W5- Responses of the brain to traumatic injury
1/119
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
120 Terms
what is the skull?
non-expansile solid structure containing a compressible brain
what is the skull comprised of?
many bones which are formed by intramembranous ossification and joined by sutures (fibrous joints)
what are the two divisions of the bones of the skull?
-cranium (consisting of cranial roof and cranial base)
-face
what is the cranium?
superior aspect of the skull
(encloses and protects the brain, meninges and cerebral vasculature)
what bones form the cranial roof (calvarium)?
-frontal
-occipital
-two parietal
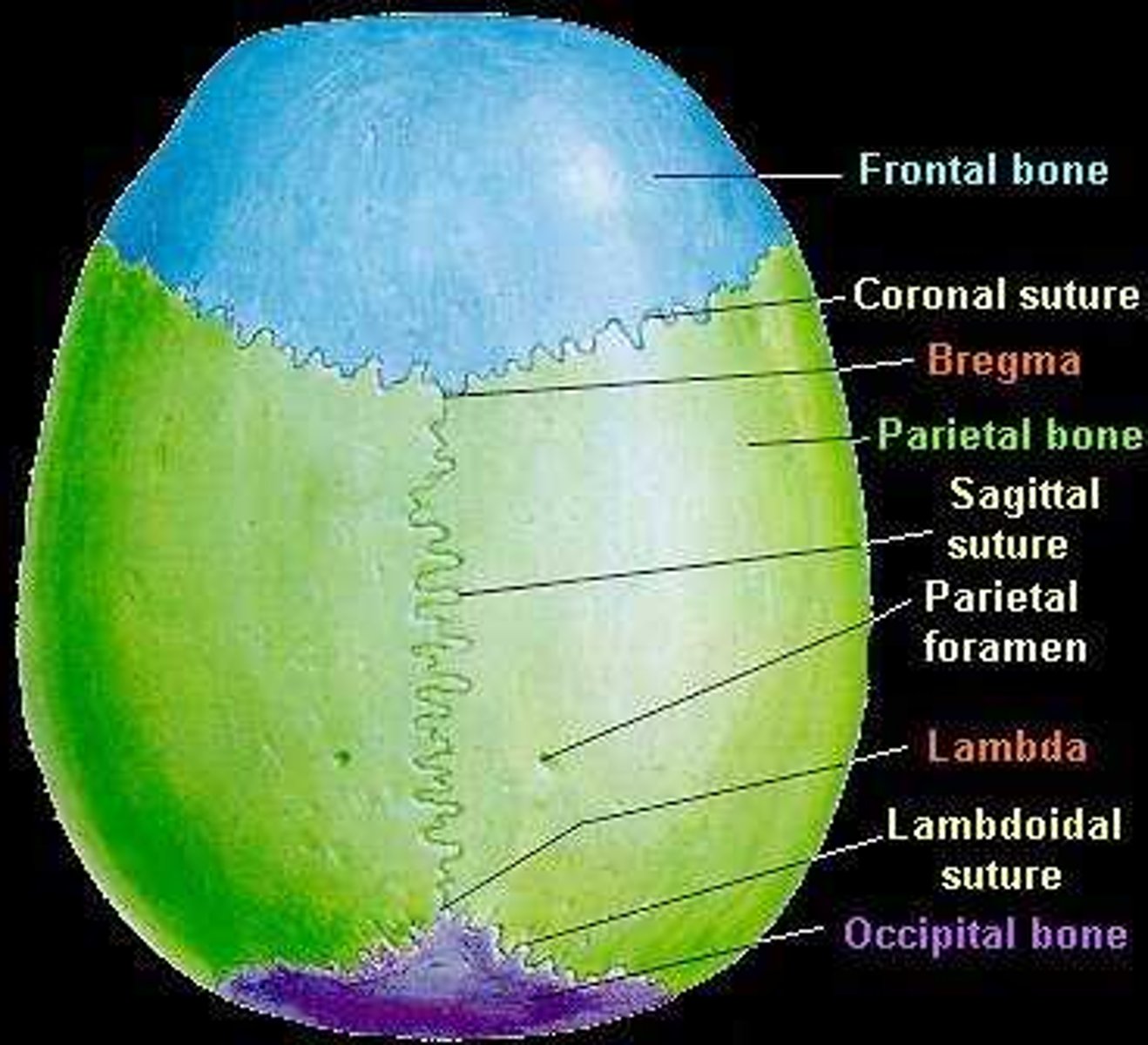
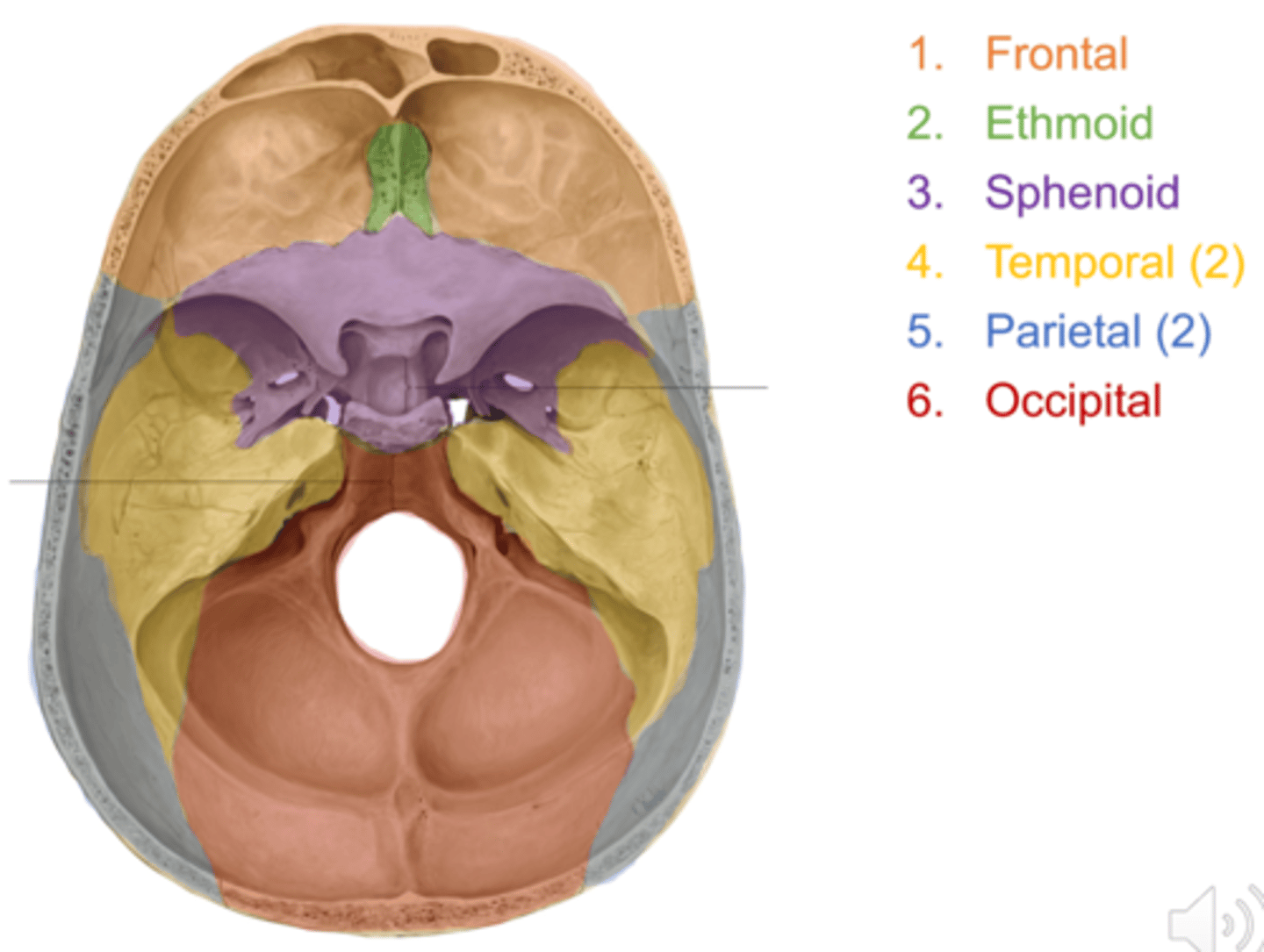
what bones form the cranial base?
-frontal
-sphenoid
-ethmoid
-occipital
-parietal
-temporal
(articulate with C1, facial bone and the mandible)
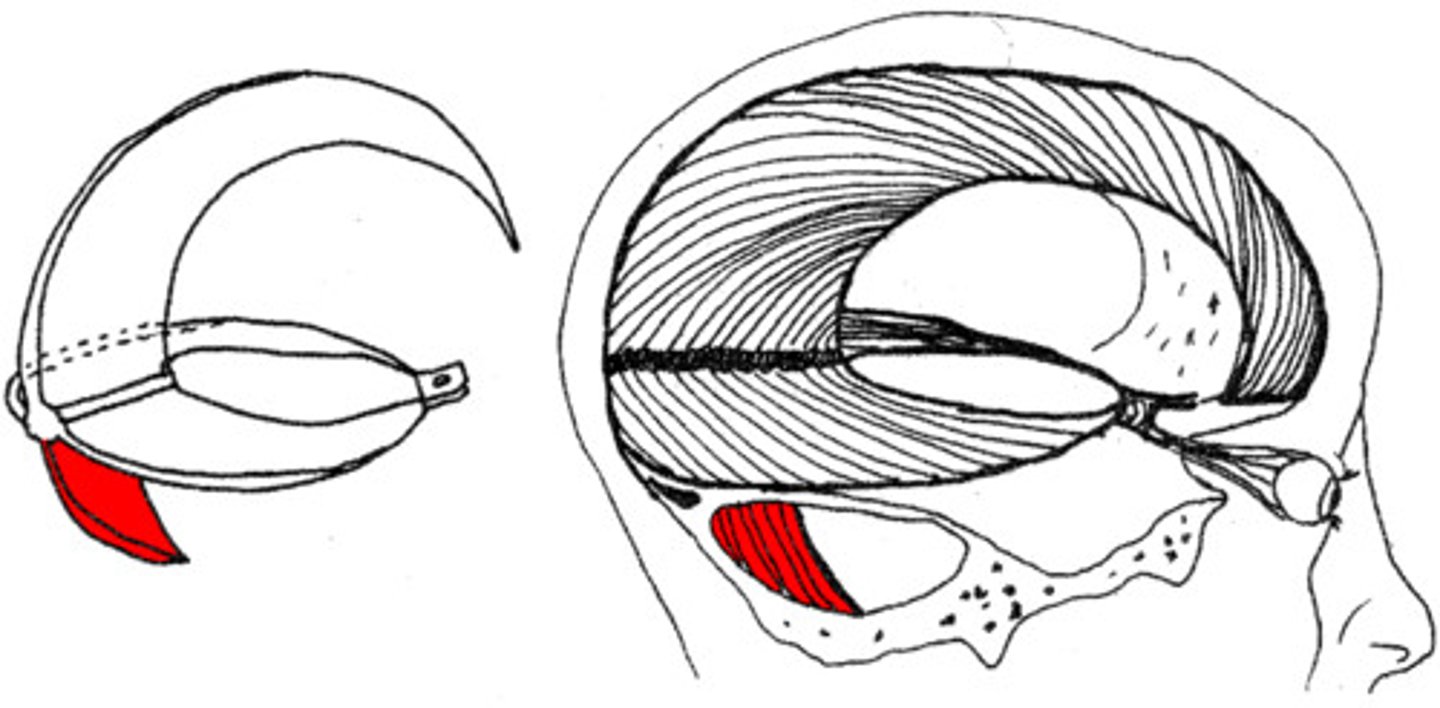
what is the pterion?
H-shaped junction between the temporal, parietal, frontal and sphenoid bones
what usually causes the fracture of the cranium?
blunt force or penetrating trauma
what might occur in a fracture of the cranium at the pterion?
-pterion overlies the middle meningeal artery
-fractures in this area may injure the blood vessel
-blood can accumulate between skull and dura mater to form an extradural haematoma
what is the dura mater?
-outermost layer of the 3 meninges that protect brain and spinal cord
-consists of fibrous connective tissue
-contains sensory nerves and blood vessels
(damage can cause bleeding and haematoma formation)
what are 3 fascial reflections of the brain?
-falx cerebri
-falx cerebelli
-tentorium cerebelli
what is the falx cerebri?
-sagittal invagination of dura mater into the longitudinal fissure
-separates the cerebral hemispheres

what is the falx cerebelli?
-small sickle-shaped fold of dura mater
-projects forwards into the posterior cerebellar notch and into the vallecula of the cerebellum
-separates the cerebellar hemispheres
what is the tentorium cerebelli?
-transverse tough fibrous tissue
-holds the cerebral hemispheres above the posterior fossa (cerebellum and brainstem)
what is the passage of the oculomotor nerve (CN III)?
-emerges from midbrain
-pierces dura mater to enter lateral aspect of cavernous sinus at base of the skull
what is the oculomotor nerve (CN III) responsible for in terms of innervation of the eye?
-extraocular eye muscles- allows movement of eyes and prevents drooping of eyelids
-parasympathetic supply to sphincter pupillae and ciliary muscles
why does brain trauma lead to pupil dilation, even in bright light?
-compression from trauma and haemorrhage leads to lack of parasympathetic response by oculomotor nerve (CN III)
-lack of parasympathetic response prevents pupil constriction in response to bright light
what causes a traumatic brain injury (TBI)?
occurs when an external mechanical force injures the brain
what are some examples of causes of TBI?
-rapid acceleration/deceleration
-impact
-penetration by projectile
what are the 3 ways in which traumatic brain injury can be classified?
-severity
-anatomical features of the injury
-mechanism of injury
how can a traumatic brain injury be classified in terms of severity?
-Glasgow Coma Scale
-post-traumatic amnesia
-loss of consciousness
how can traumatic brain injury be classified in terms of anatomical features of the injury?
-extra-axial
-intra-axial
what is an extra-axial TBI?
occurring within the skull but outside the brain
what is an intra-axial TBI?
occurring within the brain tissue
how can traumatic brain injury be classified in terms of the mechanism of injury?
-closed- brain is not exposed
-penetrating- object pierces the skull and breaches the dura mater
what features of the external mechanical force influence the severity and characteristics of a traumatic brain injury?
-type of force
-direction of force
-intensity of force
-duration of force
what is a coup injury?
damage occurs directly under the site of impact
what is a contrecoup injury?
damage occurs on the opposite side of impact
(ie cerebral contusion may occur on opposite side of cerebral concussion)
what are two clinical responses to brain injury?
-altered consciousness level
-symptoms- vomiting, pain, dizziness
why is consciousness level altered after traumatic brain injury?
trauma interrupts the reticular activating system
how can loss of consciousness be classified after traumatic brain injury?
-subjective measure= loss of tone, loss of awareness
-objective measure= Glasgow Coma Scale
what are the two types of post-traumatic amnesia?
-retrograde amnesia- unable to remember events that happened just before trauma
-anterograde amnesia- unable to remember events that have happened after trauma
why does traumatic brain injury cause vomiting (often without nausea)?
raised intracranial pressure activates vomiting centres
(chemoreceptor trigger zone in fourth ventricle)
what is the natural history of a traumatic brain injury?
1. primary brain injury
2. progressive damage
3. secondary injury
what is a primary brain injury?
-injury to the brain and its associated structures that results instantaneously from impact to the head (occurs at moment of trauma)
-may be severe and fatal if brainstem is damaged, or minor concussion
what are 4 examples of focal primary brain injury?
-contusion
-haemorrhage
-skull fractures
-penetrating head injury
what is contusion?
bruising of the brain
(may be coup or contrecoup)
what causes haemorrhage?
blood vessels damaged and bleeding occurs
what situation is likely to cause a diffuse brain injury?
shearing forces acting on the whole brain
(eg high speed car accident where there is sudden deceleration)
what are 4 examples of a diffuse primary brain injury?
-diffuse axonal injury
-hypoxic brain injury
-diffuse brain swelling
-concussion
what is diffuse axonal injury?
-damage to white matter tracts (axons) of brain
-depending on severity can lead to persistent vegetative state
what is likely to cause hypoxic brain injury?
lack of consciousness and being unable to support breathing
what is likely to cause diffuse brain swelling?
damage to circulation
why is there controversy about whether concussion is a brain injury causing disability ?
-only abnormal CT findings in 6-7%
-led to theorising that disability is related to patient factors (eg beliefs, depression) or indirectly to trauma (eg PTSD)
what is progressive damage after traumatic brain injury?
chain of events that occur in a primary brain injury and are worsened by increased intracranial pressure and reduced perfusion
(develop after initial injury)
what is the chain of events that is involved in progressive brain damage?
-mechanoporation
-calcium flux
-oxygen free radical formation and lipid peroxidation
-cytokine mediated inflammatory response
-axotomy
what is mechanoporation?
holes forming in lipid bilayer that makes up the blood brain barrier
what is calcium flux?
influx of calcium through the porous lipid bilayer into the brain
(BBB no longer protective)
what is the consequence of oxygen free radical formation and lipid peroxidation in progressive brain damage?
leads to damage within neural tissue
what is the consequence of the cytokine-mediated inflammatory response in progressive brain damage?
-increased swelling
-increased local pressure
-decreased circulation
what is axometry?
severing of axons
(can lead to irreversible functioning of brain tissue)
what is a common progressive brain injury after primary diffuse axonal injury?
-shearing from force leads to tearing of lipid bilayer
-causes disruption of BBB
-leads to calcium flux, oxygen free radical formation, lipid peroxidation and inflammation
what is secondary brain injury?
result of hypoxia or decreased perfusion of the brain tissue
(occurs immediately after trauma, produces long-lasting effects, can be prevented)
what are some examples of secondary brain injury?
-raised intracranial pressure
-hypoxic brain injury
-ischaemia brain injury
-seizures
-infection
-brain herniation
-cerebral oedema
-hydrocephalus
-chronic traumatic encephalopathy
what causes raised intracranial pressure as a secondary brain injury?
accumulation of blood and diffuse swelling
what causes ischaemic secondary brain injury?
hypovolaemia due to bleeding after traumatic injury
why are seizures very destructive as a secondary brain injury?
-take up a lot of brain substrate
-cause further brain damage
how does infection occur as a secondary brain injury?
occurs if dura integrity has been breached
(pathogens are able to enter meningeal layers)
what are the neurochemical mediators that mediate secondary injury?
-excitatory amino acids (EAAs)
-endogenous opioid peptides
how do excitatory amino acids (EAAs) cause secondary brain injury?
cause swelling, vacuolation and neuronal death
how do endogenous opioid peptides cause secondary brain injury?
modulate presynaptic release of EAA neurotransmitters (cause swelling, vacuolation and neuronal death)
what is intracranial pressure (ICP)?
pressure inside the skull, and thus in the brain tissue and CSF
what is a normal, abnormal and severe ICP?
normal= 10mmHg
abnormal= >20mmHg
severe= >40mmHg
what is the consequence of sustained increase in ICP?
decreased brain function and outcome
why does brain haemorrhage lead to increased ICP?
skull is rigid and non-expansile
how is cerebral blood flow autoregulated in healthy people?
vasodilation and vasoconstriction over wide range of blood pressures
what is a factor that affects cerebral vasodilation and vasoconstriction?
carbon dioxide conc in blood
what causes the mass effect of intracranial haemorrhage?
-changes in blood flow are initially compensated for by venous vasodilation and vasoconstriction
-since skull doesn't expand, compensatory mechanisms begin to fail and blood flow to brain is reduced
what is the Monro-Kellie doctrine?
the sum of volumes of brain, CSF and intracranial blood is constant
what does the Monro-Kellie doctrine describe with an increased intracranial volume?
uncompensated state that is reached when a mass reaches a specific size in the brain
what does the Monro-Kellie doctrine take into account?
pressure-volume relationship between ICP, volume of CSF, blood, brain tissue and cerebral perfusion pressure (CPP)
what does the Monro-Kellie doctrine state?
-cranial compartment is incompressible, and the volume inside the cranium is a fixed volume
-buffers initially respond to increased ICP (CSF, venous blood)
-eventually reaches a point when pressure rises past equalisation and brain begins to compress
what are the principle buffers for increased ICP?
-CSF- moves into spinal cord
-venous blood- moves into superior vena cava
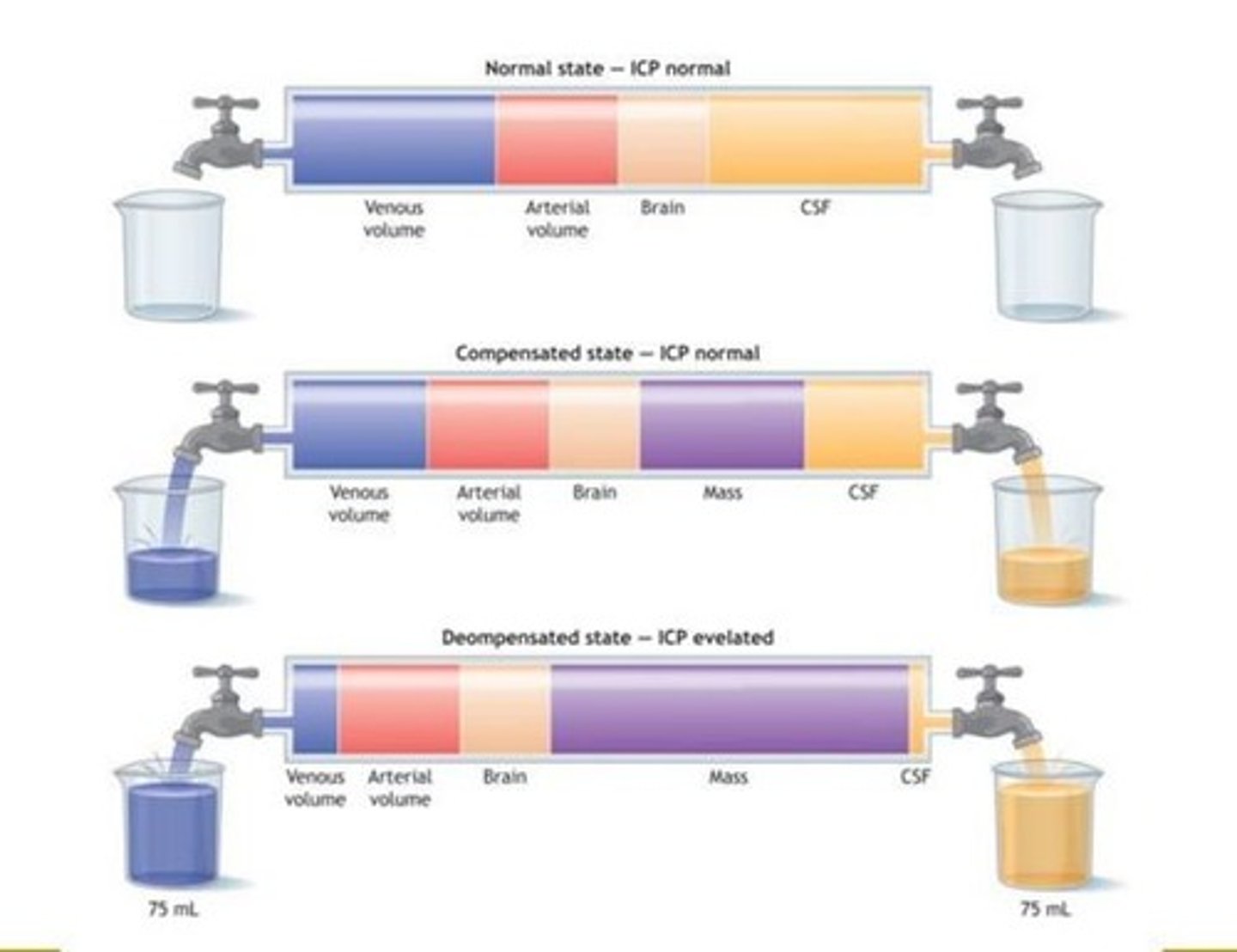
what is stage 1 of raised increased intracranail volume?
compensatory reduction in CSF and blood volume
(no rise in ICP)
what is stage 2 of increased intracranial volume?
volume increases beyond point of compensation
= ICP begins to increase
what is stage 3 of increased intracranial volume?
sustained exponential increasing ICP
= falling cerebral perfusion pressure
what is stage 4 of increased intracranial volume?
cerebral perfusion pressure ceases
= widespread necrosis and compression of brainstem (causes respiratory arrest and death)
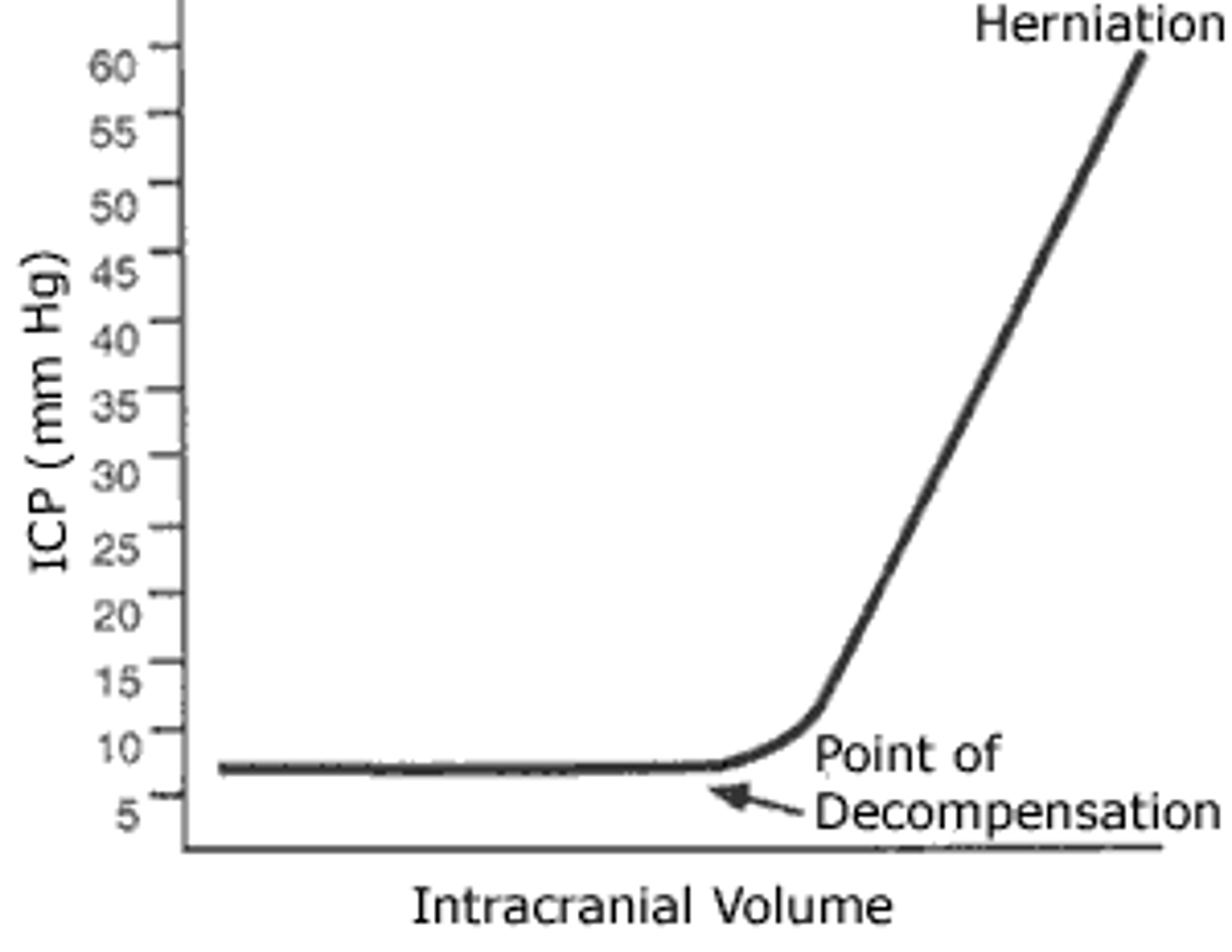
what is the volume-pressure curve that is alluded to in the Monro-Kellie doctrine?
-as intracranial volume increases, ICP does not increase initially due to compensatory mechanisms by movement of CSF and blood
-point of decompensation is reached, where pressure buffer systems equalise and cannot expand further
-ICP rises exponentially
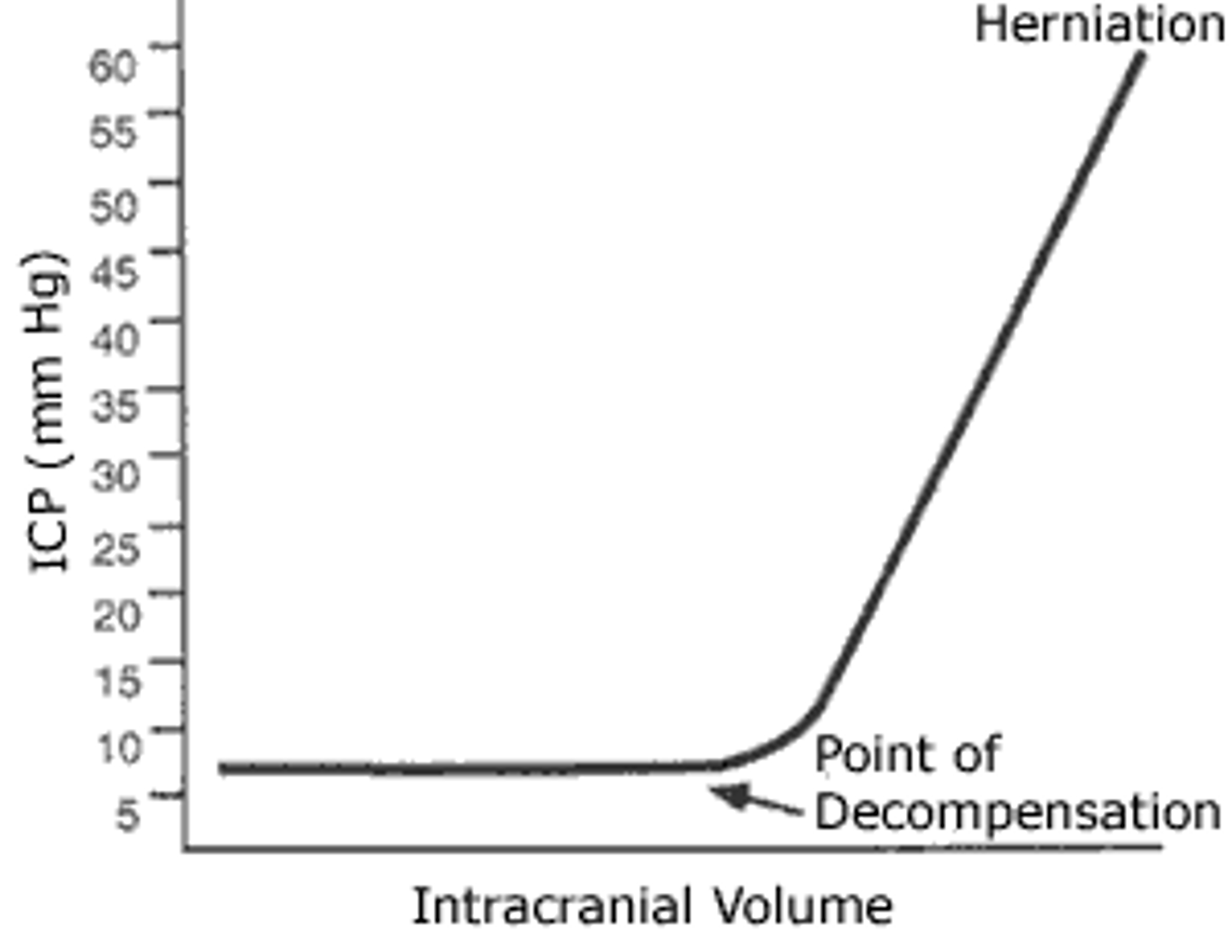
why is it crucial to identify haemorrhages before the point of decompensation?
-before point of decompensation= patient feels normal
-after point of decompensation= small time frame until herniation
what are some signs and symptoms of a raised ICP?
-headache
-vomiting without nausea
-ocular palsies
-altered levels of consciousness
-back pain
-papilloedema
what happens to the pupils after the point of decompensation in a haemorrhage?
-brainstem is compressed due to haematoma causing increased ICP
-leads to damage to CN III parasympathetic fibres which constrict the pupil
-leads to pupils being dilated, even with bright light shining in them
what occurs in uncal herniation?
-herniation of the uncus puts pressure on the midbrain
-brainstem is pushed downwards through foramen magnum (coning)
what is the uncus?
anterior extremity of the parahippocampal gyrus at the temporal lobe
(medial temporal lobe)
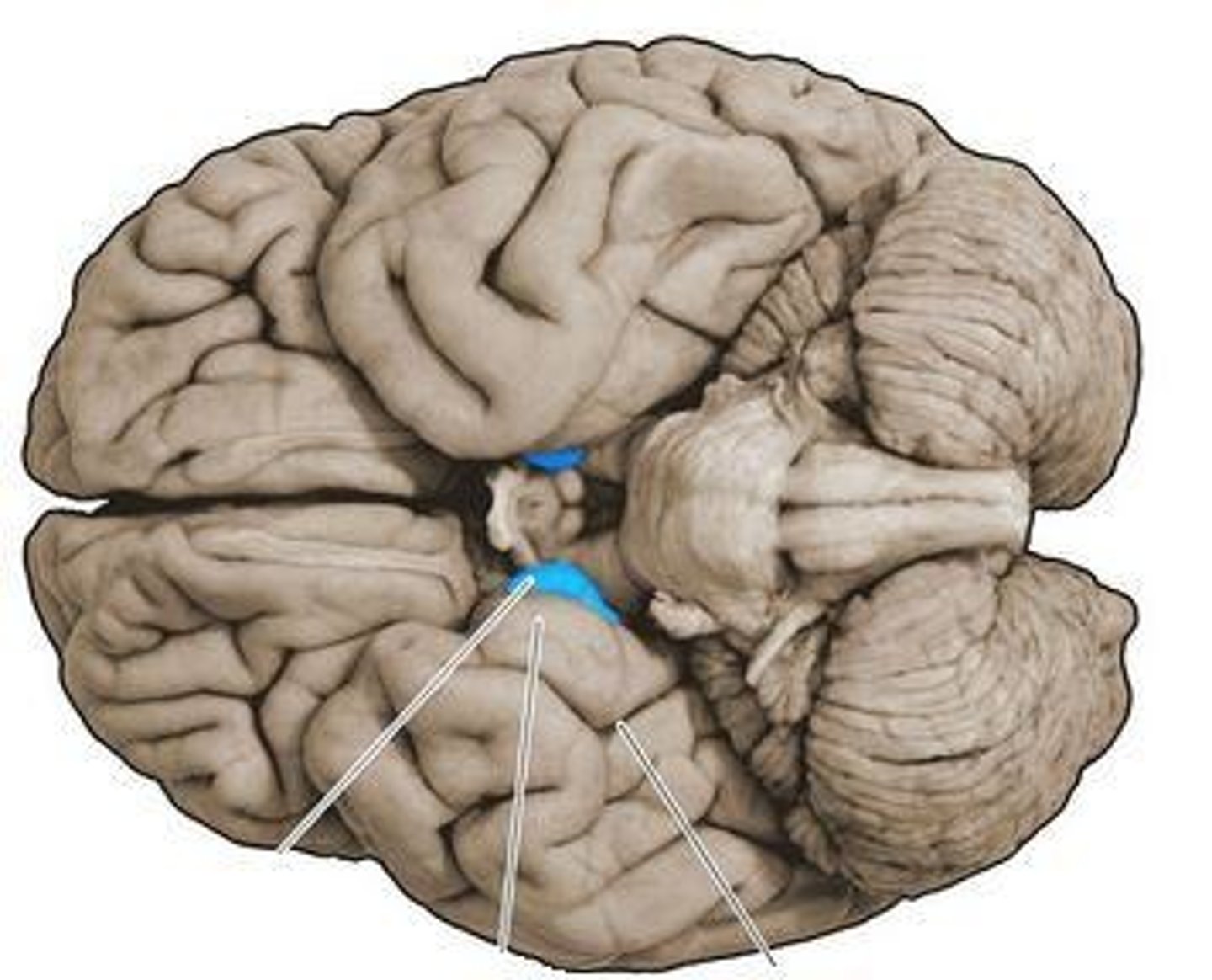
why is 'coning' (caused by uncal herniation) usually fatal?
-brainstem is pushed through foramen magnum as result of herniation of uncus putting pressure on midbrain
-brainstem contains cardiac and respiratory centres, meaning damage = death
what is cerebral perfusion pressure?
net pressure gradient that drives O2 into the cerebral tissue
why does cerebral perfusion pressure need to be maintained within a tight range?
too low = ischaemia
too high = increased ICP
how is cerebral perfusion pressure calculated?
CPP = MBP - ICP
(mean BP - intracranial pressure)
what is Cushing's reflex?
physiological adaptation allowing survival with an increased ICP
what occurs in Cushing's reflex to allow survival with an increased ICP?
-raised ICP decreases CPP (CPP = MBP-ICP)
-if ICP rises, body responds by releasing endogenous steroids to increase MBP
-increase in MBP allows CPP to remain normal
why should you NOT decrease the BP of a hypertensive patient with a brain injury?
Cushing's reflex- body releases endogenous hormones to increase mean BP in order to prevent the increased ICP affecting the CPP
(CPP = MBP-ICP)
what is a situation in which mean BP is reduced and iatrogenically causes a reduced CPP?
strong anaesthetics can be given to try and control breathing after traumatic brain injury
= decreases BP
= decreases CPP (due to increased ICP)
what happens if a patient with a traumatic brain injury is hypotensive?
-low MBP and high ICP due to brain injury = low CPP
-results in brain not being sufficiently perfused
what are two signs of increased intracranial pressure on a CT scan?
-effacement of fluid-bearing areas (eg ventricles cannot be identified)
-midline shift- soft, compressible brain is deformed
where does an extradural haematoma occur?
between the dura mater and cranium
what is a typical cause of an extradural haematoma?
trauma to temporal part of head
= damages middle meningeal artery which sits under pterion
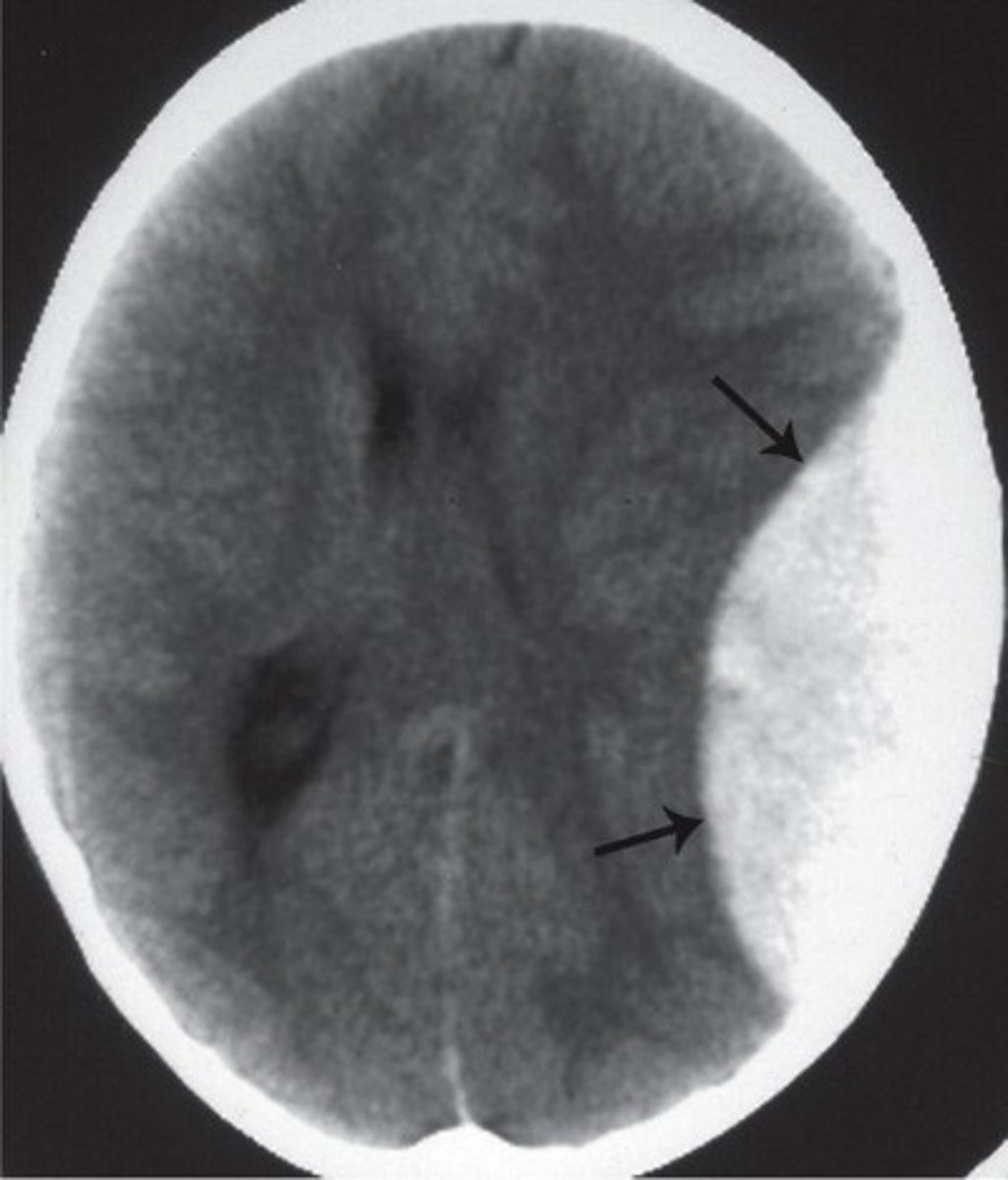
what is the characteristic shape of an extradural haematoma on a CT scan?
-white lens shape
-falx cerebri is pushed to one side
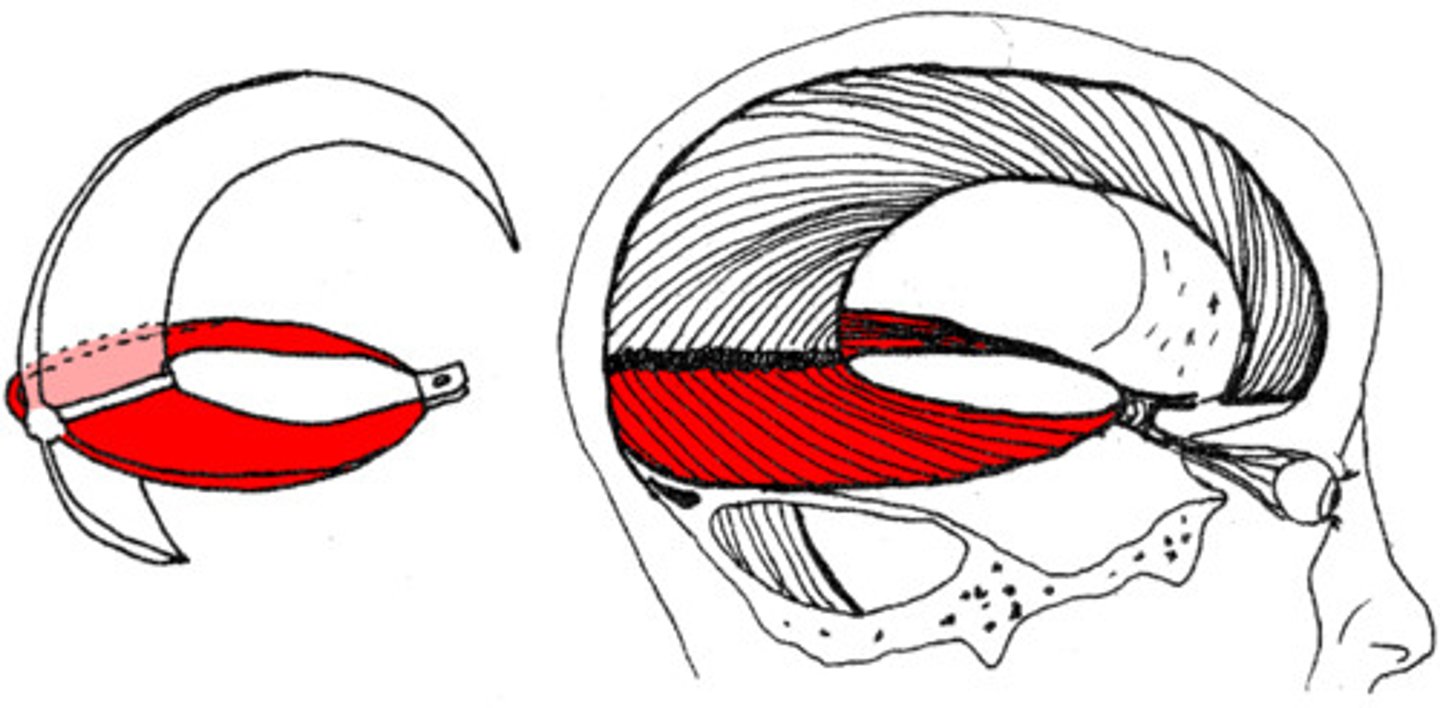
where does a subdural haematoma occur?
between arachnoid mater and dura mater
what is the typical shape of a subdural haematoma on CT?
-biconvex
-midline shift
-effacement of ventricles
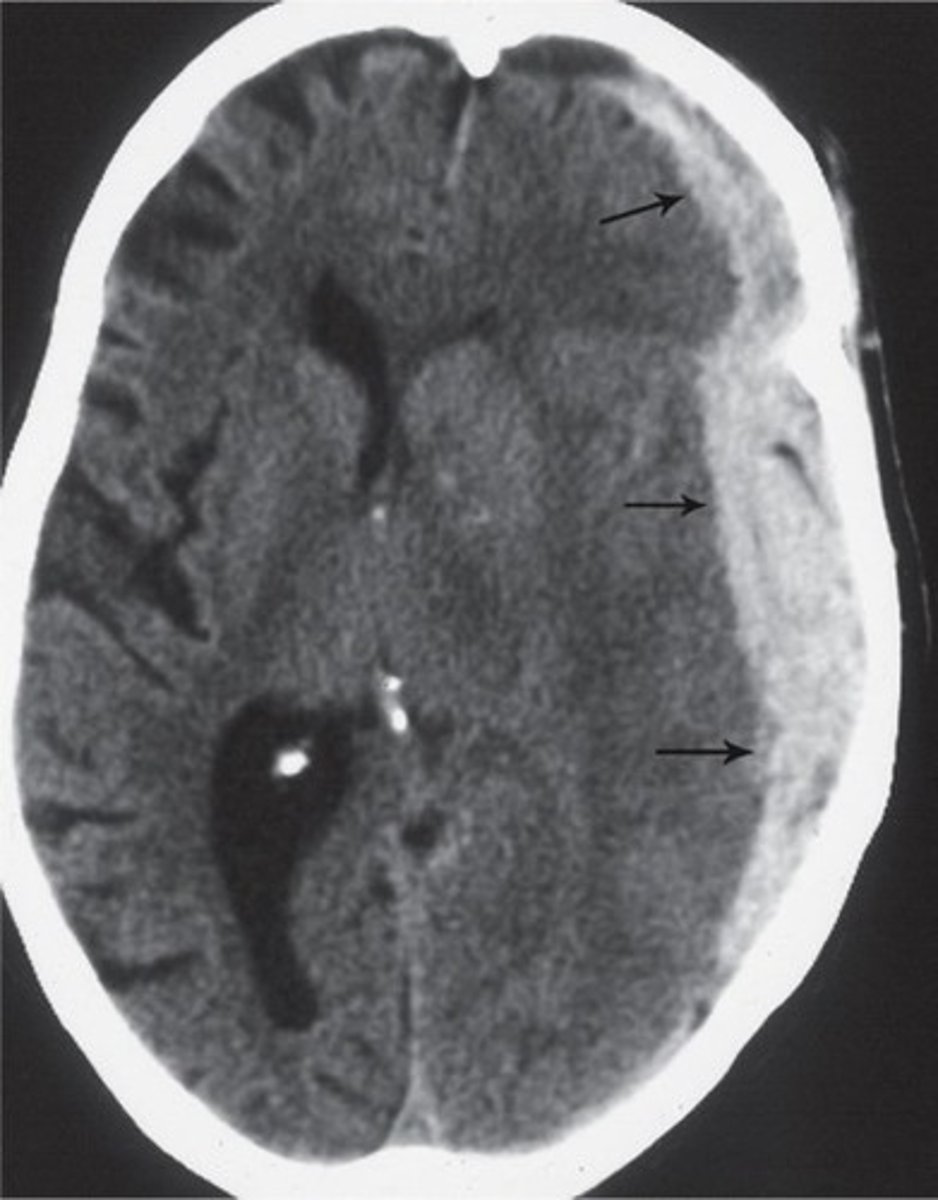
what usually causes a subdural haematoma?
venous- dural venous sinuses are located between the endosteal and meningeal layer of the dura mater
why are subdural haemorrhages more likely to occur in elderly people?
brain shrinkage due to age and dehydration