Drugs for Anxiety Disorders
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
Objectives
1. Define Generalized Anxiety Disorder, Social Anxiety Disorder and Panic Disorder
2. Discuss putative roles of GABA and norepinephrine neurotransmission in anxiety disorders
3. Describe the probable mechanism of action and general conditions of use for antidepressants, benzodiazepines and Buspirone
4. Compare and contrast the major adverse effects of antidepressants, benzodiazepines and Buspirone
5. Discuss the reasons for low priority use of barbiturates for anxiety Anxiety
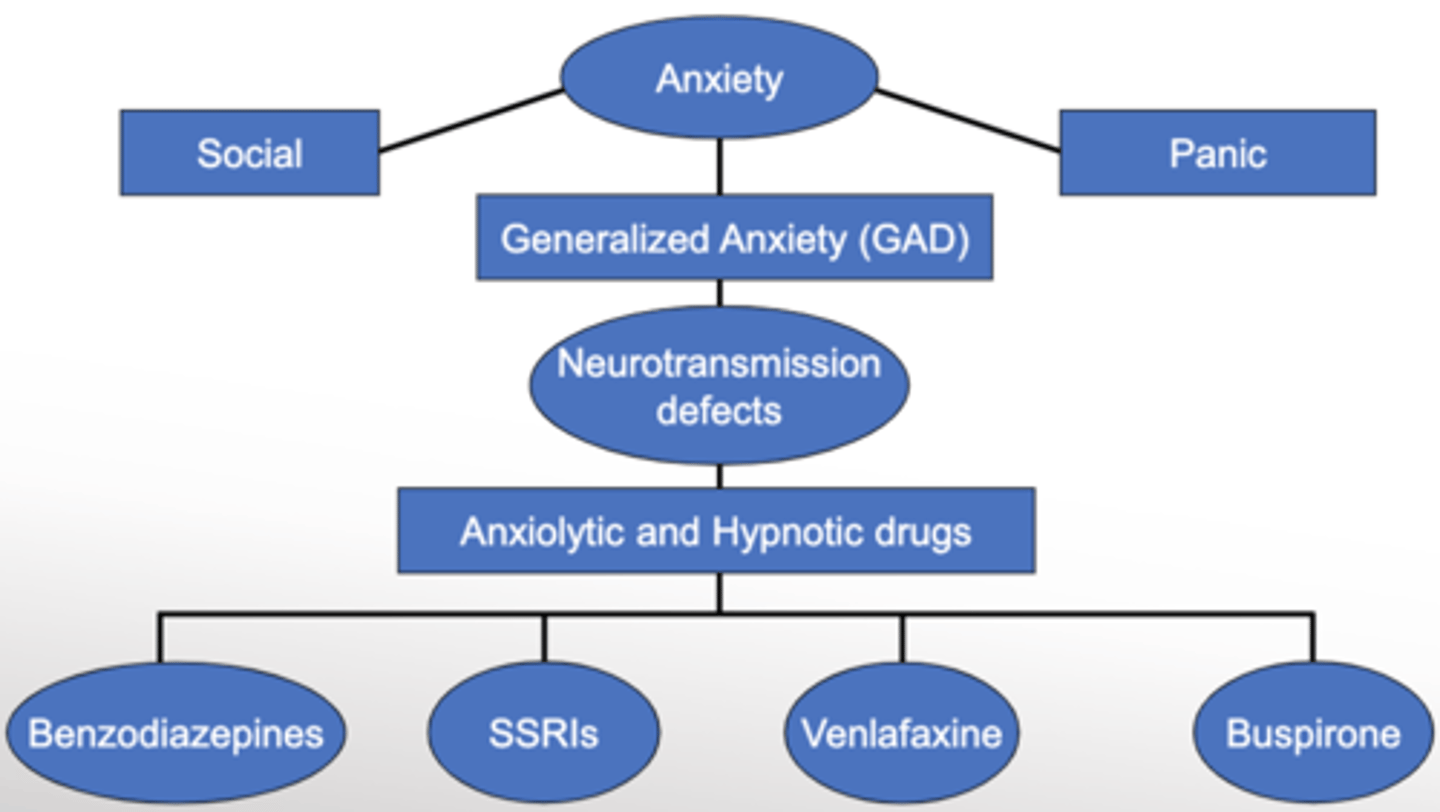
Anxiety Diagram Overview
what is anxiety?
• "Perception of real or perceived danger that threatens individual security"
What are the symptoms of anxiety?
• Debilitating psychological (think something will happen) and physiological (shortness of breath. Increased heart rate, etc) symptoms
what is anxiety disorder?
• Anxiety Disorder = persistent severe anxiety
how often is anxiety misdiagnosed?
• Often misdiagnosed ~ 23% receive proper treatment. Mistaken as physical condition a lot.
What is the prevalence of anxiety?
• One-year prevalence rate for anxiety disorders = 13% (18-54 years)
what do you know about anxiety in general?
• Often linked to other psychiatric disorders or drug abuse. Co-morbidity is high.
• Early onset
• More common in women
How is anxiety subdivided?
• Generalized Anxiety Disorder (GAD)
• Social Anxiety Disorder (SAD)
• Panic Disorder
in general, what is GAD?
• Excessive anxiety and worry about a number of events or activities
In general what is SAD?
• Intense irrational and persistent fear of being negatively evaluated or scrutinized in a social or performance situation
• Blushing, diarrhea, sweating, trembling, tachycardia
what is panic disorder?
• Spontaneous attacks of intense fear similar to life-threatening danger (~30 minutes)
• Followed by ~1 month of persistent worry about another attack
• Often with Agoraphobia
what is agoraphobia?
- the anxiety that occurs when one is in a public or crowded place, from which a potential escape is difficult, or help may not be readily available
what are the psychological and cognitive symptoms of GAD?
• Excessive anxiety
• Worries difficult to control
• Feeling "keyed up" or on edge
• Poor concentration
what are the physical symptoms of GAD?
• Restlessness
• Fatigue
• Muscle tension
• Irritability
• Sleep disturbance
NOTE: At least 3 of the symptoms must be present persistantly, that impacts functioning of life, to have GAD
who does GAD affect most?
• Most often presents in teens (pure GAD)
• Also up to 30's and 40's secondary to other anxiety disorders or other medical illness, including:
+ Heart Disease, angina, thyroid disorders, dementia, stroke, poor pain control, asthma, COPD, pneumonia
what else can cause GAD?
• Can also be drug-induced - hypothyroidism drugs, produodopa, etc
Neurochemistry - NE. How does NE influence anxiety?
• Overactive noradrenergic system originating in Locus Ceruleus
• LC projects to Vagus nerve, sympathetic ganglia, hypothalamus,
thalamus, cortex, cerebellum, amygdala
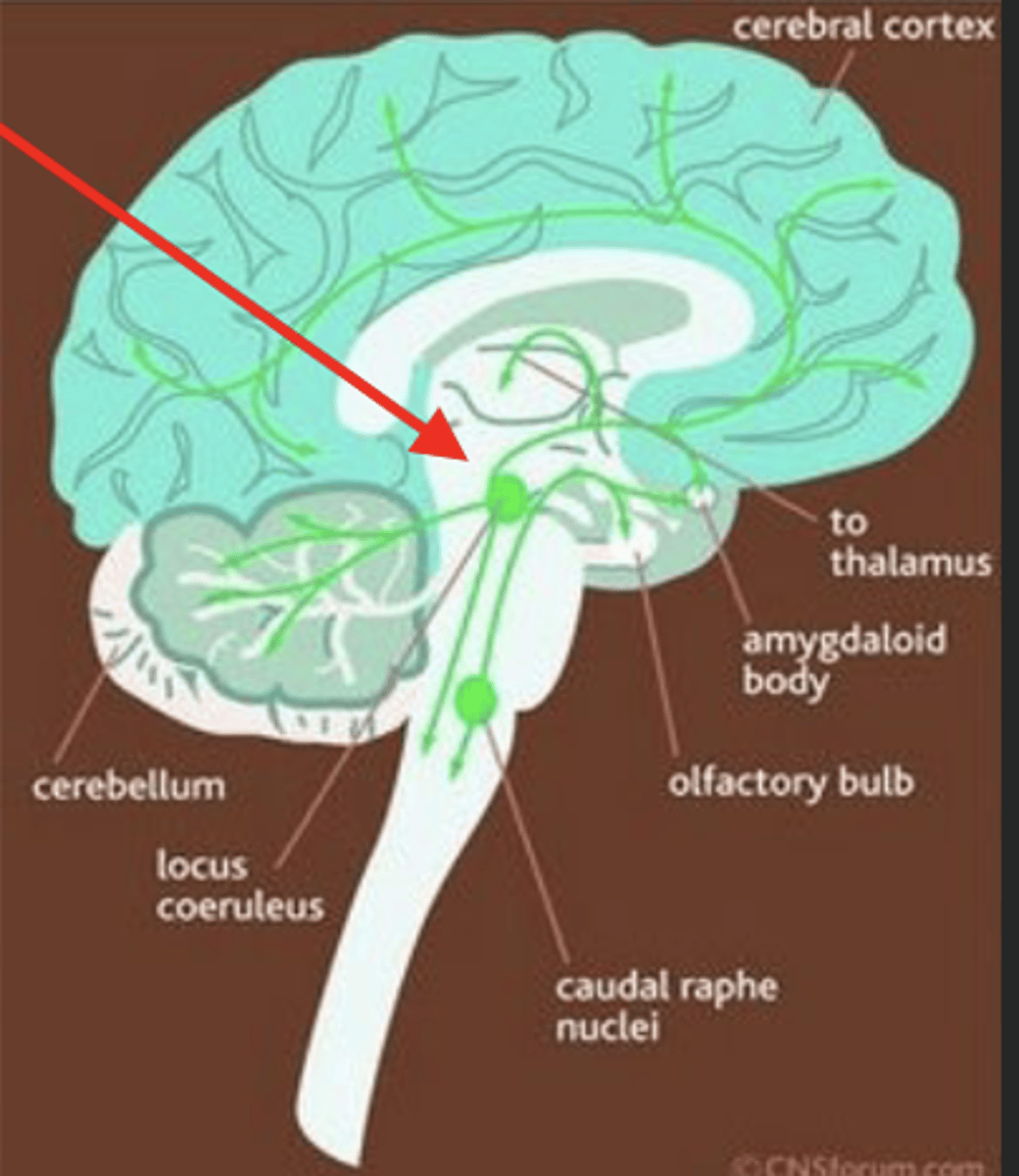
what does the Overactive noradrenergic system originating in Locus Ceruleus cause?
• Autonomic activation
• Subjective feelings of anxiety (cortex)
• CRH release (hypothalamus)
• Mood changes related to serotonin effects (Raphe Nucleus)
• Others
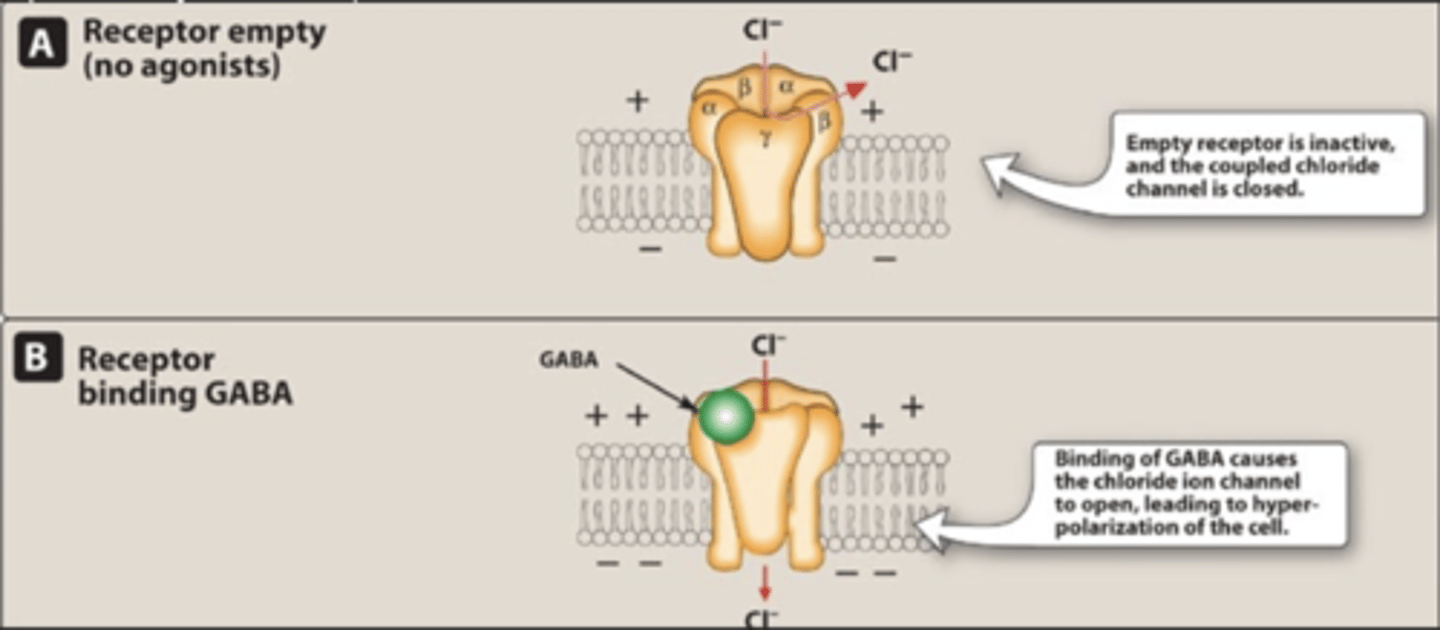
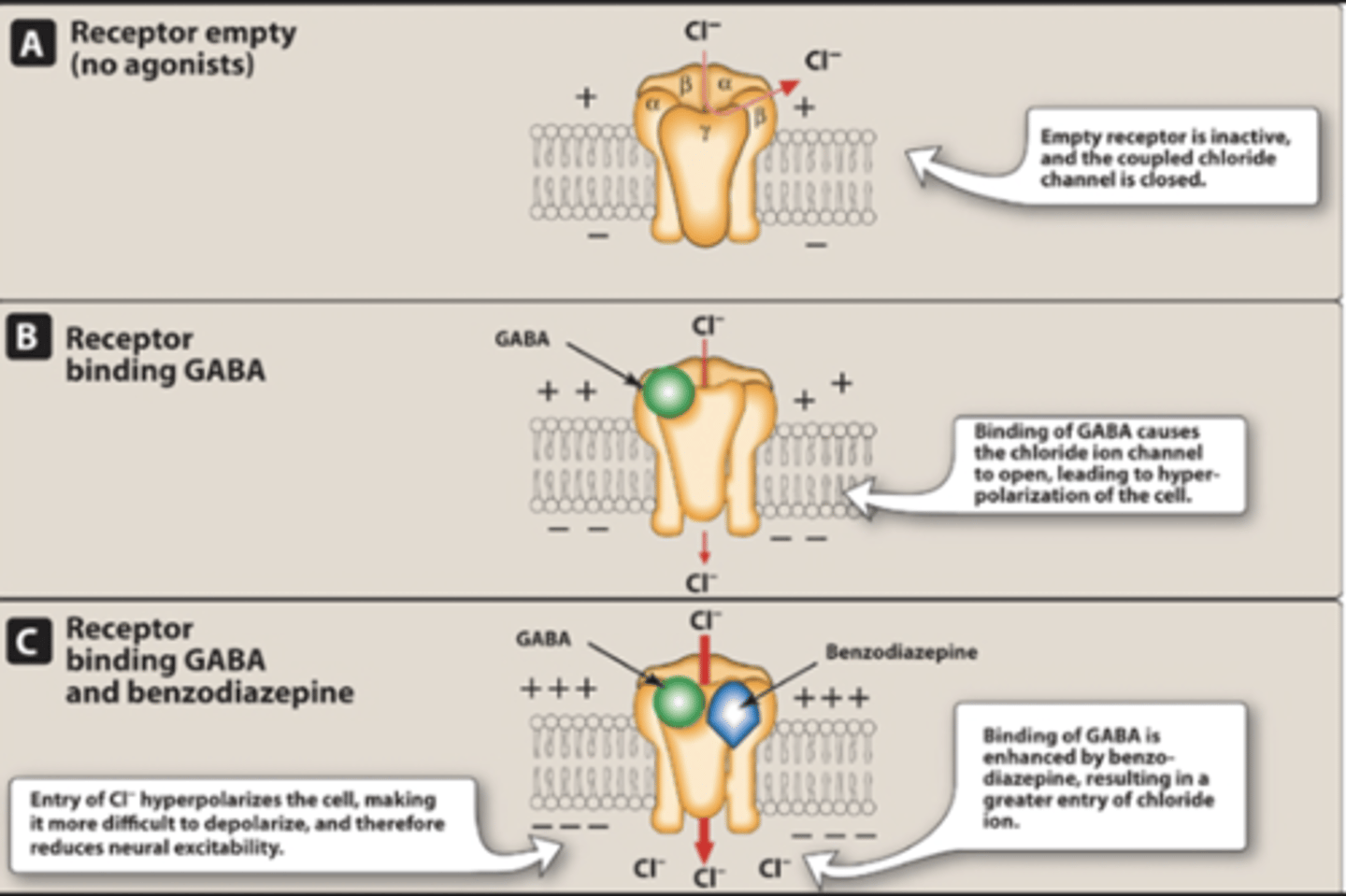
Neurochemistry - GABA. How does GABA affect anxiety?
• Anxiety associated with reduced GABAA receptors in left temporal lobe of cortex
• ↓ inhibitory GABA = ↑ excitation
what are the 2 types of GAD therapies?
non-pharmacological
pharmacological
what are the non-pharmacological GAD therapies?
• Psychoeducation
• Sort-term counselling
• Psychotherapy
• Stress Management
• Meditation
• Exercise
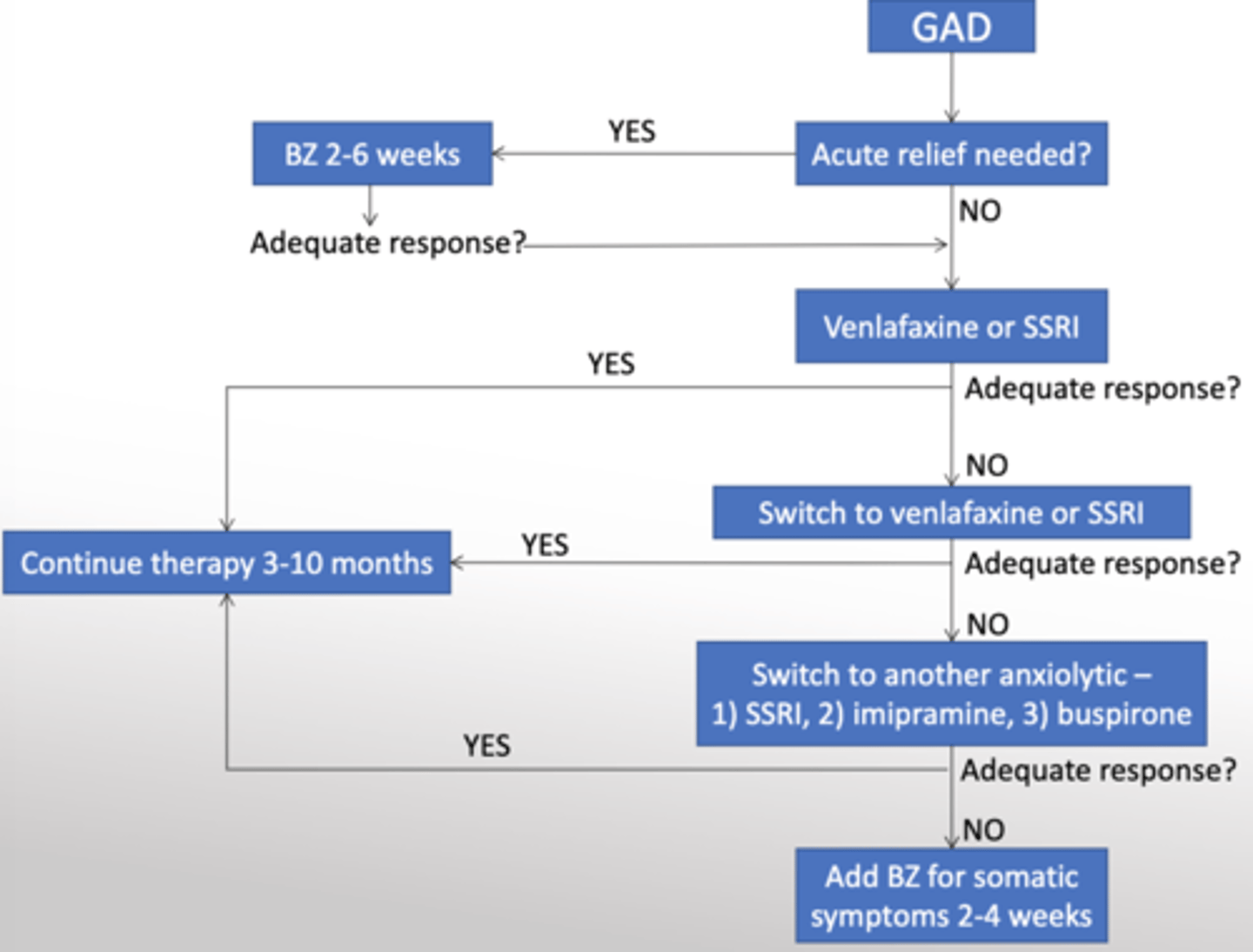
what are the pharmacological therapies for GAD?
• Benzodiazepines
• SSRI/SNRI antidepressants
• Buspirone
CNSW Depression Scale
how helpful are benzodiazepines for GAD?
• Effective in 65-75% of GAD patients within 2 weeks
• Also used as in muscular disorders, seizures and preoperatively
how are Benzodiazepines classified?
Classified by duration of action
Classified by use - anxiolytic or sedative/hypnotic
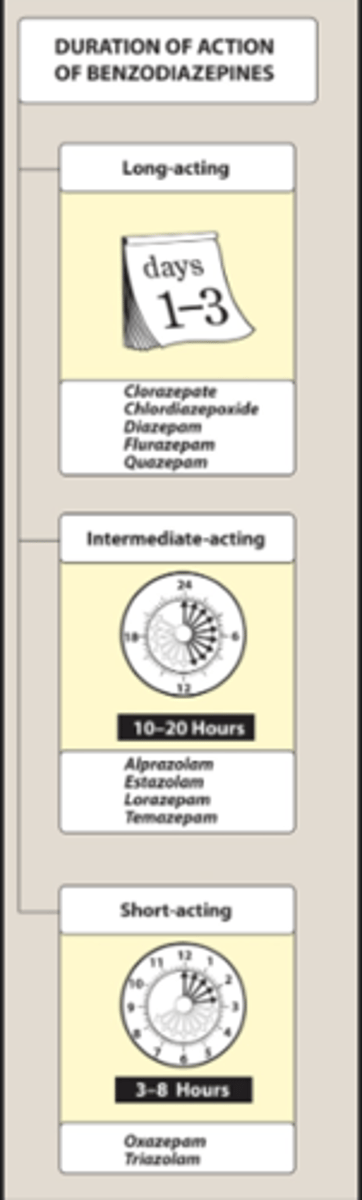
how are they classified by duration of action, and how does this impact what they are prescribed for?
• Diazepam (Valium) = long – for GAD
• Alprazolam (Xanax) = intermediate
• Oxazepam (Serax) = short – for preoperative one
how are they classified by use, and how does this impact what they are prescribed for?
• Anxiolytic - Alprazolam, Diazepam, Oxazepam and others...
• Sedative/hypnotic - Triazolam (Halcion), Temazepam(Restoril), Flurazepam (Dalmane)
How do benzodiazepines work?
+ Increase frequency of chloride channel opening
+ Hyperpolarization of membrane = reduced excitability
What are the major adverse effects of benzos?
Dependence/Tolerance
Excess CNS depression
what does excess CNS depression cause?
• Drowsiness
• Confusion
• Ataxia (motor incoordination)
• Cognitive impairment at higher doses
what is tolerance?
• Tolerance = increasing dosage requirement for constant efficacy
what is withdrawl syndrome and what impacts its severity?
• Withdrawl Syndrome = Confusion, rebound anxiety, agitation, restlessness, insomnia and tension after abrupt withdrawl
• Withdrawl severity varies directly with dose and inversely with half-life
what is physiological dependence?
• Physiologic Dependence = constant requirement to prevent withdrawl syndrome
what are the cons to Short-acting benzodiazepines?
Short-acting benzodiazepines = tolerance, morning insomnia, rebound anxiety (worse than before you started taking the drug)
how does alcohol use impact benzo patients?
• Binds GABA A receptor and potentiates BZ-induced chloride influx
• Additive depressant effects and lower therapeutic index
how do Antipsychotics, antihistamines, others impact benzo patients?
• Additive sedation
what antidepressants can we use for GAD and what do you know about them?
SNRI (Venlafaxine) and Paroxetine (Paxil) approved for GAD:
• Therapeutic lag just like MD therapy
• 60-70% response rate after 2 months with Paxil
• Equivalent efficacy to benzodiazepines
what mechanism is at play for antidepressants used for GAD?
• Mechanism not known; relief of comorbid depression likely classic AD activity
can other antidepressants be used to treat GAD?
• TCAs achieved higher remission rate than other anxiolytics, but adverse effects make them a poor choice...usually
Buspirone is another GAD drug. How does it work?
• Mechanism likely involves reduction of synaptic serotonin by activation of presynaptic 5-HT1a receptors.
why is buspirone a good choice?
Little risk of:
• Motor impairment
• Dependence
• Excessive sedation (hypnotic effects)
Adverse Effects:
• Dizziness, nausea, headaches
Despite better SE profile, buspirone is considered 2 nd-line choice. why?
• Efficacy reportedly inconsistent from patient to patient
• Lack of efficacy in comorbid depressive/anxiety
• Delayed onset (> 2 weeks)
what is buspirone useful in?
• Uncomplicated GAD
• Patients with other failed anxiolytic therapies
• Patients with a history of drug abuse
• Shorter therapeutic lag than some other options
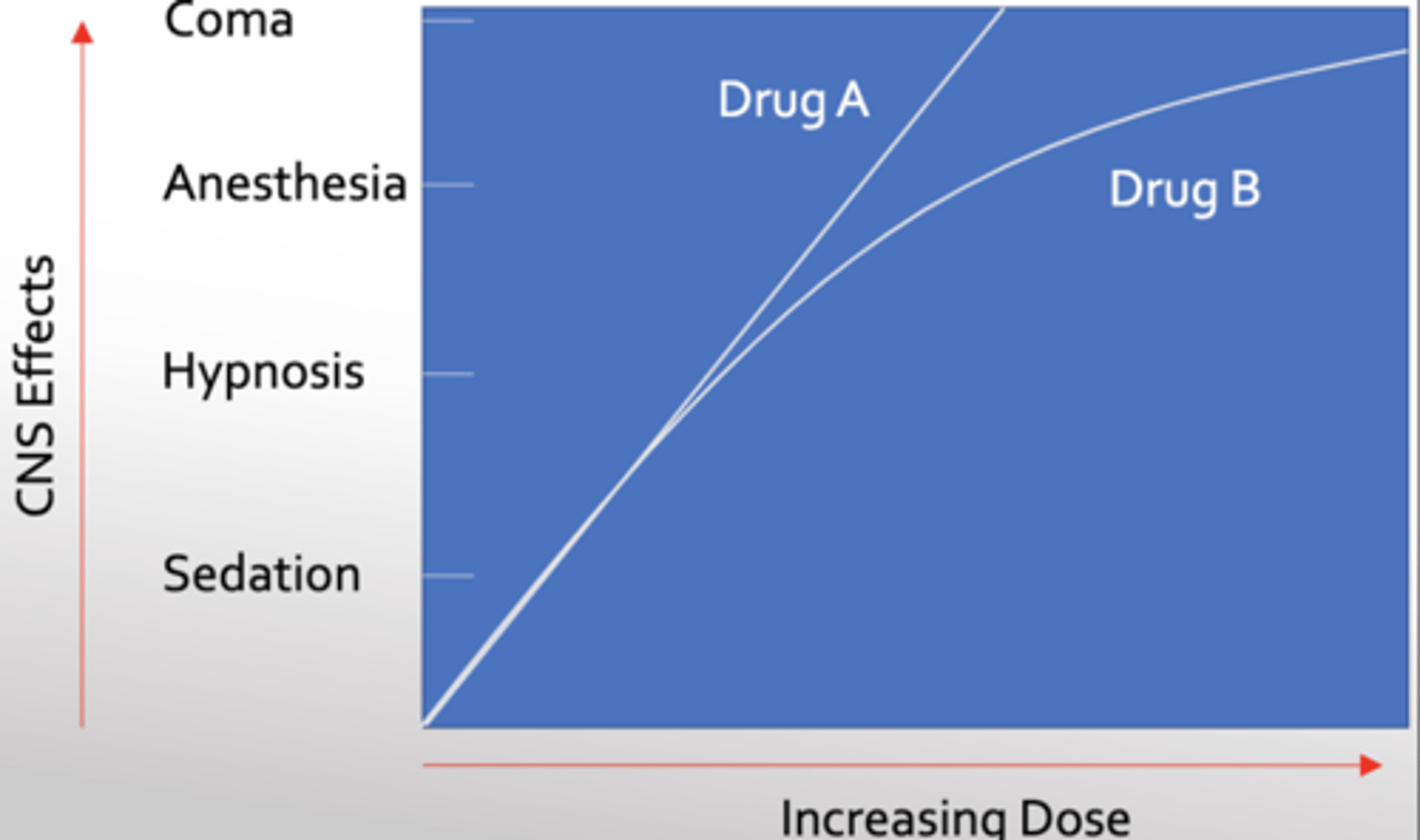
Graph showing which drugs should be prescribed based on patients needs
what are Barbiturates?
• Former first-line anxiolytic, sedative, hypnotic
+ Phenobarbital (long), Pentobarbital (short), Thiopental (ultra-short)
how do Barbiturates work?
• Prolong duration of GABAA chloride channel opening
how have Barbiturates use been limited?
Use limited by strong adverse effects:
• Drowsiness, impaired concentration, sluggishness, synergy with ethanol
• Drug hangover - nausea, dizziness
• P450 induction-related drug interactions
• Physical dependence - abrupt, severe withdrawl
• Very low therapeutic index
how are Barbiturates used today?
• Anesthesia - Thiopental for induction
• Anticonvulsant - Tonic-clonic, status epilepticus, pediatric febrile seizures
what are hypnotics? ex?
Zolpidem (Ambien), Zaleplon (Sonata) and Eszopiclone (Lunesta) are newer non- BZs
why may we prefer hypnotics over benzos?
• Benzodiazepines associated with reduced REM sleep, tolerance, amnesia
Zolpidem (Ambien), Zaleplon (Sonata) and Eszopiclone (Lunesta) are newer non- BZs that offer advantages:
• Low chance of changing sleep patterns
• Reduced chance of anterograde amnesia
• Reduced tolerance
• Reduced day-after psychomotor depression
• Rapid onset
Take Home Points
• Generalized Anxiety Disorder is a common early-onset anxiety disorder, often secondary to other illnesses, characterized by 6 months of debilitating psychological, cognitive and physical symptoms.
• Overactive NE Locus Ceruleus neurons and reduced temporal lobe GABA A receptor function are thought to be partially involved in GAD
• Classical drug treatment for GAD was barbiturates; discontinued except for refractory cases due to dependence, safety and drug interaction issues
• First line therapy is benzodiazepines, SSRI's and SNRI's; Buspirone and TCA's are second or third choices
• Benzodiazepines and non-benzodiazepine hypnotics are useful as sleep aids; newer generation non-BZ drugs are generally better tolerated.