Ch 51: Alterations in Musculoskeletal Function; Trauma, Infection, and Disease
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
52 Terms
What is osteomyelitis?
Severe pyogenic infection of bone and local tissue
Inflammation (itis) of the bone (osteon) marrow (myelo)
Describe the ways that the organism can reach the bone? Provide examples.
Bloodstream → infectious agent is introduced by blood from infection elsewhere in the body
Adjacent soft tissue → caused by burns, sinus disease, trauma, malignant tumor necrosis, periodontal infection, infected pressure ulcer
Direct introduction of organism → direct infection causes open fracture, penetrating wounds, surgical contamination, or insertion of prostheses, metal plates, or screws
In which type of diseases or populations can you expect osteomyelitis to occur?
Children < 16 y/o (avg age 6 y/o) and elderly
IV drug users
Indwelling intravascular catheters/central line
Diseases:
Sickle cell anemia
Chronic granulomatous disease (Sarcoidosis, Chron’s disease, TB, etc.)
What are the most common pathogens for osteomyelitis?
Staphylococcus aureus followed by Streptococcus Pneumoniae
What are the clinical manifestations for children with osteomyelitis?
High fever and pain at the sight of bone development
What is Brodie abscess?
Subacute osteomyelitis → localized infection enclosed by fibrotic tissue
What are the clinical manifestations for adults with osteomyelitis?
Fever
Malaise
Anorexia
Night sweats
Weight loss
What are the potential healing complications with osteomyelitis?
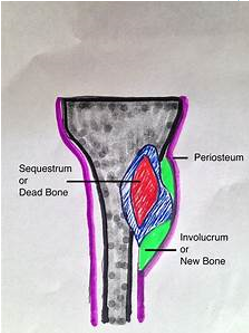
If osteomyelitis not managed or if treatment not sufficient → necrotic bone separates from healthy bone into dead segments → sequestra → chronic osteomyelitis
Abscess, or chronic infection may occur
Involucrum → prevents successful effects of antibiotics
What is the treatment for osteomyelitis?
4 to 6 weeks of antibiotic therapy (IV)
Abscess formation may require debridement
Amputation
What is scoliosis?
Lateral curvature of the spine (10° or higher)
S- or C-shaped
Idiopathic or
Consequence of
Congenital disorder (Hemi-vertebrae)
Connective tissue disorder (Marfan’s Sx)
Neuromuscular disorder (Cerebral palsy)
What are the clinical manifestations for scoliosis?
Appears after puberty
Asymmetry of shoulders, hips, chest wall
Possible respiratory problems
GI dysfunctions
Describe nonstructural scoliosis.
Resolves when the patient bends to the affected side
No vertebral rotation or bony deformity of the vertebrae is present
Can be related to postural problems, inflammation, or compensation due to leg discrepancy
Describe structural scoliosis.
Fails to correct itself on forced bending against the curvature and has vertebral rotation
Involves deformity of the vertebrae and asymmetric changes in hip, shoulder, and rib cage positions
Is scoliosis progressive? (note: one classification is progressive and the other is not)
Nonstructural scoliosis → NOT progressive
Structural scoliosis → PROGRESSIVE
What is the treatment for scoliosis?
Bracing
Exercises
Surgical interventions with spinal alignment
≥ 40-50 °
What is the most common metabolic bone disease?
Osteoporosis
What influences the rate of bone loss?
Genetics
Estrogen level
Family Hx
When does osteoporosis occur?
When the rate of one resorption is greater than that of bone formation
Normal osteoblastic and osteoclastic balance is disrupted
Mineral and protein matrix components are decreased
Leads to fragile bone → fractures
What are the risk factors of osteoporosis?
Family history
Estrogen deficiency
Small frame
Caucasian or Asian race
Menopause
Disease (Cushing dx, scurvy [vit. C. def.)
What are the clinical manifestations of osteoporosis?
Shortened stature
Muscle wasting
Back muscle spasms
Difficulty bending over
Fractures ( Colles fracture of wrist, vertebral compression fracture)
Kyphosis
How is osteoporosis diagnosed?
Based on graduations of bone mineral density (BMD)
Measured by dual energy x-ray absorptiometry (DXA)
T-scores
What does a T score of greater than or equal to -2.5 indicate?
Presence of osteoporosis
What does a T score between -1.0 and 2.5 indicate?
Osteopenia (low bone density/mass)
How is osteoporosis treated?
Calcium and vitamin D supplements
Exercise (weight-bearing)
Bisphosphonates (Alendronate → antiresorptive agent)
Recombinant human parathyroid hormone (anabolic agent/building)
What is the difference between rickets and osteomalacia?
Rickets:
Deficits in mineralization of newly formed one matrix in the growing skeleton (children)
Before puberty
Osteomalacia:
Deficits in mineralization of newly formed bone matrix in the mature skeleton (adults)
After puberty
What are the clinical manifestations of rickets and osteomalacia?
Kyphosis (hunchback)
Genu valgum → knock knee (inward knees)
Genu varum → bow leg
Pain in adults
What causes rickets and osteomalacia?
Inadequate concentration of
Vitamin D
Calcium or phosphorus
Poor vitamin D metabolism
Renal disease
How are rickets and osteomalacia treated?
Supplementation with vitamin D, calcium, and/or phosphorus
What is multiple myeloma?
The most common primary tumor of bone
Slowly growing bone marrow malignancy
What organs/systems does multiple myeloma affect?
Kidneys
Immune system
Circulatory system
What are the clinical manifestations of multiple myeloma?
Bone pain is a predominant symptom
Pathologic fractures & hypercalcemia
Kidney dysfunction
Neurologic symptoms
Unexplained anemia
How is multiple myeloma diagnosed?
Homogenous immunoglobulin is present in urine and serum
Bone marrow aspiration and biopsy
Imaging tests
How is multiple myeloma treated?
Aggressive combination chemotherapy
Local radiation
Survival >2-3 years → <10%
What is muscular dystrophy?
Group of genetically determined myopathies characterized by progressive muscle weakness and degeneration
Muscle tissue is replaced by fat and fibrous connective tissue
How is muscular dystrophy classified?
Classified by the pattern of
Inheritance
Age of onset
Distribution of muscular weakness
What is the etiology and pathogenesis of Duchenne muscular dystrophy?
Inherited as X-linked trait (only in MALES, especially boys)
Muscle cells deficient in the protein dystrophin → weakens cell membrane → allows extracellular fluid to leak into cell → muscle necrosis and degeneration
What are the clinical manifestations for Duchenne muscular dystrophy?
Diseases begins at birth and is usually apparent by age of 3
Calf muscles enlarged due to
Infiltration of fat cells and
Degeneration of muscle fibers
Distal muscle involvement leads to:
Frequent falling by the age of 5 or 6
Most children are confined to a wheelchair by ages 12-14 years old
How is Duchenne muscular dystrophy treated?
Appropriate education of patient and family
Corticosteroid therapy and preservation of function
What is myasthenia gravis?
A chronic autoimmune disease
Affects neuromuscular function of voluntary muscles
Characterized by muscle weakness and fatigability
What is the etiology of myasthenia gravis?
Acetylcholine receptor antibodies are produced → destroys or blocks acetylcholine receptors of the muscle end-plate of neuromuscular junction → impair the transmission of acetylcholine activity across the junction → muscle weakness and fatigability
What is the pathogenesis of myasthenia gravis?
Myasthenia crisis
A complication of myasthenia grave that can result from insufficient medication, emotional stress, trauma, infection, or surgery
Sudden increase in BP and pulse
Is myasthenia gravis more common in men or women?
Women
What age is the peak onset of myasthenia gravis?
20-30 years old
What are the clinical manifestations of myasthenia gravis?
Painless muscle weakness
Begins with ocular and cranial muscles
Proximal limb muscles
Improves by rest and exacerbated by repetitive use
What is the treatment for myasthenia gravis?
Anticholinesterase inhibitors
Corticosteroids
IV immunoglobulin
Plasmapheresis
Immunosuppressive agents
Thymectomy if no response to medications
What is myasthenia crisis?
A complication of myasthenia gravis
What is the etiology of myasthenia crisis?
Insufficient medication
Emotional stress
Trauma
Infection
Surgery
What are the clinical manifestations of myasthenia crisis?
Sudden increase in BP and pulse
What is cholinergic crisis?
A complication of myasthenia gravis
What is the etiology of cholinergic crisis?
Excessive medication being given to patients with myasthenia gravis
What are the clinical manifestations for cholinergic crisis?
Fasciculations, especially around the mouth
Involuntary rapid muscle twitches that are two weak to move a limb but are easily felt by patients and seen or palpated by clinicians
Do you know SLUDGE?