Female Reproductive Processes
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
46 Terms
Preantral | Primordial Follicle
primary oocyte + simple squamous follicular cells
present before birth
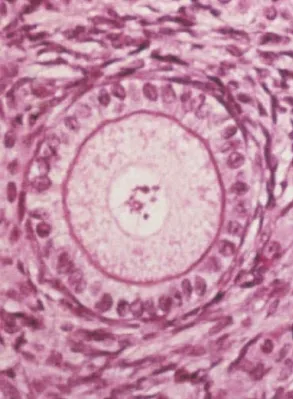
Preantral | Primary Follicle
primary oocyte + simple cuboidal granulosa cells
zona pellucida forms between the primary oocyte and granulosa cells
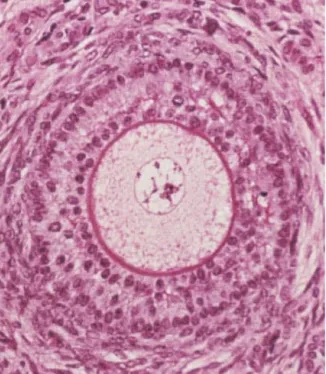
Preantral | Secondary Follicle
primary oocyte + stratified cuboidal granulosa cells
granulosa cells now hormone sensitive and therefore can be recruited by FSH
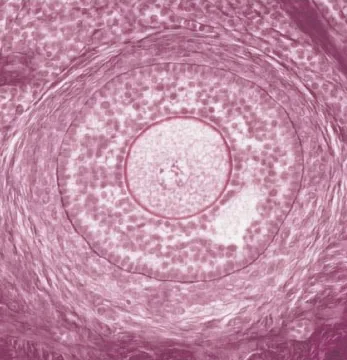
Preantral | Late Secondary Follicle
primary oocyte
fluid appears between granulosa cells
thecal cells form at periphery
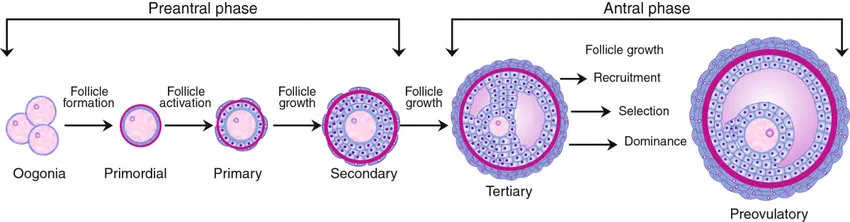
Antral | Vesicular (Teritary) Follicle
central fluid-filled cavity (antrum) forms
innermost granulosa cells attach to zona pellucida to form the corona radiata
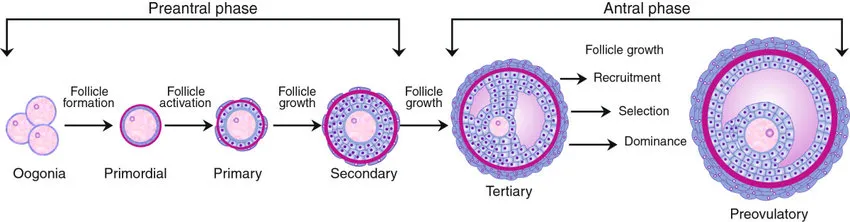
Antral | Mature Vesicular (Graafian) Follicle
oocyte isolated with surrounding corona radiata
primary oocyte completes meiosis I → secondary oocyte and 1st polar body
2.5cm in size
Luteal Phase | Corpus Luteum
post ovulatory luteinised follicle
Luteal Phase | Corpuse Albicans
scar tissue remnant of corpus luteum
why does follicular atresia begin halfway through gestation?
primordial follicles present before birth spontaneously activate and develop to the secondary follicles stage but undergo atresia as further growth is dependent on gonadotrophins, which are absent until puberty
at puberty, pulsatile hypothalamic GnRH elevates LH + FSH levels, allowing further follicular growth as part of the menstrual cycle
The Stages of The Ovarian Cycle | follicular phase
FSH recruits a small cohort of secondary follicles for further growth
when thecal cells form in late secondary follicles, growth is accelerated by FSH + LH
LH acts on theca cells to produce androgens, FSH acts on granulosa cells to convert the androgens to estrogens
increasing estrogen and inhibin decrease FSH by negative feedback as follicles grow
follicle selection and atresia results in the maturation of 1 dominant follicle
ovulation
Fun Fact → Large Follicle has the most FSH receptors and this is known as the Dominant Follicle
To help follicles mature for ovulation
Steps of Ovulation
elevated estrogen from the dominant follicle initiates an LH surge by positive feedback
the LH surge stimulates the resumption of meiosis I in the primary oocyte, forming a secondary oocyte arrested in metaphase II, and final follicle growth and weakening of the follicle wall
the follicle ruptures to release the secondary oocyte and corona radiata
estrogen levels decline
Occurs at day 14 of menstral cycle | but the whole process takes place between day 10 and day 14.
what do prostaglandins promote during ovulation?
increased pressure via inducing muscle contraction and increased ovarian blood flow
what enzyme breaks the follicular wall?
collagenase
The Stages of The Ovarian Cycle | The Luteal Phase
It is the post-ovulatory formation then regression of the corpus luteum
after ovulation, LH stimulates granulosa and theca cells of the ruptured follicle to differentiate into large and small luteal cells respectively, forming the corpus luteum
luteinised granulosa cells secrete more progesterone than estrogen; progesterone decreases FSH and LH via negative feedback to pause folliculogenesis
luteinised granulosa cells also inhibit FSH by inhibin
estrogen declines, and progesterone becomes the dominant hormone
rising progesterone signal that ovulation has occurred and makes the endometrium receptive to the implantation of a fertilised gamete
how many days of the menstrual cycle for the Luteal Phase
Day 15- Day 28
Luteal Phase | Pregnant Cycle
sustained by hCG (LH-like), secreted from syncytiotrophoblasts starting 6-8 days after fertilisation and lasting for 8-12 weeks until placentation completes
continues producing progesterone to pause folliculogenesis
Luteal Phase | Non-Pregnant Cycle
Corpus Luteum degenerates 10 days after ovulation (self-limiting)
decreased progesterone ∴ folliculogenesis resumes in next menstrual cycle
eventually forms a residual scar on the ovary called corpus albicans
why don't all the follicles die when FSH dips?
primordial and primary follicles grow independent of FSH (hormone insensitive)
what causes the peak of LH on about day 14 of the cycle?
switch from negative to positive feedback by sustained and elevated estrogen (surge centre)
what is the function of elevated FSH around day 5 of the cycle?
recruitment/ stimulation of secondary follicle growth right after menstruation
what causes the FSH peak on day 14? functions? why is it lower than LH?
Caused by : surge of GnRH caused by sustained elevated estrogen
Function: burst of follicle growth
It is lower than LH because: elevated inhibin partially suppresses FSH
what are the 3 layers of the uterus?
endometrium (inner lining)
myometrium (muscular layer)
perimetrium (outer serous layer)
what are the functions of each stratum of the endometrium?
stratum functionalis supports implantation/ shedding during menstruation
stratum basalis rebuilds the functional layer
what is the purpose of the uterine cycle?
prepare the uterus to receive the fertilised egg after ovulation (receptive to implantation and able to support developing embryo during pregnancy)
Uterine Cycle | Menstural Phase
Day 1 - Day 5
shedding of the old functional endometrium layer
CL regresses into the corpus albicans, estrogen and progesterone decrease
when progesterone reaches its lowest level, the spiral arteries constrict and spasm (starving the endometrium of oxygen, nutrients, and hormones)
the degenerating functional layer fragments and sloughs-off as menstrual flow
Uterine Cycle | Proliferative Phase
Day 6 - Day 14
rebuilding of the functional layer
high estrogen levels stimulate thickening of the endometrium, growth of endometrial glands, and the emergence of spiral arteries and progesterone receptors
arcuate arteries in the myometrium develop branches in the endometrium
cervical mucus thins (more hospitable to sperm)
Uterine Cycle | Secretory Phase
Day 15 to Day 28
enrichment of blood supply and nutrient secretion by endometrial glands
cervical mucus thickens to form the cervical plug
progesterone binds to receptors and and stimulates the endometrial glands to produce more secretions (prepare the uterus for potential pregnancy)
Spiral Arteries
support the functional layer
hormone-sensitive (constrict when estrogen and progesterone levels are low)
starves layer of O2 nutrients, and hormones → menses
Straight Arteries
support the basal layer
hormone insensitive
maintains reserve tissue
Ectopic Pregnancy | Most Common Site
Uterine Tubes
Ectopic Pregnancy | How is abdominal ectopic pregnancy possible
discontinuity between ovary and uterine tubes
Hormones | GnRH
hypothalamus → anterior pituitary
stimulates secretion of LH + FSH
Hormones | LH
stimulates secretion of androgens by theca cells
luteinisation of thecal and granulosa cells (formation of CL)
stimulates secretion of progesterone and inhibin by lutein cells
Hormones | FSH
granulosa cells
stimulates conversion of androgens to estrogens
stimulates secretion of inhibin
Hormones | Inhibin
inhibits FSH
Hormones | Progesterone
negatively regulates GnRH, LH + FSH release (pauses the menstrual cycle)
supports the endometrium in the secretory phase
stimulates primary and secondary female sex characteristics
how does the processes occurring in the ovarian cycle explain hormone fluctuations | Follicular Phase → answer with diagram on Luka Notes
day 5 FSH increase recruits/ accelerates growth of secondary follicles
granulosa cells produce estrogen
estrogen and inhibin negatively feedback on FSH, FSH dip drives follicle selection
estrogen levels rise with the growth of the dominant follicle
right before ovulation, elevated estrogen levels stimulate a massive surge of LH and FSH by positive feedback (increasing pituitary sensitivity to GnRH)
how does the processes occurring in the ovarian cycle explain hormone fluctuations | Luteal Phase → answer with diagram on Luka Notes
luteinised granulosa cells secrete progesterone (becomes predominant over estrogen)
progesterone decreases LH and FSH by negative feedback
in turn, the CL, unsupported by LH and FSH regresses, and progesterone levels decrease
Steps to oogensis
oogonium → primary oocytes (before birth) by mitosis
primary oocyte arrested in prophase I
completes meiosis I in response to LH surge → secondary oocyte and 1st polar body
secondary oocyte is arrested in metaphase II
ovulation of the secondary oocyte
completes meiosis II in response to fertilisation → ovum and 2nd polar body
Cohesion weaken with age, why is this a problem?
chromosome segregation (nondisjunction) predominantly during metaphase I
increase in aneuploidy with increasing maternal age
How long can oocytes be kept in meiotic arrest?
50 years
meiosis I begins at [time of life] but cells are arrested in [phase]?
at birth
prophase I
at what time of life do oocytes continue meiosis? why then?
puberty
LH surge (in ovulation)
oocytes are arrested again, in what stage? and for how long?
metaphase II
until fertilisation
Theca Cells
Have LH Receptors
Produce Androgens
Granulosa Cells
Convert Androgen into Estrogen
Receptors for FSh