5.10. Impaired metabolism of carbohydrates, lipids, and bilirubin. Diabetes mellitus. Morphology of alcoholism quiz
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
What are the accumulating substances, their localization and Pathogenesis mechanisms
Substance types:
Normal (e.g. fat, water, protein) in excess
Abnormal (e.g. pigments, drugs)
Locations:
Intracellular
Interstitial
Inside hollow organs
Mechanisms:
Increased intake/synthesis
Impaired degradation or excretion
What is lipidosis and define the different forms of it
Subtype | Description | Example |
Steatosis | Triglycerides in parenchymal cells (like liver, heart) | Fatty liver (hepatic steatosis) |
Obesity (Adipositas) | Triglycerides in adipocytes (fat cells) | Visceral and subcutaneous fat expansion |
Systemic lipidosis (Tesaurismosis) | Lipid accumulation in macrophages | Gaucher’s disease |
Cholesterol crystals in arteries | Leads to atherosclerosis | CAD, stroke risk |
Cause and macro/microscopic findings in steatosis
Cause: Hypoxia (e.g., heart failure), toxins (e.g., alcohol, CCl₄), obesity
Macroscopic: Yellow, greasy, enlarged liver
Microscopic: Clear vacuoles in hepatocytes (fat droplets)
Cause and macro/microscopic findings in cardiac steatosis
Caused by chronic hypoxia, malnutrition (e.g., cachexia, diphtheria)
Macroscopic: Tiger-striped heart (yellow streaks in myocardium)
Microscopic: Vacuolated cytoplasm in cardiac muscle cells
What is obesity (adipositas), etiology localization and complications
Definition: Generalized increase in adipose tissue mass.
Etiology:
High-calorie diet (especially saturated fats)
Endocrine disorders (e.g., Cushing’s)
Genetic and hypothalamic dysfunction
Localization:
Subcutaneous fat (under skin)
Visceral fat (around organs: liver, heart, intestines)
Complications:
Metabolic: insulin resistance → diabetes mellitus type II
Vascular: atherosclerosis, hypertension
Biliary: ↑ cholesterol → gallstones

What is this
Cardiac Obesity (Fatty Heart)
Seen in advanced obesity
Excess epicardial fat may compress coronary arteries
Heart may appear large, with thick fat covering
Which disease can be caused by cholesterol and cholesterol esters and what are they
Location | Condition |
Arterial walls | Atherosclerosis (plaques with lipid cores) |
Skin & tendons | Xanthomas (yellow plaques, often in hyperlipidemia) |
Gallbladder submucosa | Cholesterolosis (foamy macrophages in mucosa, “strawberry gallbladder” |
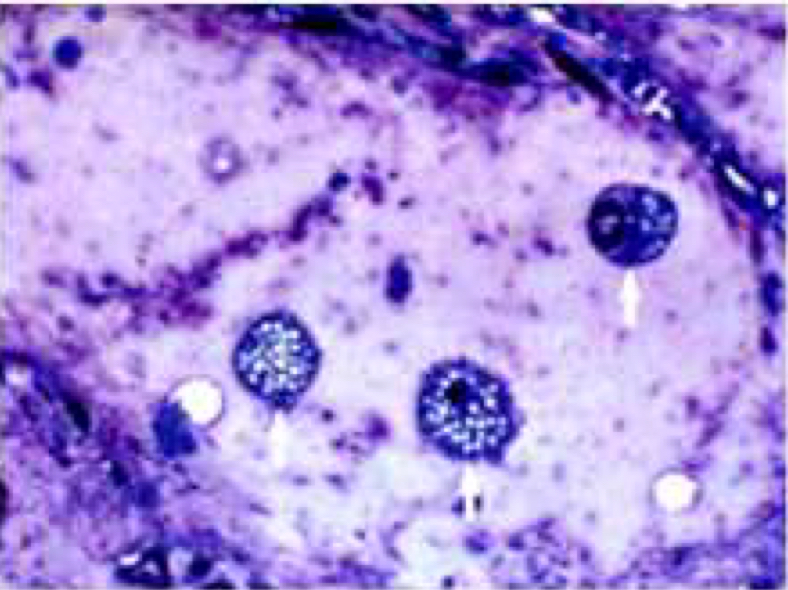
What are the arrows pointing at?
Foamy macrophages: Lipid-laden phagocytes seen in atherosclerosis and xanthomas
What is jaundice?
Jaundice = yellow discoloration of skin and sclera due to dissolved bilirubin or increased amount of bile pigments in blood or tissue fluids
What are the types of jaundice
Type | Site | Bilirubin Type | Mechanism |
Prehepatic | Before liver | unconjugated | Hemolysis → overproduction |
Hepatic | In liver | unconjugated or both | Impaired uptake, conjugation, or excretion |
Posthepatic | After liver | conjugated | Obstruction (e.g., gallstones, tumor) |
What are stones and why do they form?
Stones (s. concretions, calculi)– accumulations of salts in cavities or excreting ducts.
Stones form in ducts/organs due to:
Supersaturation of salts (e.g., Ca²⁺, uric acid)
Formation of a nucleation center
Stasis or impaired excretion
Name the different localization of stones
Location | Stone Name |
Gallbladder | Cholelith (gallstone) |
Kidney/UT | Urolith (renal stone) |
Salivary glands | Sialolith |
Pancreatic duct | Pancreolith |
Appendix | Coprolith (hard fecal mass) |

What’s this
Urate stones: Radiolucent, linked to gouT
what are the morphological features of stones
Any shape, consistency and color
Gall stones → round or cube-shaped with smooth surface, black, dark green or yellowish
Kidney stones → calcium, phosphate, oxalate, uric acid, with rough surface, can acquire the form of calyces and pelvis
What are langerhans islets and their functions
Langerhans islets are clusters of endocrine cells scattered throughout the pancreas.
They make up about 1–2% of the pancreatic mass but are vital for glucose homeostasis.
What are the cell types in langerhans islets and what is their functional role
Cell Type | Hormone | Function |
β-cells (70%) | Insulin | Lowers blood glucose by increasing uptake into tissues |
α-cells (20%) | Glucagon | Raises blood glucose by stimulating glycogenolysis and gluconeogenesis |
δ-cells | Somatostatin | Inhibits both insulin and glucagon |
PP cells | Pancreatic polypeptide | Regulates pancreatic secretion activity |
ε-cells | Ghrelin | Appetite regulation |
Functional Role:
These endocrine cells sense blood glucose levels and adjust hormone secretion accordingly.
Disruption in β-cell function or mass is central to diabetes mellitus.
What is diabetes mellitus
A group of metabolic disorders characterized by the common feature of chronic hyperglycemia, resulting from:
Defective insulin secretion
Defective insulin action
Or both
What is type 1 diabetes mellitus, cause, Pathogenesis and morphology
Type I Diabetes Mellitus
Also called: Juvenile or insulin-dependent diabetes
Cause: Autoimmune destruction of β-cells → absolute insulin deficiency
Pathogenesis: Often involves HLA-linked immune response with T-cell–mediated insulitis
Morphology:
Early: No gross changes
Later: Lymphocytic infiltration in islets (insulitis)
Islets may become atrophic or disappear
What is type 1 diabetes mellitus, cause, risk factors, Pathogenesis and morphology
Type II Diabetes Mellitus
Also called: Adult-onset or non–insulin-dependent diabetes
Cause: Combination of insulin resistance and relative insulin deficiency
Risk factors:
Obesity
Sedentary lifestyle
Genetic predisposition
Gestational diabetes
Morphology:
Gross: Pancreas appears more lobulated
Microscopy:
Atrophy of islets
Amyloid deposition in and around islets (derived from islet amyloid polypeptide or IAPP)
Fewer β-cells
What are other diseases that can cause diabetes mellitus
Exocrine pancreas diseases: pancreatitis, neoplasms, cystic fibrosis
Endocrine disorders: Cushing’s syndrome, acromegaly, pheochromocytoma
Hormonal drugs/agents: glucocorticoids, thyroid hormones, interferon-α
Genetic syndromes: Down, Klinefelter, Turner syndrome
What is gestational diabetes
Gestational Diabetes
Occurs during pregnancy due to placenta producing hormones that inhibit the the functioning insulin → blood glucose is increased
Resolves postpartum in most cases
Increases risk of developing Type II DM later in life
Morphologcial features of pancreas in diabetes type 1
Type I DM
:
Early stages: no gross changes
Later:
Lymphocytic infiltration of Langerhans islets (insulitis)
Progressive β-cell destruction
Remaining islets may appear atrophic
What vascular injuries can be caused by diabetes mellitus (glucotoxicity)
Chronic high blood sugar leads to:
Non-enzymatic glycation of proteins → reduced elasticity, protein trapping
AGEs (Advanced Glycation End-products) promote inflammation, stiffening
Oxidative stress → endothelial cell injury
Smooth muscle proliferation → vascular wall thickening
↑ TGF-β → excessive basement membrane material
What types of vascular injuries in diabetes mellitus
Macroangiopathy
Affects large & medium arteries
Accelerates atherosclerosis
Major complications:
Coronary arteries → Myocardial infarction
Cerebral arteries → Stroke
Peripheral arteries → Gangrene of extremities (diabetic foot)
Microangiopathy
Affects capillaries and small arterioles
Key features:
Thickened basement membranes
Reduced capillary function
Organs:
Kidneys → diabetic nephropathy
Retina → diabetic retinopathy
Peripheral nerves → diabetic neuropathy

What is this disease called
Diabetic macroangiopathy: atherosclerosis of coronary arteries may lead to myocardial infarction

What is this disease called
Diabetic macroangiopathy: diabetic foot–focal necrosis of soft tissues of lower extremities due to atherosclerosis and polineuropathies
Ischemia + peripheral neuropathy → tissue necrosis
May develop ulcers, infection, gangrene
Risk of amputation

What is this disease called
Diabetic microangiopathy: Injury of small renal blood vessels and capillaries
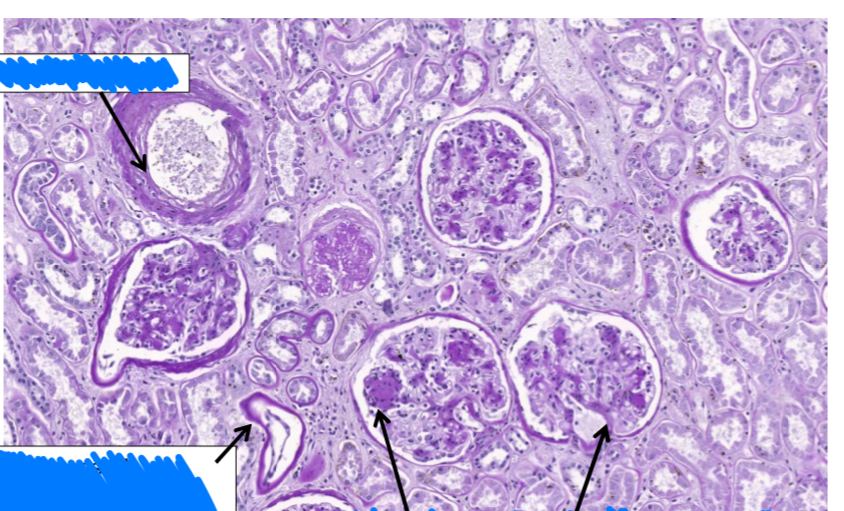
What does this slide show
Microscopy (PAS stain):
Arteriolosclerosis: hyaline thickening of small arteries
Tubular damage: thickened basement membranes
Glomerulosclerosis:
Mesangial matrix expansion
Sclerosis (e.g., Kimmelstiel-Wilson nodules)
Morphological features of alcoholism in the nervous system
NERVOUS SYSTEM
Alcoholic encephalopathy
Memory loss, confusion, ataxia
Wernicke’s encephalopathy (due to thiamine deficiency):
Classic triad: confusion, ophthalmoplegia, ataxia
Peripheral neuropathy
Demyelination of nerves
Burning, numbness, weakness in extremities