Anatomy Exam 3
1/121
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
122 Terms
Regarding surface anatomy, describe the two patterns used to break up the abdomen into different regions
quadrants - RUQ, LUQ, RLQ, LLQ
regions - right hypochondriac, epigastric, left hypochondriac, right lumber, umbilical, left lumbar, right iliac, hypogastric, left iliac
Describe the layers of the anterior abdominal wall (superficial to deep)
skin, Camper’s fascia (fatty layer), Scarpa’s fascia (membranous layer), external oblique muscle, internal oblique muscle, transversus abdominis muscle, transversalis fascia, extraperitoneal fascia, parietal peritoneum
What muscles are located on the anterior abdominal wall? (superficial to deep)
anterolateral: external oblique muscle, internal oblique muscle, transversus abdominis muscle
anteriormedial: pyramidalis, rectus abdominis
Action and Innervation of External Oblique Muscle
Action: compress abdominal contents, flex trunk (bilateral), rotation of trunk (unilateral)
Innervation: anterior rami of T7-T12
Action and Innervation of Internal Oblique Muscle
Action: compress abdominal contents, flex trunk (bilateral), rotation of trunk (unilateral)
Innervation: anterior rami of T7-T12
Action and Innervation of Transversus Abdominis
Action: compress abdominal contents
Innervation: anterior rami of T7-T12
Action and Innervation of Rectus Abdominis
Action: compress abdominal contents, flex trunk (bilateral)
Innervation: anterior rami of T7-T12
Action and Innervation of Pyramidalis
Action: tenses linea alba
Innervation: anterior ramus of T12 (subcostal nerve)
How is the rectus sheath formed?
Formed by the aponeuroses of the external, internal and tramsversus abdominis muscles
Above arcuate line, anterior: external+internal
Above arcuate line, posterior: internal+transversus
Below arcuate line, anterior: external+internal+transversus
At what point is the rectus sheath not present? What is posterior to the rectus sheath at this point?
Not present below the arcuate line, posterior
transversalis fascia
What is the arterial supply of the anterior abdominal wall? What is their parent artery? Where are these arteries located?
Superior Wall: superior epigastric artery, musculophrenic artery (branches of internal thoracic artery)
if superior to arcuate line, superior epigastric artery is between the posterior restus sheath and rectus abdominis
Inferior Wall: inferior epigastric artery (branch of external iliac artery)
If inferior to arcuate line, inferior epigastric artery is between the transversalis fascia ad rectus abdominis
Why is the abdominal wall weakened in the inguinal region?
because of the inguinal canal
What is the processus vaginalis?
a pouch that protrudes through the layers of the anterior abdominal wall during the descent of the testis
What is the gubernaculum?
In males: a tether that attaches the inferior end of the gonad to the scrotum
In females: a tether that attaches the inferior end of the gonad to the labia majora
What structures demarcate the beginning and end of the inguinal canal?
begins at the deep inguinal ring, ends at the superficial inguinal ring
What structures pass through the inguinal canal?
genitofemoral nerve (genital branch), ilioinguinal nerve, spermatic cord (men), round ligament (women)
What are the borders of the inguinal canal?
Roof: transversalis fascia, internal oblique muscle, transversus abdominis muscle
Posterior: transversalis fascia
Anterior: aponeurosis of external oblique, internal oblique muscle
Floor: inguinal ligament, lacunar ligament
What is the difference between an indirect and direct inguinal hernia?
Indirect: herniated contents pass thru deep and superficial rings, occurs lateral to inferior epigastric vessels
Direct: herniated contents pass thru only the superficial ring, occurs medial to inferior epigastric vessels
What are the three fascial coverings that surround the spermatic cord or round ligament of the uterus? From what structure does each fascial layer originate from?
External spermatic fascia (superficial): from external oblique muscle
Cremasteric fascia (middle): from internal oblique muscle
Internal spermatic fascia (deep): from transversalis fascia
Describe the spermatic cord. Where does it begin and end? What are its contents?
begins at the deep inguinal ring and ends at the scrotum
contents: pampiniform plexus of veins, ductus deferens, cremasteric artery, testicular artery, artery of the ductus deferens, genital branch of genitofemoral nerve, sympathetic nerve fibers, lymphatic vessels
What is the cremaster muscle and cremaster reflex?
Cremaster muscle: a thin muscle that surrounds the testicles and spermatic cord in males, is responsible for raising and lowering the testicles, which regulates temperature and offers protection
Cremasteric reflex: superficial reflex triggered by stroking the inner thigh, causing the cremaster muscle to contract and elevate the testis
Describe the round ligament of the uterus. Where does it begin and end?
remnant of the gubernaculum, has the same fascia coverings as the spermatic cord, begins at the uterus to the skin of the labia majora
Describe the peritoneum.
2 layers: parietal peritoneum (lines the abdominal wall) and visceral peritoneum (adheres to abdominal structures) + peritoneal cavity
What are the two divisions of the peritoneal cavity? What structure connects the two divisions?
Greater sac and lesser sac
Epiploic foramen
What are the different types of peritoneal folds?
Omenta, mesenteries, ligaments
What are the attachments of the greater and lesser omentum?
Greater: attached to greater curvature of stomach
Lesser: attached to lesser curvature of stomach, 1st part of duodenum, liver
Why is the greater omentum considered the policeman of the abdominal cavity?
because of its ability to move around the abdominal cavity, look for foreign objects, and physically wall off areas of inflammation to prevent the spread of infection
What two ligaments are found within the lesser omentum? What structures pass through these ligaments?
hepatogastric ligament = gastric vessels
hepatoduodenal ligament = proper hepatic artery, portal vein, bile duct
What is the role of omenta?
act as double layer of peritoneum
What is the function of mesenteries?
Attach viscera to posterior abdominal wall
What is the difference between intraperitoneal and retroperitoneal? Which organs are intraperitoneal? Which organs are retroperitoneal?
intraperitoneal = within the peritoneum
esophagus, stomach, jejunum, ileum, cecum, appendix, transverse colon, sigmoid colon
retroperitoneal = outside the peritoneum
duodenum, pancreas, kidneys, ascending and descending colon
What are the four regions of the stomach?
What structure separates the stomach, and which stomach region, from the esophagus?
What structure separates the stomach, and which stomach region, of the duodenum?
cardia, fundus, body, and pylorus
lower esophageal sphincter
pyloric sphincter
What are rugae? Where is it found and what is its function?
wrinkles or folds in the stomach, helps stomach to increase in size and surface area to accommodate food
What are the three parts of the small intestine? Which is their correct order, and therefore, which structures do they connect to?
duodenum (connects to stomach), jejunum, ileum (connects to cecum of large intestine)
Which organ is found nestled into the curvature of the duodenum?
pancreas
What are the four parts of the duodenum?
What is found within the second part of the duodenum?
What structure is attached to the fourth part of the duodenum and jejunum? What is the point called? What is the function of this structure?
superior, descending, inferior and ascending
minor and major duodenal papilla
ligament of Treitz, widen the angle of the duodenojejunal flexure during contraction
What are some features that allow you to differentiate the jejunum from the ileum?
Jejunum: long vasa recta, less rows of arterial arcades
Ileum: short vasa recta, more rows of arterial arcades
What structure separates the ileum from the cecum?
Ileocecal valve
What are the different parts of the large intestine? What are three characteristics that are unique to the large intestine?
ascending colon, transverse colon, descending colon, sigmoid colon
taeniae coli, haustra of colon, omental appendices
What structure hangs off the cecum?
appendix
What are the four lobes of the liver?
What structure separates the right and left lobes on the anterior aspect? What is on the inferior aspect of this structure?
What structures border the quadrate and caudate lobes?
right, left, caudate, quadrate
falciform ligament, round ligament of the liver (ligamentum teres)
caudate: inferior vena cava and ligamentum venosum
quadrate: gallbladder and ligamentum teres
What is the porta hepatis? Where is it located? What enters/exits this structure?
where structures are going to enter or exit the liver
posterior side of the liver, in the center
enter: hepatic portal vein and right and left hepatic artery - proper hepatic artery
exit: right and left hepatic duct - common hepatic duct
Bile leaves the gallbladder and liver through which ducts? These ducts combine to form what duct? Where does the duct empty into?
Bile from the liver through the left and right hepatic ducts= merge to form the common hepatic duct
Bile from the gallbladder travels through the cystic duct
common hepatic duct + cystic duct = form the common bile duct, which empties into the duodenum through the major papilla
What is the relationship of the pancreas to the duodenum?
head of pancreas nestled in the curvature of duodenum
neck of pancreas is anterior to the superior mesenteric vein and artery
Where does the main and accessory pancreatic ducts empty into?
main pancreatic duct drains into the major papilla of duodenum
accessory pancreatic duct branches off of main and drains into the minor papilla
What structure forms when the main pancreatic duct and common bile duct combine?
hepatopancreatic ampulla
Where is the spleen located in the abdominal cavity? Why is the spleen not considered a digestive organ?
located behind the stomach, next to pancreas
because it is part of the immune system where its function is to recycle old RBCs
What are the main three arteries branching off the abdominal aorta?
celiac trunk, superior mesenteric artery, inferior mesenteric artery
What is the primitive gut? What organs belong to each region?
Foregut = esophagus, stomach, proximal duodenum, liver, pancreas, gallbladder
Midgut = distal duodenum, jejunum, ileum, cecum, appendix, ascendin colon, 2/3 transverse colon
Hindgut = 1/3 transverse colon, descending colon, sigmoid colon, rectum, upper anal canal
What are the branches of the celiac trunk? What pathway do they take? Which organs do they supply?
left gastric artery - go along the left side of the lesser curvature of the stomach
branch: esophageal arteries - going up towards esophagus
splenic artery - go to the left, under the pancreas and towards the spleen
branch: left gastroepiploic artery - goes along left side of the greater curvature of stomach
common hepatic artery - goes to the right and branches into the proper hepatic and gastroduodenal artery
proper hepatic artery branches: right and left hepatic artery - goes to liver, cystic artery - goes to gallbladder, right gastric artery - goes along right side of the lesser curvature of the stomach
gastroduodenal artery branches: right gastroepiploic artery - goes along right side of the greater curvature of stomach, superior pancreaticduodenal artery - between the duodenum and pancreas
What are the branches of the superior mesenteric artery? What pathway do they take? Which organs do they supply?
middle colic artery - right side of SMA, top, towards large intestine
right colic artery - right side of SMA, middle, towards large intestine
ileocolic artery - right side of SMA, bottom, towards large intestine
jejunal and ileal arteries - left side of SMA, bottom, towards jejunum and ileum
contains arterial arcades and vasa recta
What are the branches of the inferior mesenteric artery? What pathway do they take? Which organs do they supply?
left colic artery - go and supply for the transverse and descending colon
sigmoid arteries - go towards sigmoid colon
superior rectal/rectal artery - go and supply for the rectum
Anastomoses
right and left gastric arteries
right and left gastroepiploic arteries
superior and inferior pancreaticoduodenal arteries
right branch of middle colic artery and ascending branch of right colic artery
left branch of middle colic artery and ascending branch of left colic artery
descending branch of right colic artery and ileocolic artery
descending branch of left colic artery and sigmoid arteries
sigmoid arteries and superior rectal artery
What is the portal vein? What organs drain into the portal vein? After draining into the portal vein, what is the pathway of venous drainage?
the portal vein (formed from splenic vein, superior mesenteric vein, inferior mesenteric vein) is the final common pathway for GI venous blood
stomach, small and large intestines, gallbladder, pancreas and spleen drain into it which then goes to the liver
after the liver detoxifies the blood, the blood returns to the IVC and the heart
The portocaval anastomoses connects which two structures from the portal and systemic venous systems?
inferior esophagus: portal - esophagus branch from the left gastric vein, caval - esophageal vein from the azygos vein
rectum: portal - superior rectal vein from the inferior mesenteric vein, caval - inferior and middle rectal veins from the internal iliac vein
umbilicus: portal - paraumbilical vein from the hepatic portal vein, caval - superficial epigastric vein from the external iliac vein
What is the significance of this anastomoses? What happens when there is a blockage in one of the structures that contributes to the anastomosis?
allows blood to reach systemic venous system if there’s an obstruction in the portal system
What is the difference between extrinsic and intrinsic innervation of the gastrointestinal track?
extrinsic - autonomic nervous system (parasympathetic and sympathetic)
intrinsic - enteric nervous system
What is the role of the autonomic nervous system in digestion? What are the nerves controlling the parasympathetic and sympathetic nervous systems?
parasympathetic - rest and digestion, vagus nerve
sympathetic - fasting state, greater lesser and least splanchnic nerves
What the three splanchnic nerves? Which organs do they innervate?
Foregut (vascularized by celiac trunk) = greater splanchnic nerves (T5-T9/T10)
Midgut (vascularized by SMA) = lesser splanchnic nerves (T10/T11)
Hindgut (vascularized by IMA) = least splanchnic nerve (T12)
What are the basic lymphatics of the abdomen to the extent discussed within lecture?
Foregut - celiac lymph nodes - cisterna chyli - thoracic duct
Midgut - superior mesenteric lymph nodes - cisterna chyli - thoracic duct
Hindgut - inferior mesenteric lymph nodes - cisterna chyli - thoracic duct
What structures are found on the posterior abdominal wall?
abdominal aorta, IVC, nerves, muscles (psoas major, psoas minor, iliacus, quadratus lumborum), kidneys and lymphatics
Action and innervation of Psoas Major
Lateral flexion of trunk, flexion of the thigh
Anterior rami of L1-L3
Action and innervation of Psoas Minor
Weak flexion of trunk
Anterior rami of L1
Action and innervation of Quadratus Lumborum
individually: lateral flexion of trunk, depression of rib 12
together: extension of trunk
anterior rami of T12, L1-L4
Action and innervation of Iliacus
flexion of the thigh
femoral nerve (L2-L4)
What are the nerves of the posterior abdominal wall?
sympathetic trunks which give off lumbar splanchnic nerves which contribute to formation of the
prevertebral plexus (celiac plexus (between celiac trunk and SMA), aortic plexus (between SMA and bification of abdominal aorta), superior hypogastric plexus (after bification))
lumbar plexus
The anterior rami of which spinal nerves form the lumbosacral plexus?
anterior rami of L1-L4
What are the major nerves of the lumbosacral plexus?
Subcostal nerve (T12)
Iliohypogastric nerve (L1)
Ilioinguinal nerve (L1)
Genitofemoral nerve (L1, L2)
Lateral cutaneous nerve of thigh (L2,L3)
Onturator nerve (L2-L4)
Femoral nerve (L2-L4)
What is the difference between the right and left kidneys?
right kidney is a vertebral level lower than the left because of the liver
Describe how the kidneys are enclosed, the order they enclosures lay, and their function.
Deep to superficial -
renal capsule (thin and translucent, prevents infection), perirenal fat (adipose tissue, cushion and protect kidneys), renal fascia (dense, tough CT), pararenal fat (fat, only on posterior aspect of kidney)
Which structures do the renal artery and vein branch off of or drain into?
right and left renal arteries branch off the abdominal aorta
right and left renal veins drain into the IVC
What is the nutcracker syndrome?
compression of the left renal vein, causing backup of fluid and stops the drainage of the left kidney
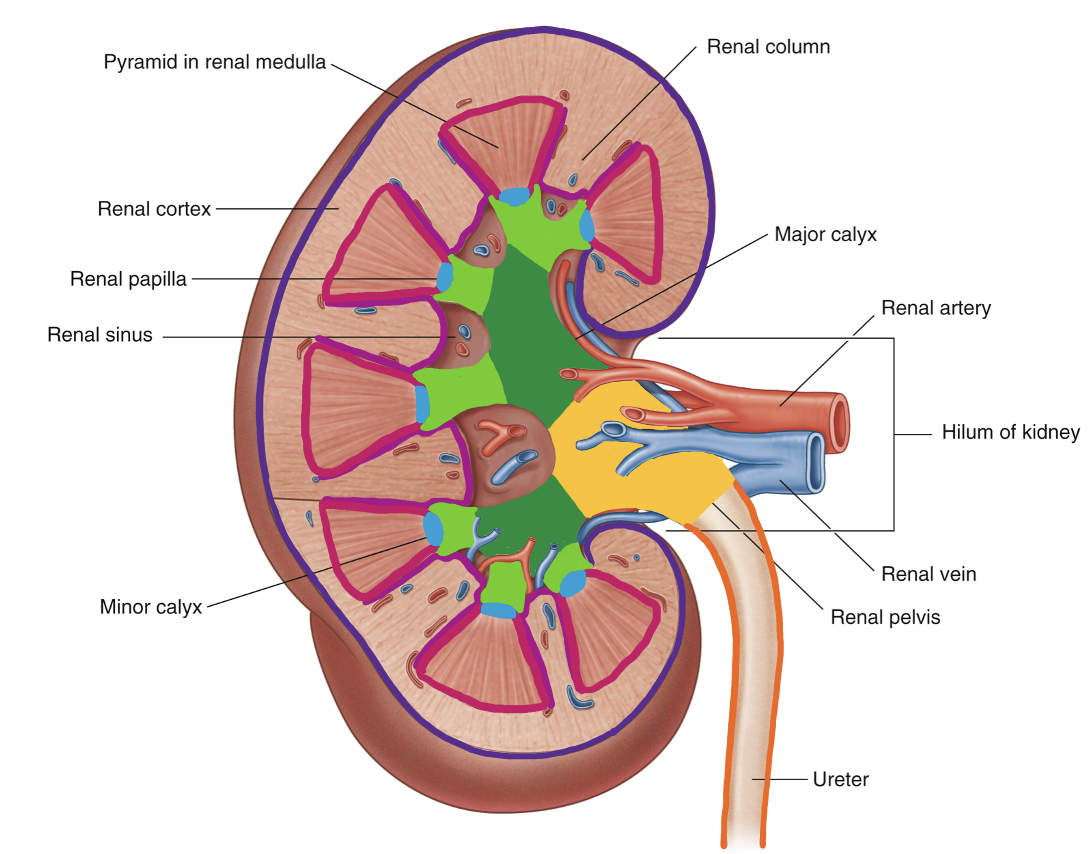
Structures of the kidney
renal cortex - outer layer
columns
renal medulla - inner layer
pyramids
papilla - where urine exits
minor calyx - one for every pyramid
major calyx - multiple minor calices form the major calices
renal pelvis
ureter
What structures do the ureters connect?
connect the kidneys to the urinary bladder
What are the three constriction points of the ureters?
ureteropelvic junction - where renal pelvis becomes ureter
crossing over the external iliac artery
ureterovesical junction - where ureter enters bladder
What arteries vascularize the ureters?
superior ureter - renal arteries
middle ureter - abdominal aorta, gonadal arteries, common iliac arteries
inferior ureter - internal iliac arteries
What is the relationship of the suprarenal/adrenal glands and the kidneys?
located on top of the kidneys
What is the vascularization of the suprarenal/adrenal glands?
For each artery, what is their parent branch?
For each vein, where does it drain into?
superior suprarenal arteries - parent branch = inferior phrenic artery
middle suprarenal artery - parent branch = abdominal aorta
inferior suprarenal artery - parent branch = renal artery
right suprarenal vein - drains into IVC
left suprarenal vein - drains into left renal vein
What is the innervation of the kidneys and suprarenal/adrenal glands?
T10-L2
Describe how the shape of the pelvis is different for men and women.
women: pubic arch 80-85 degrees, circular pelvic inlet, ala is more broad and spread away from each other, ischial spines are less prominent
men: pubic arch 50-60 degrees, heart-shaped pelvic inlet, ala is more curved and project more medially toward each other, ischial spines project more medially
What bones, ligaments, and muscles form the (lateral) pelvic wall?
bones: sacrum, coccyx, ilium, pubis, ischium
ligaments: sacrospinous ligament, sacrotuberus ligament
muscles: piriformis muscle, obturator internus muscle
Action and innervation of Piriformis muscle
laterally rotate and abduct the thigh
S1 and S2
Action and innervation of Obturator Internus muscle
laterally rotate and abduct the thigh
nerve to the obturator internus
What is the pelvic diaphragm? What muscles comprise the levator ani?
muscles that forms the base of the pelvic cavity
levator ani (puborectalis, pubococcygeus, iliococcygeus) + coccygeus = pelvic diaphragm
Action and innervation of Levator Ani
support pelvic viscera, maintain closure of rectum and vagina
inferior rectal branch of pudendal nerve (S2-4)
Action and innervation of Coccygeus
support pelvic viscera, pulls coccyx forward after defecation
S3-S4
What is the role of the puborectalis muscle in defecation?
Acts as a sling around the rectum
At rest, it contracts to pull the rectum forward, creating a sharp angle that prevents stool from passing unintentionally
During defecation, it relaxes so th rectum is almost straight and allows stool to pass more easily
What is the trigone of the bladder?
small, triangular area on the inner surface of the bladder floor
defined by the openings of the two ureters and the urethra
Compare and contrast male and female urethras.
Male = long, used for both urine and semen
Female = short, used only for urine
What is the anatomical relationship of the bladder, uterus, and rectum?
uterus separates the urinary bladder and rectum
anterior to posterior = bladder, uterus, rectum
Trace the pathway beginning with the creation of sperm to its ejection in the form of semen.
testes (where sperm is produced) - epididymis - vas deferens - ejaculatory duct (vas deferens + seminal vesicle, mix fluids from seminal vesicles and prostate gland to form semen) - ejected from urethra during ejaculation
What are the different parts of the epididymis?
head, body and tail
Describe the pathway the ductus deferens takes from the scrotum to the pelvic cavity.
passes thru the inguinal canal, crosses the external iliac artery, crosses the ureter, joins the seminal vesicle to form the ejaculatory duct
Where do the bulbourethral glands empty their secretions into? The duct passes through which structure?
bulbourethral glands empty their secretions into spongy urethra
bulbourethral duct passes thru perineal membrane and corpus spongiosum
List the structures that pass through the prostate.
urethra, ejaculatory duct
What is the anatomical relationship of the prostate to the rectum?
prostate is anterior to the rectum
What are the ovaries? Which ligaments are attached to the ovaries? What do they connect the ovary to?
ovaries = female gonads
mesovarium ligament = mesentery, suspends the ovaries
suspensory ligament = attaches ovaries to lateral abdominal wall
ovarian ligament = attaches ovaries to uterus
What are the different parts of the uterine/fallopian tubes? Which parts catches the egg? Which part is where fertilization occurs? Which part is connected to the uterus?
Fimbriae = catches the egg
Infundibulum
Ampulla = where fertilization occurs
Isthmus = connected to the uterus
What are the different parts of the uterus?
Fundus, body and cervix
myometrium is the muscle that surrounds the entire uterus
the body is lined with endometrium
Why can the uterus be found in both the abdominal and pelvic cavities?
during pregnancy, the uterus expands superiorly into the abdominal cavity