mechanics of breathing
1/42
Earn XP
Description and Tags
block 2 week 1 ctb
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
43 Terms
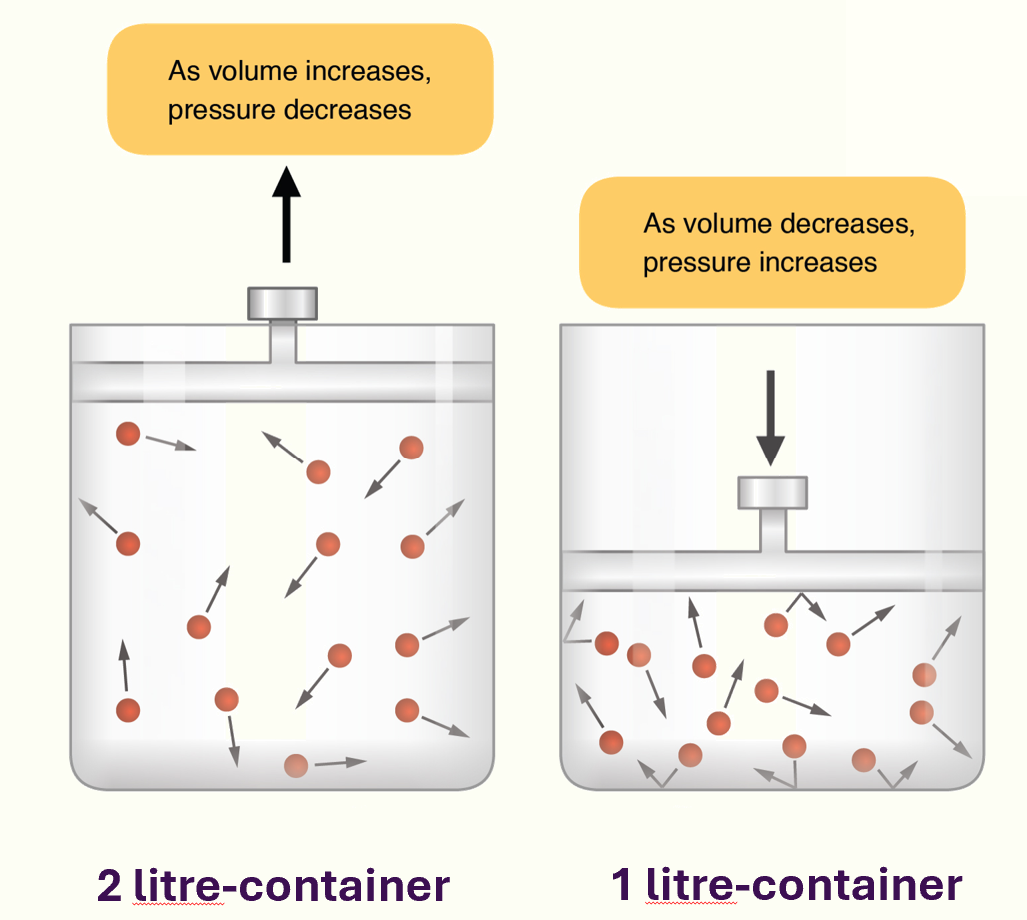
Boyle’s Law
at a given temperature, the pressure and volume of an ideal gas are inversely proportional
air flow
air moves by bulk flow down a pressure gradient: high pressure → low pressure
airflow achieved by creating a pressure gradient with the air around us
an INCREASE in lung volume DECREASES pressure, air flows in
a DECREASE in lung volume INCREASES pressure, air flows out
tidal breathing
quiet breathing at rest
tidal breathing: inspiration
contraction/flattening of the diaphragm INCREASES thoracic volume
contraction of external intercostals → rib cage moves upwards and outwards
tidal breathing: expiration
passive
muscle relaxation and elastic recoil of the lungs
forced inspiration
involves accessory muscles of respiration
accessory muscles are not primarily involved in respiration but act to enlarge the ribcage in any way possible, to increase the amount of air breathed in
greater contraction of external intercostals: they raise ribs to a greater extent than in quiet inspiration
forced breathing occurs when demand for oxygen is high (eg exercise, diseased states, singing)
lateral and anteroposterior diameter of thorax is increased
joints between posterior ends of the ribs and the transverse processes of the vertebrase enable lower ribs to swivel upwards and outwards to increase lateral diameter of chest (bucket handle effect)
sternocleidomastoid muscle and neck scalene contraction: raise ribs
tripod sign: arms planted, shoulder girdle fixed and pectoralis major and latissimus dorsi pulls chest outwards (sign of resp distress when displayed at rest)
forced expiration
active process
abdominal muscles contract, increasing intrabdominal pressure
forced abdo organs up against diaphragm (helps to decrease volume of the thoracic cavity)
contraction of internal and innermost intercostal muscles, displacing ribs down and back to decrease volume of the thorax
pleura
serous membrane that covers lungs and thoracic cavity
similar to peritoneal coverings in abdomen (in lungs: referred to as pleura)
visceral pleura = layer that covers lungs:
visceral pleura adheres tightly to lung tissue at reflects back on itself at hilum to become parietal pleura
parietal pleura = lines the mediastinum, diphragm and ribcage
between visceral and parietal pleura = pleural cavity/pleural space
pleural space/pleural cavity
contains few mm of pleural fluid (which acts as lubricant)
pleural layers can only be separated by considerable force but they can slide over each other easily
pleural space is held at NEGATIVE PRESSURE
-ve pressure is key in preventing pneumothorax
pressures
atmospheric pressure (PB)
alveolar (intrapulomary or intralaveolar pressure) (PA)
intrapleural pressure (PIP)
atmospheric pressure (PB)
pressure exerted by weight of the atmosphere
at sea level: 101.3 kilopascals
relatively constant so referred to as being ‘zero cm of water’
pressures > atmospheric pressures = positive
pressures < atmospheric pressures = negative
alveolar (intrapulomary or intralaveolar pressure) (PA)
prsssure inside the alveoli
must be equal to atomospheric pressure at the end of inspiration and expiration
intrapleural pressure (PIP) definition
pressure within the pleural space (between parietal and visceral pleural layers)
intrapleural pressure
opposing forces of outward recoil and inward recoil of the lungs pull the pleural layers apart
the 2 opposing forces pull the visceral and parietal layers apart and mean that the pleural space has a -ve pressure
intrapleural space is subatmospheric: a vacuum is created
during breathing, intrapleural pressure changes by becoming more or less -ve, which affects volume of the lung tissue
transpulmonary pressure (TPP)
alveolar pressure - pleural pressure = TPP
it is a transmural pressure (pressure across a wall)
if TPP is +ve, it acts as an expanding pressure on the lungs
after expiration, the alverolar pressure will be zero (same as atomospheric pressure) and intrapleural pressure will be -5cm of water
therefore TPP will be +5cm of water
helps hold lungs partially expanded
TPP is the force resisting the inward elastic recoil of the lungs
the greater the TPP, the greater the lung volume up
as TPP increases, lungs will expand further
tidal inspiration
↑ thoracic cavity volume
↑ pleural space volume
↓ intrapleural pressure (becomes more -ve)
↑ transpulmonary pressure
↑ lung volume
↓ alveolar pressure
airflow in, down the pressure gradient from atmosphere into the lungs
will continue until alveolar pressure once again equals atmospheric pressure
tidal expiration
↓ thoracic cavity
↓ pleural space volume
↑ intrapleural pressure
↓ transpulmonary pressure
↓ lung volume
↑ alveolar pressure
airflow out, air will be expelled out of lungs until alveolar pressure = atmospheric pressure
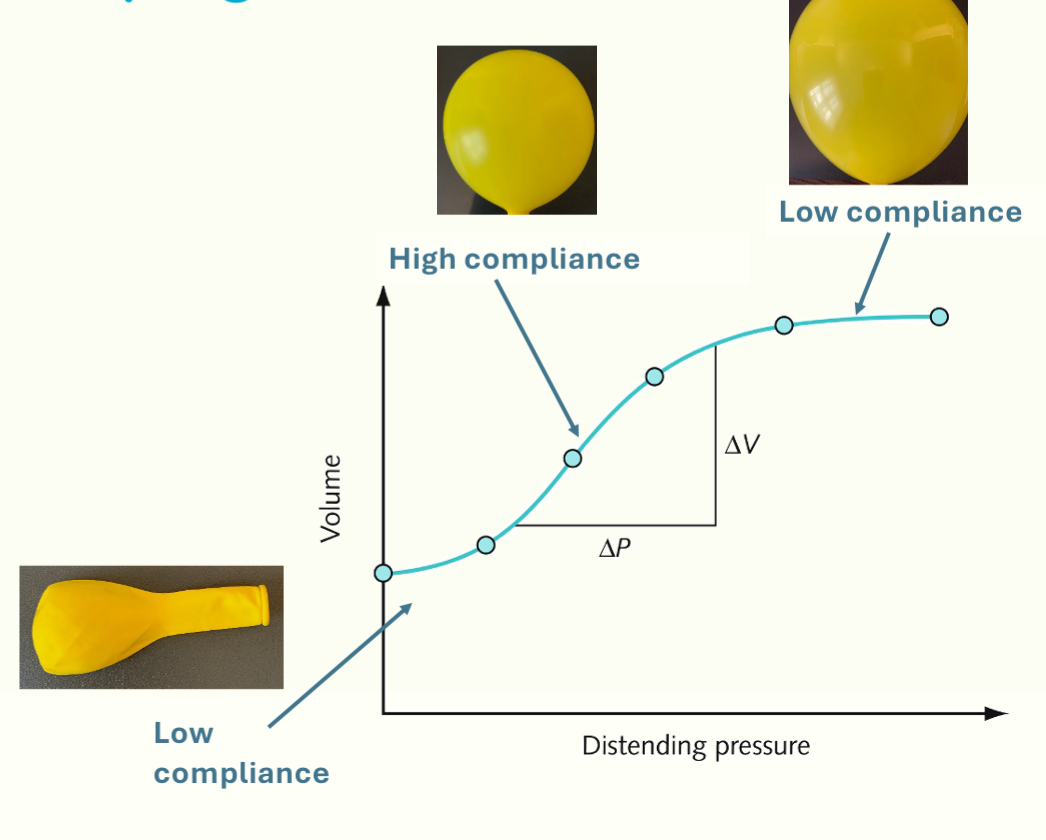
compliance
how easily the lungs can be distended/stretched when external force is applied on them
compliance = ΔV / ΔP
a measure of how much the volume changes with a change in the transpulmonary pressure
volume is directly proportional to compliance
the greater the change in volume per unit change in pressure, the greater the compliance
elasticity
resistance to stretch and tendency to return to their previous configuration when distorting force is remove
opposite of compliance
respiratory compliance
distensibility of chest wall and lungs
chest wall tendency: to spring outwards and lungs to spring inwards
to change the thorax volume, resp muscles must overcome lung and chest wall’s mechanical properties: most importantly the lungs’ tendency to recoil
elastic properties of the lung
caused by lung tissue itself: elastin and collagen fibres
elasticity: caused by elastin and surface tension
emphysema: loss of elastic lung tissue (elastic properties decreased)
pulmonary fibrosis (replacement of normal lung tissue with scar tissue)
static compliance
static lung mechanics because the volume is measured at each change in pressure but doesn’t take into account airflow (which changes with time)
lung doesn’t expand linearly with increasing pressure, so compliance is not the same throughout lung expansion
at first, a higher pressure is required for a small change in volume (compliance = low)
the lungs then become easier to distend → slope steepens
small change in transpulmonary pressure results in a large change in lung volume
curve flattens out again: any further increase in pressure will not lead to a change in volume
alveoli = well inflated and close to their elastic limit so compliance is low again
steepest part of the curve= normal tidal breathing (this reduces trhe work of breathing)
slope of the curve = compliance
compliance during tidal breathing
residual volume = air left in the lungs when you have breathed out as much air as possible
lungs never fully deflate (always some air left inside them)
FRC (functional residual capacity)= air left in lungs at the end of a normal tidal expiration
TLC (total lung capacity)= how mucb air in lungs when you’ve taken the biggest breath you can
hysteresis= a phenomenon when the pressure vol curve is different for inspiration and expiration
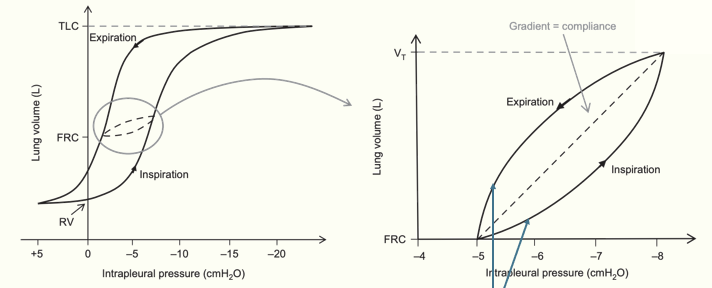
lung volume and compliance
compliance highest= low lung volumes
compliance lowest= high lung volumes
a larger increase in transpulmonary pressure is needed to produce only a small change in volume (because alveoli are maximally stretched)
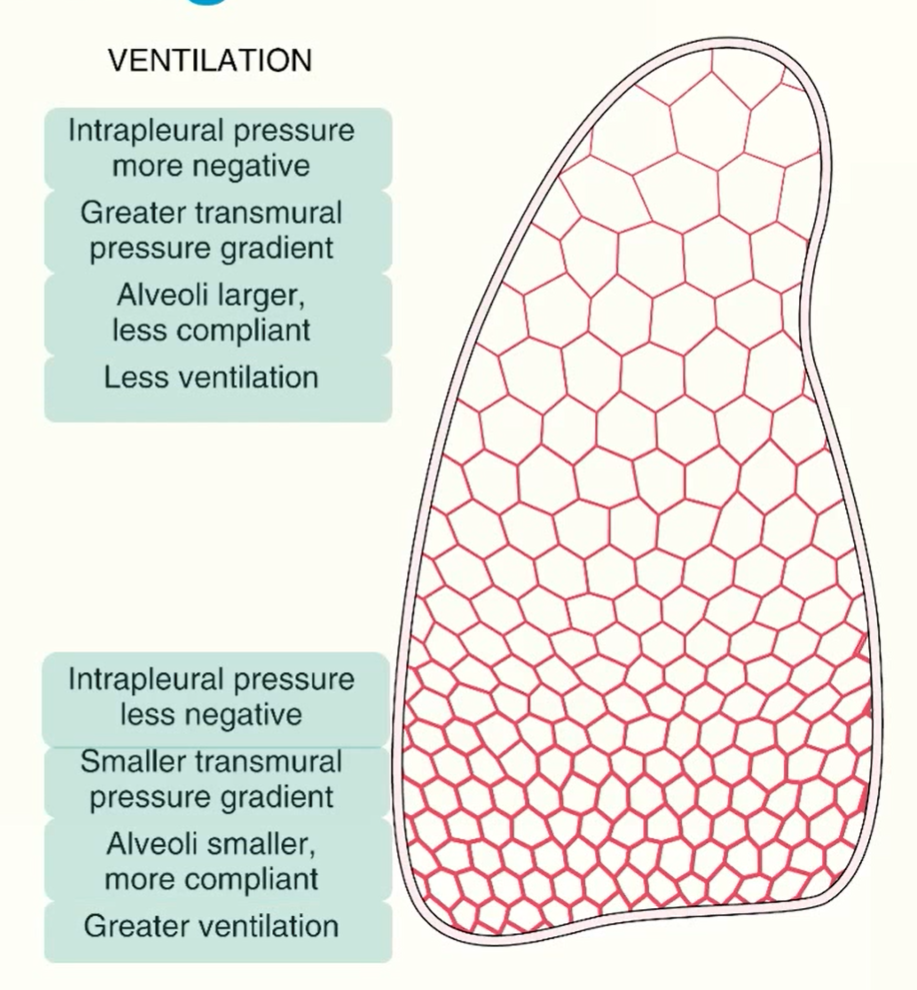
compliance throughout lung
base of lung → compressed by lung tissue above it and has greater intrapleural pressure compared to apex
weight of fluid in the pleural cavity increases intrapleural pressure at base (so it’s less -ve than at the apex)
based of lung also has greater initial compliance compared to the apex
magnitude of pressure changes the same throughout, base of lung will expand more (greater ventilation)
alveoli at the base are less distended than at the apex at the end of expiration
as alveolar pressure is same throughout the lung, the difference between the alveolar pressure and the intrapleural pressure (transpulmonary pressure) is therefore less at the base at the end of expiration
therefore alveoli at the base are less distended than at the apex at the end of expiration
base of lung has a greater initial compliance than the apex as compliance is greater at lower lung volumes
ventilation diagram
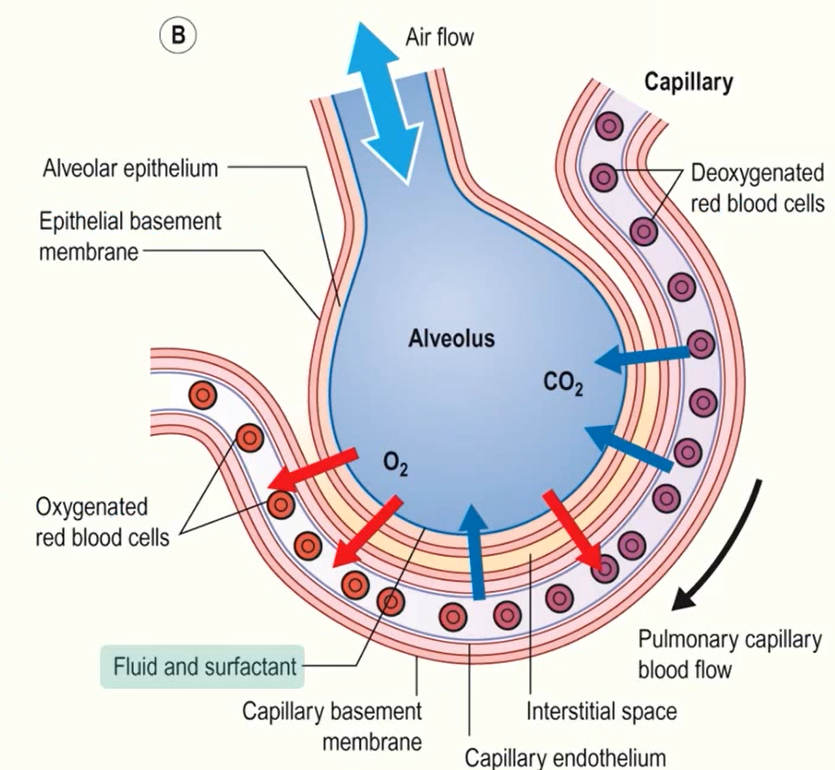
alveolar fluid
functions:
protects alveolar epithelium
immune role: solvent for antimicrobial peptides and cytokines, environment for alveolar macrophages
mediates gas transfer
forms an air-fluid interface
alveolus diagram
surface tension
cohesive forces via hydrogen bonds between surface molecules are stronger, allowing the surface of a liquid to resist external force
they don’t have any molecules above them, so they attract more strongly to the molecules on either side and below them
allows surface of the liquid to resist external forces applied to it
surface of water contracts to minimise contact with air, leading to formation of bubbles
surface tension in alveoli
alveolar can be thought of as spherical structures, considered similar to tiny interconnecting bubbles
surface tension at the air-fluid interface creates an inward collapsing pressure in the alveoli
alveolar surface is covered by a thin layer of fluid and the air-fluid interface has surface tension that’s trying to reduce the area of the interface and so is trying to collapse the alveoli
Laplace’s Law
pressure within the alveoli can be predicted using Laplace’s Law
states that the pressure within the bubble = twice the surface tension / radius
P= 2T/ r
pressure and radius are inversely proportional
the smaller the bubble/alveoli, the greater the inward collapsing pressure and a greater pressure is needed to keep it inflated
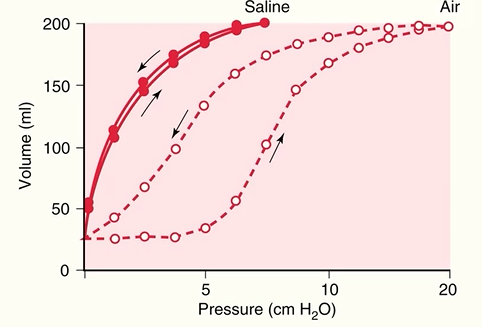
surface tension and lung elastic recoil
elastic recoil in the saline-filled lung is a result of the lung tissue alone
elastic recoil in air-filled lung is the lung tissue and the surface tension at the air-fluid interface in the alveoli
surface tension contributes more to elastic recoil than elastic lung tissue, affecting compliance
problems with surface tension
smaller alveoli are harder to inflate as they require a greater transpulomary pressure to overcome the inwards collapsing pressure
significantly increases the work of breathing
if alveoli of different sizes connected to a common airway, the smaller alveoli may collapse into the bigger alveoli
if surface tension is constant, the smaller alveolus would have a greater pressure compared to the larger alveolus, so air would move down the pressure gradient, causing the smaller alveolus to empty into larger alveolus
collapsed alveoli would then require a higher distending pressure to inflate again
inwards force of the surface tension would tend to suck fluid would suck fluid from the interstitium into the alveolus
forces which stabilise alveoli
mechanisms which act to reduce surface tension in the lungs
structural interdependence of alveoli
other than the alveoli on the pleural surface, alveoli are surrounded by other alveoli which exerts traction which opposes collapse
pores of Kohn and canals of Lambert
connect adjacent alveoli and provide collateral ventilation and help equalise pressure
surfactant
decreases surface tension in smaller alveoli more than larger alveoli
results in stabilisation of the alveoli
surfactant
secreted by exocytosis from cuboidal type II pneumocytes
a mix of phospholipids, neutral lipids, fatty acids, proteins
disrupts hydrogen bonds between surface water molecules and reduces surface tension
forms a thin film that lines the alveoli and acts as a barrier at the air-liquid interface
stabilises inflation of alveoli as it differentially reduces surface tension more at lower volumes (where surfactant molecules are closer together) and higher volumes (where surfactant molecules are further apart)
instead of staying constant, the surface tension increases as the alveoli become larger and decreases as alveoli become smaller
Laplace’s Law: it will reduce the pressure needed to keep the alveoli inflated as the lung volume decreases
makes it easier for lungs to inflate during inspiration and therefore increases compliance/reduces effort needed for expansion
work of breathing
energy consumed by respiratory muscles during resp cycle
consists of:
elastic work
resistive work
elastic work
done on inspiration to overcome elastic properties of the respiratory system
outward recoil of the chest wall
inwards recoil of the lung tissue
inward recoil of the alveolar surface tension
some of the energy used in elastic work is stored as potential energy in elastic structures of the lung/chest and used as a driving force for normal expiration
resistive work
to overcome friction
tissue resistance: result of tissues moving against each other during breathing
airway resistance: frictional forces on gas molecules during air flow
majority of resistive work
due to frictional forces on gas molecules as they interact with each other and the walls of the airways
the energy used in resistive work is wasted as it dissipates as heat and sound
work of tidal breathing
quiet tidal breathing is very efficient
doesn’t require that much work and energy required is less than 2% of the basal metabolic rate
lung pathology can increase the work of breathing substantially (up to 30% of BMR in some cases) and can lead to respiratory muscle fatigue and resp failure
airway resistance
factors affecting airway resistance
turbulent air flow
change in airway radius
when airway resistance is increased, pressure gradient must be increased to maintain flow (increased resp effort)
flow = pressure gradient / resistance
turbulent air flow
gas flow is only turbulent in the trachea
increased veolcity (due to increased resp rate can cause turbulent flow in the large bronchi for a greater propoertion of the respiratory cycle
upper airway obstructuin can increase velocity and turbulence
reduced airway radius
bronchoconstriction
low lung volume- airway reduces on expiration due to reduced radial traction from deflating lung
dynamic airway compression: during forced expiration, intrapleural pressure can become positive, causing collapse of aurwats without cartilage in their walls
can be worsened in diseases which cause airway narrowing or loss of elastic tissue