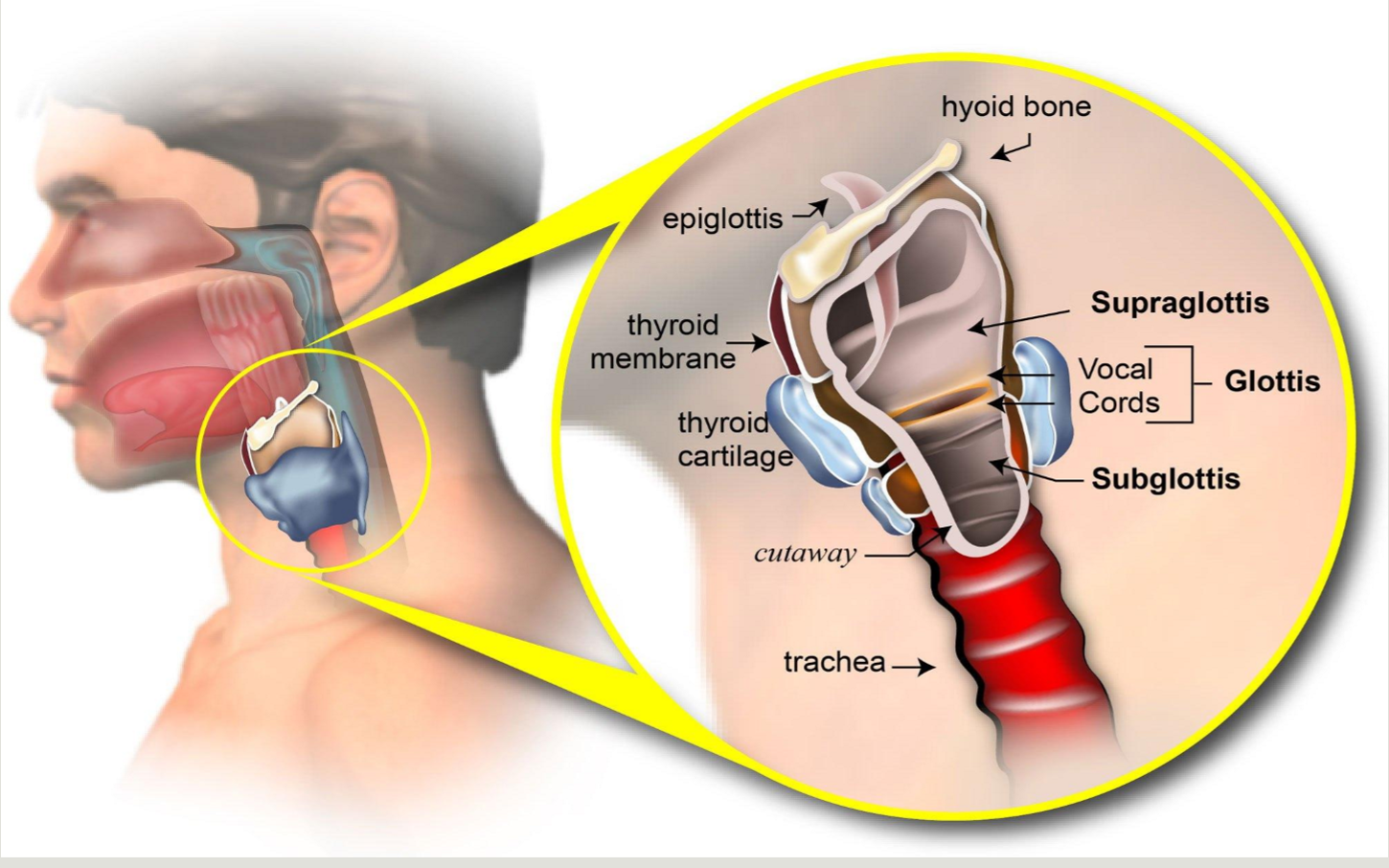
what is contained in the glottic larynx
the true vocal cords and ant/post commissures
are there any LN in the true vocal cords?
no
what is the most common site of laryngeal cancer
the glottic larynx
what is contained in the subglottic larynx
it is the area 1 cm inf to true vocal cords to the lower border of the cricoid cartilage or first tracheal ring (1 cm long)
primary cancers here are rare
larynx cancer epidemiology
M:F ratio
age range
what percent are diagnosed in early stage
M:F = 5.5:1
age: > 65 years
50% are diagnosed as early stage
etiological factors of laryngeal cancers
smoking and excessive alcohol consumption
HPV +
occupational exposure (woodworking, metal, leather)
lower socioeconomic status
poor nutrition and vitamin status
clinical presentation of supraglottic laryngeal cancer
pharyngitis, odynophagia, dysphagia, otalgia, enlarged LN’s
clinical presentation of glottic laryngeal cancer
hoarseness of voice, pharyngitis
clinical presentation of subglottic laryngeal cancer
no symptoms until locally extensive - hoarseness of voice
describe the natural history of laryngeal cancer
arises from the epithelial lining of the mucous membrane that can spread by local invasion to supra or subglottic regions
mobility impairment of vocal cords may be caused by direct invasion of tumor into thyroarytenoid muscle
what lymphatic levels are involved in supraglottic pharyn(midline rich lymphatics)
levels II, III, and IV
what lymphatic levels are involved in the glottic laryngeal cancer
rare since devoid of lymphatics but levels II, III, IV, and VI are possible
what lymphatic levels are involved in subglottic laryngeal cancer
also rare but level VI is possible
what is the most common site of mets of laryngeal cancer
lung is most common
mediastinal LN’s, bone, and liver
good prognostic indicator of laryngeal cancer
lack of LN involvement (75-95%)
depends on site, bulk, and degree of infiltration
poor prognostic indicator of laryngeal cancer
vocal cord immobility
what indicators have the highest risk of recurrence in 2-3 years
stages III and IV
close or positive surgical margins
perineural, lymphovascular or extracapsular (nodal) spread
primary tumor in oral cavity
what imaging investigations can be done to diagnose laryngeal cancer
laryngoscopy, encoscopy, barium swallow, CXR (for lung mets), CT or MRI with contrast, PET
what two types of biopsies can be used for larryngeal cancer
endoscopic or FNA
what is the most common pathology of laryngeal cancer
squamous cell carcinoma (95%)
Non-SCC: adenocarcinoma and very rare sarcomas
what are the two different subtypes of SCC laryngeal
keratinzing (HPV unrelated)
non-keratinizing (HPV related)
what are the general staging categories for laryngeal cancer
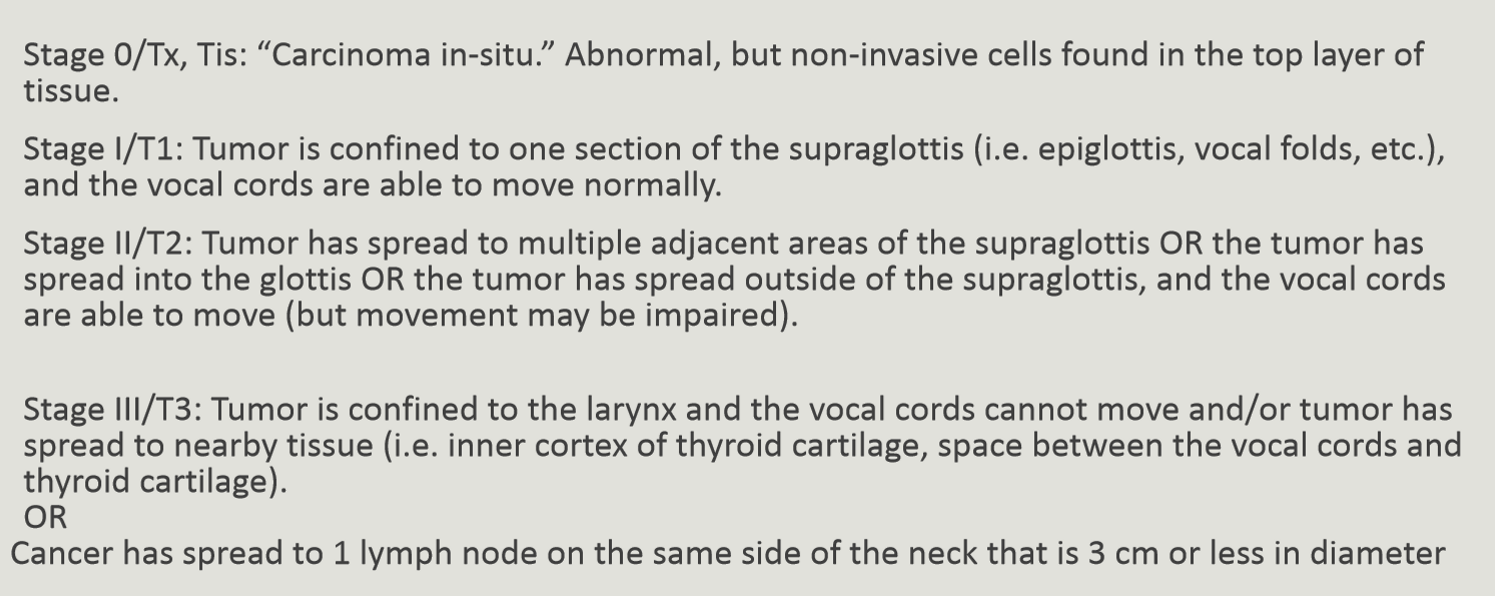
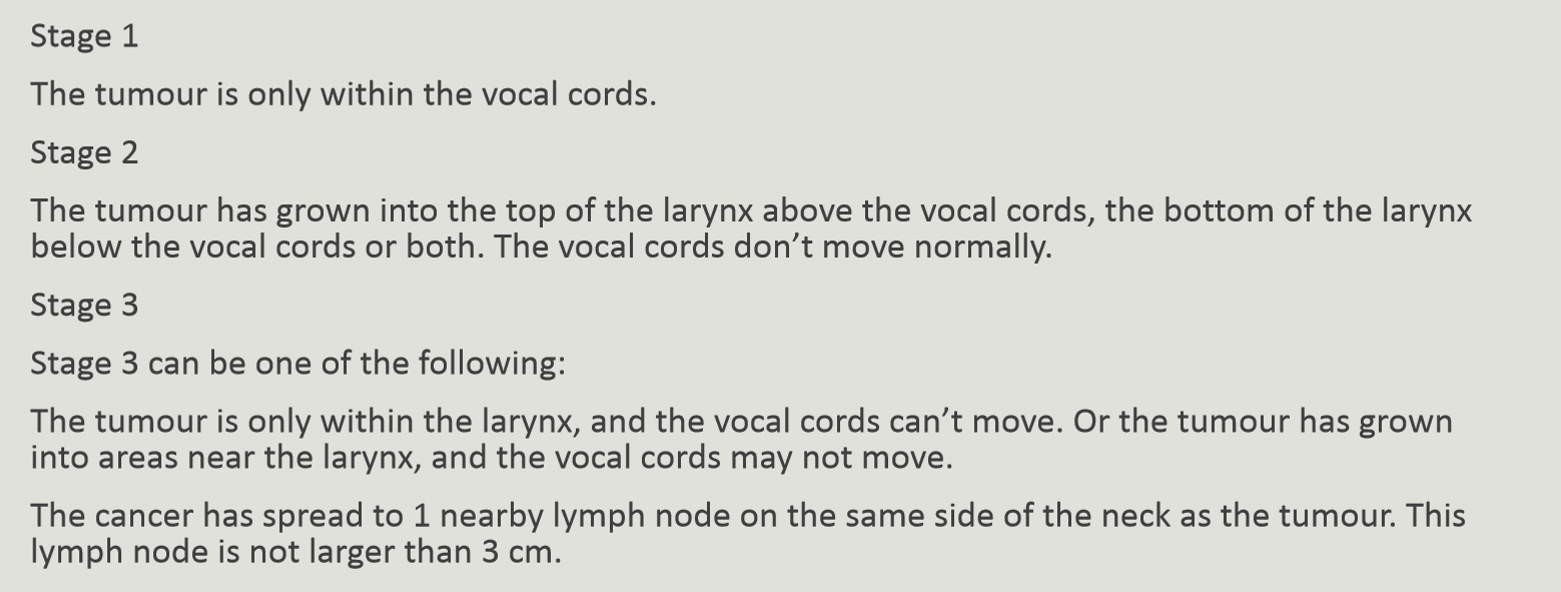
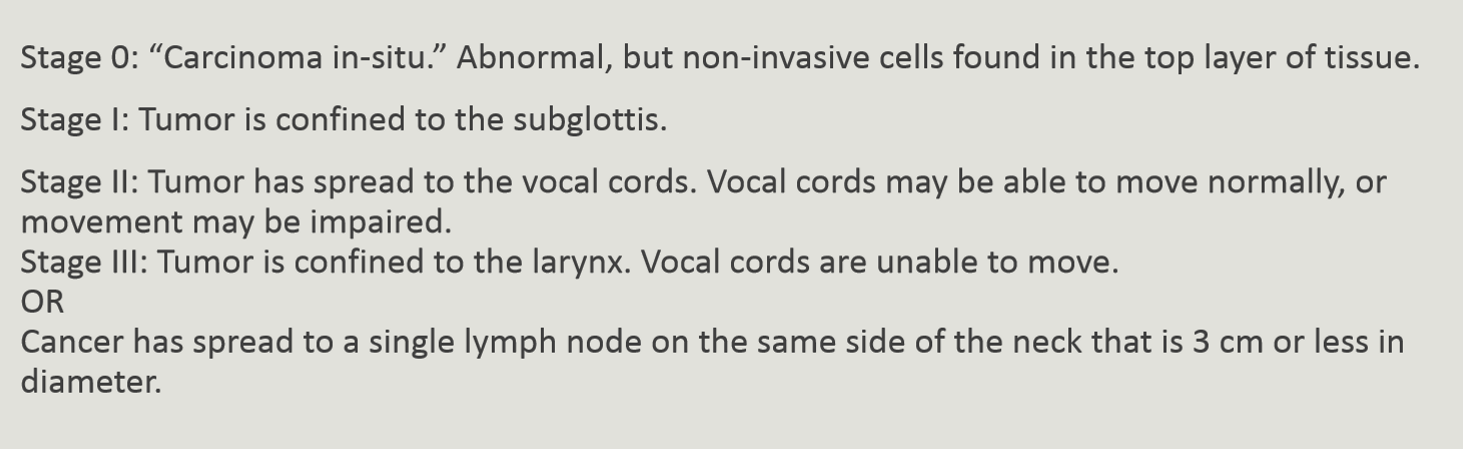
stage 0 = carcinoma in situ
early = stages 1 & 2
locally advanced = stage 3
advancec = stage 4
Staging (T) for supraglottic cancer
Staging (T) for glottic cancer
Staging (T) for subglottic cancer
Stage IV for all larynx cancers
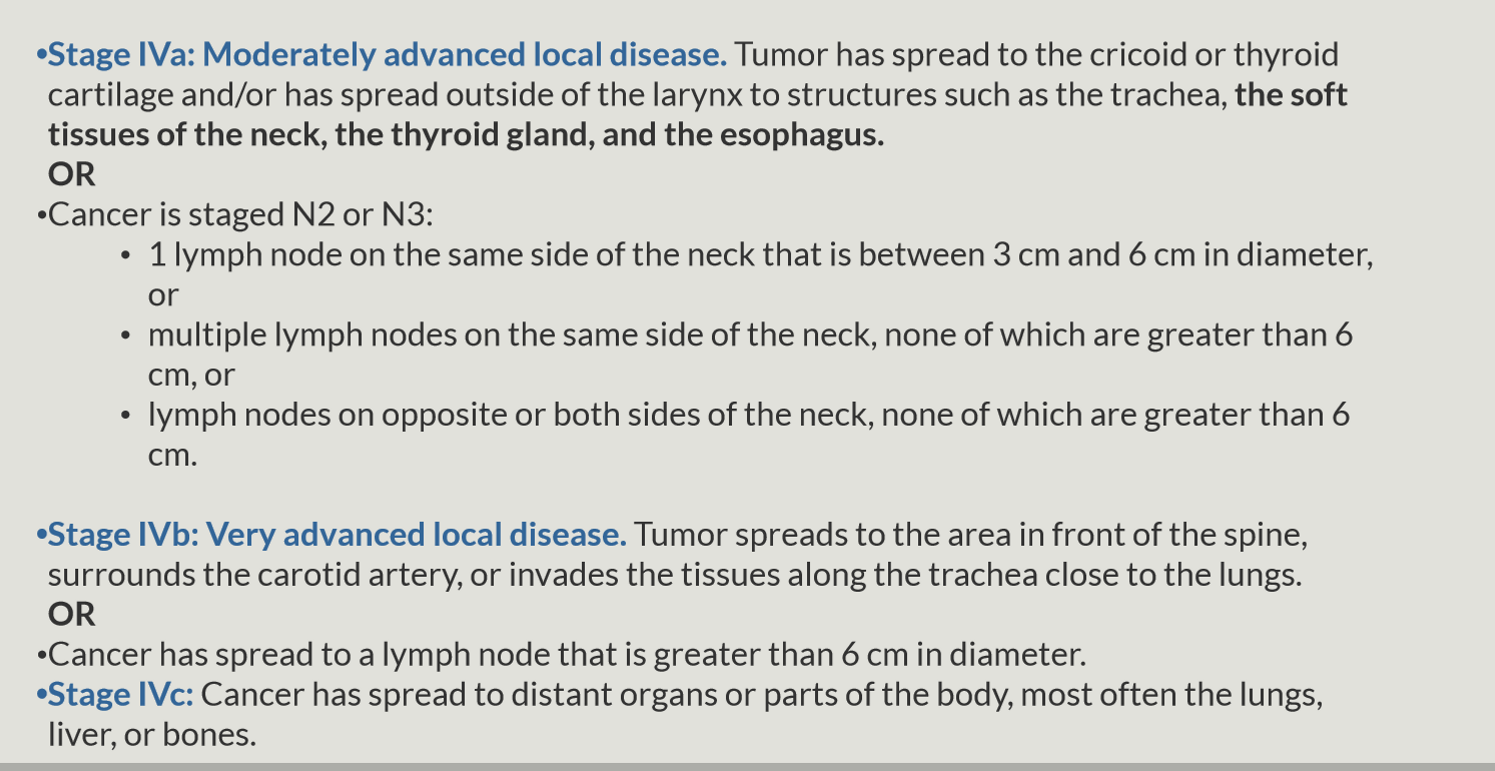
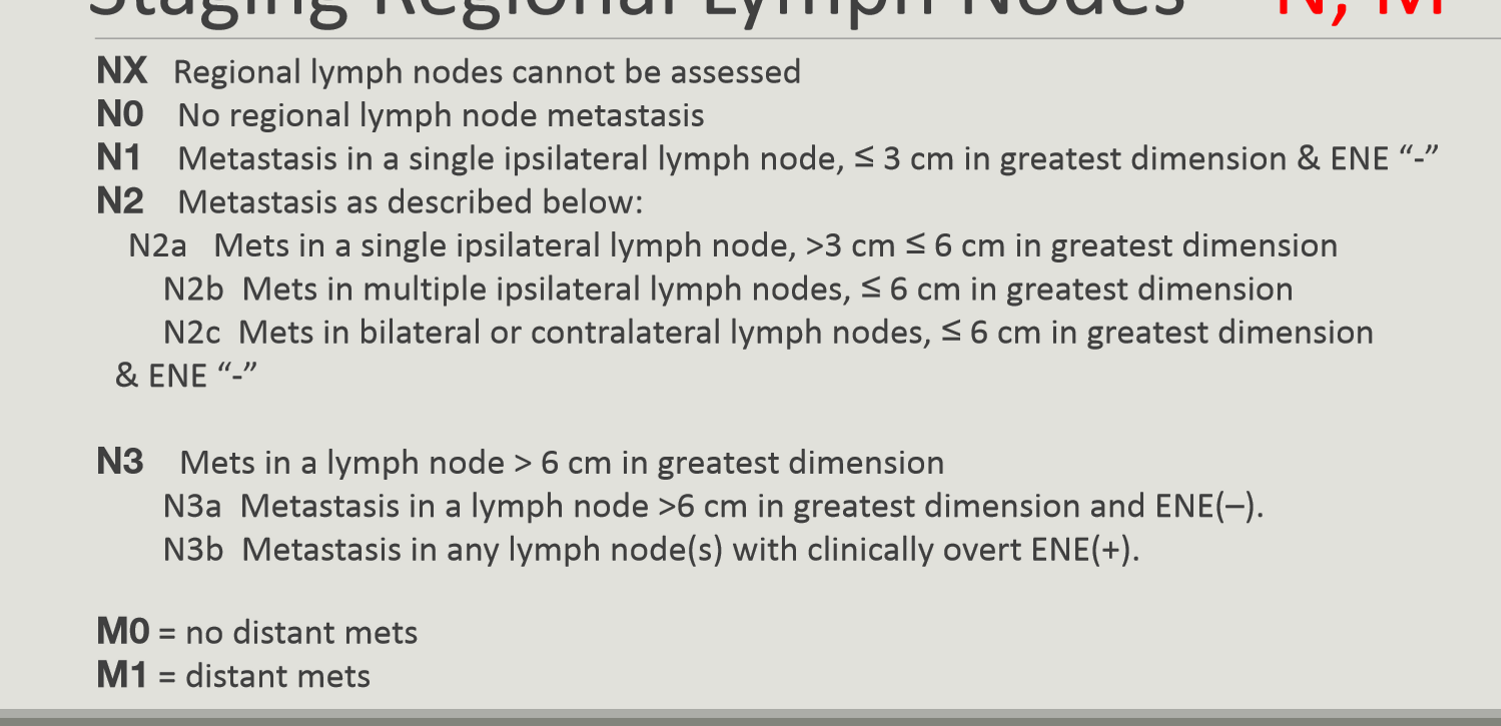
larynx cancer TNM Staging - N and M
management strategy for laryngeal cancer is dependent on what two things
LN status of neck
prescence of distant mets
what surgeries can be done for smaller early stage laryngeal tumors
laser surgery, vocal cord stripping or coredectomy
what type of surgeries can be done for larger more advanced-stage tumors
partial laryngectomy or total laryngectomy + LN dissection
why is EBRT done for laryngeal cancers
to preserve voice and allows surgery to be reserved for salvaging failures
when is PORT done for laryngeal cancers
positive margins, subglottic extension > 1 cm, cartilage, extracapsular or perineural invasion, multiple positive neck nodes
what chemos are used in the treatment of laryngeal cancer (done pretty much anytime alongside Sx or RT)
cisplatin + 5FU
what biological therapy can be used to treat laryngeal cancers alongside RT and surgery
cetuximab
EGFR inhibitor
Stage I Laryngeal cancer management
supraglottis
glottis
subglottis
supraglottis: EBRT (66-74 Gy) or laryngectomy
glottis: EBRT or Surgery (laryngectomy, laser excision, cordectomy)
subglottis: EBRT for voice preservation ± Sx
Stage II Laryngeal cancer management
supraglottis
glottis
subglottis

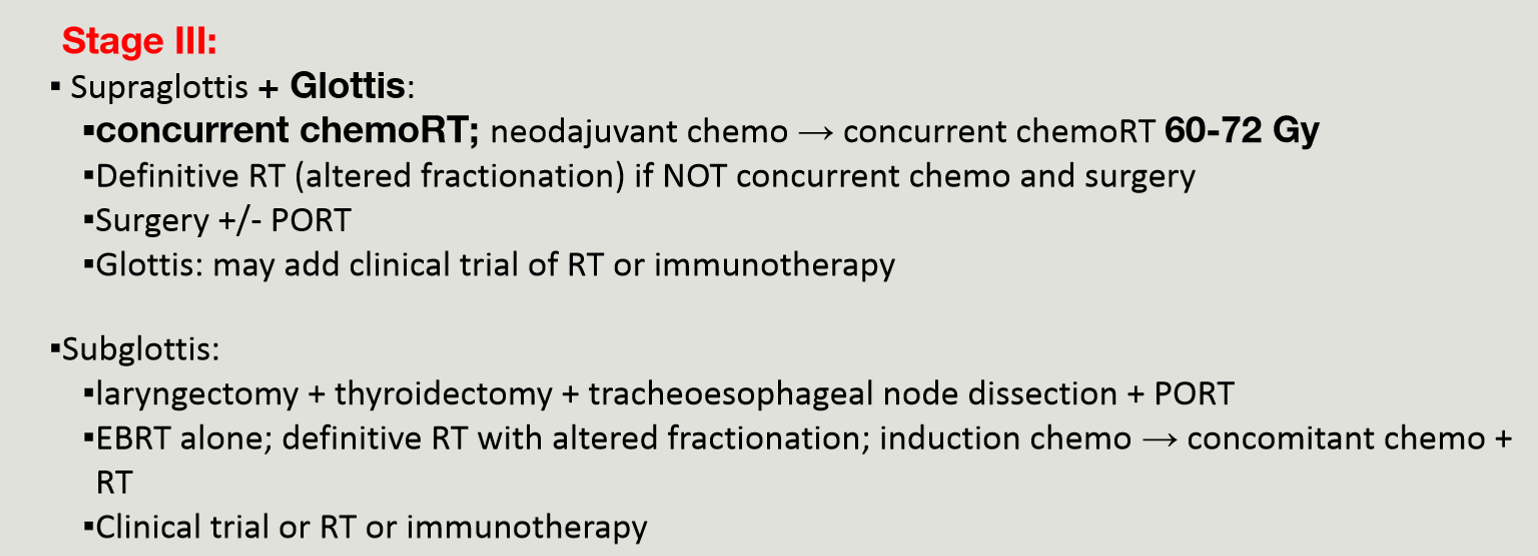
Stage III Laryngeal cancer management
supraglottis + glottis
subglottis
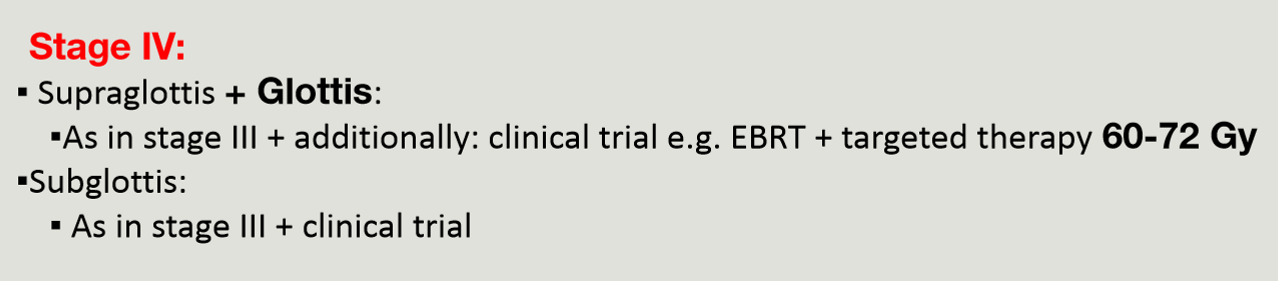
Stage IV Laryngeal cancer management
supraglottis + glottis
subglottis
what are some of the various treatments of metastatic or recurrent laryngeal cancer
Surgery ± EBRT, EBRT, chemo, immunotherapy, clinical trials
what is the mainstay of treatment for early stage glottis cancer
radiation therapy
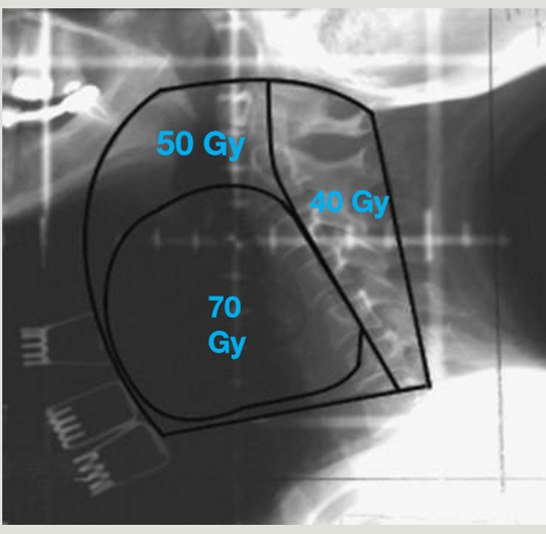
RT glottis set-up
supine on AIO board, 4-point shell, arms by sides with knee and ankle rests
RT glottis
energy
technique
collimator angle
D/F accelerated conccurent boost
D/F Post-op
6 MV
lat POP with fields centered on vocal cords (5×5 fs)
angle follows vertebral bodies
70 Gy / 35 fraction
64-60 Gy / 27-30 fraction
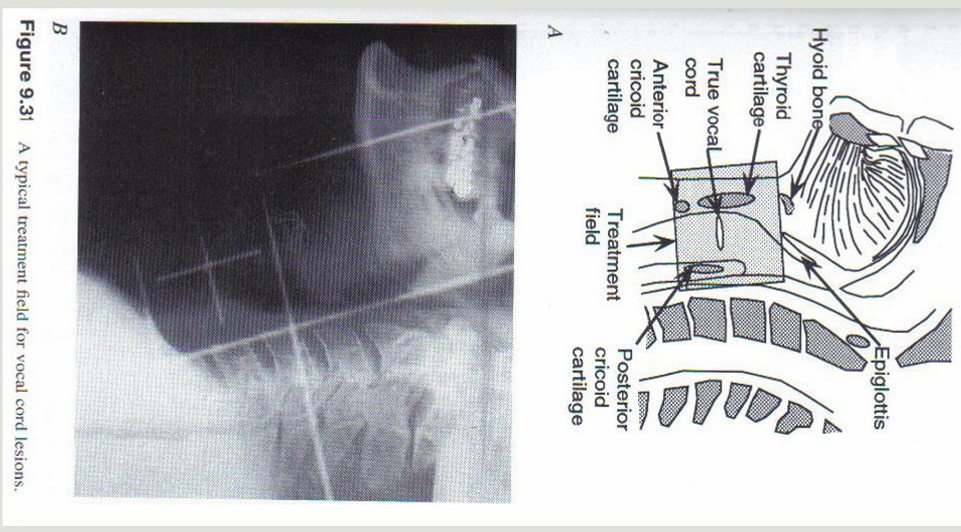
what are the sup, inf, ant, and post RT borders for glottic cancer
sup = thyroid notch or hyoid bone
inf = border of cricoid cartilage (c6)
ant = clear skin 1-1.5 cm at level of vocal cords (FLASH) + 1 cm bolus for nodal treatment
post = between ant edge and middle of vertebral body, including anterior portion of pharyngeal wall
are fieds larger for supraglottic or glottic lesions
supraglottic lesions
sup, inf, ant, post fields for supraglottic lesions
sup = extends along mandible (to include jugulodigastric and middle jugular LN’s if advanced dx)
inf = inf of cricoid cartilage
ant = clear skin surface/flash
post = spinal accessory chain / spinous process
supraglottic cancer RT
energy
technique
shielding
D/F
6 MV
IMRT, VMAT, or shrinking field conventional
shielding = trachea and spinal cord
66-70 Gy / 33-35 fractions
advantages of supraglottic cancer RT vs surgery
increased voice preservation, decreased carotid damage, better for patients with short thick necks
subglottic lesions are rare but …
very aggressive
can cause airway obstruction if advanced
with T3 laryngeal lesions, are larger or smaller fields used to treat it?
larger portals to cover level II-IV lymph nodes
dose to T3 laryngeal lesions
54-60 Gy
what is the goal of treatment of T3 lesions
larynx preservation
with T4 laryngeal lesions, are larger or smaller fields used to treat it?
larger fields than T3, to cover LN levels II-IV + VI
is larynx preservation acheivable with T4 lesions
no, it is rarely acheivable
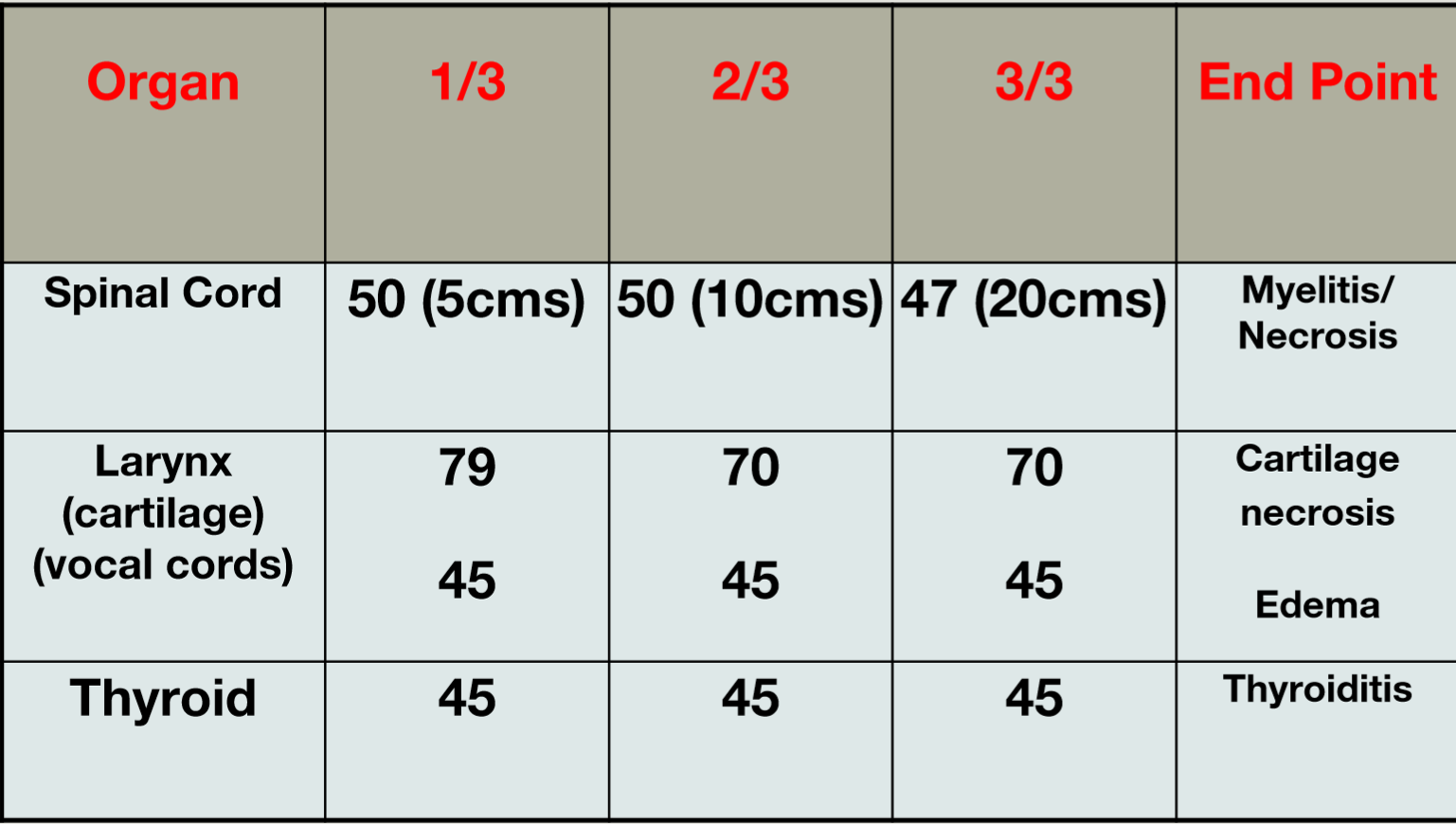
what are three organs at risk for laryngeal cancer treatment and their TD5/5 for 1/3 of the organ
spinal cord: 50 Gy for 5 cm
Vocal cords: 45 Gy
thyroid: 45 Gy
list 4 acute reactions to laryngeal RT and management of the side effects
mucositis
gargle/rinse of crushed aspirin
hoarseness
rest voice
erythema/dry desquamation/moist
skin care
dysphagia
maintain fluid and nutrition via IV, gargles
additional: ageusia, fatigue, hearing issues
what are some chronic reactions to laryngeal RT
otalgia, fetid odor, severe hemorrhage/stroke due to carotids in RT field, telangietasia, hypothyroidism, malnutrition
what rehab can be done for significant dysphagia
esophageal dialation, swallowing therapy, surgical replacement of larynx
what rehab can be done to maximize speech post laryngectomy
esophageal speech, electrolarynx, tracheoesophageal puncture
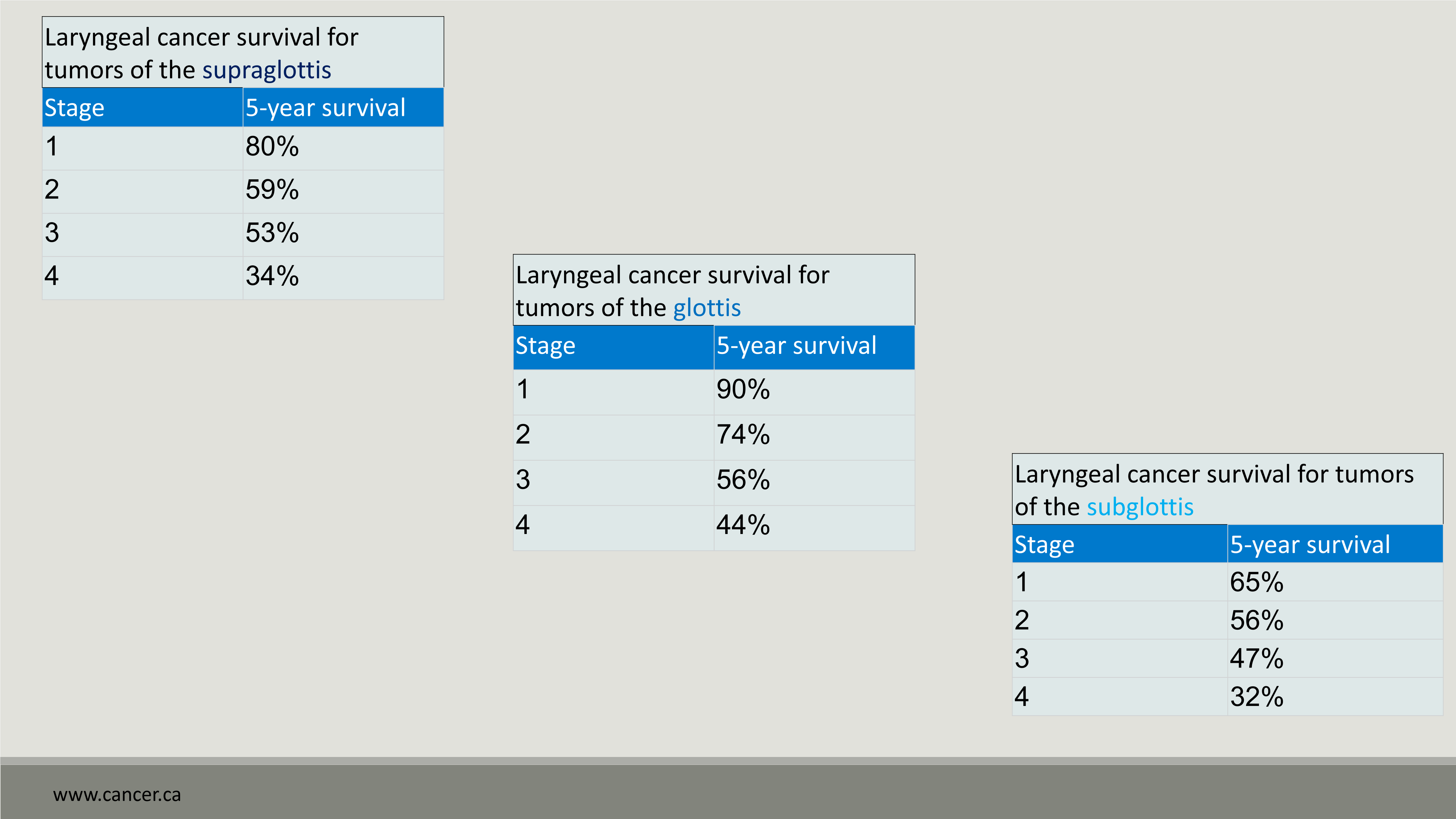
survival rates of laryngeal cancer
subglottis has the lowest 5YS while glottis has the best
hoarseness is a early common symptom in ___ cancer while it is a late symptom for ____ and _____ cancers
early: glottic
late: subglottic and supraglottic (needs to spread)
Early stage laryngeal cancer (T1-T2) is treated with …
surgery or radiation therapy
T3 laryngeal cancer is treated with …
RT ± chemo
advanced laryngeal cancer (T4) extending outside the larynx is treated with …
surgery then post-op chemoRT
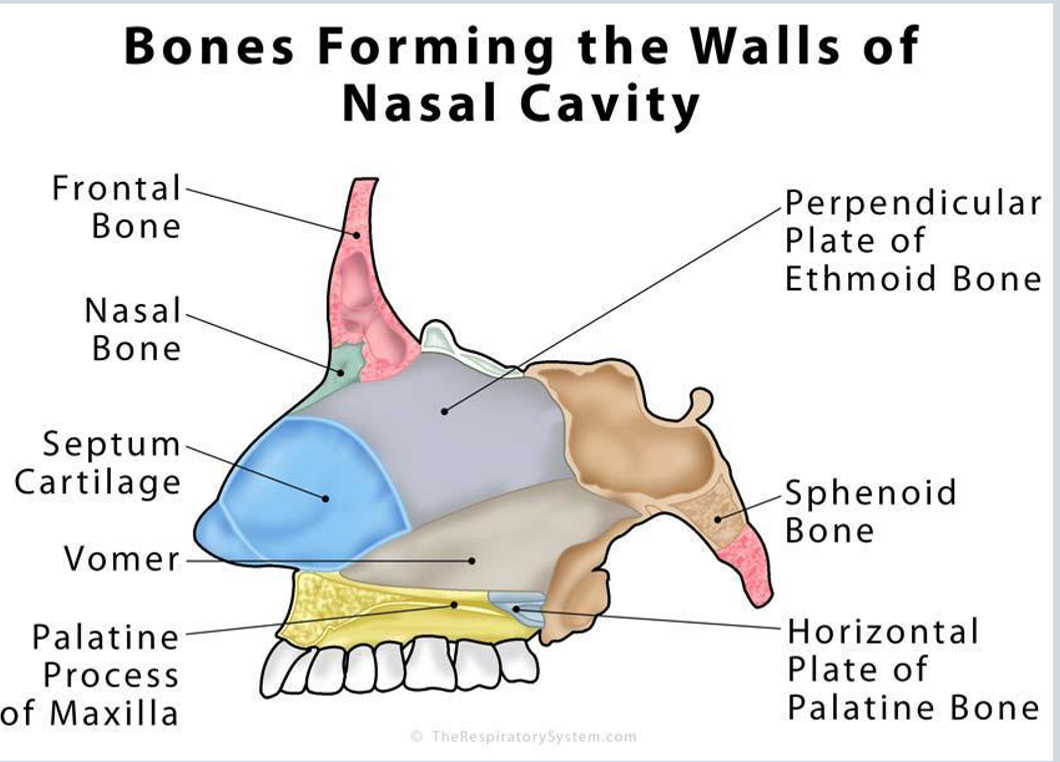
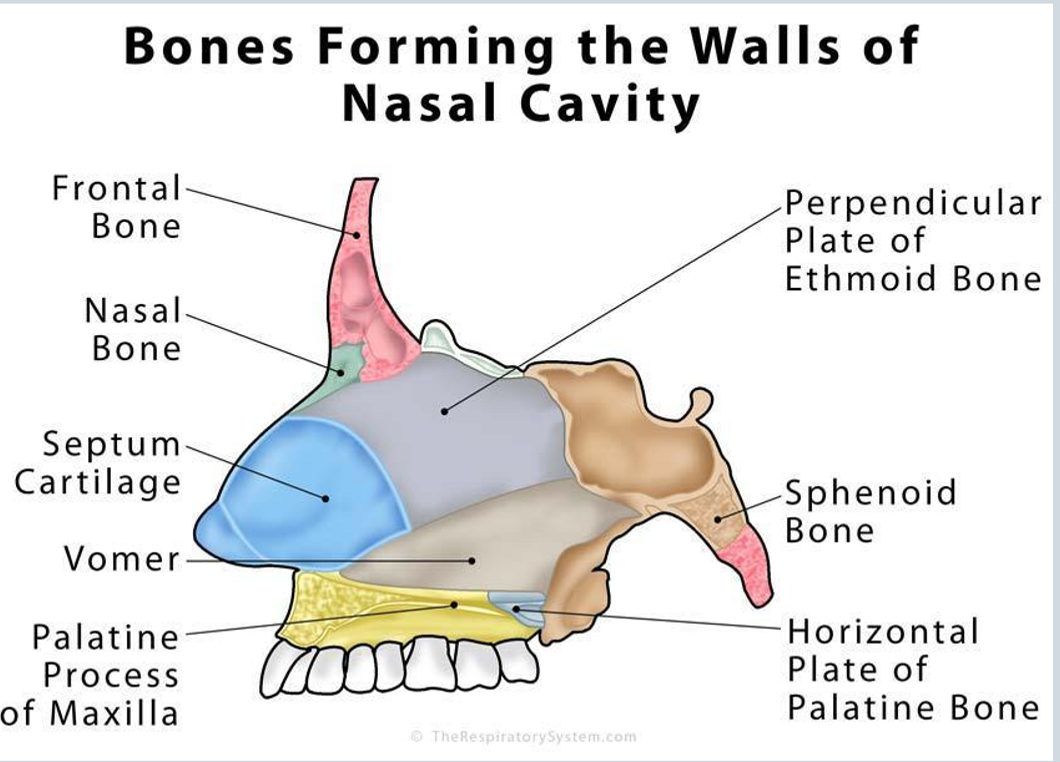
What bones form the walls of the nasal cavity?
anteriorly = frontal bone and nasal bone
posteriorly = sphenoid bone
inferiororly = vomer and palatine bone
superiorly = frontal bone
lateral = ethmoid bone
are the maxillary sinuses paired or unpaired
paired: one on each side
what type of epithleium lines the maxillary sinsues, and where to the secretions drain
the maxillary sinus is lined by pseudostratified columnar epithelium and the secretions drain into the middle nasal meatus
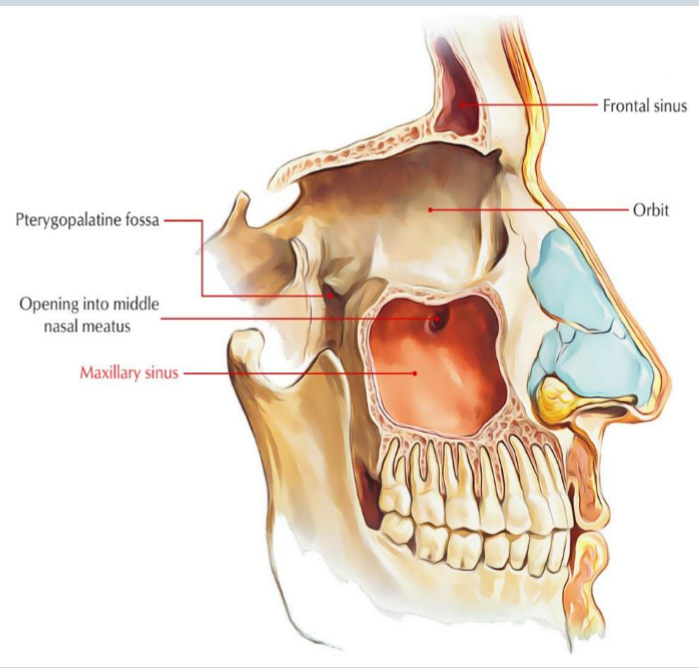
what are the sup, inf, post, and medial borders of the maxillary sinus
sup = infraorbital rim
inf = hard palate (roots of teeth penetrate cavity(
post = nasopharynx
medial = nasal wall
what are the functions of the maxillary sinus
decrease skull weight, impact resonance of voice, humidify and warm inhaled air, filter debris, immunodefensive action
nasal cavity cancer epidemiology
where to most tumors occur
where do least tumors form
M:F
age
countries where most common
uncommon cancer
most commonly in maxillary sinus or nasal cavity
least common in frontal and sphenoid sinus
M:F = 2:1
> 55
more common in south africa and japan
5 etiological factors of nasal cavity cancer
smoking
exposure to leather dust, nickel, chromium
HPV (SCC)
Epstein-Barr Virus (NHL)
RT for retinoblastoma
describe the natural history of nasal cavity cancers
most lesions are advanced on presentation and have ability to invade into the orbit from the maxillary sinus
rare nodal involvement and hematogenous spread
how does cancer get from ethmoid sinus get into the cranial fossa
through the orbit and into the cribriform to get into the cranial fossa
what are the two categories of maxillary sinus cancer
suprastructure tumors
nasal cavity, ethmoid cells, orbit, infratemporal fossa, base of skull
poor prognosis as it can invade into skull
infrastructure tumors
palate, alveolar process, gingivobuccal sulcus, soft tissue of cheek, nasal cavity
lymphatic spread from maxillary sinus cancer is rare, but what nodes would if go to first?
subdigastric and submandibular nodes
lymphatic spread from ethmoid and frontal sinus cancer would go to …
submaxillary nodes
lymphatic spread from sphenoid sinus cancer would go to …
jugulodigastric nodes
lymphatic spread from lesions involving oral cavity and cheek would go to …
submandibuar and upper jugular nodes
lymphatic spread from lesions involving nasal cavity and nasopharynx would go to …
retropharyngeal and upper jugular nodes
is hematogenous spread common for maxillary sinus cancer
no
early and advanced presentation of nasal vestibule cancer
early: asymptomatic plaques or nodules (crusting and scabbing)
advanced: pain, bleeding, ulceration
early and advanced presentation of nasal cavity cancer
early: chronic unilateral discharge, ulcer, obstruction, headache
advanced: proptosis, expansion nasal bridge, diplopia, anosmia
presentation of ethmoid sinus cancer
central or facial headaches, referred pain to nasal region, proptosis, diplopia
early and advanced presentation of maxillary sinus cancer
early: vague, mimics sinusitis or inflammation
advanced: facial swelling, epistaxis, orbital pain, unhealed tooth socket
early and advanced presentation of sphenoid sinus cancer
early: vague headache
advanced: CN III, IV, V, VI neuropathy
what imaging tests can be done to diagnose nasal cavity/sinus cancers
CT (cortical bone erosion through cribriform plate)
MR (direct intracranial/leptomeningeal spread)
PET or bone scan
what biopsy is done to diagnose nasal cavity/sinus cancer
transnasal biopsy paired with a fiber optic nasal endoscopy
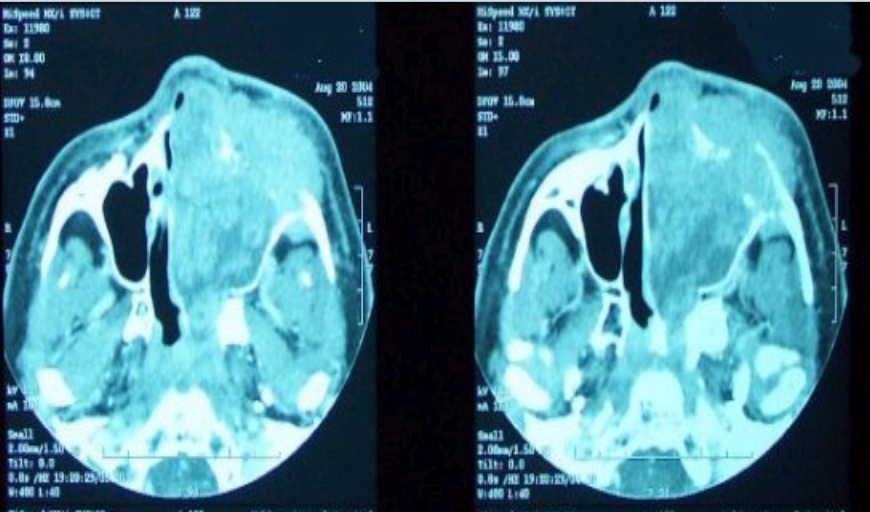
what would be the diagnosis from this scan
left paranasal sinus invaded with tumor
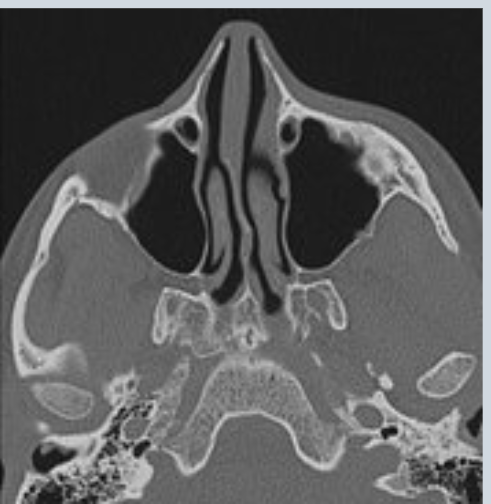
what would be the diagnosis from this scan
right maxillary bone has been fractured/destroyed by a tumor
three patient prognostic indicators of cancer of nasal cavity/sinus
age (younger is better)
sex (female has better prognosis)
performance status (higher is better)
4 disease prognostic indicators of nasal cavity/sinus cancer
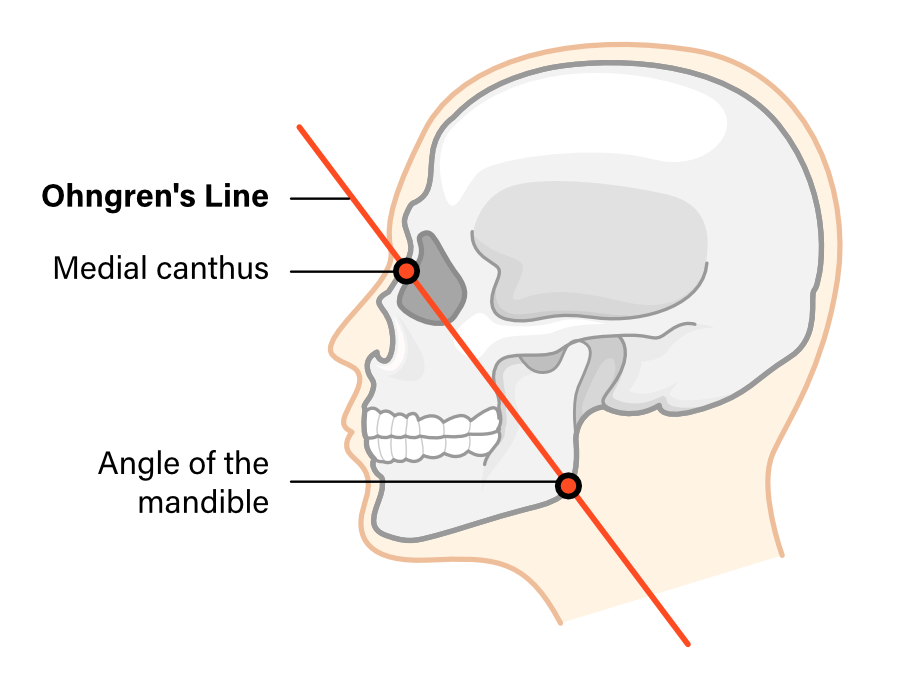
location (below Ohngren’s line is better, higher in skull is worse)
histology
locoregional extent
perineural
what do most patients die of from when diagnosied with nasal cavity/sinus cancer
direct extension into vital skull areas
what is the most common pathology of nasal cavity/sinus cancers
squamous cell carcinomas (70-80%)
three lesser pathologies of maxillary antrum cancers
adenocarcinomas
melanoma
sarcoma
three lesser pathologies of nasal cavity/sinus cancers
salivary gland
lymphomas
some osteogenic sarcomas
maxillary sinus TNM staging - T
Tx: primary tumor cannot be assessed
Tis: carcinoma in situ
T1: Mucosa
T2: Bone erosion/destruction, hard palate, middle nasal meatus
T3: Posterior bony wall maxillary sinus, subcutaneous tissues, floor/medial wall of orbit, pterygoid fossa, ethmoid sinus
T4a: moderately advanced local dx: (Anterior orbit, cheek skin, pterygoid plates, infratemporal fossa, cribriform plate, sphenoid/frontal sinus)
T4b: very advanced local dx (Orbital apex, dura, brain, middle cranial fossa, cranial nerves other than V2, nasopharynx, clivus)
Nasal cavity / ethmoid sinus cancer TNM staging - T
Tx: primary tumor cannot be assessed
Tis: carcinoma in situ
T1: One subsite +/- bony invasion
T2: Two subsites or adjacent nasoethmoidal site
T3: Medial wall/floor orbit, maxillary sinus, palate, cribriform plate
T4a: moderately advanced local dx (Anterior orbit, skin of nose/cheek, anterior cranial fossa (minimal), pterygoid plates, sphenoid/frontal sinuses)
T4b: very advanced local dx (Orbital apex, dura, brain, middle cranial fossa, cranial nerves other than V2, nasopharynx, clivus)