HOSA- Clinical Laboratory Science - 2024-2025
1/468
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
469 Terms
What are the education requirements to be a Medical Laboratory Scientist?(MLS)
- Generally have a 4-year baccalaureate degree and completed a clinical training in a medical laboratory scientist program from an accredited program by the NAACLS
-Passed national examinations to be certified (ASCP)
- Can preform bench work and hold leadership positions
What educational requirements are there to be a Medical laboratory technician? (MLT)
- 2-year associates degree and completed clinical training in medical laboratory science program. ( Also accredited by the NAACLS)
- Passed national examinations to be certified
What are the education requirements for specializing in clinical laboratory science?
All the other requirements plus additional academic work,clinical training and certification as per the specialty.
What is the NAACLS?
National Accrediting Agency for Clinical Laboratory Sciences
What is ASCP?
It is the credential agency that assures the competence of non-physician medical laboratory personnel.
What employment opportunities are there for clinical laboratory science? (9)
-Technologists
- Supervisors
- Lab directors
- Administrators
- Also can be part of product development/sales
- Part of technical service departments
-Research
- Pharmaceuticals
-Education
Where can clinical laboratory scientists work? (6)
- Hospitals
- Clinics
- Physician Offices
- The military
-Places or research and education
- Public health agencies
What are the three points of patient privacy/confidentiality?
- Patient information is confidential; only to be given to other healthcare employees to improve care
- HIPAA outlines patients guide to confidentiality
- Proper digital security measures to be in place
What is HIPAA?
Health Insurance Portability and Accountability Act of 1996
How to clinical medical laboratory professionals interact with patients? (2)
- Patients primarily contact labs via lab technicians, medial technologists or phlebotomists
- They must remain respectful and considerate and understanding of patients
What is a phlebotomist?
A trained professional in blood drawing
What can professional organizations do for clinical laboratory professionals ? (3)
-Contribute to competence of professionals
- Provide opportunities for higher education/professional growth via journals,seminars, and workshops
- Help lab professionals contribute to the wellbeing of communities
What obligations do lab professionals have to society? (3)
- Contribute to well being of community
- Comply with laws/regulations
- Encourage colleagues to meet high care standards
What obligations to lab professionals have towards their colleagues? (3)
- Help profession advancement
- Establish cooperative relationships
- Maintain honesty, reliability, integrity as well as dignity/repspect for profession.
What obligations to laboratory professionals have towards patients? (4)
- Provide high standard of service
- Use good judgment to evaluate lab tests
- Maintain patient confidentiality
- Protect patients from incompetent care
What are the main 6 credentialing agencies in Canada
- ASCP BOC
- AMT
- AAB
- AAMA
- ASPT
-NPA
What has the development of waived tests allowed?
More catagories of health professionals such as paramedics, medical assistants, phlebotomy technicians, point of care technicians and nurses to administer specific lab analyses.
What is a waived test?
A laboratory test that has been determined by CLIA to be a simple procedure that is easy to perform and has a low risk of error.
What is the AMT?
American Medical Technologists
What is AAB?
American Association of Bioanalysts
What is AAMA?
American Association of Medical Assistants
What is NPA?
National Phlebotomy Association
What is ASPT?
American Society of Phlebotomy Technicians
True or False; Lab professionals never interact with patients/do clerical tasks.
False. Some lab professionals do interact with patients or do clerical duties.
What were early laboratories like?
In the US, they were extremely basic, usually only made up of a table and microscope run by physicians.
What happened when laboratories became more popular?
It raised the need for laboratory education and standardization of terminology. This led to schools for medical technology and credentialing agencies like the National Credentialing Agency for Lab Personnel. (NCA)
How did labs begin to change after 1950?
As more efficient lab technology arose, it was possible for testing methods to be more complex. And the introduction of computers allowed increased complexity of analyses.
Why are changes continuously made to the roles of laboratory professionals?
Changes are made to reflect the needs in healthcare, new technology, and federal regulations
How have laboratory focuses shifted in the present day?
Laboratory focus has shifted to preventative medicine, with research focused on solutions that limit the need for long hospital stays
What did the NCA merge with in 2009?
The NCA merged with ASCP to form the ASCP BOC, or ASCP Board of Certification. The ASCO BOC established two catagories of lab professionals; MLS and MLT.
What was the primary way of handling infectious dieseases before the 50's?
Isolating the sick was the main form of treatment. But much has changed since then, and as knowledge about infection agents increased, methods used to control the spread and how to treat patients have evolved.
When did infectious diesease and TB hospitals begin to shut down and why?
They began shutting down in the 60's as patients were infecting/reinfecting others, leading to worse outcomes. Patients were then moved to regular hospitals but kept in isloated rooms.
How did isloation procedures evolve during the late 1900s?
Glove wearing, hand washing, disinfection, and not re-capping needles were adopted to limit the spread of diesease in hospitals. The CDC outlined isolation techniques in 1970, adapted in 1975 to increase specificty, and released guidlines for isolaing communicable dieseases in 1985.
What is the CDC?
Centers for Disease Control and Prevention
What is a communicable disease?
A disease that is spread from one host to another.
What is the Universal Precautions?
Using same infection control procedure in regards to blood specimens for ALL patients for a given procedure.

What is OSHA?
Occupational Safety and Health Administration
What was the Body Substance regulations? (BSI)
Regulations developed in 1987 that reccommened precautions for body fluids/ potentially infectious substances. Thoug at the time, some diesease transmission methoods weren't understood, like airborne transmission.
What are standard precautions? What must all patients be regarded as under them?
Are the guidelines used today that were created by the CDC to protect people from healthcare associated infections. They include aspects of all previous guidelines and are continually evolving. And all patients must be viewed as potentially infectious including mucous, membrane, organs, wounds and bodily fluids.
What do the Standard guidelines provide healthcare workers with? Where must the Standard precuations be used?
Provides vital techniques/knowledge on how to handle patients safely and appropriately, like PPE, needle safety and hand hygiene. The Standard precuations are require in allll healthcare facilities.
To whom must the exposure control handbook be accessible to?
Everyone employed at lab. The guidelines hold the safe handling practices, with OSHA guidelines being reviewed when it's written.
What must healthcare employees at risk of infection from exposure do?
They must be identified and then given extra training, including an annual one that is given about biological hazards, access to new safety manuals.
What is dialysis?
The clinical purification of blood by dialysis, as a substitute for the normal function of the kidney.
What must healthcare facilities provide employers? (4)
- Appropriate PPE
- Biohazard warning labels
- Free vaccine for anyone at risk to HPV exposure.
- instructions for specimen control
Who does at-risk healthcare workers include? What safety measures must employees be provided with?
-Engineering control to isolate them from hazards (Bench top splash shields, biohazard containers etc.)
- Training in wearing PPE
- Training in hygiene
What are work practice controls?
Controls specific to each institution that reduce the likelihood of exposure by altering the manner in which a task is performed. (Disinfection, PPE, needlestick prevention etc.)
What are the most common waterless hand antiseptics?
Alcohol based antiseptics, which can come as rises, gels and foams. They are applied to the hand and then rubbed intensely for 30 second/ until they have evaporated. (HAND SANITIZER)
What are the proper hand antisepsis actions?
While Waterless antiseptics are convenient, hand washing with anti microbial/septic sops is still necessary. (Wet hands with warm water, apply soap and rub vigorously and thoroughly including wrists, dry hands and use paper towel to turn of sink. (Should take about 40-60 secs.)
What are the safety precautions for gloves?
-Must be changed frequently
- Hand washing in between uses
- Pulled down to protect cuff/wrist
- Should be removed properly.
How should gloves be properly removed?
1. Use gloves hand to pull one outer cuff over itself.
2.while removed glove is still held I gloves hand, insert free thumb into the inner cuff of the gloves hand and pull it over itself.
NEVER TOUCH WHAT IS IN THE GLOVE
What are the proper face protection measures?
Worn when working with splashable things and aerosols
Face shield or combo of mask and goggles to be used to protect eyes nose and mouth.
How are coats/gowns used?
-Usually worn while in lab or with patients
- Fluid resistant coats/gowns are used to protect from spills, stains and contaminants.
What do Exposure Controls do?
Eliminate risks of exposure incidents, though accident do happen. (Can involve needlesticks, splashes, aerosol exposure etc.)
What will exposure plans usually recommend? (4)
Flooding exposed areas with water
Cleaning wounds with antiseptic and water
Report incident to supervisor/safety officer
Seek medical help.
Will vary based on incident
What are autoclaves?
High pressure steam equipment used to most effectively sterilize.

What is used to do sterilization in a lab?
An Autoclave
What is the difference between sterilization and disinfection?
Sterilization refers to the killing of all organisms/viruses
Disinfection refers to the reduction or elimination to organisms/viruses form inanimate objects
They do sometimes overlap
What is dilute chlorine bleach used for? What is the dilution ratio?
1:10 dilution is used for disinfection
What percentages of alcohol is used for disinfection?
70-90%
What are Iodophors and what concentration is used for disinfection?
A preparing with iodine in it as well as something to solubize it. 4.5ml/L/4.5%
What are phenols?
A type of organic chemical containing a hydroxyl, -OH, functional group directly bonded to an aromatic ring.
What are some common disinfectant solutions?
-Dilite chlorine bleach
-Ammonium compounds
- Iodophors
- Phenols
-Alcohols
What is antisepsis?
Removing pathogens from living tissue.
What are antisepsis chemicals used for?
what do they commonly include?
Used for skin clearing in general, but especially before injections, surgery and wound clearing.
they commonly include
- Alcohols
- hydrogen peroxide (h2o2)
- Triclosan
-Iodine
- Chlorhexidine
What environmental controls must be maintained in a lab?
-Air flow must be recorded/logged daily for inspection
-Humidity
-Room air exchange
- Pressure
- Temperature
Inspecting agencies include OSHA and CECE
What materials and tools are needed for solution preparation?
-A solute and a solvent and the right type of pipette
How do you change concentration of stick solution?
Dilute (add solvent) or concentrate (add solute)
What are the different types of pipettes?
Volumetric
- To transfer one specific amount of liquid
- Has a bulb and line to show volume of device
- Pipette aid or filler is required to suction up liquid
Graduated/Setological
- Pipette aid or filler required
- has volume marking and can be used for any amount of liquid within volume range
Micropipette
- For less that 1 ml
-disposable tip
What is the molarity equation?
Molarity (M) = moles of solute/liters of solution
What is molarity?
The number of moles of solute per liter of solution.
What are the 3 types of percent solutions?
- Weight/Volume (A specific weight of solute (Solid) dissolved in 100ml of solvent g/ml)
- Volume/Volume (Specific volume (Liquid) of solute mixed in volume of solvent to equal 100ml, ml/ml.)
- Weight/Weight (Specific weight of solute in a volume that totals 100ml of solution g/g)
What are the 3 main types of solutions?
-Molar
-Percent
-Normal
How do you convert grams to moles and vice versa?
Using molar mass, we can find out how many grams of each solute is equal to 1 mol. (If there is more than one molecule, add the atomic weights together to gain #g/1mol)
How do you prepare a molar solution?
The amount of solute in grams (Equal to one mol) must be dissolved in 1 L of solvent.
What is a molar solution?
A solution that contains one mole of solute in each litre of solution.
What is valency?
The number of electrons in the outer shell of an atom which are able to be used to form bonds with other atoms. (NaCL has a valency of 1 and MgCL2 has a valency of 2)
How do you gram equivalents?
gram molecular weight (how many grams in a mol) / valence
How do you make a normal solution?
The gram equivalent of solute + 1 L of solvent
How do you calculate normality?
N = gram equivalents/ L solution
What are serial dilutions?
Creating a set of solutions that decrease in concentration by the same factor each time. They are used to find the titer of the sample and there are 2 types; two-fold and compound.
What is two-fold serial dilution?
A serial solution where where each sample is diluted by a factor of 2 compared to the previous one.
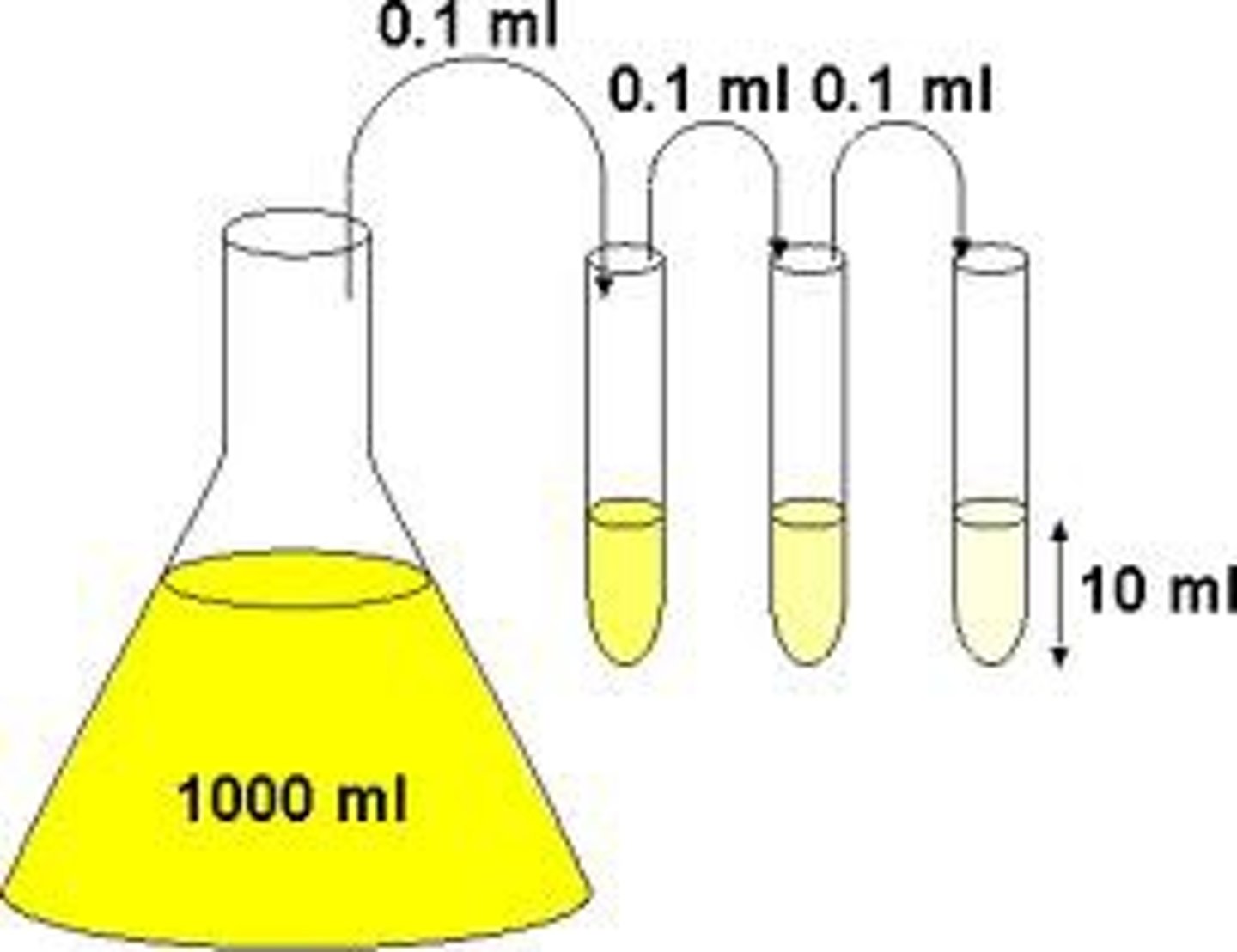
What is compound serial dilution?
If very high dilution factor is needed, each vial can have a dilution factor >2. (Usually 10)
What is a titer and how is it determined?
The lowest concentration of a sample that still gives a positive result. (Measure of reactivity) One way to determine it is serial dilution.
What is a hemostatis?
The stopping of a flow of blood to prevent too much loss of blood.
What is hematology?
Study of blood and blood forming tissues
How is blood transported through the circulatory system?
-Arteries (Strong, elastic vessels that carry blood from the heart.0
-Viens (Weak and elastic vessels that carry blood to the heart)
-Capillaries (Transistion areas between viens/arteries; connect venules and arterios (Smallest viens/arteries). They have thin walls to allow diffusion of fluids,nutrients,waste.)
What is hematopoiesis?
Blood cell formation. Happens in the blood marrow, all blood cells are derived and specialize from hematopoietic stem cells and after maturing in bone marrow, are sent into the blood stream to do their jobs. This process continues throught life.
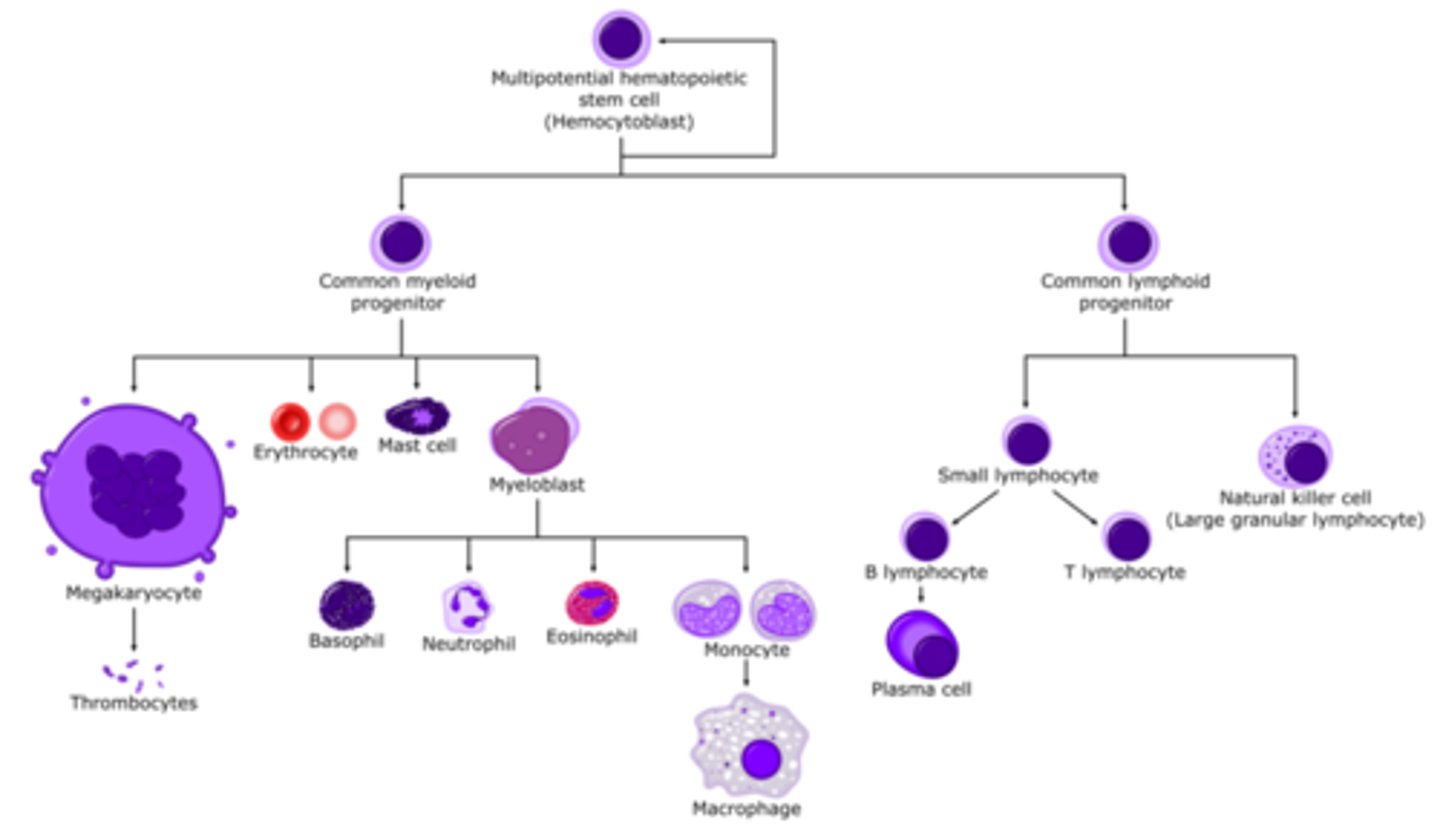
What do ___ do?
-Red blood cells
-White blood cells
-Platlets
RBC's (erythrocytes) carry oxygen using hemoglobin molecules in cells, and the blood becomes red when the oxyhemoglobin is formed from the two binding. Live for 120 days.
WBC's (leukocytes) fight infections and have verying lifespans based on the type of WBC.
Platelets are pieces of cytoplasm that play a role in homeostasis, specically blood clotting (Coagulation) they live for 10 days
What does plasma do? What is it made out of?
Plasma is very complex and can contain WBCs,platelets,proteins, lipids and carbohydrates. It dissolves all of bloods cellular parts and makes up 50-60% of blood's volume, the rest being RBCs.
What is a hematological diesease?
Hematological dieseases happen when there is a blood disorder, they can be inherited like hemophilia, a blood clotting diesease or aquired from many things such as a heart condition.
What is a CBC test?
A common laboratory test that analyses many things including cell counts, platelet counts, hematocrit (RBC to plasma) amd blood cell morphology (shape/structure/shape of cells.)
What blood specimens are used for testing?
Cepillary/venous blood samples;; chpoice of the specific specimen is based on volume needed and biiomarkers needed.
What is hemoglobin?
A protein in red blood cells that carries oxygen. Made up of globin (4 protein chains linked together) and heme groups with iron in them to help bind with oxygen.
What is and how would you preform a michrohematocrit test?
A laboratory test to determine RBC volume of patient.
A test sample is collected from a capillary puncture or from venus blood with anti-clotting and are drawn through very thin tubes (Capillary tubes) through capillary action
The tubes are balanced in the centerfuge and are spun very quickly (!0,000 RPM) for 2-4 min.
Microhematocrit readers are used to find test values and the RBC part is measured/value produced.
How do we test hemoglobin counts?
Specific gravity technique:
This is only an approximation, with a CuSO4 solution with a graviooty of 2.053 which is about the same as low-hemoglobin blood. If float, hemoglobin low, is fall through, the count is healthy.
Chemical methods:
Hemoglobin concentration can also be found chemically, like when blood is reacted with Drabkin's solution which reacts with hemoglobin to change the solutions colour when it forms cyanmethemoglobin so it can be photometrically analysed to find out hemoglobin concentration.
What are hemacytometers?
A precise microscope slide that has a counting chamber that allows you to manually count the # of cells in a sample. Usually they are glass with two counting chambers, and a coverglass needs to be placed on top to contain the sample.
How are the two counting chambers in a hemacytometer divided?
Each counting area is divided into 9 squares, the corners are divided into 16 squares usually used to count WBCs, and the central square is divided into 625 squares, with the 4 red and 1 center squares being used for RBC count. Platelet count is done in the circle.
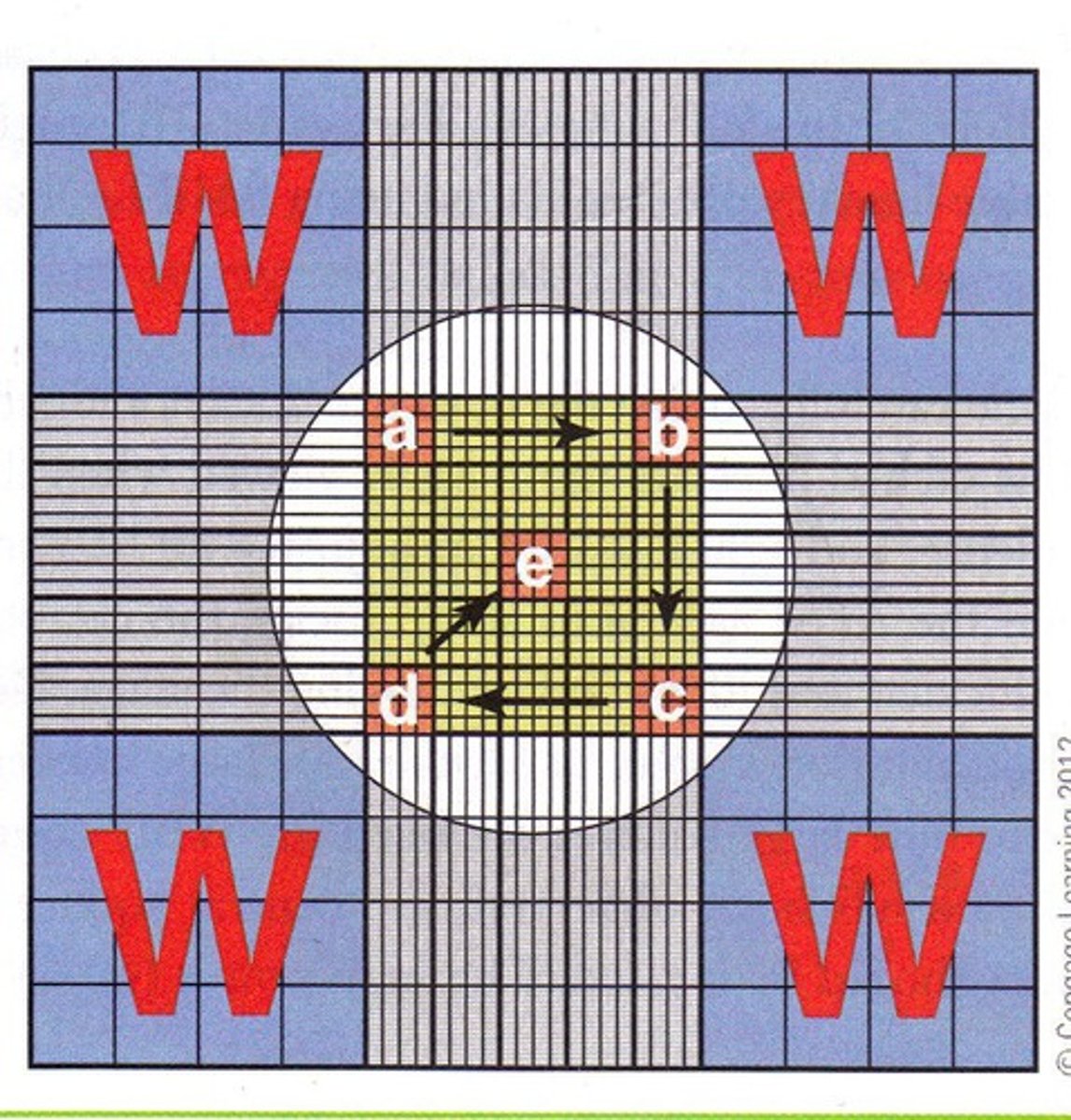
How do you use a hemacytometer? (4 steps)
Wear PPE before you start.
1. Prepare the sample. (Dilute according to type of cell.)
2. Use a micropipette to place around 10ul or 0.01 ml in a smooth/unbroken stream.
3. Count the cells using the cell coutning pattern.
4. Use cell coutning formula to find the cells/ul
How much do you dilute RBC, WBC, and platelets for hemacytometer counts?
RBC : 1:200 WBC and Platelets : 1:100 or 1:20
What is the proper cell counting pattern?
Within the boundry lines of the square you're using to count, go in a serpintine pattern starting in the top left corner.