Vasc (3) test prep
1/119
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
120 Terms
what are venous waveforms affected by?
Respiratory variations, and Right Atrium pressure
how is antegrade and retrograde venous flow displayed?
Below baseline= movement away from transduce (Antegrade Venous Flow)
Above baseline= movement toward transducer (in Red) (Retrograde Venous Flow)
What is spontaneous blood flow ( venous)
Spontaneous Blood Flow
• End resistance of Right Atrium is very low ( 0-5 mmHg)
• Therefore blood flows spontaneous toward Right atrium
– Changes in flow based on respiration
• As diaphragm compresses IVC during Inspiration, Blood flow decreases and can even briefly change direction
for expiration theres less venous return in upper extremities and more in the lower (opposite with inspiration)
normally become less spontaneous as travel distally (Especially common in calf)
• Muscle contraction propels blood flow back towards heart
– Valves maintain antegrade flow
– Calf muscle pumps venous flow during contraction (walking)
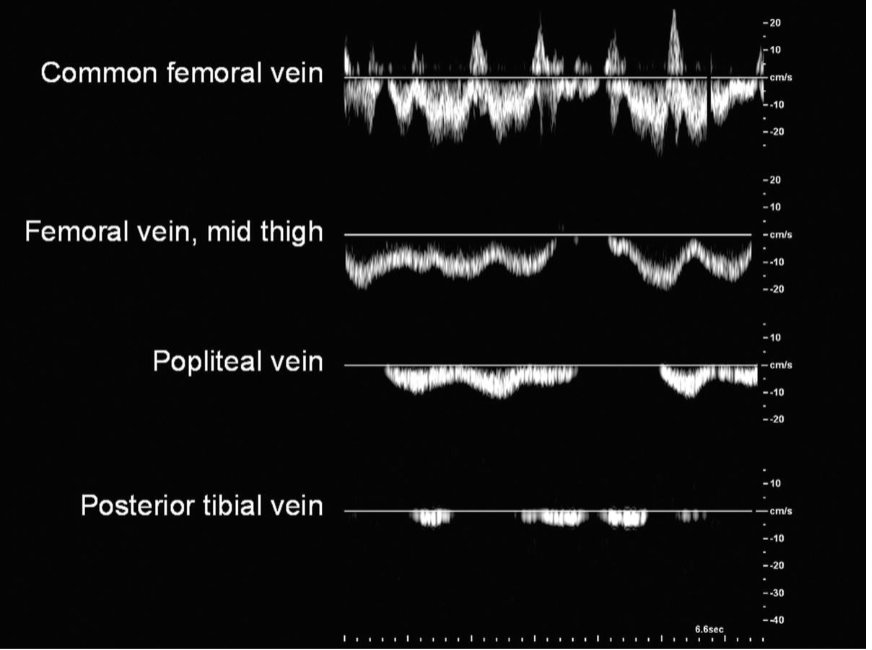
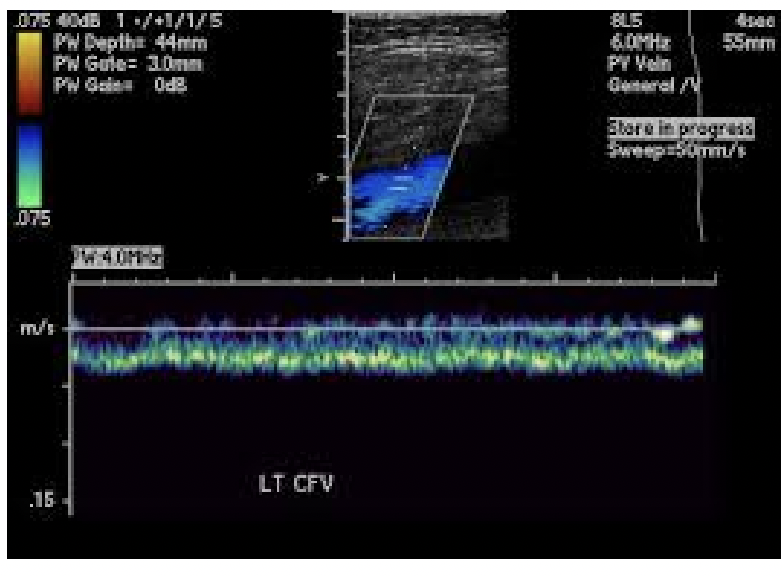
Based on these waveforms, explain at what point the patient is breathing in vs out
With expiration theres less venous return in upper extremities and more in the lower, so when we see cessation ( no flow) that means they’re inspiring and when we see flow they’re breathing out.
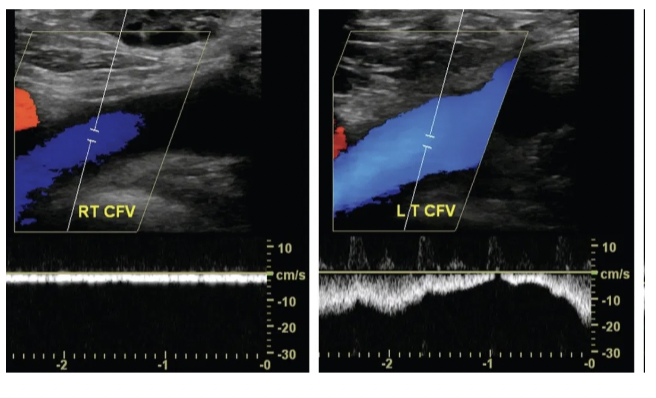
Why do we compare phasicity of venous waveforms side to side
Since both vessels are equidistant from the heart, the phasicity of the blood flow should be equivalent.
Continuous waveform may be indicative of proximal obstruction ( closer to heart)
Based on this image, Here the Left CFV signal appears much more phasic then the Right. You need to evaluate proximally, so evaluate the REIV, and RCIV for thrombus
what is normal venous compliance
applying pressure directly top of vein Results in veins walls coapting completely
Applying pressure distally to where insonating will result in increased antegrade venous flow
Applying Pressure proximally to where insonating, will stop blood flow just a little bit (will see cessation) and when u release your grip you’ll see retrograde flow again.
what does a echo filled lumen indicate, what precautions should you take.
venous thrombosis, be careful with venous compression because there is a risk of embolization if applying too much pressure.
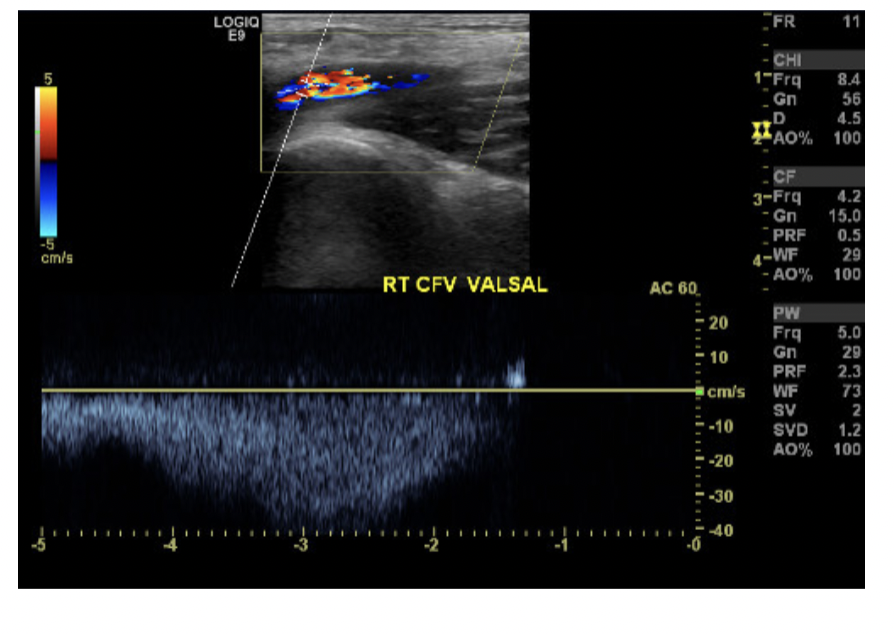
What is the Valsalva maneuver
( used it PT’s legs are sensitive)
Pt takes a deep breath in and bears down (tightens stomach muscles) increases
intrathoracic pressure
Normal response is no venous flow during Valsalva and augmented antegrade flow when pt releases
– Abnormal is retrograde flow throughout Valsalva
Is this venous valve competant or not? how can you tell.
Proximal compression assesses competence of venous valves
We can tell it competent because competent valve prevent retrograde venous blood flow, and we see w/compression a cessation rather than retrograde flow.
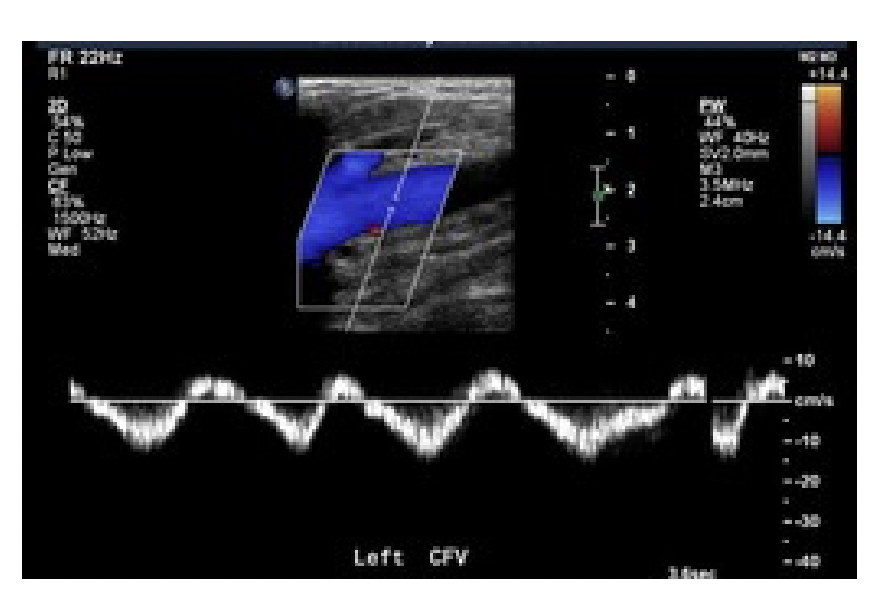
is this waveform abnormal or normal?
this is pulsatile flow which is abnormal, Due to increased Right Atrial Pressure. Indicative of Congestive Heart Failure
Based on this, is this a normal venous blood flow?
No, this is a abnormal continuous venous blood flow. Indicative of proximal obstruction
But this could also be
• Venous thrombosis
• Patient Position or Breathing related
Do not perform Valsalva or Compressions Maneuvers on a patient with Continuous
Venous Waveforms until you rule out proximal venous thrombosis ( risk of embolization)
What are our deep veins, superficial and perforating veins
Deep Veins : CFV, PFV, FV, POP, PTV, PER
– Have Accompany arteries
Superficial Veins: GSV, SSV
– Do not have accompanying arteries
Perforating Veins: name by location (ie. prox calf)
– Connect deep and superficial veins
What are the objjectives for LEV exam,
To detect Venous Thrombosis (DVT/ SVT) and To evaluate for Venous Insufficiency (Reflux )
( you will be told what is needed to be assessed)
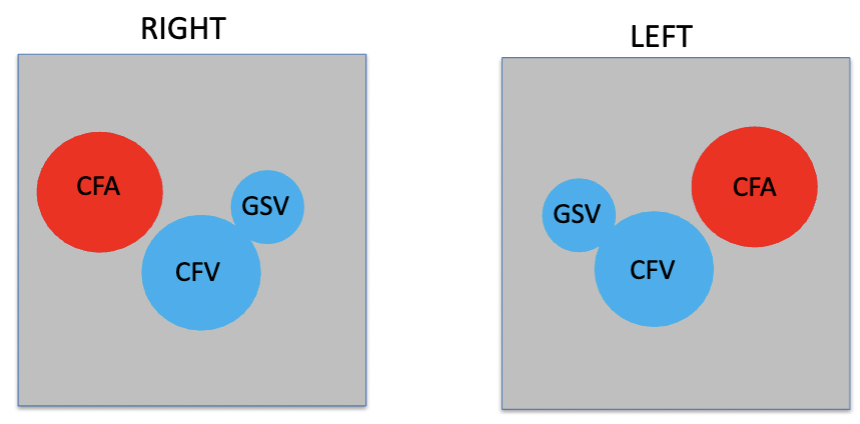
What vessels are in the mickey mouse sign
memorize, look at image.
how do you begin your LEV exam
start with bilateral CFV, if it’s phasic then we can perform our maneuvers (valsalva, prox compression and dist)
if its not phasic then investigate iVC and iliacs for prox obstruction with color and spectral doppler only. ( for risk of embolization)
If CFV appears continuous what would you do?
Investigate proximally (IVC, CIV and EIV)
Where does the PFV run, why is it important?
runs medially and posteriorly from the CFV
• At proximal-mid thigh joins proximal popliteal vein
• Profunda serves as important collateral pathway for venous return from calf
if FV is Bifid what would you do?
normal variant in approx. 25 % of patients ( means it’s duplicated)
• Both bifid branches need to be evaluated during exam
What passes through the adductor canal?
Passageway from medial anterior thigh to posterior leg
bordered by 3 muscles
Femoral Artery, Femoral Vein and Saphenous Nerve pass through
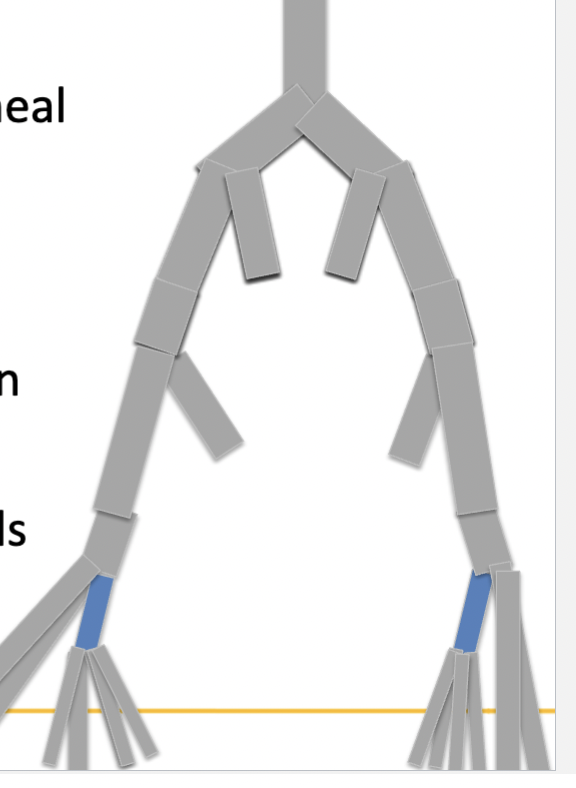
Based on this image what is being shown? what vessels does it bifuricate into?
the TPT, distal to Anterior Tibial Veins origin
• Bifurcates into four vessels ( PTV and PER)
PTV is the more anterior set of vessels
PER is more posterior to PTV, deeper than PTV. Terminates into 2 branches at ankle
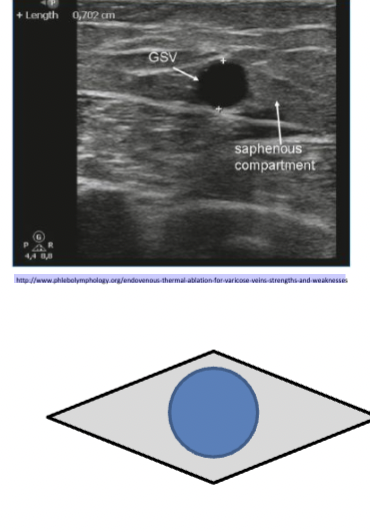
Where are the superficial veins located.
Great Saphenous Vein (GSV)
• Medial on thigh and calf
Small Saphenous Vein (SSV)
• Posterior on calf
Both GSV and SSV
In fascial layer: “Cleopatra eye” landmark ( shown in image)
• Have branches
• Have no accompanying arteries
Axial (main ) trunk is located within “Cleopatra eye”
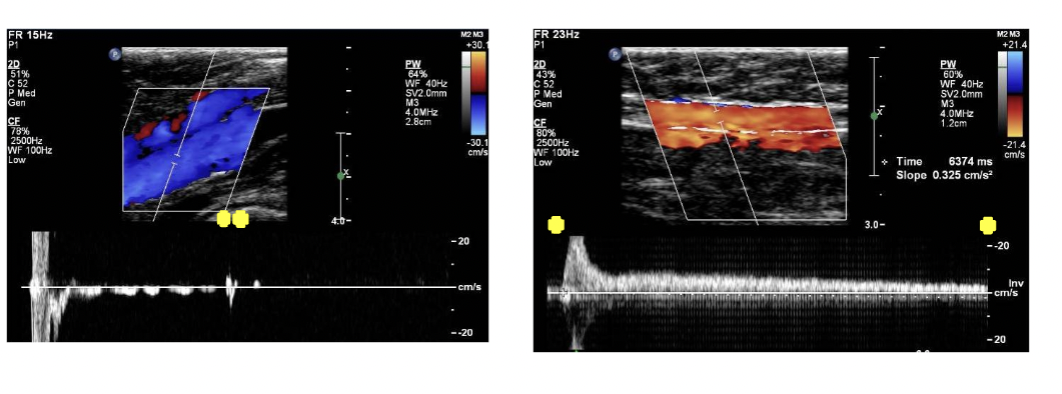
What is the criteria for venous insufficiency ( reflux)
normal valve closure <0.5 sec ( in left image)
Abnormal valve closure >0.5 sec ( in right image)
Blood flow stops flowing in a vein, becomes coagulated (semi-solid or solid state)
• Location of thrombus determines its name
• Age, location and occlusive nature of thrombus important to note ( if it’s newer it’s not as solid)
What is virchows triad
(trauma, stasis, hyper-coagulability) by having these three symptoms will increase their risk for venous thrombosis.
What are critical results
findings which need a physician to see the patient directly after the exam
These typically include:
• >5.0 cm AAA or >2.5 cm CIA or EIA aneurysm
• 80-99% ICA stenosis
• Acute DVT
• ABI below 0.3 with Acute Arterial Occlusion
REMEMBER: don’t give critical results to patients state something like this “ I want to make sure we have everything for the doctor, I’ll be right back”
What is a critical venous thrombus finding
Acute DVT
An Acute SVT that is:
• Extensive (bilateral full length of GSV)
• Near junction with deep vein (measure distance)
If you can’t get ahold of reading physician to report critical finding what would you do?
recall in 5 mins, if still no answer, contact your direct supervisor and transport patient to ED ( emergency department)
• Essential to not send a patient home with critical results
How do you determine DVT from SVT
Deep veins are near bones and typically have adjacent arteries, superficial veins are within fascial layer and do not have accompanying arteries
•Remember to look for anatomical variants
Bifid Femoral veins
Hypoplastic veins (smaller or not well developed veins) Does not mean they are superficial just because they appear small.
When do varicose veins develop, how do they appear?
When superficial venous valves are incompetent. Incompetent valves allow retrograde blood flow (reflux)
– Retrograde flow leads to venous hypertension in distal vein segments
– Varicose veins can occur in Deep veins, but this happens less often and they typically do not show superficially
• Veins with reflux appear ropy, protruding, and tortuous
• Can be painful and cause swelling
• Most commonly found in lower extremities
Whats the difference between competant and incompetant venous valves
Competent valves: 90mmHg in veins while standing to 20-30
mmHg while walking ( from a competent venous pump)
Incompetent Valves: Lead to persistent increased venous pressure
in calf veins due to retrograde blood flow (toward the foot)
• Results in soft tissue edema, skin thickening, hyperpigmentation and skin ulceration
Where is venous insufficiency more likely to occur? What veins are affected with venous ulceration?
More likely to occur in superficial veins than in deep veins
• If in deep veins, likely associated with chronic DVT. Will less likely appear superficially like when superficial veins are affected
– Symptoms: swelling, aching, pain
• Patients with venous ulceration following DVT, often have both deep and superficial venous reflux present
What is the venous disease progression
Veins visibly bulging
Leg swelling
Skin Discoloration
Ulcerations
Nonhealing ulcerations
( only gets to non healing ulcerations if no prevention is done)

What is the Clinical C classification ( for venous insufficiency) CEAP Classification ( only C category)
( shown in image)
C0: No clinical signs
C1: small varicose veins
C2: large varicose veins
C3: Edema
C4: skin changes without ulceration
C5: skin changes with healed ulceration
C6: skin changes with active ulceration.
What is clinical presentation for venous insufficiency
Patients often have pain, edema, dilated visible veins, skin changes near ankle, swelling in extremity, or a feeling of heaviness or aching with prolonged standing.
• Note that some patients may describe venous claudication- severe
cramping and burning pain with walking
Often associated with hypertension in both deep and superficial
venous systems and obstruction of iliofemoral vein in cases of poor
collateral pathways
Recall that hydrostatic pressure (typically 90mmHg) in the lower
extremities will not be alleviated as well with insufficiency even with calf pump assistance
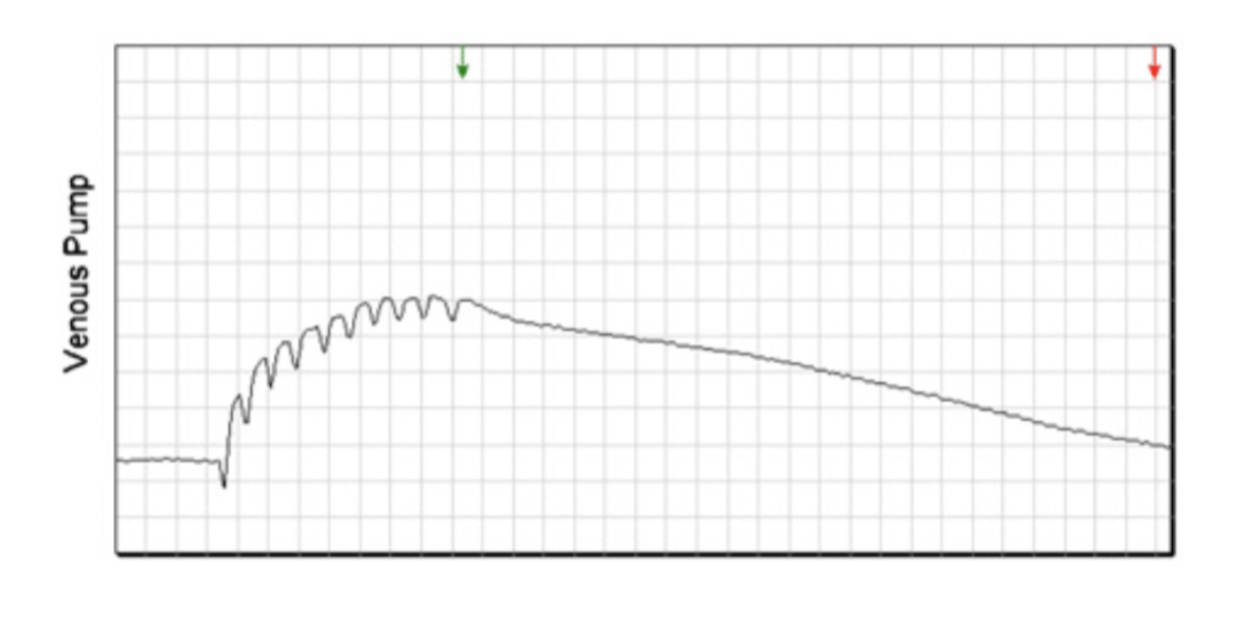
How does PPG test for Reflux, Whats the criteria?
Can use PPG probes to determine venous refill time (VRT)
• PPG is a measure of volume of blood flow in tissue (Less commonly used)
Place probe on distal GSV at medial malleolus and have patient perform dorsi flexion
Amount of time for veins to refill recorded ( image of a normal refill time is shown on term, abnormal is shown on definition card)
• Venous Refill Time Criteria:
– Normal >40 seconds
– Borderline 20-40 seconds
– Abnormal <20 seconds
What is LEV Insufficiency Exam Patient History Assessment
Risk Factors for DVT
• LE Trauma
• History venous ulcers or varicosities
• History vein surgeries or venous interventions
– Venous ablation
– Venous stripping
– Vein harvesting
– Iliac vein stenting (History of May Thurner’s Syndrome)
• Family history of venous thrombosis
Congestive Heart Failure (CHF)
What Instrumentation would you use for a LEV Insufficiency Exam
Usually use a 5-7 MHz linear transducer
May change depending on vein location for better visualization
More superficial veins may require higher frequency
Deeper veins may require lower frequency
• Rapid cuff inflator may be used instead of manual distal augmentation
Standardizes the compression of distal augment with predetermined
cuff size and mmHg over specified time
– May be ergonomically helpful, however only useful in thigh (for calf
measurements still need to distally augment)
Not all labs will have this device
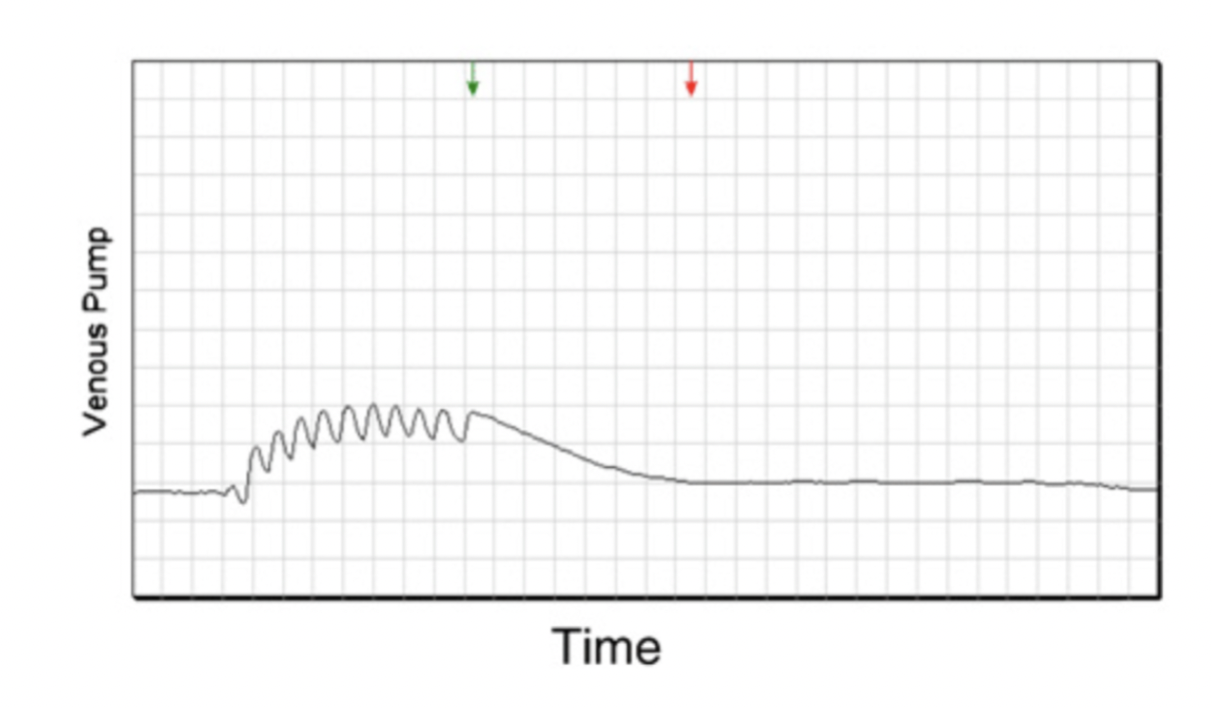
What is Patient Positioning for LEV Insufficiency
supine portion
• Reverse Trendelenburg (patient lies on back with head higher than the lower limbs. Head elevated 20 degrees)
Leg externally rotated
• For better visualization can use Prone position for
» POP Vein
» Prox PER and Prox PTV
» Soleal veins
» SSV
Dependent position (leg hanging off bed) ( to dilate calf veins (PTV and PER))
standing portion
• Leg externally rotated
• Care taken patient keeps weight on leg not being evaluated
– Allows for distal augmentations to be easier
What is protocol for second part of exam, (standing or in upright
position)
Bilaterally: Obtain 5 images:
• Venous Compression
• Color Doppler with distal Augment
• Spectral Waveform with Valsalva / proximal compression and
• Spectral Waveform with Distal Augment
• AP and width transverse measurments
– At the each of the following
• SFJ (sapheno-femoral junction)
• GSV thigh prox, mid and distal
• GSV knee
• GSV calf prox, mid and distal
• SPJ (sapheno-popliteal junction)
• SSV prox, mid and distal
• GIAC
What is the protocol for the First part of exam, complete LEV for Thrombus
• Bilaterally:
– Venous compressions from hip to ankle
– Obtain 4 images:
• Venous Compression
• Color Doppler with distal Augment
• Spectral Waveform with Valsalva / proximal compression and
• Spectral Waveform with Distal Augment
– At each of the following
• CFV
• PFV
• FV prox, mid and distal
• POP prox mid and distal
• PTV prox, mid and distal
• PER prox, mid and distal
• GSV thigh, knee and calf
• SSV calf
What is the protocol modification for venous insufficiency
While in Reverse Trendlenburg
– Assessment of deep veins for DVT and reflux :
• Bilateral CFV, FV, POP, PTV and PER
• Remember bilateral CFV part of every unilateral LEV
– Evaluate superficial veins for SVT and reflux:
• SFJ, GSV origin, prox thigh, mid thigh, distal thigh, kneed, prox calf, mid
calf, distal calf
• SPJ, SSV origin, prox calf, mid calf , distal calf
What would you do if the GSV and SSV are positive or negative for reflux?
if GSV and SSV positive for reflux in Reverse Trendelenburg position, then exam complete ( no need to go beyond this)
IF GSV or SSV negative for reflux in Reverse Trendelenburg,
then patient does standing portion, reassess junctions and or area of visible varicose veins for reflux
What are the two types of varicose veins
Primary: Direct or congenital failure of venous valves ( EX: injury)
Secondary: Failure of venous valves due to acquired condition
• EX: DVT, Pregnancy, Klippel-Trenaunay Weber (KTW) Syndrome
What are varicose vein symptoms
Visible bulging veins
• Heaviness in lower extremities
• Itchy
• With progression of reflux: you’ll see Skin discoloration and Venous stasis ulcerations
Where do most varicose veins (VV) originate
saphenous veins or saphenous branches
• Important to note valvular competency of
saphenous branches
GSV: Anterior lateral accessory saphenous and Posterior medial accessory saphenous
SSV: Giacomini
Posterior calf VV= SSV reflux
Medial thigh VV = GSV reflux
Medial calf vv GSV reflux (may also be calf perforator)
Anterior lateral thigh VV = AL Acc of GSV reflux
Posterior medial prox thigh vv= PM Accessory of GSV reflux
Posterior thigh vv= Giacomini reflux
For venous insufficiency what valve closure time is considered pathologic
Greater than 0.5 sec is considered pathologic
• Remember refluxing veins typically are larger than veins with competent valve
When documenting venous reflux what is important to add
specify specific location ( this determines intervention)
Finding source of reflux is important to treatment
• Junction, perforators, etc
Finding termination of reflux is important to treatment
– Multiple thigh vv, perforator, etc

What is KTW syndrome
Rare congenital condition
• Malformation of veins and lymph nodes
• Commonly presents with deep venous anatomy variations
– Ex: Hypertrophic Femoral vein with significant collaterals ( FV looks thick)
Patient may have: Port wine stains, Soft tissue Hypertrophy, AVMS (arteriovenous malformations), Varicose Veins, Variations in venous anatomy, Extra veins or absent veins
( port wine stain shown in image)
What is Venous Insufficiency Treatment
Limb Elevation: ( Legs elevated above heart after periods of prolonged standing or sitting)
Compression Therapy: ( Unna Boots and Compression Stockings
• Ask for RN assistance to remove Unna Boot prior to exam
– Patients frequently have ulceration under boot, Boot is meant to help heal the ulcer, Boot will need to be cut off to remove
Sclerotherapy: sclerosis= hardening of tissue, hardens vein walls to close it
• In office procedure, Injection of foam solution into vein to sclerose
• needle injection or catheter. Can be ultrasound guided or vein light guided
• Often treatment of choice for small veins (EX: reticular or spider veins and sometimes for perforators)
Ablation- Laser, RFA (Radiofrequency Ablation): Patient is awake, often no sedation given. Catheter based. Heat is applied directly inside refluxing superficial vein to close it.
• Either uses radiofrequency (RF) or laser energy to create the heat needed for the ablation. Sonographer ensures tip of catheter is approx. 2 cm away from deep vein in Sagittal view.
Surgery- Ligation: performed in the OR with patient under general
anesthesia. Refluxing superficial vein is cut at the junction and knee
and any branches are tied off.
Ablation procedure will leave vein and branches in place, while ligation
and stripping will remove it entirely
What is Phlebectomy, what is it used for
Can be done after ablation if there are remaining varicose veins that cause lingering symptoms, especially for the bulging superficial VV (Cosmetic reasons)
What is LE Vein mapping
The evaluation of a vessel course (pathway), patency (including wall condition) and diameter
• Mapping is usually a pre-surgical procedure to determine suitability of vessel for use as a bypass graft conduit, dialysis access fistula, or CABG
How do you determine if a vein is adequate for use as an arterial bypass graft?
To serve as bypass graft, vein needs to be large and patent. Too small a vein will not sustain arterial graft blood flow
Areas of decreased size create stenosis within graft
Occlusive or partially occlusive thrombus within vein will obstruct arterial graft blood flow
What is LEV Patient Positioning for vein mapping
Supine with leg rotated outwardly
– If needed for POP, PTV, PER or SSV you can use prone position
• Reverse Trendelenburg
• you need Warm room with limbs covered until imaging
( usually use a Linear 5- MHz transducer High frequency transducer may be needed for more superficial veins)
What is the LEV Mapping Protocol
• Venous compressions and Spectral waveforms with distal augment and Valsalva or proximal compression of the following
– CFV
– SFJ
– FV prox, mid and distal
– Popliteal vein
– PTV, PER
• Remember all LE venous exams (including unilateral) require bilateral CFV images
Then AP and Width diameter measurements of
– GSV origin
– GSV thigh (prox, mid, and distal)
– GSV knee
– GSV calf (prox, mid, and distal)
– SSV origin, prox, mid, and distal
What is the order of the LEV vein Preferred for LEA bypass ( In order of most preferred to least)
Same leg as bypass
• Typically GSV preferred over SSV (GSV is larger)
– Contralateral leg to planned bypass
– Arm vein
– Synthetic
When are tourniquets used
used for upper extremity vein mapping, Tourniquets are not used for Lower Extremity Vein mapping
What is the LEV mapping criteria
0.35 cm is considered adequate size of a vein for use as an arterial bypass graft
• to small will cause graft failure, so most important to note any areas that appear < 0.35 cm
what is patient positioning for UEV
Supine with head turned away from side examining for access to IJV and Subclavian vein
• Extend arm down bed or can use a pillow to support patient across lap if needed
For mapping want veins as large as possible:
– Limb in Dependent position ( below level of body)
– Warm patient- use blanket to cover limb prior to exam
– Tourniquet typically used on upper extremity
For UEV mapping how do you place a tourniquet
placed at upper arm, near axilla
• Tourniquet should be tightly placed around arm
• Avoid tying tourniquet into a knot, as gel will make untying difficult
CANT use a tourniquet on a patient with a history of ipsilateral mastectomy or lympadenectomy
How does the UEV mapping protocol change for Bypass or dialysis access
if mapping for peripheral vascular bypass or coronary artery bypass= only need to assess veins
If mapping for dialysis access= need to assess both arteries and veins
Regardless if the exam if unilateral or bilateral for UEV what do you always need to scan bilaterally
bilateral B-mode, Color Doppler and Spectral Doppler images of Subclavian veins are needed ( RT and LT)
How do you mark for UEV mapping
Best way to mark is use center of transducer as a guide
– Locate vessel in transverse
– Place vessel in center of image
– Make small dot with sharpie in center of transducer
• Straw occasionally helpful if sharpie unable to mark through gel, straw
makes indent while remove gel to place sharpie mark
– Connect dots to draw course of vessel
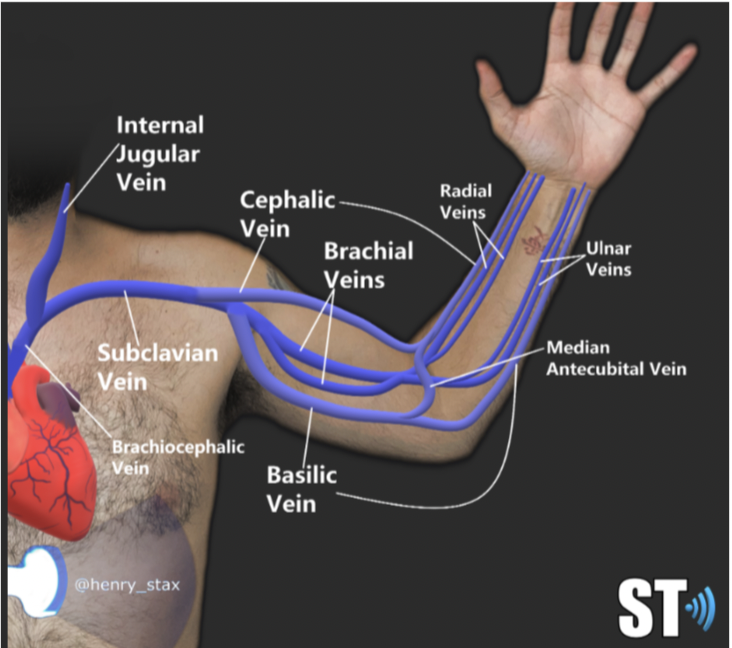
What is the UEV mapping protocol for UEV DVT assessment and UEV superficial vein mapping.
UEV DVT assessment
• B-mode, Color Doppler and Spectral waveforms of IJV, Innominate and Subclavian,
• Transverse compressions, Color Doppler and Spectral waveforms with distal
augmentation Brachial, Radial and Ulnar
UEV superficial vein mapping
• Transverse compressions and distal augmentation
• Cephalic vein
– Upper arm: proximal, mid and distal
– Elbow
– Lower Arm: proximal, mid and distal
• Basilic vein
– Upper arm: proximal, mid and distal
– Elbow
– Lower Arm: proximal, mid and distal
What is the criteria for UEV mapping, what would you do if the basilic and cephalic appear inadequate
Vein is considered adequate if
• Appears patent with no wall damage, No evidence of thrombosis or wall thickening
• Diameter greater than 0.4 cm for arterial bypass graft or 0.25 for dialysis
access
If both basilic and cephalic appear inadequate modify protocol with
addition to assess brachial veins
• Remember median cubital vein can connect upper arm cephalic
and upper arm basilic to form longer segment if needed
– Typically mapping upper extremity for bypass graft if lower extremity
veins were not adequate as typically bypass will be planned for lower
extremity
What is the cephalic vein a common location for, where does it originate and run
Originates from subclavian vein posterior to the clavicle
– Important to document cephalic arch diameter
• Common location for stenosis in dialysis access fistulas
Vein typically courses anterior along deltoid and anterior to
bicep muscle
– Be sure to note any deviation from common course on preliminary
report
How can you identify and scan the cephalic vein during an ultrasound exam
Use the thumb as a landmark—vein runs along the lateral portion of the arm
Look in the antecubital space to locate and follow it laterally
Extend the patient’s arm away from their body
Optional: place arm on a pillow
Ensure the arm is in a dependent position ( below body)
How can you identify and scan the basilic vein during an ultrasound exam?
Confluences with the proximal brachial vein in the upper arm, then enters fascial layer
Use the little finger as a landmark, vein runs along the medial aspect of both upper and lower arm
Start in the antecubital space and follow medially
May course posteriorly in the lower arm (note this in preliminary report)
Extend patient’s arm away from body
Optional: place arm on pillow
Keep arm in a dependent position
What are the UEV mapping considerations for different pre-op procedures?
For Arterial Bypass Graft or CABG (Coronary Artery Bypass Graft):
Only assess vein diameters
Lower extremity veins (especially GSV) are often mapped first
For Dialysis Access Fistula (Pre-op for CKD patients):
Assess vein and artery patency, course, and diameters
Fistula connects artery to vein, creating high-pressure system for repeated needle access
Used in chronic kidney disease patients with low renal function
Dialysis = external blood filtration, often 6 hours, 4 days/week
What are the UEV Mapping Protocol additions for mapping for placement of Dialysis Access
Obtain longitudinal B-mode, Color Doppler and Spectral waveform and transverse AP and width diameter of
– Subclavian artery prox, mid and distal
– Axillary artery
– Brachial artery prox, mid and distal
– Radial artery prox, mid and distal
– Ulnar artery prox, mid and distal
• Important to ensure adequate vein and artery diameters as well as no venous thrombosis or significant arterial stenosis that would compromise blood flow to a dialysis access
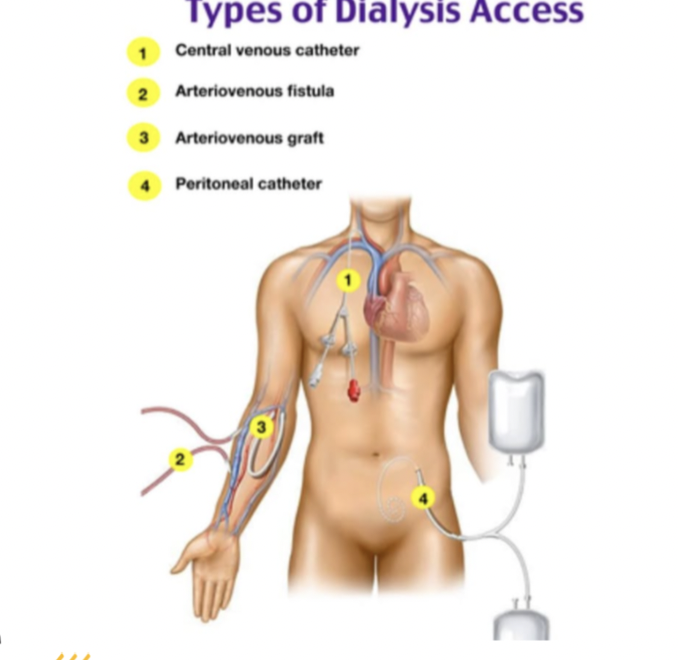
What are the types of dialysis access, and how does vein mapping help determine the method? ( UEV)
Dialysis Access Types:
Chest catheter
Upper extremity fistula (requires UEV mapping first)
Upper extremity graft
Lower extremity graft
Peritoneal dialysis (through abdomen)
Key Info:
Dialysis requires repetitive needle access into a vein + high pressure
AV Fistula (AVF): Native artery ↔ native vein
AV Graft (AVG/DAG): Native artery → synthetic graft → native deep vein
Vein Mapping Purpose:
Confirms if patient’s native vein is patent and large enough for a fistula
If too small, synthetic graft is used instead
What are the indications for vein mapping in a patient preparing for dialysis access?
Performed pre-op for dialysis access fistula planning
Assess arterial and venous diameters
Determine preference and feasibility of access sites
Possible Access Options:
Forearm Cephalic Vein Fistula
Non-dominant arm (preferred)
Dominant arm
Upper Arm Cephalic Vein Fistula (dominant or nondominant)
Upper Arm Basilic Vein Transposition Fistula (dominant or nondominant)
Forearm Loop Graft
Upper Arm Straight Graft
Upper Arm Loop Graft (axillary artery to axillary vein)
Lower Extremity Loop Graft (common femoral artery to vein
( if in yellow it uses both patients arteries and veins)
All of the above use the patients arteries
What is the Criteria for mapping for AVF (UEV)
Adequate vein diameter is 0.25 cm and greater
Adequate arterial diameter is 0.20 cm and greater
What is the "Fistula First, Catheter Last" campaign, and why is it important?
Promotes early placement of AV fistulas in patients with declining renal function
Goal: Have fistula ready and usable before dialysis is needed
Alternative: Central venous catheter (Subclavian or Innominate vein)
Higher risks: More prone to occlusion and infection
Encourages patients to meet with vascular surgeons early to avoid catheter use
What is UEV hemodynamics for inspiration and expiration
Inspiration: Increases venous return to right heart from upper
extremities
– Diaphragm lowers and decreases pressure in thoracic cavity
Expiration:
Decreases venous return to the right heart from upper
extremities
Diaphragm raises and increases pressure in thoracic
cavity
What is the UEV Protocol
B mode compression, Color Dolor and Spectral Doppler waveforms
with distal augment of
– IJV
– Innominate vein (Brachiocephalic vein)
– Subc vein at prox, mid and distal
– Axillary Vein
– Brachial Vein at prox, mid and distal
– Radial Vein
– Ulnar Vein
– Cephalic vein (upper arm prox mid and distal and lower arm prox mid
and distal)
– Basilic vein (upper arm prox mid and distal and lower arm prox mid
and distal)
Always do Bilateral SUBc veins even it’s a unilateral exam
What major vein can you locate by following the internal jugular vein (IJV) proximally toward the heart?
following the IJV proximally toward the heart, you can locate the innominate vein (also known as the brachiocephalic vein), which is also the origin of the subclavian vein
What is important to know about imaging the innominate (brachiocephalic) vein in upper extremity venous studies?
Also called the brachiocephalic vein
Cannot be compressed due to its location posterior to the sternum
Must rely on Color Doppler and Spectral Waveform analysis
Be sure to image the innominate vein proximal to the subclavian vein origin, not the subclavian vein itself
How is the subclavian vein evaluated in upper extremity venous (UEV) studies, and why is bilateral imaging important?
Bilateral subclavian vein spectral Doppler is required to compare waveform phasicity
Evaluates for proximal obstruction, especially since these veins are obstructed by the sternum
Compression is typically not possible due to the clavicle, so rely on Color Doppler and Spectral Waveforms
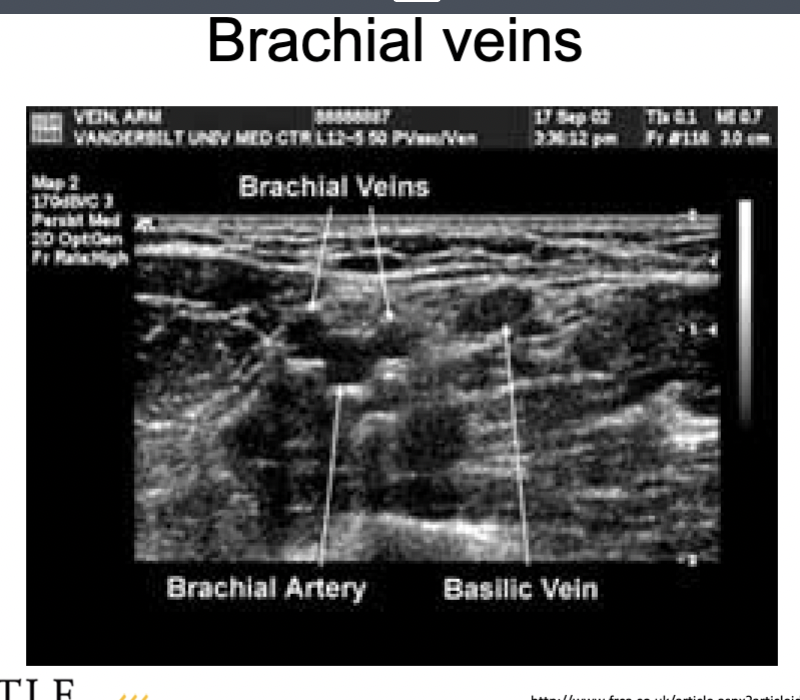
What are key ultrasound characteristics of the brachial veins in upper extremity venous studies?
Often paired but may have large branches
Always follow the brachial artery—brachial veins stay adjacent to it
Watch for the brachial nerve bundle and basilic vein
Basilic vein travels into the fascia layer without an accompanying artery
What should you know about imaging the axillary vein during an upper extremity venous (UEV) exam?
It’s the first compressible vein in the UEV protocol
Innominate, IJV, and Subclavian veins are typically not compressible
Diagnosis in non-compressible veins relies on hemodynamics (Color and Spectral Doppler)
Position the patient with arm extended and abducted for better access
Normal variant: Axillary vein may not lie directly adjacent to the axillary artery
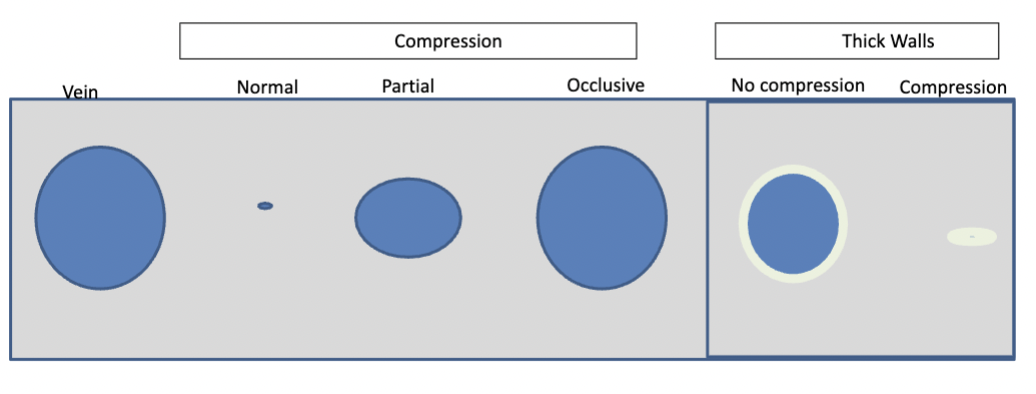
How would you asses vein patentcy through compressions
Transverse compressions throughout vein (every 2 cm ) to ensure no thrombus
present
• If wall appears uniformly thickened with no evidence of thrombus, note on the report “thick walls” vs partially incompressible
Possible causes of thickened vein walls: venous hypertension, inflammation from Behcet’s disease, phlebitis, or post-thrombotic syndrome
What considerations should be made during an upper extremity venous exam when a patient has a central venous catheter? ( venous thrombus from venous trauma)
Increased incidence of axillary and subclavian DVT due to central venous catheters (e.g., PICC lines, dialysis catheters)
Do not disturb catheters to avoid infection risk
Document in report: “Cannot visualize proximal subclavian and innominate vein due to right shoulder catheter”
IVs can commonly cause superficial venous thrombosis (SVT)

Whats being shown in this image, what does this indicate
small varicosities indicative of DVT. Likely indicative of Axillary or Subclavian obstruction as small collaterals enlarge to reroute blood blocked by obstruction
What is Paget-Schroetter Syndrome and how does it typically present?
Also called Effort Thrombosis
Most common cause of axillary-subclavian DVT in outpatient settings
Caused by repetitive motion injury or clavicle impingement, sometimes linked to cervical rib abnormalities
More common in men and in the dominant arm
Symptoms: Arm pain and swelling, may be acute or vague/subtle
A form of venous thoracic outlet syndrome (TOS)
What are key sonographic and treatment considerations for Paget-Schroetter Syndrome?
Clavicle may limit visualization, so rely on Spectral Waveform analysis
Do not abduct the arm during exam—abduction may cause continuous waveforms that mimic proximal obstruction
Treatment options:
Anticoagulation therapy
Thrombolysis
First rib resection (decompression)
Balloon angioplasty
What is Superior Vena Cava Syndrome (SVCS), and how is it caused, diagnosed, and treated?
Definition: Compression of the Superior Vena Cava (SVC)
Causes:
Thoracic cancers
Repeated central venous lines
Compression by nearby structures
Symptoms:
Gradual onset of facial and arm swelling
Heaviness in upper extremities
Visible collateral veins on skin
Coughing, dyspnea, lightheadedness, confusion
Diagnosis:
Use Spectral Doppler of bilateral subclavian veins
Minimal, monophasic waveforms
Low amplitude with little cardiac influence
Direct SVC visualization is difficult due to its location behind the sternum
Treatment:
Venography with balloon stenting
Post-op success = return of respirophasic waveforms with normal amplitude in both subclavian veins
What is a fibrin sheath, and how is it identified and managed in vascular imaging?
A fibrin sheath forms around central lines, catheters, and ICD leads
Commonly seen in the internal jugular (IJ) and subclavian veins
Can disrupt venous flow
Not a thrombus, but a collection of fibrin that remains even after catheter removal
Should be documented with cine loops and monitored over time
Contrast-enhanced catheter venography is the gold standard for official diagnosis
What is Hemodialysis?
Minimally invasive procedure
• Cleans excess fluid and waste material from the blood through
a semi-permeable membrane
– Known as a “dialyzer”
• Bridge to transplant for renal failure patients
Why is dialysis needed?
Patients who undergo dialysis are unable to adequately excrete
waste products through urine
• Without dialysis patients will:
– Experience azotemia (build up of waste in the blood)
– Experience uremia ( ill feeling secondary to azotemia)
– Eventually pass away
• Patients are weighed before and after dialysis with measurable
weight loss following procedure
Whats the difference between fistula and graft
Fistula = patient’s native artery and vein
Graft= patient’s native artery and synthetic vein material
If you don’t know, “dialysis access” refers to either
• Vein mapping determines if a patient’s own vein is patent and large enough for a dialysis fistula, if too small then synthetic material used instead
What patient history factors affect the selection of location and type of dialysis access?
A new access cannot be placed distal to an old one
Previous grafts may cause stenosis (possibly why a new access is needed)
Increased risk of infection near previous access
Compromised venous flow can lead to swelling and reduced dialysis efficiency
Surgery is more complicated in areas with previous access
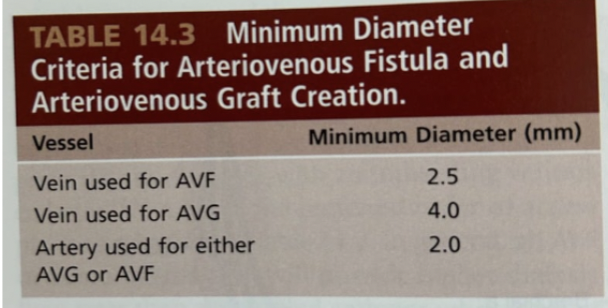
What is the selecting criteria for dialysis access
Non-dominant arm used first
• Vein diameter >0.25cm
• Arterial inflow adequate
– >0.2 cm with no significant stenosis
What are AV fistulas advantages and disadvantages
Native artery and native vein
Advantages: Lower infection rate, Higher blood flow rates, Lower thrombosis/stenosis rates
Disadvantages: Longer maturation time (time before it can be used for dialysis), Potential for steal syndrome, Aneurysmal formation
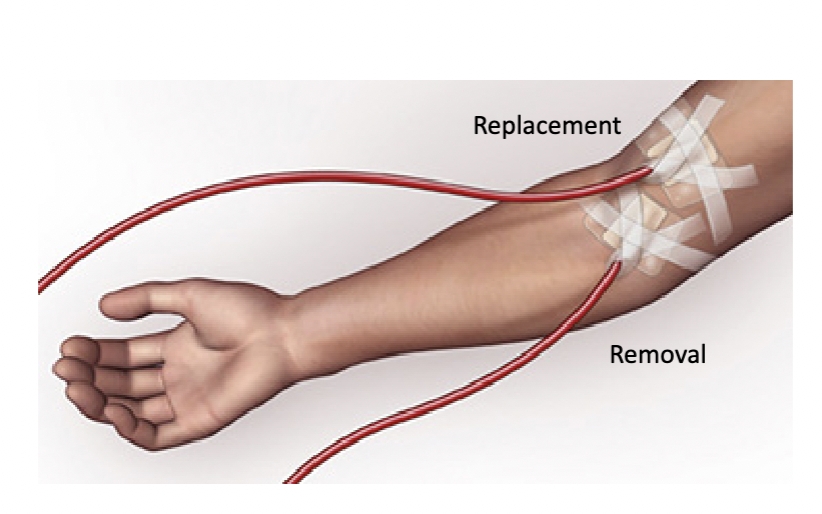
How is dialysis performed using a fistula or graft?
Two large-gauge needles are inserted into the fistula or graft
The distal needle removes blood and sends it to the dialysis machine
The proximal needle returns the cleaned blood to the body
Needles puncture only the vein or graft material, not the artery
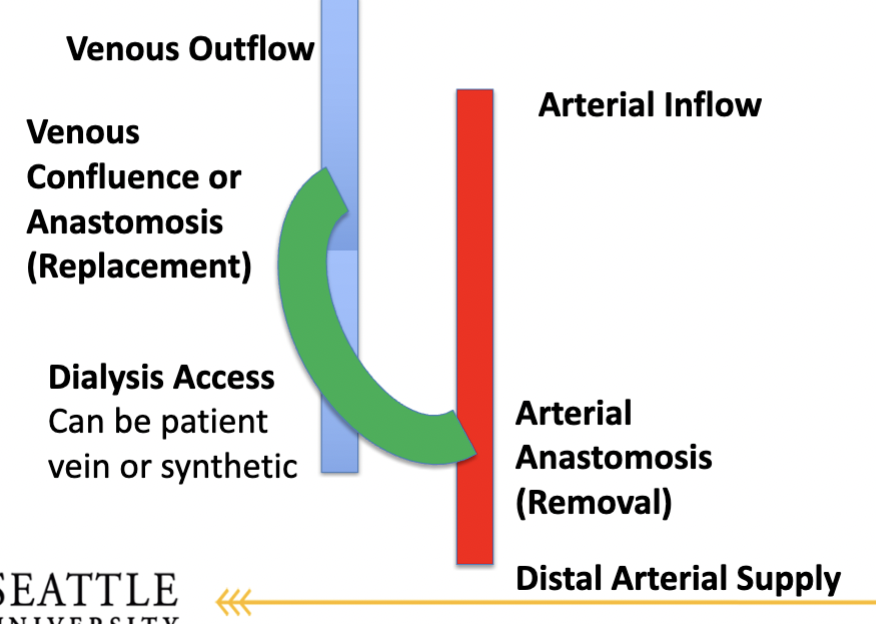
What structures are involved in dialysis access, and how is it similar to an arterial bypass graft? What does the distal part do?
Involves an arterial anastomosis (where blood is removed from the artery and enters the graft or fistula)
Involves a venous anastomosis (where blood returns from the graft into the vein)
Can use a patient’s vein or synthetic graft
Has both a proximal anastomosis (near the heart, for blood entry into the graft) and a distal anastomosis
What does the distal part do?
The distal anastomosis refers to the artery beyond the access site, which supplies blood to the hand or lower extremity
It’s crucial to assess this area because dialysis access can steal blood from distal circulation, potentially leading to hand ischemia (steal syndrome)
What are the 4 key areas to evaluate in dialysis access hemodynamics?
Arterial inflow
Dialysis access (graft or vein)
Venous outflow
Distal arterial supply
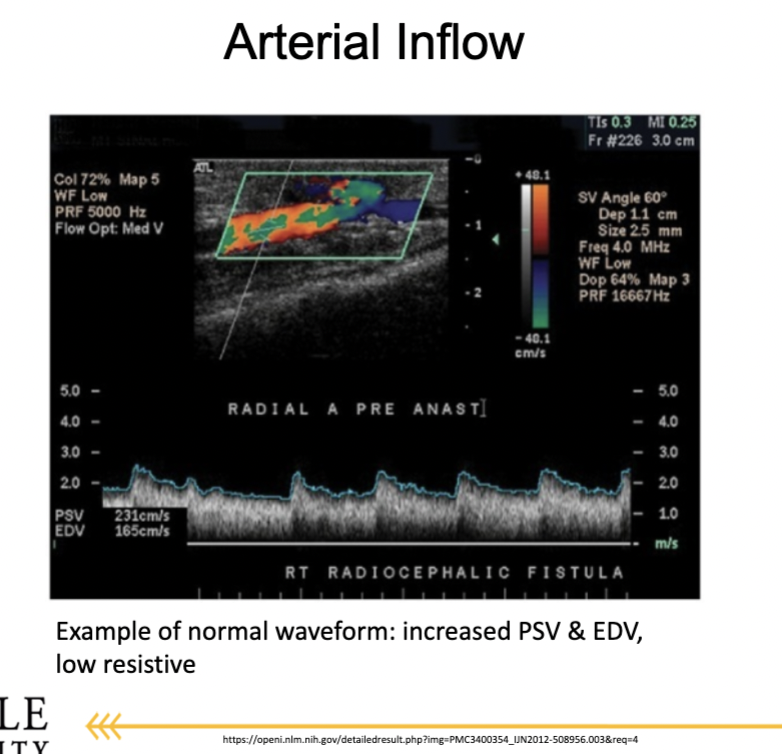
What should arterial inflow and venous outflow waveforms look like in a functioning dialysis access?
They should be inverse waveforms of each other due to the loop created by the access, assuming no obstruction
What arteries are evaluated for arterial inflow in dialysis access, and how are they affected?
Start evaluation at the subclavian artery and follow down to the proximal access anastomosis
All arteries proximal to the access are affected by the dialysis circuit:
Upper arm access: subclavian, axillary, brachial
Forearm access: subclavian, axillary, brachial, and radial or ulnar artery
What are normal and abnormal arterial waveform findings near a dialysis access?
Normal: Low-resistive waveform with increased diastolic flow and elevated peak systolic velocity
Abnormal: High-resistive waveform may suggest distal access obstruction