GI 11: Large Intestine
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
the large Intestine is marked proximally by the _____ and distally by the _____
proximally: Ileocecal Sphincter & Valve
distally: External Anal Sphincter
the large Intestine is anatomically distinguished how?
from orad → caudad:
- Cecum
- Ascending
- Transverse
- Descending
- Sigmoid Colon
- Rectum
- Anal Canal
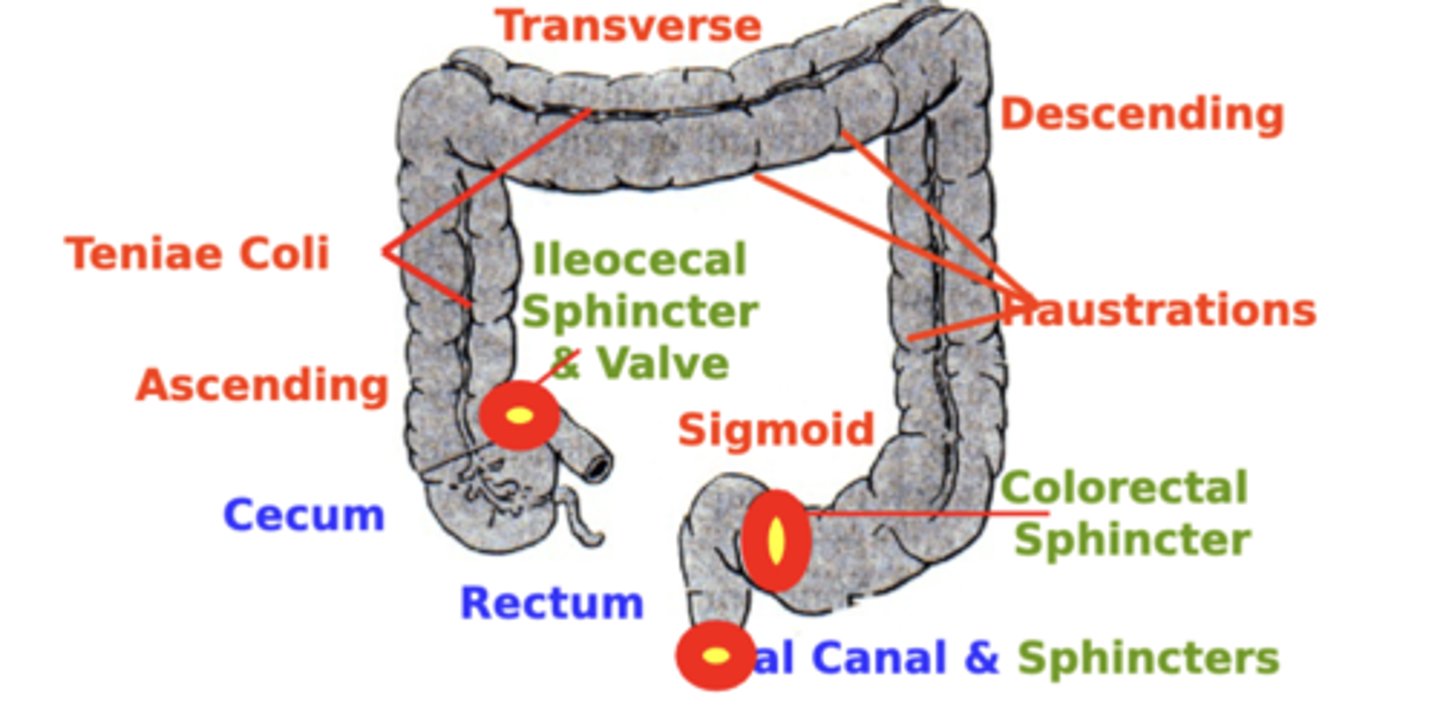
Colorectal Sphincter
separates the rectum and anal canal
Large Intestine Smooth Muscle
1. outer longitudinal layer
- organized into three distinct flat bands called Teniae Coli
2. inner circular layer
- continuous through the anal canal, where it increases in thickness to form the internal anal sphincter
3. smooth-striated muscle transition region
- leads to purely Striated Muscle bundles that comprise the external anal sphincter
Haustra
result from properties of the colon:
1. structural (smooth muscle thickening)
2. functional (segmenting colonic contractions)
give the colon a characteristic segmented appearance
Ileocecal Valve
mainly functions to Prevent Fecal Reflux from the colon into the ileum
- Its lips protrude into the lumen, acting as a one-way valve
- When colon pressure pushes fecal contents backward, the valve closes, preventing reflux into the ileum
Physiologically importance of the Ileocecal Valve
important in order to maintain Sequestration of Most Bacteria within the Colon
Ileocecal Sphincter
primarily functions to Control Ileal Emptying Rate into the colon
- normally remains mildly constricted, causing a general slowing of ileal emptying into the cecum
Physiologically importance of the Ileocecal Sphincter
important because the ileum is the “Point of No Return” in terms of Digestion & Absorption of Major Nutrients
- since the colon does not largely participate in nutrient digestion or absorption
basal constrictive tone of the ileocecal sphincter is maintained by?
intrinsic myogenic control
distension
of adjacent proximal (Ileum) or distal (Colon) intestinal regions modulate sphincter tone and ileal emptying rate
Ileal Distension
- decreases Sphincter Tone
- SPEEDS Ileal Emptying Rate into the colon
- prevents build-up of material in the ileum
Colon Distension
- increases Sphincter Tone
- SLOWS Ileal Emptying Rate into the colon
- prevents excess filling of the colon
Haustrations
Segmenting Contractions
• the most common colonic motility action
• local constricting contractions
• act to Mix intestinal contents with little net propulsion of material
Force of Haustrations
• Colonic segmenting contractions exert Greater Force
• 2-4x Longer in Duration (12-60 sec.) than those of the small intestine
• Contractions deeply constrict the lumen, causing the characteristic Haustrations
Mass Movements
Peristaltic Contractions
- serve in the Propulsion of intestinal contents toward the rectum
Mass Movement Frequency
compared to small intestine peristalsis
- Less Frequent (1-3x/day)
- Longer in Duration (10-30 min.)
- propel material a Greater Distance (20 cm)
SI Peristalsis: 8-12x/min; 4-5 sec., 1-4 cm
Inter-regional Reflex
coordinated with
a. Gastroileal Reflex and
b. Duodenalcolic Reflex
serve to coordinate movement of contents along tract
Duodenalcolic Reflex
Coordinated with the actions of the gastrocolic & gastroileal reflexes
• Duodenal Distension (e.g. After Meal)
• Colon Mass Movement
• Augments Gastrocolic & Gastroileal
• Defecation Sensation After Eating
Gastrocolic Reflex
• Stomach Distension (e.g. After a Meal)
• Colon Mass Movement
• Coordinated w/ Gastroileal Reflex
Duodenal Distension
augments stimulation of Colon Mass Movements
Composition of Feces
- Normal Human Feces is about 75% Water and 25% Solids
- More than half of the components of feces is of Non-Dietary Origin