B16 & 17 - Structure of the lungs and mechanism of breathing
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
What structures are found in the upper respiratory tract?
Pharynx
Nasal cavities
Vocal cords
Larynx
What is the role of the upper respiratory tract?
Warm inhaled air (to preserve body temperature)
Humidify air
Filter air
What structures are found in the lower respiratory tract?
Trachea
Left and right bronchus
Left and right lung
What is a likely first point of infection for SARS-CoV-2?
Nasal ciliated and secretory cells
Study done found high number of virions suggesting efficient viral replication
What is the role of type 1 alveolar cells?
Very thin cells
Allow for efficient gas exchange
What is the role of type 2 alveolar cells?
Thick cells which release surfactant
This reduces surface tension inside the alveoli, making the lungs easier to expand
What percentage of the surface of alveoli are covered by capillaries?
80-90% of the surface of alveoli
Allows for efficient gas exchange by maintaining a gradient
What does Boyles’ Law say?
Pressure and volume have an inverse relationship
If volume increases then pressure decreases and vice versa
How does Boyles law allow our lungs to function?
As lung volume increases, the pressure decreases below atmospheric pressure.
This causes air to flow into the lungs
As lung volume decreases, the pressure increases above atmospheric pressure
This causes air to flow out the lungs
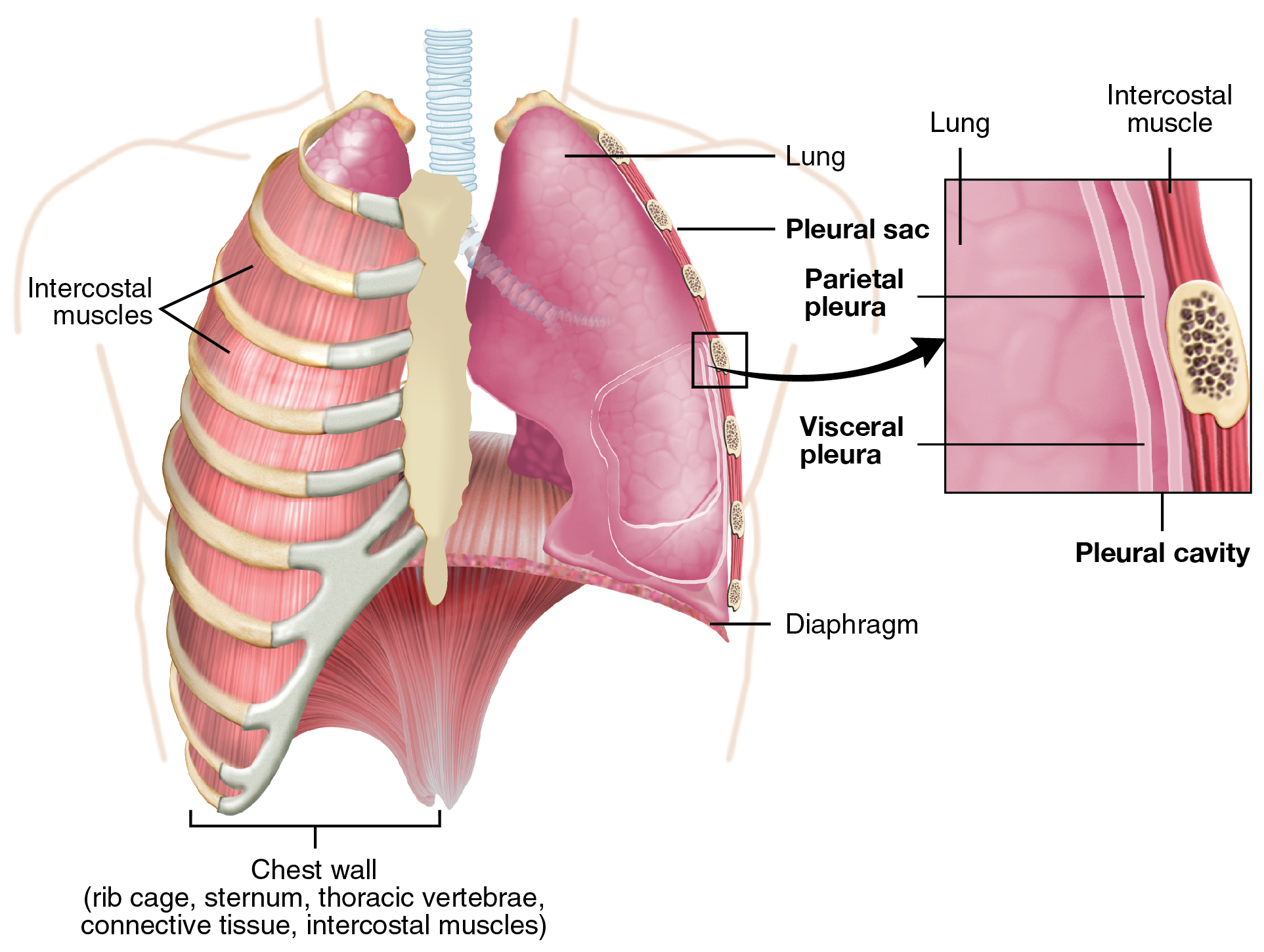
What is the pleural sac?
Also known as the pleural cavity
A two-layered serous membrane which covers the lungs and attaches to the chest wall
What muscles contractions are involved in inspiration?
External intercostal muscles
Diaphragm
Scalenes
Sternocleidomastoids
What muscle contractions are involved in expiration
Internal intercostal muscles
Abdominal muscles
Where does the thoracic cage move during inspiration?
Upwards and outwards
What causes the majority of the change in thoracic volume?
Most of the change is due to the diaphragm
30% of the volume change is due to muscles in the ribs
As the diaphragm contracts, thoracic volume ___________.
As the diaphragm contracts, thoracic volume increases.
What is FEV1?
Forced expiratory volume in one second (FEV1)
How much air a person can exhale in the first second of a forced breath
What is MVV?
Maximum voluntary ventilation
How much air a person can breathe in and out in 12 seconds
What is FVC?
Forced vital capacity
Maximal volume of air exhaled with maximally forced effort from a maximal inspiration
Internal intercostal muscles are not needed during resting breathing due to the elastic property of the lungs
True or False.
True.
Resting breathing is ‘passive’ and the internal intercostal muscles are not needed
What is the normal pH of the blood?
7.35-7.45
How does the body control pCO2 and blood pH?
By altering the respiratory rate to allow more or less CO2 to be removed.
What is partial pressure and how do you calculate it?
Air pressure is ~760mmHg and 21% of the air is oxygen. What is the pO2?
Partial pressure is the pressure exerted by a specific gas within a mixture of gases (like air)
Partial pressure can be calculated by using the % gas in the mixture and the pressure of the mixture.
E.g. 760mmHg x 0.21 = 160mmHg
pO2 = ~160mmHg
Why do you absorb less oxygen at high altitudes?
As you get higher the pressure decreases but the percentage of oxygen does not change.
This means the partial pressure of oxygen at high altitudes will be near that of venous blood
This means there is very little gradient to drive oxygen absorption
Where are central chemoreceptors located?
Brain stem
Where are peripheral chemoreceptors located?
Arterial chemoreceptors in carotid bodies and aortic arch
There is too much CO2 in the blood. How do chemoreceptors fix this?
Chemoreceptor senses the high pCO2 and sends signals to respiratory muscles
This allows for changes in breathing to alter conditions (e.g. faster ventilation to remove excess CO2)
Where is the rhythmic cycle generated from?
The medulla oblongata
Which neurones (inspiratory/expiratory) are found in the dorsal root ganglia?
Mainly inspiratory neurones
Send signals to diaphragm and intercostals
Which neurones (inspiratory/expiratory) are found in the ventral root ganglia?
Contains both inspiratory and expiratory neurones
Sends impulses to larynx, pharynx, diaphragm and external intercostals
What is the role of the Pons in respiration?
Modifies the output from the medullary centres
How do central chemoreceptors detect CO2 levels?
CO2 can cross the BBB but H+ and HCO3 cannot.
The central chemoreceptors can therefore respond to the pH of the CSF which changes when CO2 diffuses in
CSF has little buffering capacity
What do central chemoreceptors respond to?
Changes in pCO2 (and pH)
What do Peripheral chemoreceptors respond to?
Changes in pO2
Also detect changes in CO2 and pH
If you remove the peripheral chemoreceptors, you will stop breathing as they are key to maintaining a rhythmic breathing cycle.
True or False.
False.
They can be removed and you won’t stop breathing.
They are not essential and are a backup system in case the central chemoreceptors fail