physiology of large intestine
1/26
Earn XP
Description and Tags
week 3 ctb
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
27 Terms
large intestine
caecum
ascending, transverse, descending and sigmoid colon
rectum
anal canal
ileocecal sphincter prevents reflux into ileum
colonic musculature
circular muscle of colon contracts to divide colon into segments called haustra
longitudinal muscles are 3 non overlapping bands known as taeniae coli
coupling of circular and longitudinal muscles less efficient than in SI
structure of LI
no villi
lined by surface epithelial cells
surface interspersed with colonic crypts
surface epithelial cells primarily responsible for electrolyte absorption
colonic gland cells responsible for ion secretion
folds increase SA
functions of LI
reabsorption of Na+, Cl-, and water
production of semi solid or solid faeces
absorb short chain fatty acids produced by colonic bacteria
secrete K+ , HCO3- and mucus
make and store faeces
moves faeces towards rectum
faeces
non digested/non absorbed dietary food products
colonic bacteria and metabolic products
dead epithelial cells
biliary metabolites
water
excretory products
iron and copper
anions and cations
intestinal fluid and electrolyte transport
fluid load to SI: 8-9L/day
6.5L absorbed by SI
1.9 L absorbed by colon
0.1L excreted in faeces
max absorptive capacity is 4-5L/day
tight junctions
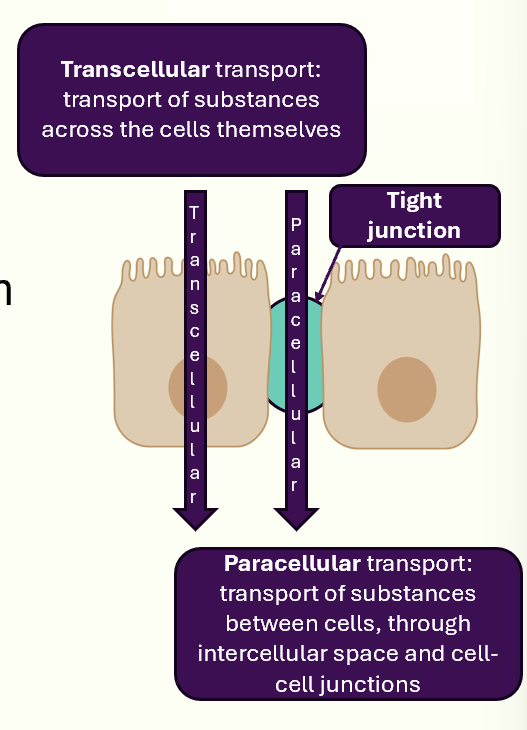
fluid and electrolyte absorption take place by transcellular and paracellular routes
permeability of tight junctions determines which route is used
tight junctions in SI are leaky
tight junctions in LI are tight
majority of fluid movement in colon is via transcellular route
what drives water absorption in the colon?
NaCl absorption
short chain fatty acid absorption
absorption of Na+
NaCl absorption
coupled uptake of Na+ and Cl-
stimulated by various growth factors
inhibited by various hormones
water follows NaCl
absorption of short chain fatty acids
short chain fatty acids absorbed from lumen by surface epithelial cells
absorbed in a Na+ dependent manner
symporters
uptake driven by low intracellular Na+ conc established by basolateral Na+K+ ATPase
short chain fatty acids used as an energy source
absorption of Na+
localised to distal part of colon
driven by epithelial Na+ channel: ENaC (also found in kidney)
channel opens in response to neurotransmitters/hormones
chloride ions follow via paracellular route to maintain electrical neutrality
water absorbed via paracellular route as a result of transepithelial osmotic gradient
last line of defence to prevent excessive water loss in stool
chloride absorption
Cl- absorption occurs throughout SI and LI
closely linked to Na+ absorption
can be passive:
driven by electrochemical grad for Cl-
paracellular or transcellular
driving force for Cl- absorption derives from eitherL
nutrient coupled transport
ENaC (epithelial sodium channel) channels in distal end of colon
chloride secretion
simulated by secretogogues: ACh
involves 3 transport pathways on basolateral membrane:
Na+-K+ ATPase
Na+/K+/Cl- cotransporter
K+ channels
Cl- channel present on apical membrane
Na+-K+ ATPase generates a low intracellular Na+ conc
generates driving force for Cl- entry through Na/K/Cl cotransporter
intracellular Cl- conc rises and electrochemical grad favours Cl- secretion acrtoss apical membrane
control of chloride secretion
Cl- secretion requires stimulation by secretogogues:
bacterial exotoxins
hormones and neurotransmitters
products of cells of immune system
laxatives
works to increase Cl- conductance of the apical membrane either by activating channels ro inserting new channels
diarrhoea
induction of apical Cl- channels is important in pathophysiology of diarrhoea
both a symptom: increase in no. of bowel movements or decrease in consistency
sign: increase in stool volume
osmotic diarrhoea: failure to absorb a dietary nutrient
secretory diarrhoea: endogenous secretion of fluid and electrolytes from intestine
infections with E. coli and cholera
raise concs of secondary messengers
LI motility
material not absorbed in SI enters LI
faecal material moves from caecum through colon to rectum
proximal colon:
non propulsive segmentation
mass peristalsis
control of LI motility
proximal colon stimulated by vagal input + ENS
remainder innervated by pelvic nerves
voluntary input from spinal cord via branches of pudenal nerves
regulates contraction of external anal sphincter
regulates pelvic floor muscles
non-propulsive segmentation contractions
produces circular muscle contractions
churn colonic contents
material retained in proximal colon
allows continuation of fluid and electrolyte absorption
occurs in caecum and proximal colon
mixes contents of LI
associated with sack like segments called haustra
mass movements
function to move contents of LI over long distances (mass peristalsis)
occurs 1-3 times/day
water absorption occurs in distal colon
faecal contents become semi solid and increasingly difficult to move
final mass movement propels faecal contents into rectum for storage until defecation
distal colon
responsible for drying of faeces
contractile movements of sigmoid colon causes retention of colonic contents
promotes drying of faeces and reduction in faecal volume
retention can be 36h or longer
promotes water retention
rectum
colon terminates in the rectum
rectum and colon joined at an acute angle: rectosigmoid junction
rectum lacks circular muscle
surrounded by longitudinal muscle fibres
reservoir for storage of faeces
rectum joints anal canal
internal sphincter
has both circular and longitudinal muscle
involuntary control
external sphincter
encircles rectum
contains only striated muscle
controlled by both voluntary and involuntary mechanisms
disention of rectum inititates rectosphincteric reflex
defecation
entry of faecal matter into rectum causes contraction of smooth muscle in rectal wall
internal anal sphincter relaxes in the rectosphincteric reflex
external anal sphincter relaxes in the rectosphincteric reflex
external anal sphincter is still tonically contracted
once rectum fills to 25% capacity, there is an urge to defecate
when appropriate external anal sphincter is voluntarily relaxed, smooth muscle of rectum contracts
faeces forced out through anal canal
enteric microbial ecosystem
vast assortment of bacteria and other microorganisms
established shortly after birth
matures as child grows
fluctuates depending on diet and circadian rhythms
drastic perturbations can be caused by ABs or aggressive pathogens
roles of colonic microbiota
metabolic reactions (e.g undigested polysaccharides)
formation of secondary bile acids
conversion of bilirubin to uribilinogen
salvage nutrients
degrade digestive enzymes
digest mucus
synthesise certain vitamins (e.g vit K)
limiting growth of pathogenic microorganisms
synthesis and secretion of microbicidal compounds
functions as a physical barrier
influences gene expression in epithelium