NSCI 2101 Exam 2
1/197
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
198 Terms
Brainstem
- Evolutionarily Old
- Contains cranial nuclei
- Contains tracts that run long distances
- Contains circuits innervating many different parts of CNS (Reticular formation (sleep) and Monoamine neurotransmitters (Serotonin, Norepinephrine, Dopamine))
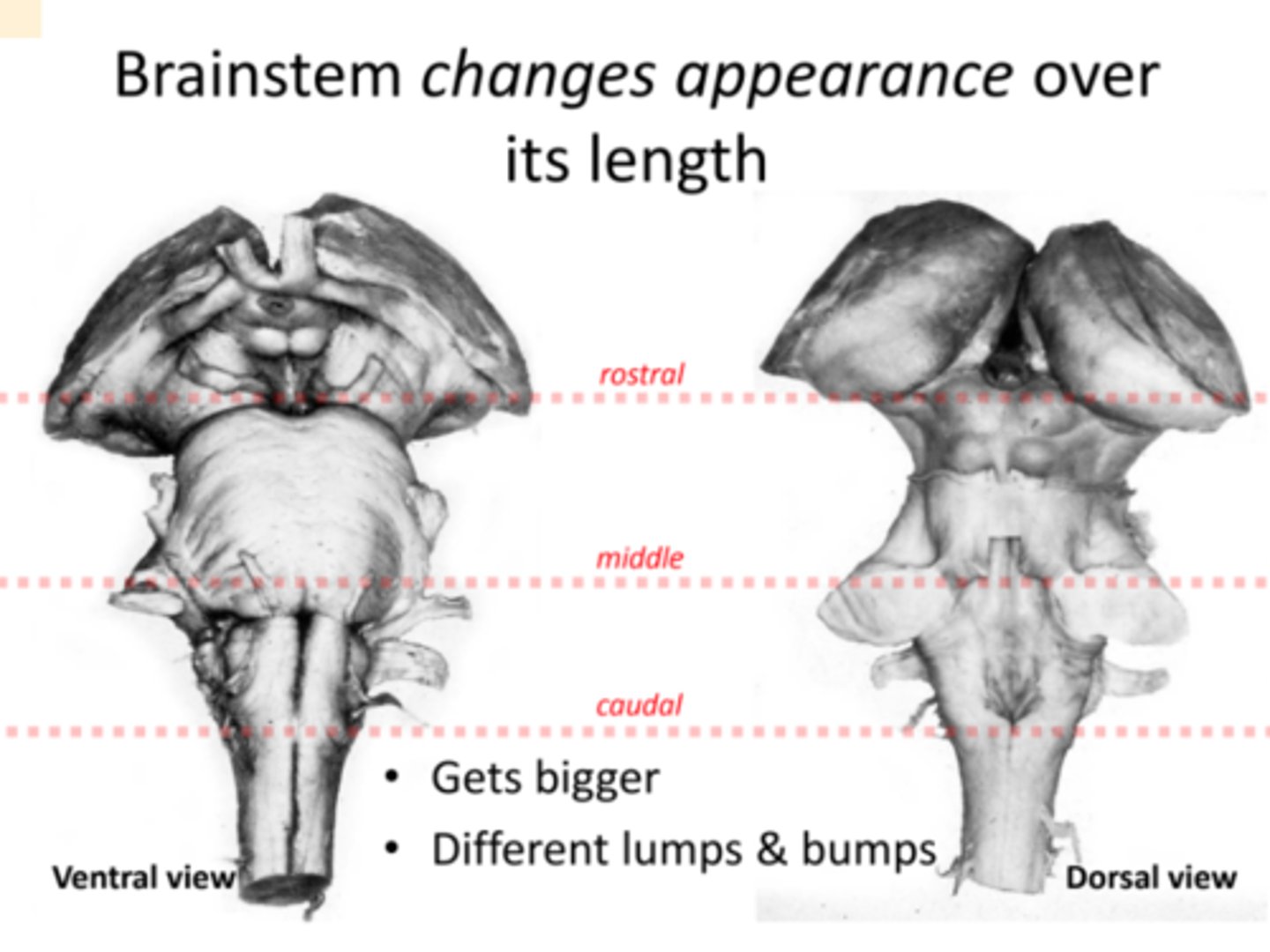
Why does brain stem change shape?
- Structures (tracts or nuclei) get added
- Structures end
- Structures change size
- Fiber (axon) tracts move (e.g., start dorsally and end ventrally; may cross midline)
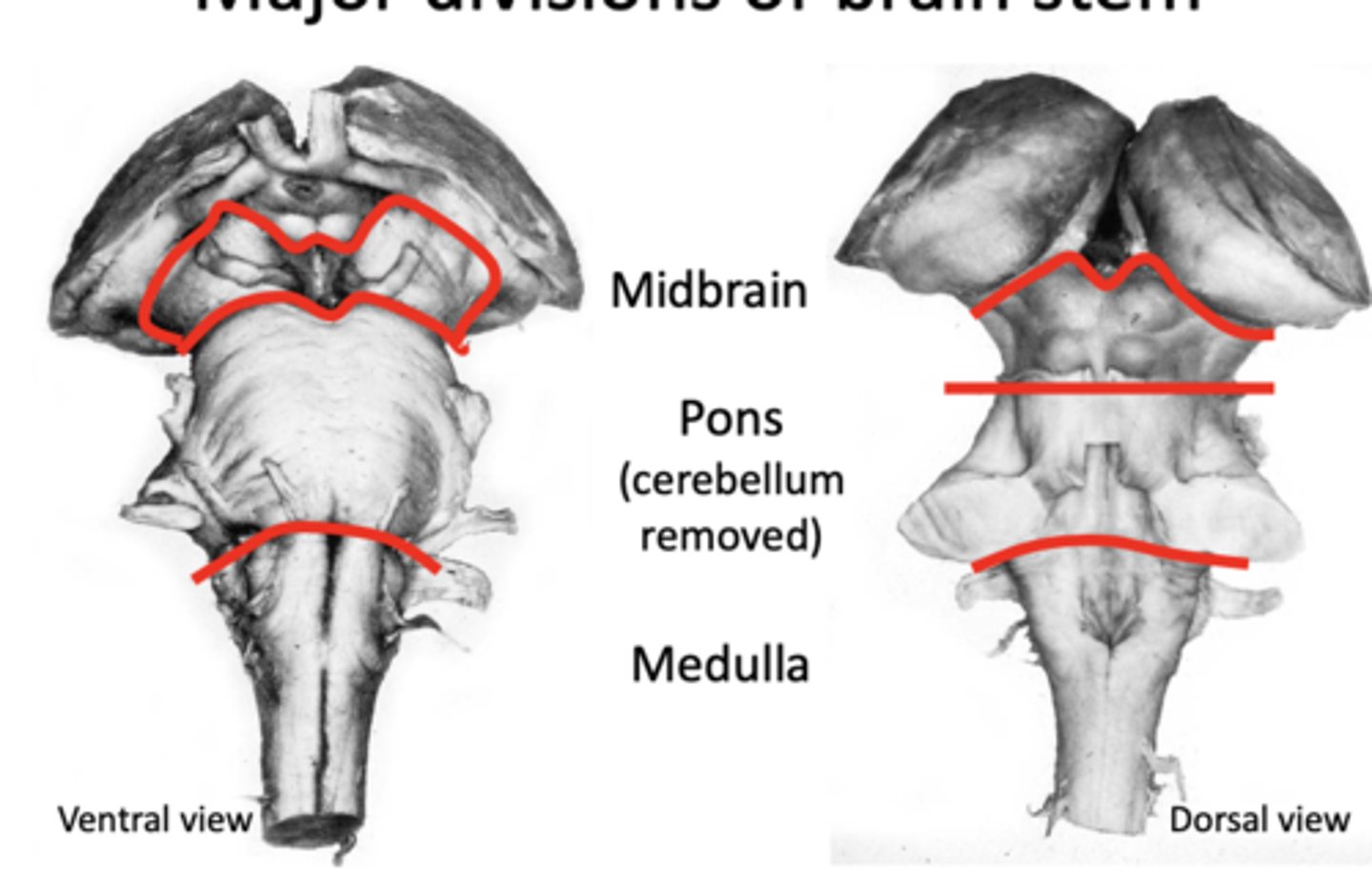
Major Divisions of brain stem
- Rostral half of medulla (top half) is covered by part of the 4th ventricle
Caudal Medulla compared to Spinal Cord
- Corticospinal tract looks like it is gone
- Dorsal horn is much bigger
- Ventral horn is much smaller
- More fibers between ventral horns (pyramidal decussation)
- Dorsal columns present but not growing within them (somatosensory fibers are synapsing onto gracile and cuneate nuclei
- Spinothalamic tract and spinocerebellar tract unchanged
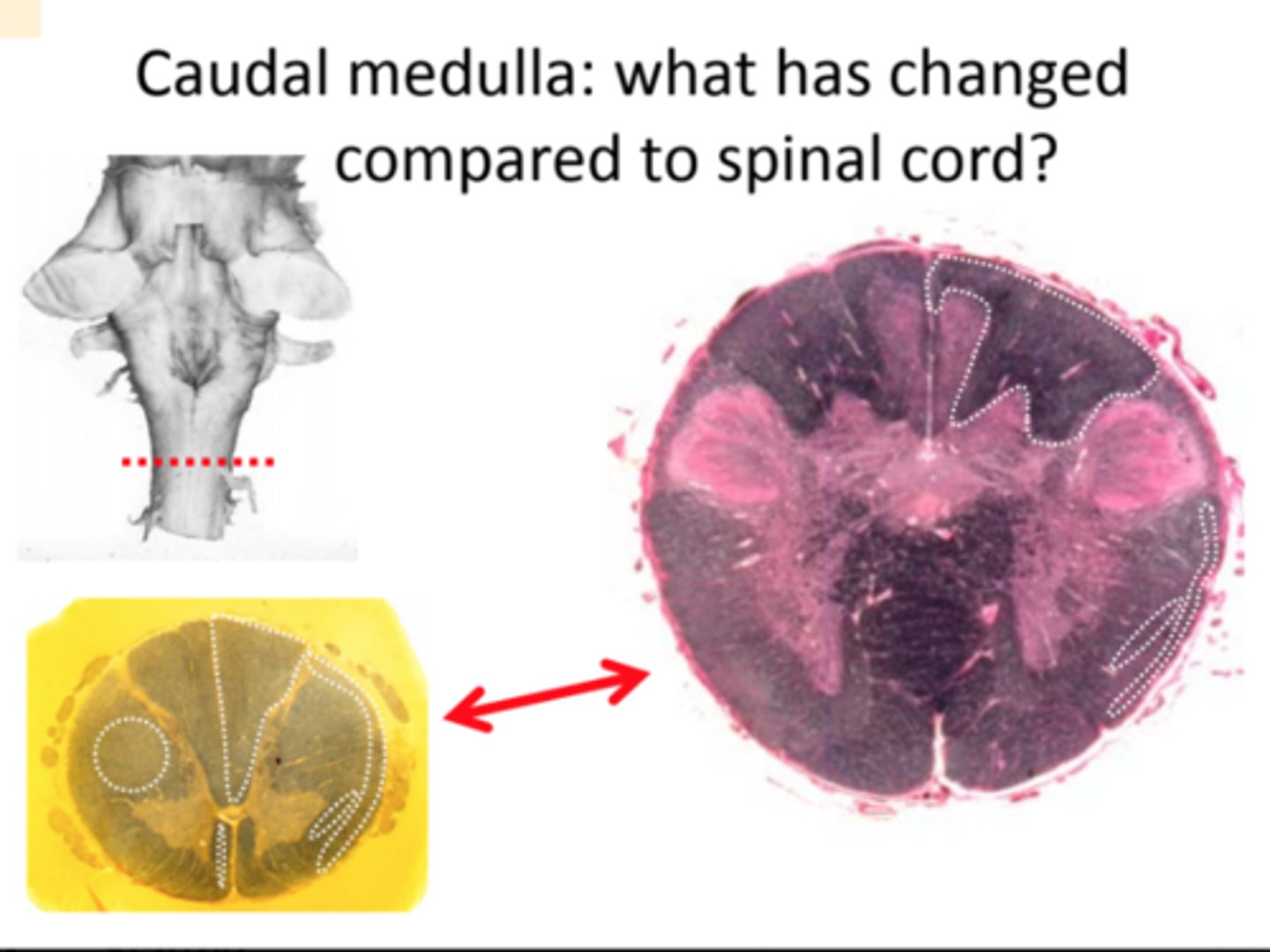
Structures in Caudal Medulla
- Spinal Trigeminal Tract and Nucleus
- Nucleus Cuneatus
- Nucleus Gracilis
- Left Dorsal funinculus
- Pyramidal decussation
- Pyramidal Tracts

Border of caudal and rostral medulla
- Note pyramids (corticospinal tract) are larger—now fully formed
- Nucleus cuneatus and nucleus gracilis are larger; the dorsal columns are smaller since many of the fibers have ended by synapsing in nucleus cuneatus or gracilis.
- Spinothalamic tract and spinocerebellar tract still unchanged.
Border of caudal and rostral medulla: sensory decussation
- Dorsal column axons synapse onto nucleus gracilis (medial) and nucleus cuneatus (lateral), part of the somatosensory system. Axons from n. gracilis and n. cuneatus project to somatosensory thalamus as the "medial lemniscus"
- Nucleus gracilis forms a bump on the medial part of the dorsal surface of the medulla: the "gracile tubercule". - Somatosensory thalamus in turn projects to somatosensory cortex
- Spinothalamic tract and spinocerebellar tract still unchanged.
Rostral Medulla
- At this level, the 4th ventricle has opened up.
- Sulcus limitans is visible on its ventrolateral floor.
- The inferior olive is a major new structure—it innervates the cerebellum. Its axons cross the midline and join those of the spinocerebellar tract (no longer visible) to form the inferior cerebellar peduncle—the bundle of axons on the dorsalateral aspect of the brain stem.
- The spinothalamic tract has been moved dorsally by the development of the inferior olive.
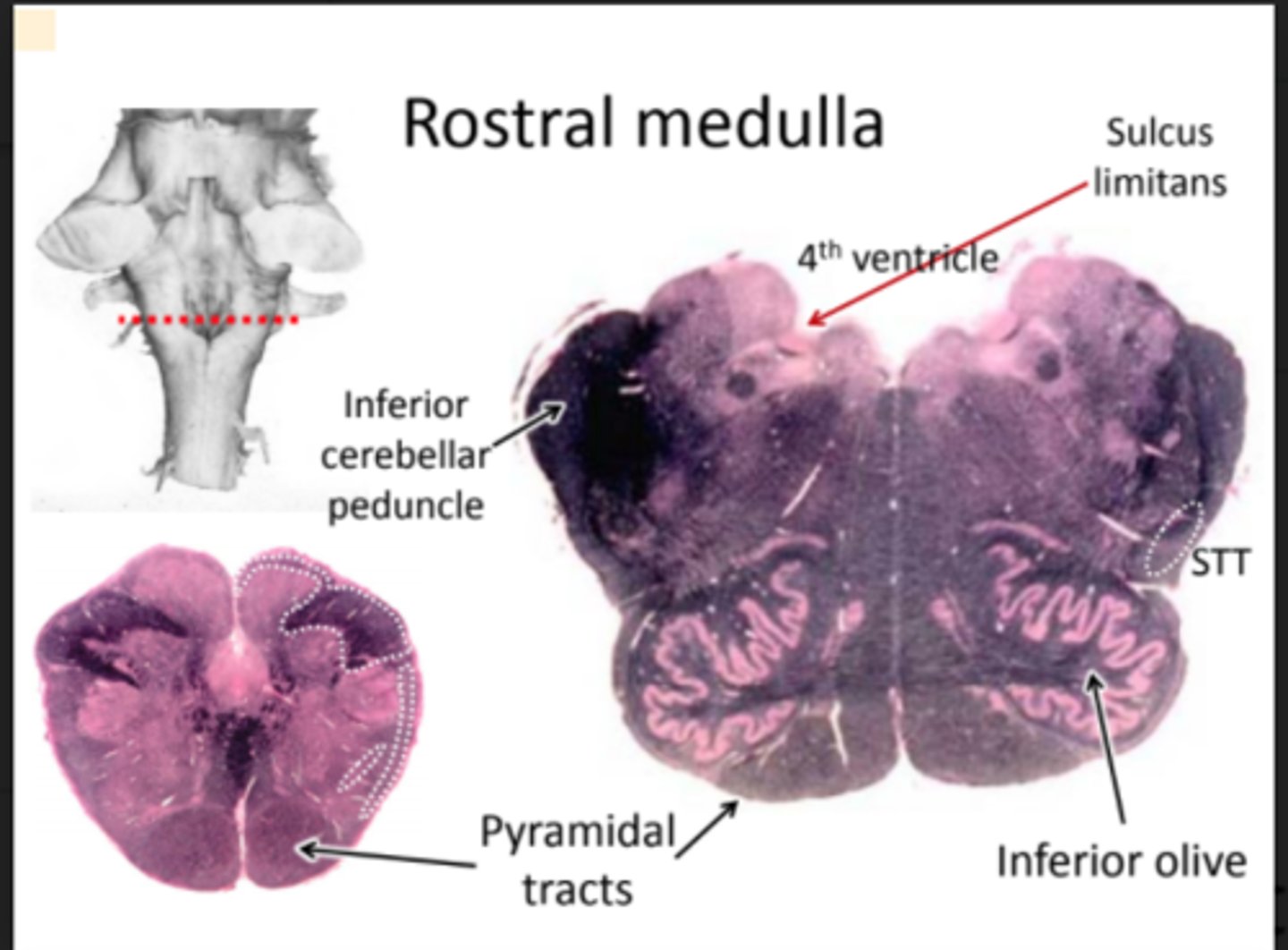
Gross structures of rostral medulla
- 4th ventricle
- Bulges from inferior olive and pyramidal tracts
- Spinothalamic tract and spinocerebellar tracts displaced dorsally/posteriorly
Brain stem "reticular formation"
Reticular formation is involved in sleep, wakefulness, autonomic function, modulating motor reflexes, modulating pain, and other non-conscious behaviors.
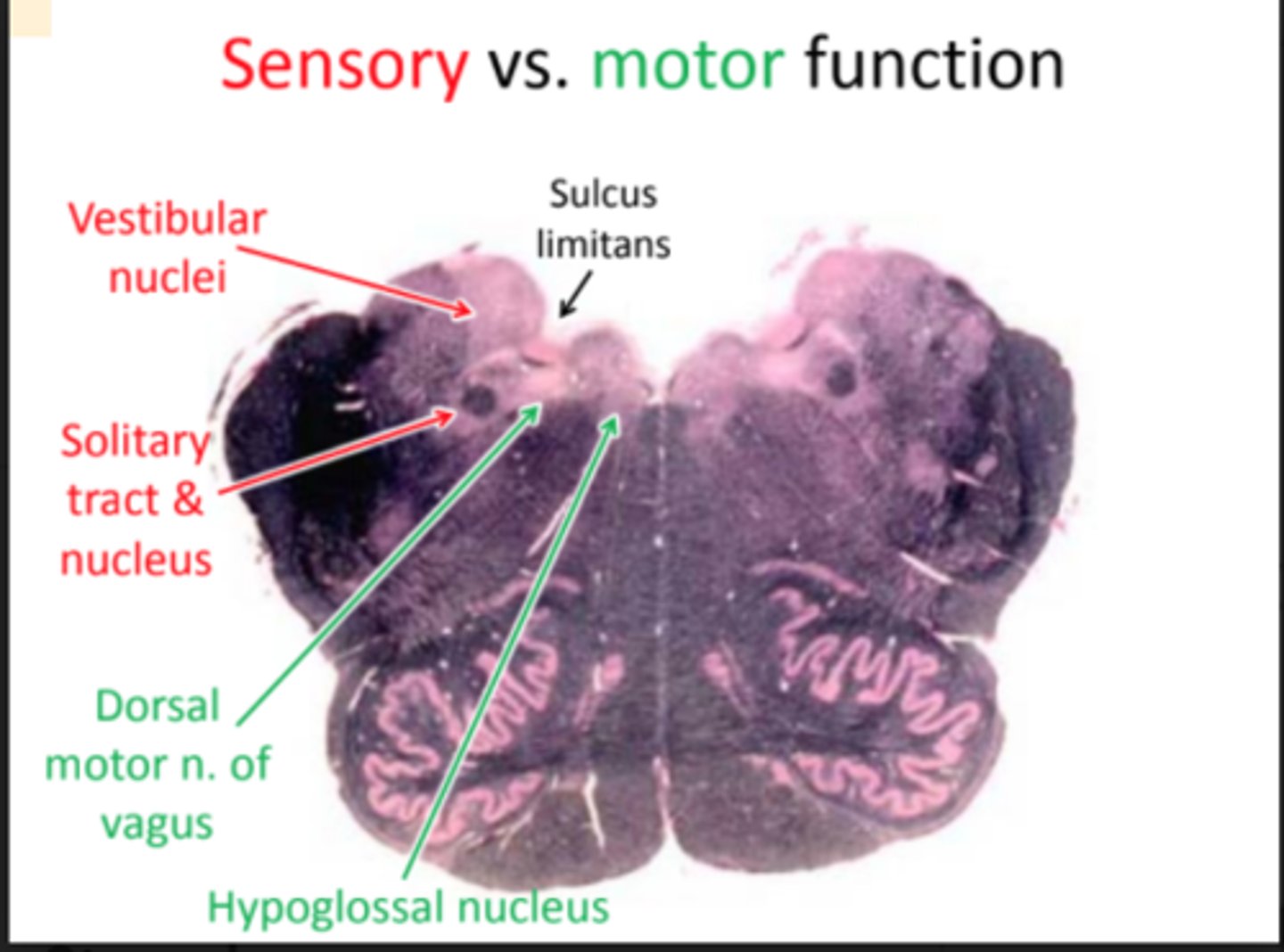
Sensory vs. motor function of medulla
- Separated by sulcus limitans just as in spinal cord
Pons
Pons is marked by the cerebellum lying over its dorsal surface and the pontine nuclei forming a bulge on its ventral surface
Pontine Nuclei
- Create the big bulge of the ventral side of the pons
- At base of brain stem
Pyramids Fascicles
- Pyramidal tracts become surrounded by pontine nuclei and break into bundles called ......
- Made of corticospinal fibers and corticopontine fibers innervating pontine nuclei
- Nuerons in the pontine nuclei then sent axons across the midline to synapse onto cerebellar neurons, letting the cerebellum know what the cortex is doing
Spinothalamic tract (STT) in pons
- STT is in roughly the same place at it was in the medulla, relative to the pyramidal tracts/pyramidal fascicles
Monoamine neurons
The reticular formation has neurons that use monoamines (e.g., serotonin, dopamine, norepinephrine, and epinephrine) as neurotransmitters
- Locus coeruleus: norepinephrine
- Raphe nuclei: serotonin
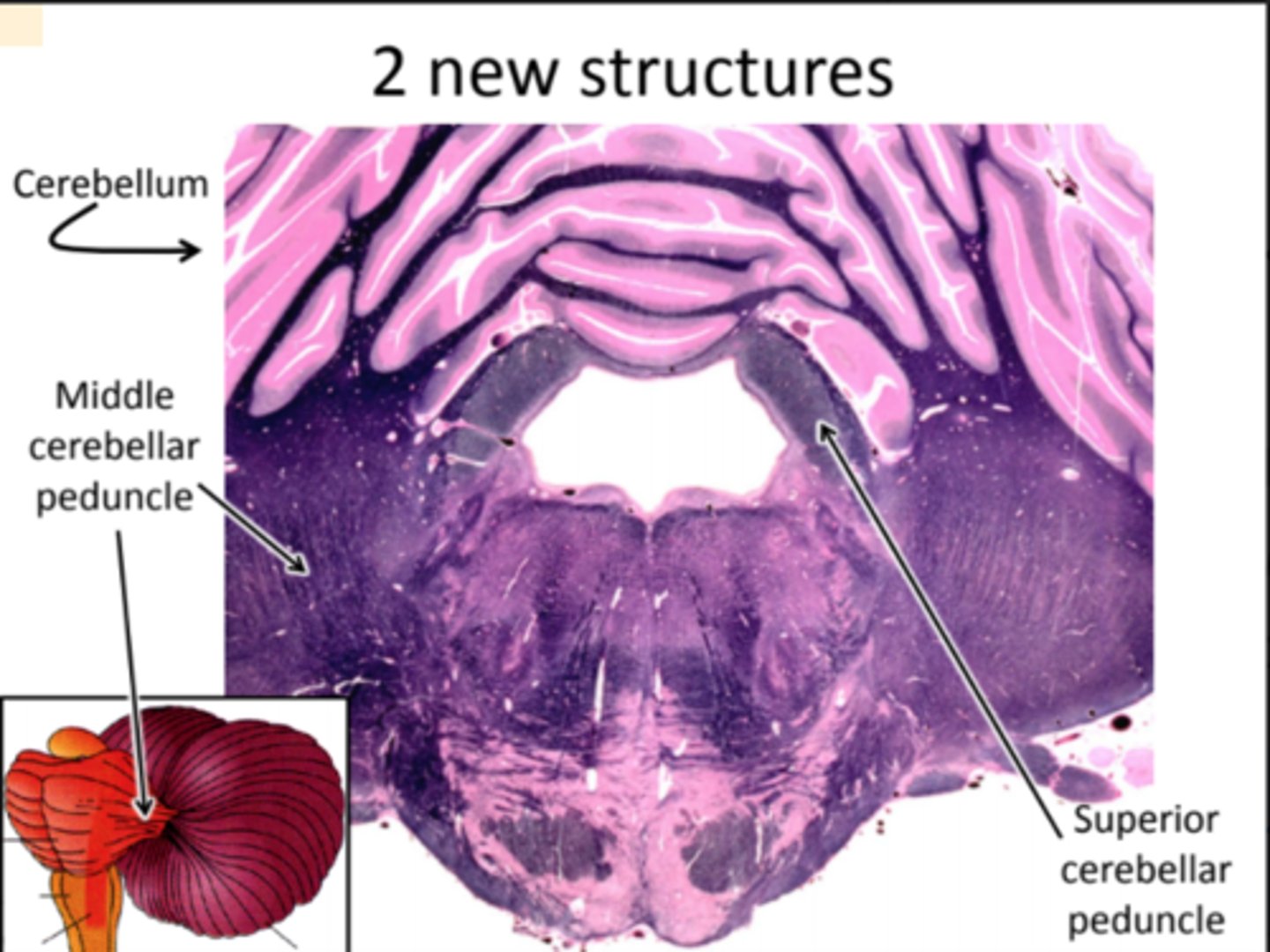
Midbrain: Two new structures
- Cerebellum: attached to pons mainly via middle cerebellar peduncle, which is composed of fibers from the pontine nuclei that have crossed the midline - their axons synapse in the cerebellum
- Superior Cerebellar Peduncle: composed mostly of fibers originating in the cerebellum and projecting to the rostral midbrain and the thalamus
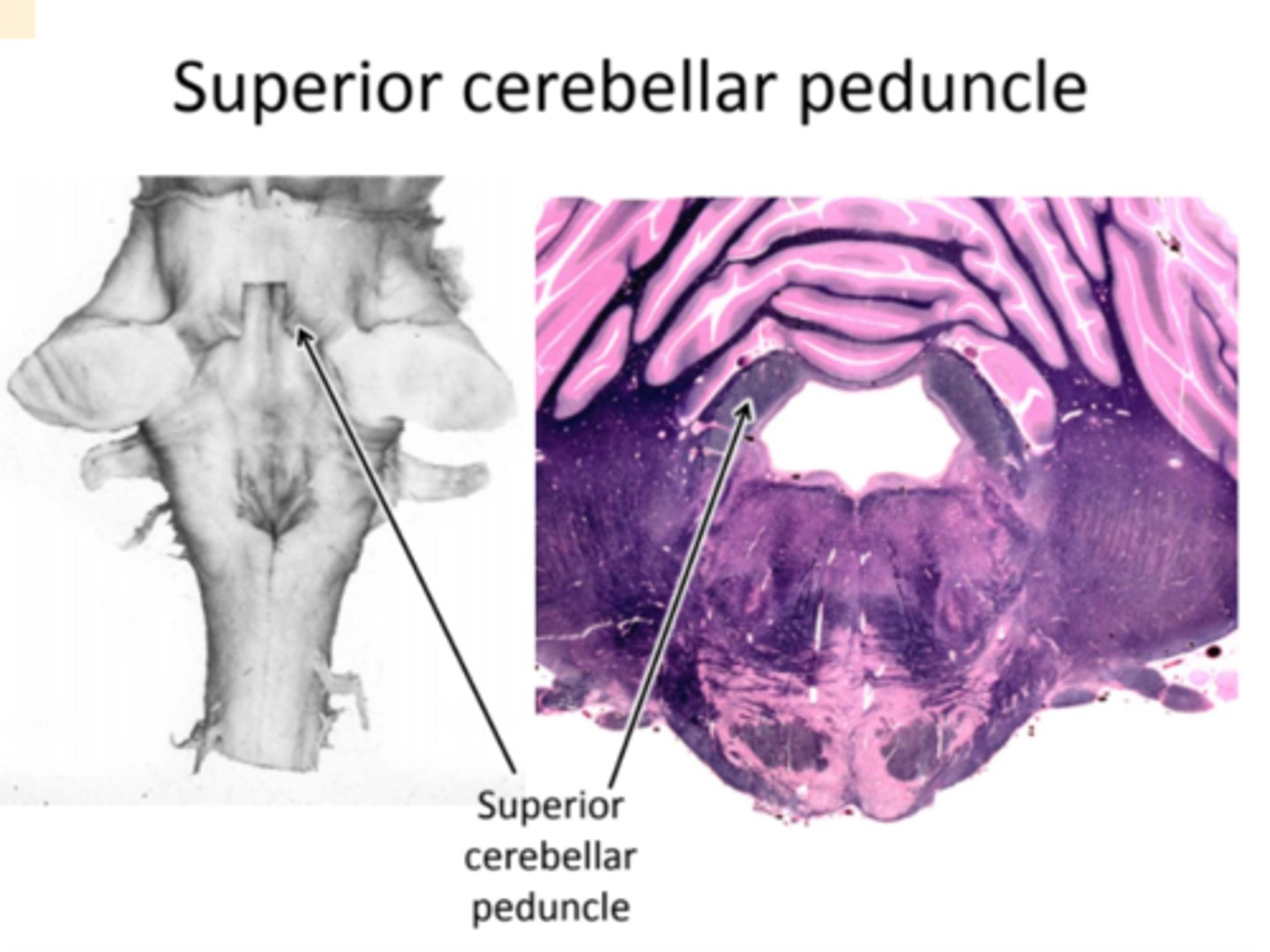
Superior Cerebellar Peduncle
- superior cerebellar peduncle is composed mostly of fibers originating in the cerebellum and projecting to the rostral midbrain (--Red nucleus) and the thalamus. These axons are involved in control of movement
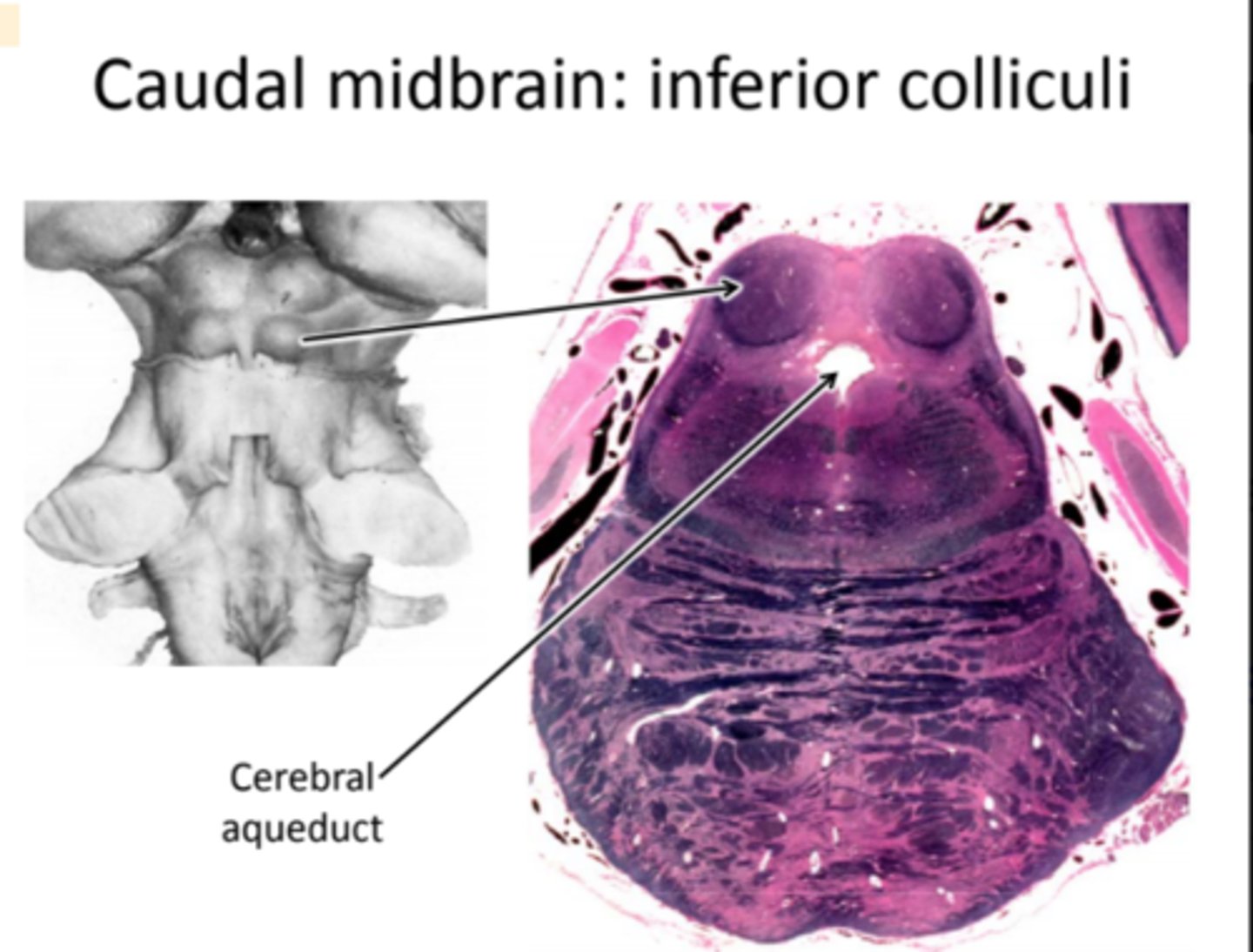
Caudal Midbrain
- Ventricular system is smaller and surrounded by gray matter = cerebral aqueduct
- Middle cerebellar peduncle is smaller (ending).
- Superior cerebellar peduncle has moved ventrally and medially relative to the ventricular system
- Pontine gray is still visible because section is cut at an angle to the neuraxis.
Caudal Midbrain: inferior colliculi
Inferior colliculus has appeared: auditory processing.
- Colliculus: Latin for "small hill"
- There are two pairs of bumps on the dorsal midbrain: the inferior colliculi and the superior colliculi.
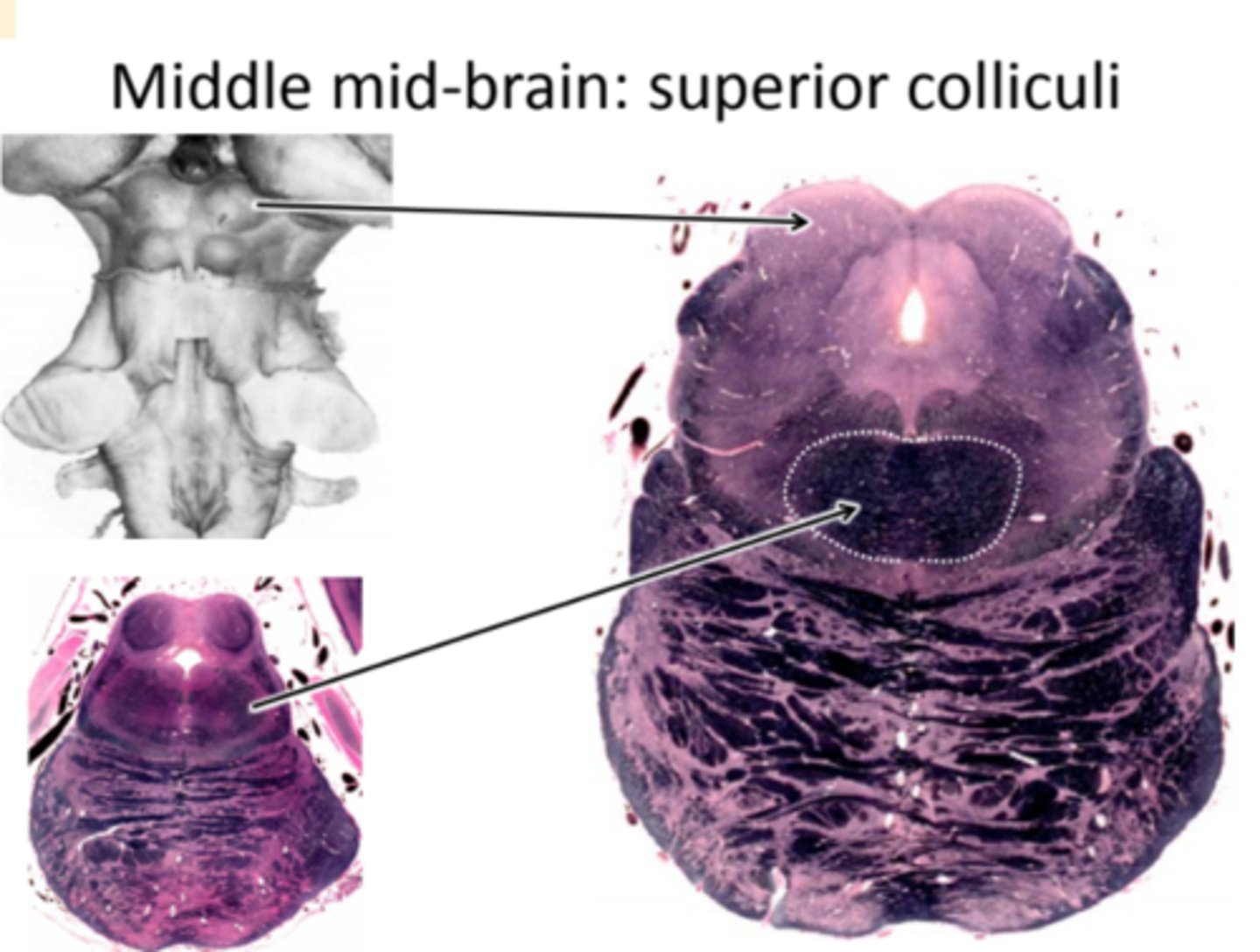
Middle Midbrain: superior colliculi
- Superior colliculus is present: flat, not round. It's not outlined in black like the inferior colliculus
- Cerebral aqueduct is round rather than pointy
- Middle cerebellar peduncle is almost gone
- Superior cerebellar peduncle is crossing midline: Decussation of the Superior cerebellar peduncle
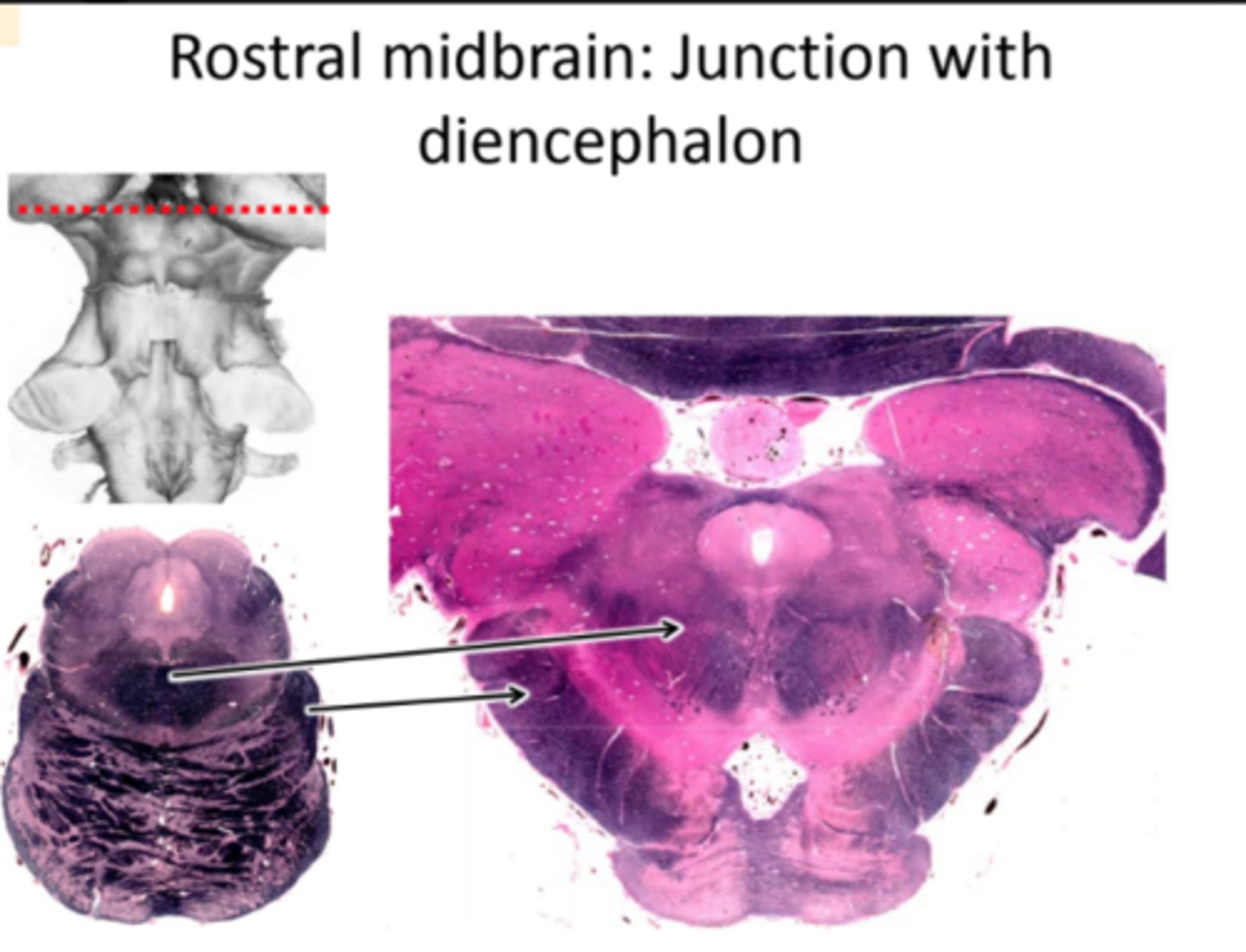
Rostral midbrain: Junction with diencephalon
- This section contains portions of both the midbrain and the diencephalon (e.g., the pulvinar and medial geniculate nuclei).
- Superior colliculi are gone.
- Cerebral peduncles have become fully developed
- Superior cerebellar peduncle is ending in the red nuclei
- Cerebral aqueduct is still present.
Three Primary Brain Vesicles
- Forebrain (prosencephalon) develops into diencephalon, telencephalon, and retina)
- Midbrain (mesencephalon)
- Hindbrain (rhombencephalon)
Diencephalon
- Above the midbrain
- Below and surrounded by the telencephalon
- Includes: hypothalamus, subthalamus, thalamus, and epithalamus
Hypothalamus: many essential functions
- Temperature regulation
- Feeding and drinking
- Circadian rhythms
- Aggression and flight
- Sexual activity
Hypothalamus: neuroendocrine function
Hypothalamic neurons release hormones into the blood that act on the pituitary gland
The pituitary gland is attached to the hypothalamus by the pituitary stalk
Thalamus: 2 types of nuclei
- Relay nuclei: relay specific sensory or motor information to specific regions of cortex
- Diffuse nuclei: have diffuse projections to cortex or within thalamus
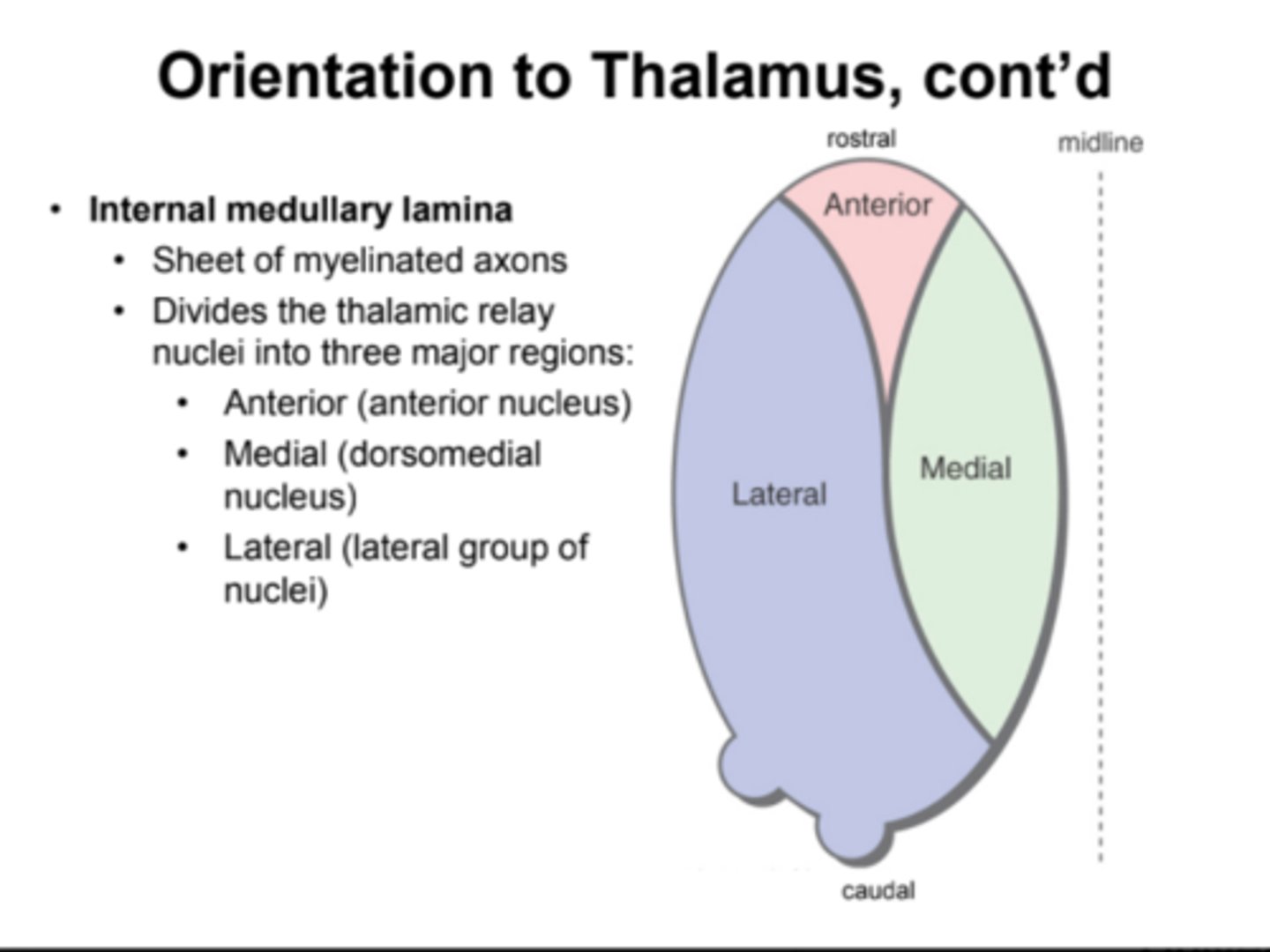
Orientation to. Thalamus
- 2 halves separated by 3rd ventricle
- touch at interthalamic adhesion (thalamic adhesion)
- Internal medullary lamina: sheets of myelinated axons, divides the thalamic relay nuclei into three major regions: anterior, medial, lateral
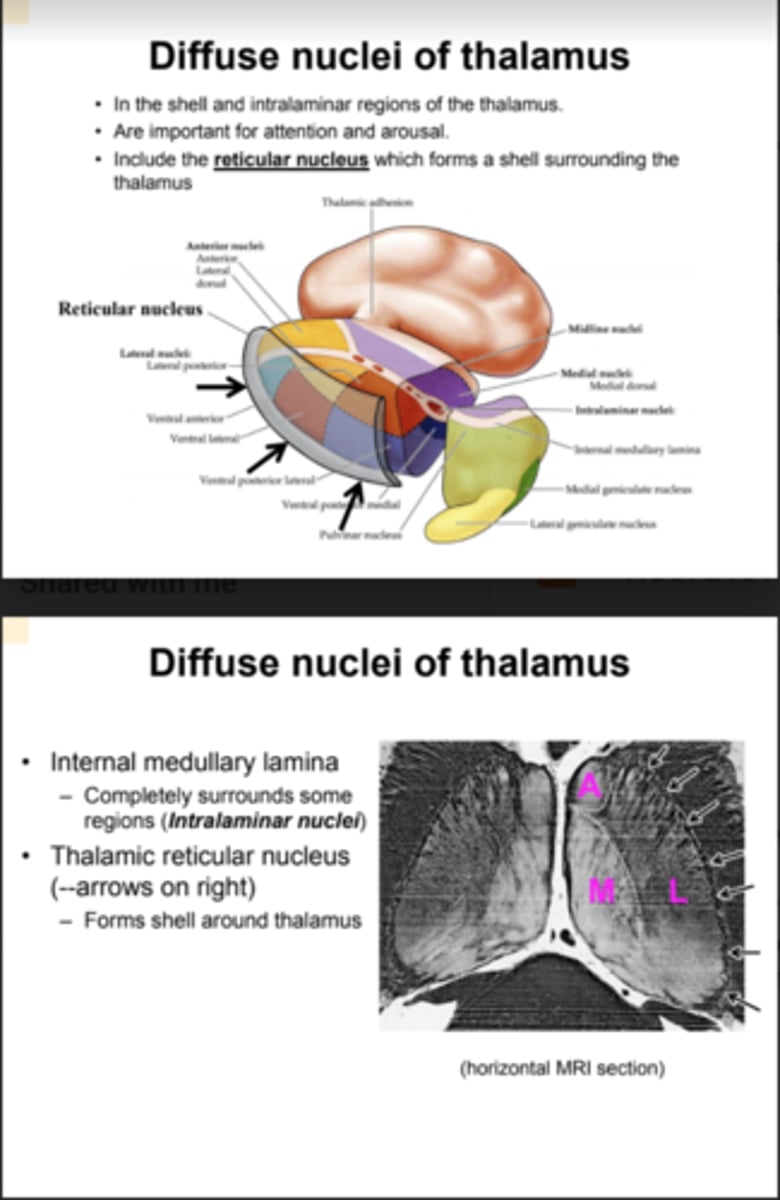
Diffuse nuclei of thalamus
- In the shell and intralaminar regions of the thalamus
- are important for attention and arousal
- include the reticular nucleus which forms a shell surrounding the thalamus
Lateral thalamic relay nuclei
- Relay nuclei send axons to cortex
- Their projection is ipsilateral (to the same side)
- Placement of the nuclei in the thalamus approximately matches the pattern of their connections to cortex
- Lateral group differ from each other by their connections and functions
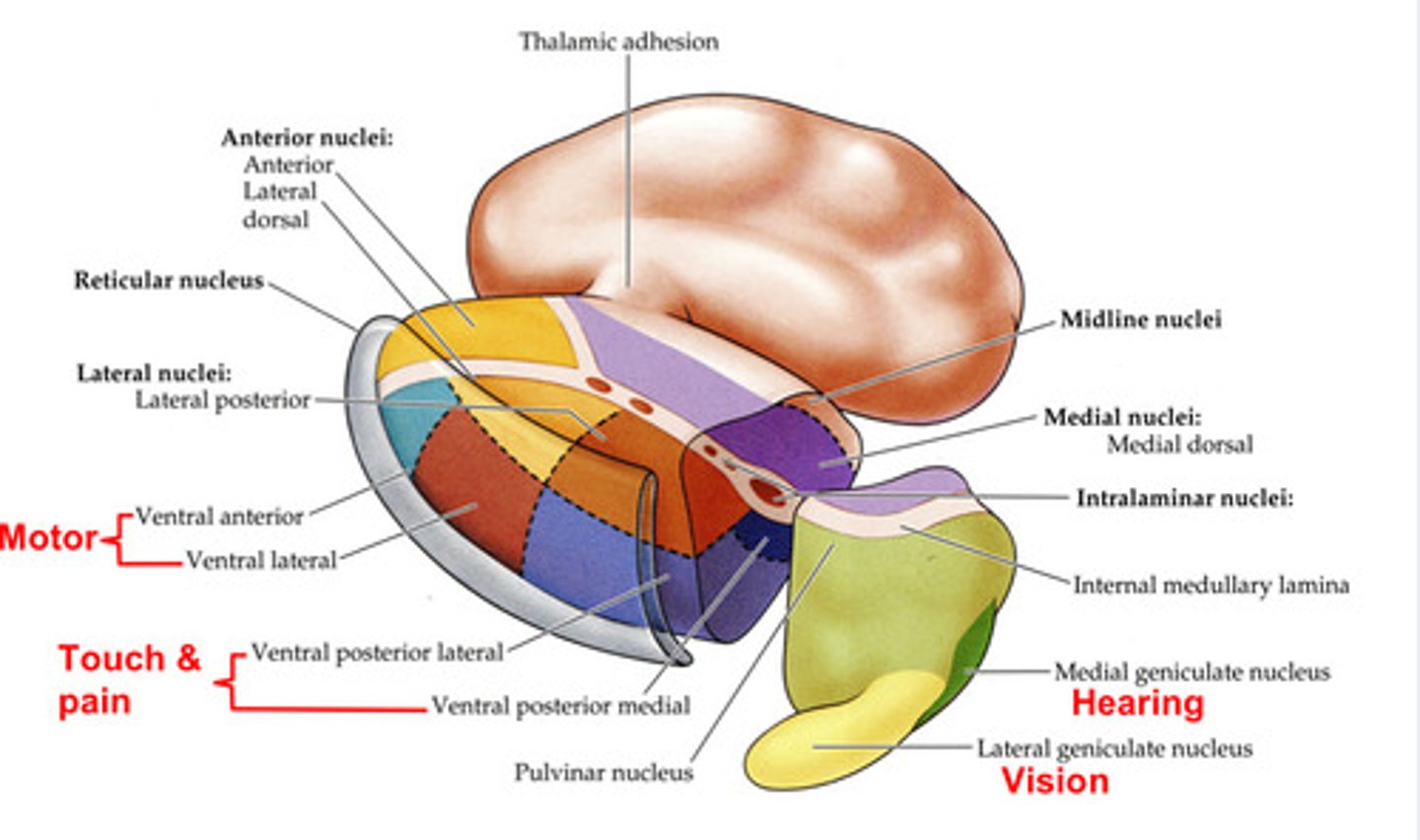
Input/Output of thalamic relay nuclei
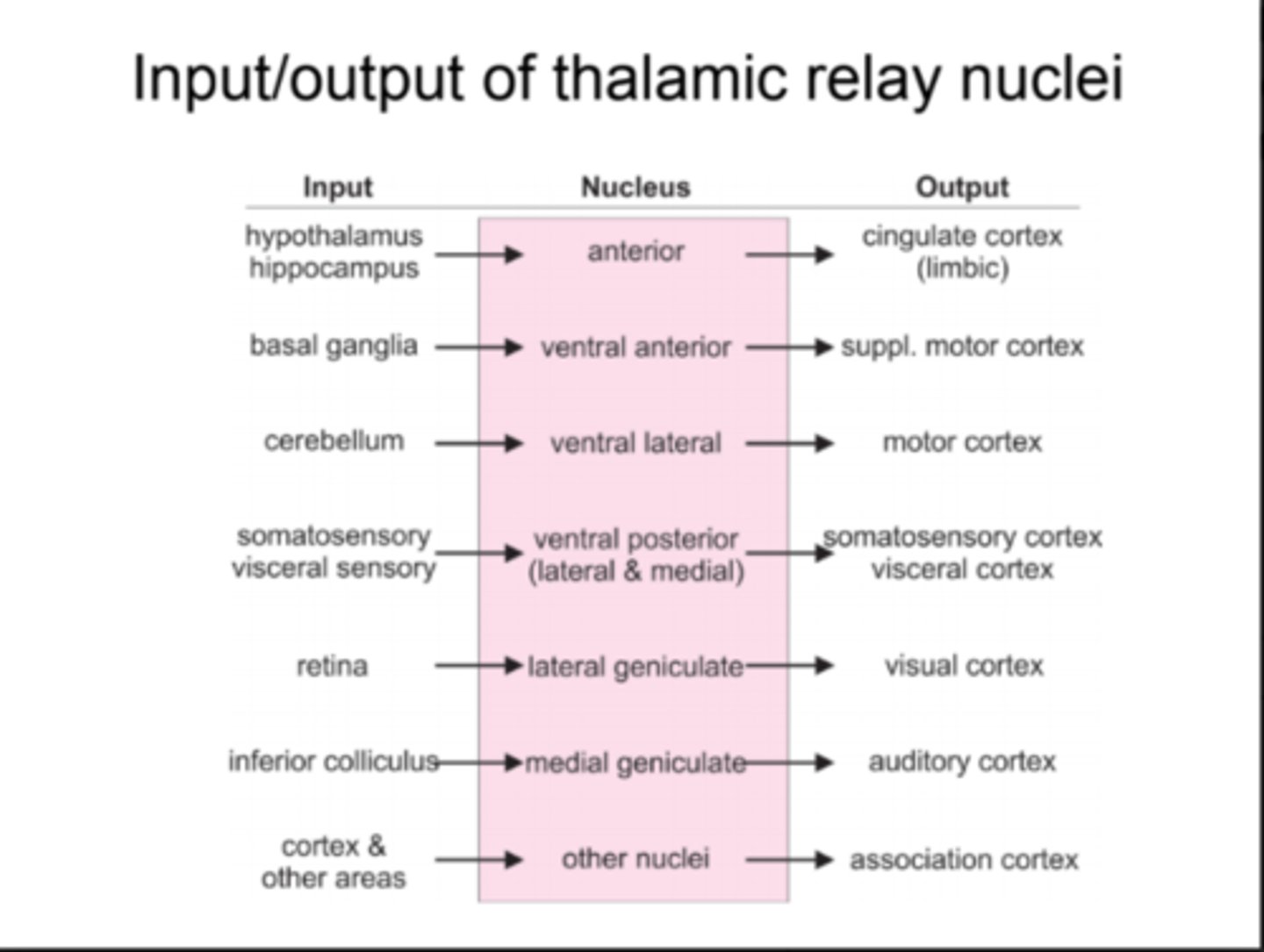
Thalamus to association cortex
Dorsomedial (medial dorsal) nucleus to prefrontal association cortex
Pulvinar to parietal-occipital-temporal association cortex
Both carry information from more than one sense
Thalamus and Information Flow
The flow of information from the thalamus to cortex is gated by inputs from the cortex and from the brain stem reticular activating system (via the reticular nucleus of the thalamus)
- The reticular nucleus inhibits the output of other thalamic nuclei
- Gating is an important way to reduce the flow of information when it is not needed: sleep and concentration
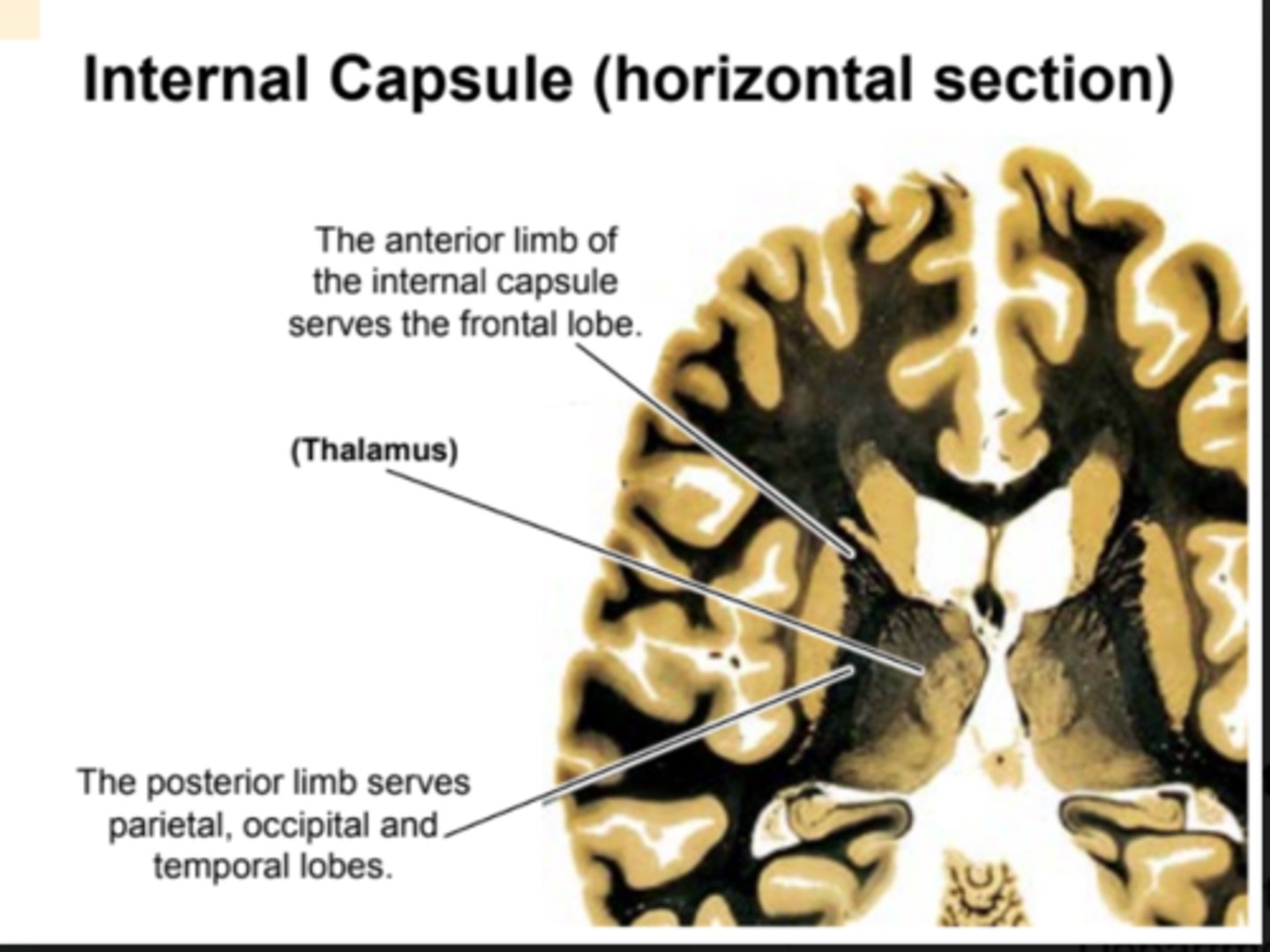
Cortical connections to thalamus: Internal Capsule
A superhighway of axons entering and exiting the cortex
- axons from neurons in thalamus ascend to the cortex via the internal capsule
- Axons from neurons in the cortex descend to thalamus via the internal capsule
- Axons projecting to the brain stem or spinal cord also follow the internal capsule and pass just lateral to the thalamus
Telencephalon
Two hemispheres separated by the interhemispheric fissure
- Three interrelated parts: neocortex, limbic & olfactory systems, basal ganglia
Cerebral Cortex (Neocortex): Five lobes
Frontal, parietal, occipital, temporal, limbic
Structures of cerebral cortex
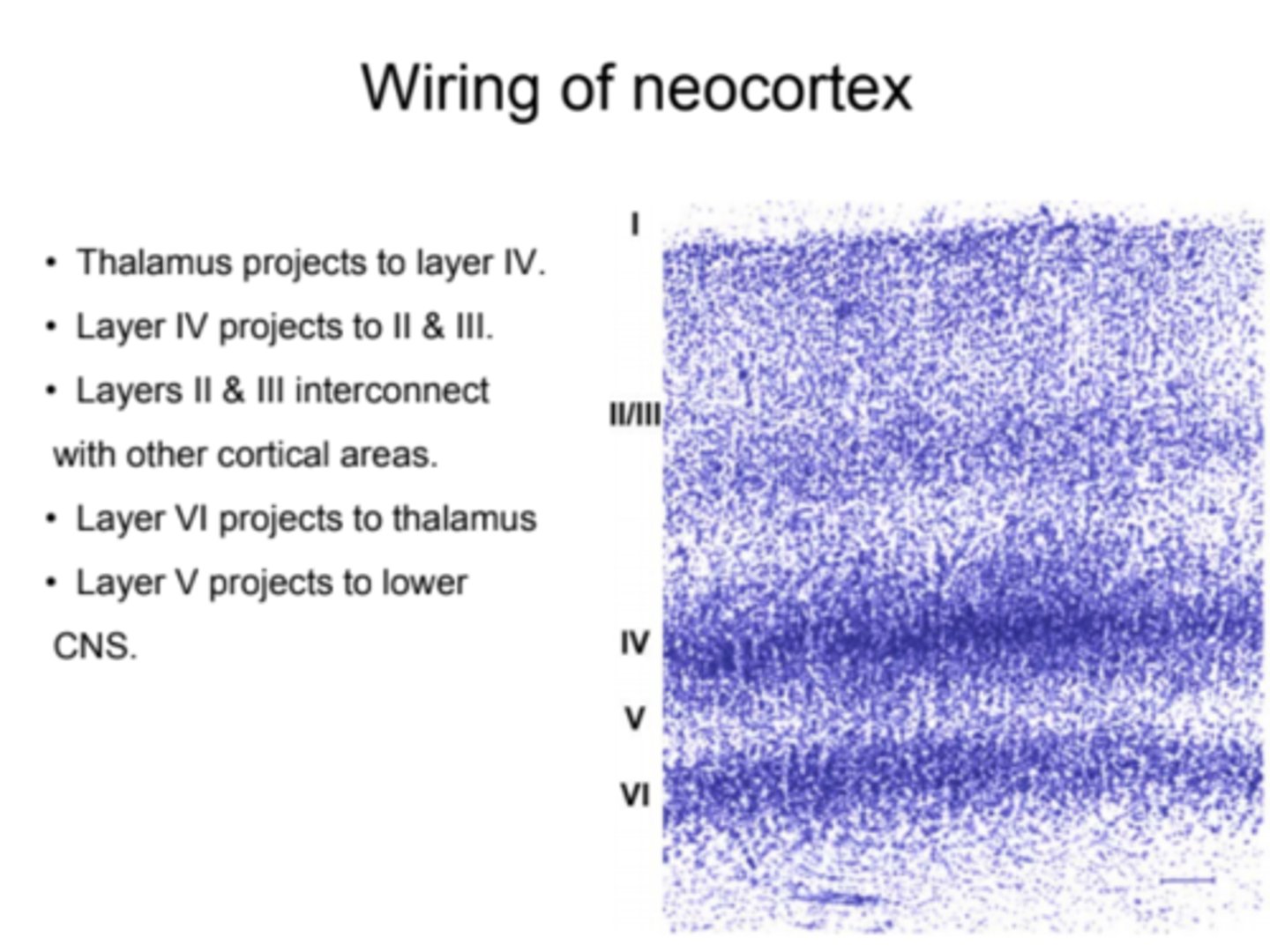
- Neocortex: six cell layers
- Allocortex: 3-5 cell layers, evolutionary old and involves hippocampus
Association Cortex
- Association cortex does not receive direct input from our senses and does not innervate motor nuclei. However, it receives input from cortical regions that DO receive direct sensory input or that directly innervate motor nuclei. Allows more complex and conditional responses than do simple reflexes.
- Located in: parietal cortex, prefrontal cortex, and limbic cortex
Cerebral Commissures
- Discrete bundles of axons that cross the midline: a region of cortex on one side of the brain communicates with the same region on the other side
- Two main commissures of cerebral cortex: corpus callosum and anterior commissure
Lesions of the corpus callosum
- Epilepsy is characterized by seizures, which an result in the uncontrolled contraction of large groups of muscles
- It is caused by synchronous excitatory activity in the cortex that spreads from an activation site
- In severe cases, portions of the corpus callosum can be surgically
However, cutting the corpus callosum can result in a person who effectively has two minds: one in each hemisphere. Each mind is privy only to the information that that hemisphere receives.
Limbic and Olfactory areas
Includes: olfactory bulb and tract, hippocampus, septal area, amygdala, anterior commissure and PARTS OF: prefrontal cortex, cingulate gyrus, anterior nucleus and other nuclei of the thalamus, mammillary bodies and other nuclei of hypothalamus, midbrain reticular formation
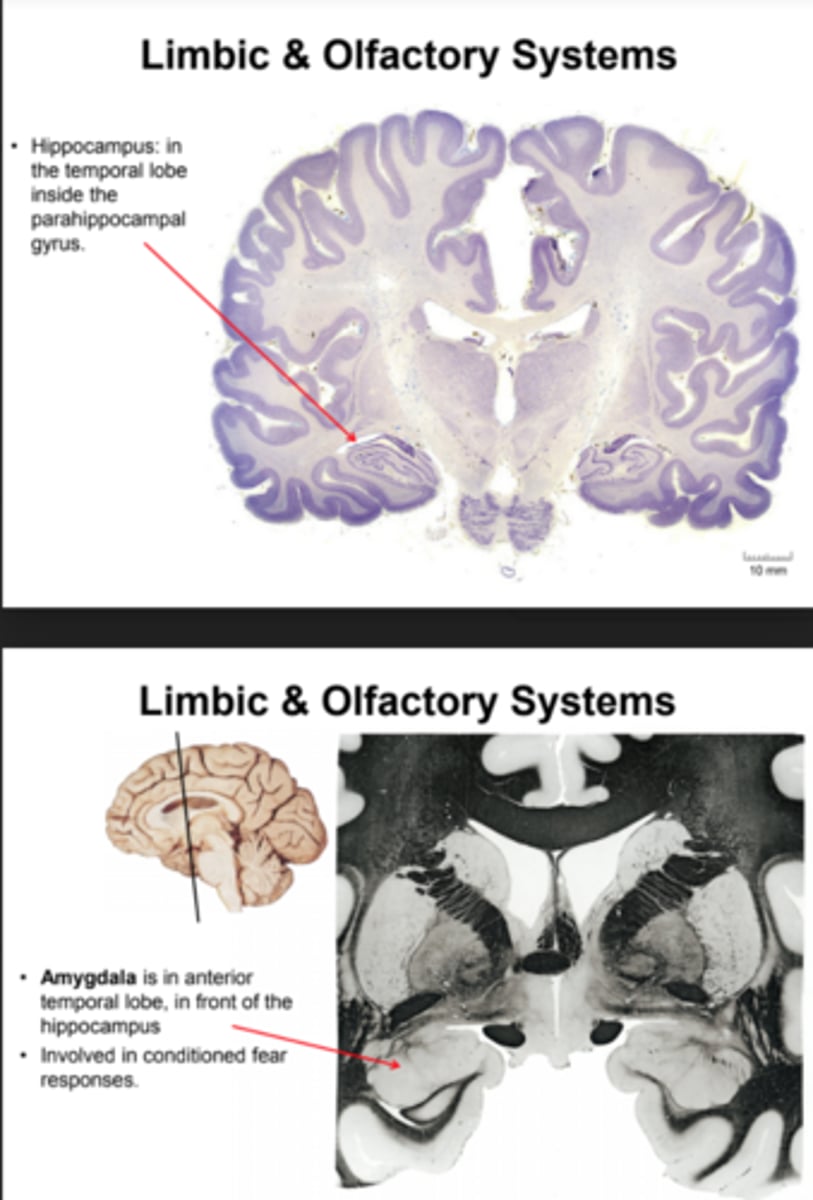
Limbic and Olfactory systems
- Hippocampus is in the temporal lobe inside the parahippocampal gyrus
- Amygdala: is in anterior temporal lobe, in front of the hippocampus (involved in conditioned fear responses)
- Basal Ganglia: group of nuclei in the midbrain, diencephalon, and basal region of the telencephalon (important role in the motor system and motivation (incl. drug abuse))
- Major Nuclei: Striatum (telencephalon), Globus pallidus (telencephalon), subthalamic nucleus (diencephalon), Substantial nigra (midbrain)
Limbic System, learning and memory: the Papez Circuit
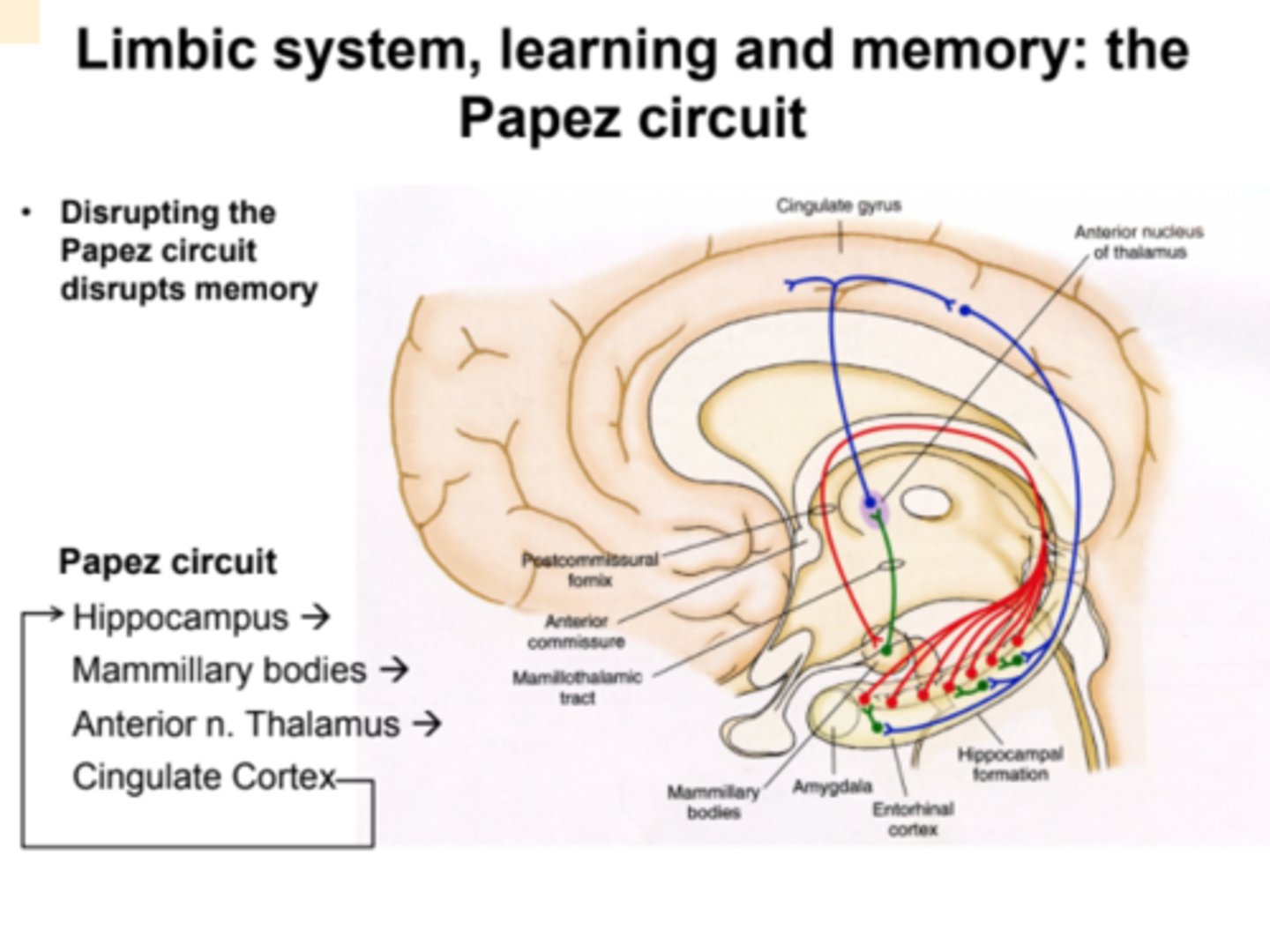
Tracts of the limbic system
- Fornix: hippocampus to mammillary bodies
- Mammillothalmic tract: mammillary bodies to anterior nucleus of thalamus
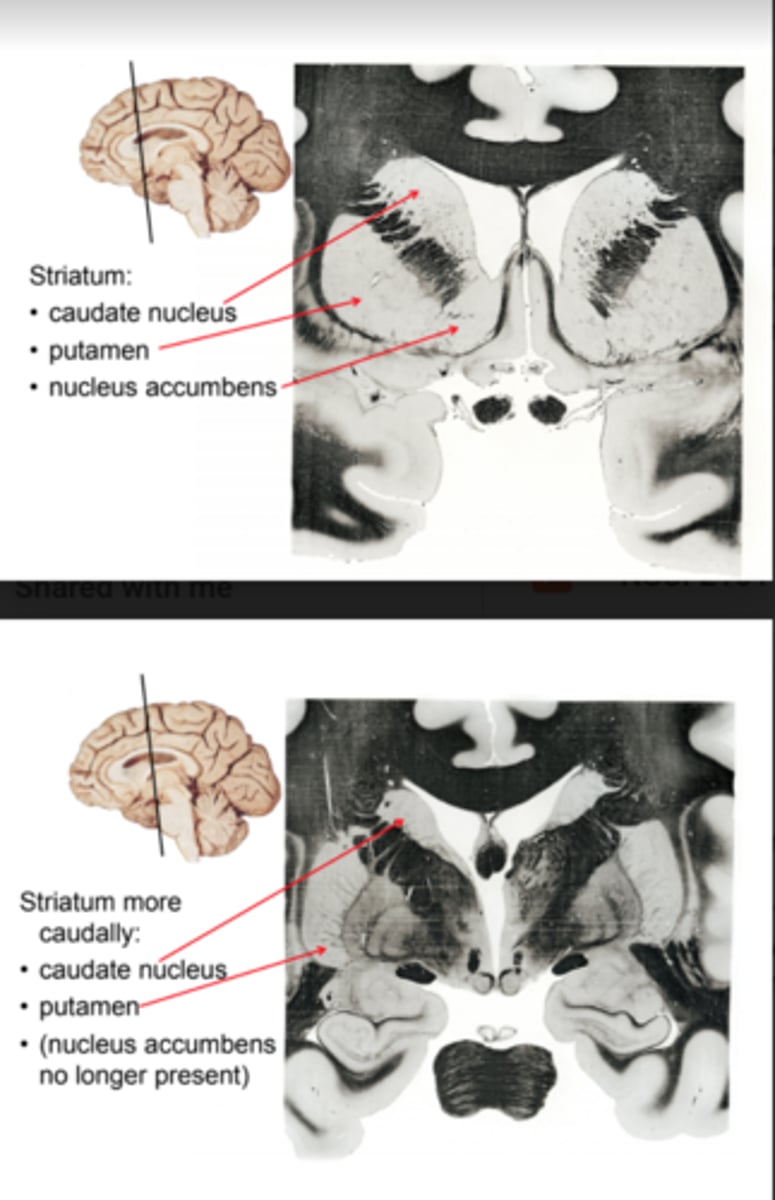
Basal Ganglia Anatomy: Striatum
- Three sub-nuclei: caudate nucleus, putamen, nucleus accumbens
- Can be thought of as one nucleus: sometimes divided by the internal capsule, forms a single structure at the anterior-most part of the internal capsule
globus pallidus
Two divisions:
- External (GPe): internal circuitry of globus pallidus
- Internal (GPi): output circuitry
Basal Ganglia: subthalamic nucleus
Part of diencephalon, positioned just ventral to the thalmus and dorsal to the midbrain
Twelve Cranial Nerves (CN)
1. Olfactory
2. Optic
3. Oculomotor
4. Trochlear
5. Trigeminal
6. Abducens
7. Facial
8. Vestibulocochlear
9. Glossopharyngeal
10. vagus
11. spinal accessory
12. hypoglossal
- "On old Olympus's towering tops, a Finn and German viewed some hops"
CN that carry one of the special sense
1. Olfactory (smell)
2. Optic (vision)
8. vestibulocochlear (Hearing)
Five CN innervate skeletal muscle
3. Oculomotor (eye)
4. Trochlear (eye)
6. Abducens (eye)
11. Spinal accessory (neck/shoulder)
12. Hypoglossal (tongue)
One CN innervates muscle but also carries "general sensation" (touch, vibration, pain)
5. Trigeminal (jaw muscles; sensation for face, head, mouth)
Three are mixed function: innervate skeletal muscle, carry a special sense [taste], carry general sensation, innervate autonomic ganglia
7. Facial
9. Glossopharyngeal
10. Vagus
CN1: Olfactory nerve
- Olfactory nerves are embedded in the mucosa of the upper nasal cavity and have receptors for thousands of scents. They project their axons through small holes in the anterior cribiform plate, in the floor of the skull.
- Olfactory nerves synapse onto olfactory bulbs
CN 2: Optic Nerve
retinal ganglion neurons to the optic nerve to the optic chiasm to the optic tract to the lateral geniculate nucleus (thalamus) to the visual cortex (occipital lobe)
CN 8: Vestibulocochlear nerve
- Emerges from inferior pontine nucleus, the groove at the caudal, ventral edge of the pons, out on the lateral edge of the brain stem, adjacent to the medulla
- Hearing and Balance: cochlea (senses sound) and vestibular apparatus (senses head position and movement) are physically connected and both contain 'hair cells' with cilia on them.
CN 3: Oculomotor Nerve
- Oculomotor nerve: 4 of 6 extraocular skeletal muscles (plus eyelid)
- Extraocular muscles direct our gaze to what we want to look at, without our having to turn our heads.
- Medial rectus is what we use to cross our eyes.
- Inferior oblique moves the eye up and lateral.
- Inferior and superior rectus move eye down & up respectively.
- Oculomotor nerve also is responsible for the muscle allowing conscious opening of the eyelid.
ALSO
Parasympathetic output of oculomotor nerve: focuses lens and constricts pupil (neurons in oculomotor also innervate the ciliary ganglion in the back of orbit ("eye-socket") in turn controls focus and pupil diameter
CN 4: Trochlear Nerve
- Only cranial nerve to exit the dorsal surface of the brain
- superior oblique pulls gaze down and lateral
CN 6: Abducens nerve
- Lateral rectus muscle
- Each abducens nerve innervates the lateral rectus muscle for that eye (right nerve will cause right eye to look right; left nerve will cause left eye to look left)
CN 11: Spinal Accessory Nerve
Unusual Cranial Nerve!
- Its motoneurons arise from spinal cord - fibers form a bundle of roots (arrows) that enters skull through foramen magnum
- Nerve exits through jugular foramen
- Innervates trapezius and sternocleidomastoid
- May also carry axons originating in brain stem and innervating larynx
CN 12: Hypoglossal Nerve
- Emerges between olive and pyramids!
- Skeletal muscles in tongue
- genioglossus, styloglossus, hyoglossus, and more muscles within tongue
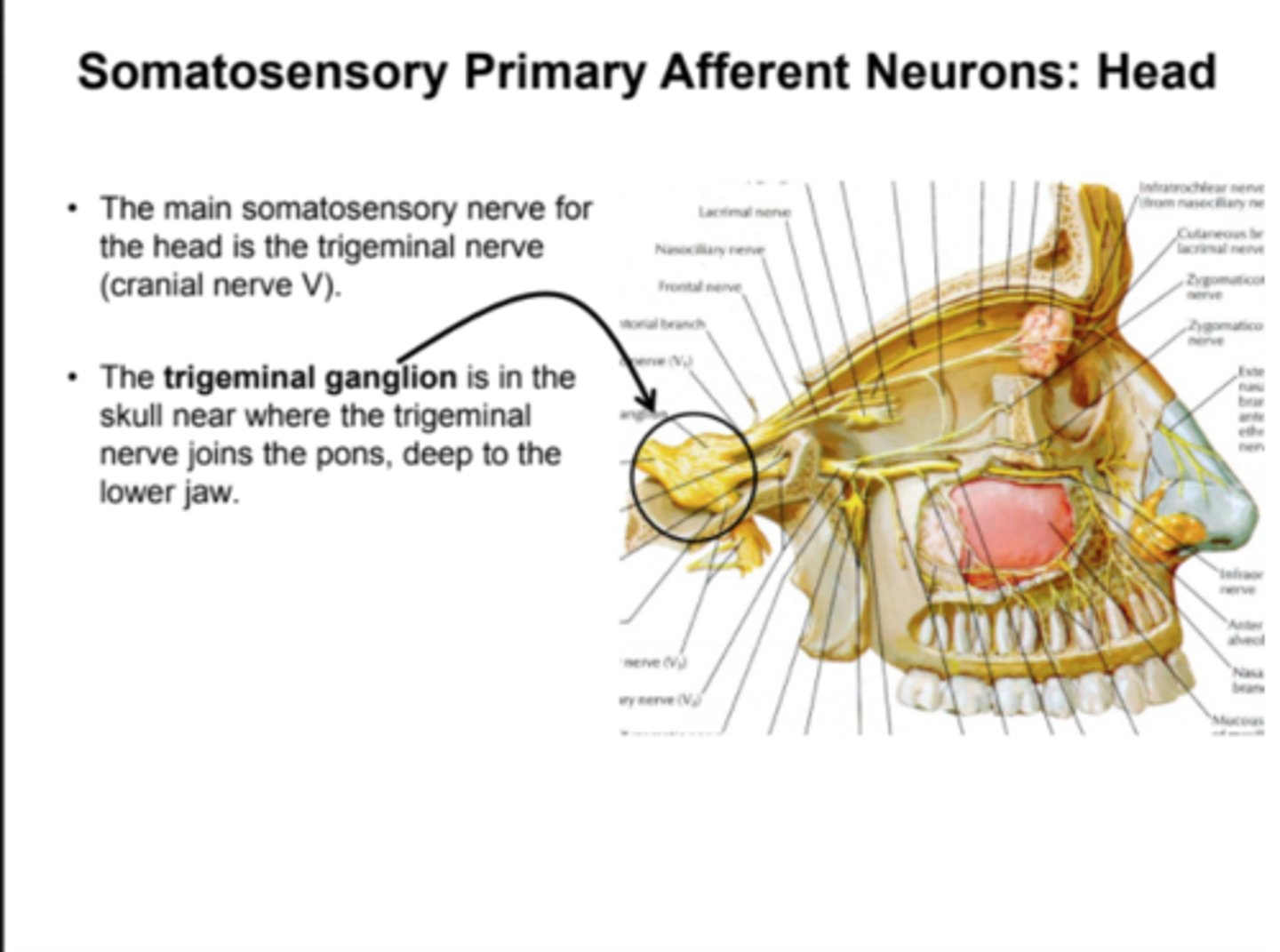
CN 5: Trigeminal nerve
Only cranial nerve to exit pons
- Muscles of mastication (i.e., chewing; temporalis, masseter)
- Cutaneous sensation to face & head into 3 subdivisions: ophthalamic (forehead), maxillary (cheek and nose), mandibular (lower jaw)
CN 7: Facial Nerve
- Superficial muscles embedded in, and attached to, the skin of the face.
- Innervates skeletal muscle (facial expression muscles)
- innervates autonomic ganglia (pterygopalatine g.: lacrimal gland and nasal mucosal glands; submandibular g.: sublingual and submandibular salivary glands)
- carries general sensory afferents (touch)
- carries special sensory afferents (taste; innervates taste receptors in anterior 2/3 of tongue)
CN 9: Glossopharyngeal nerve
- Innervates skeletal muscle (stylopharyngeus m.: elevates pharynx during swallowing)
- innervates autonomic ganglia (otic ganglion: parotid salivary gland)
- carries general sensory afferents (touch, pain, etc. from posterior 1/3 of tongue)
- carries special sensory afferents (taste; taste receptors in posterior 1/3 of tongue)
- carries information about O2 and CO2, and/or blood pressure (carotid artery)
CN 10: Vagus nerve
- Innervates skeletal muscle (throat and larynx)
- innervates autonomic ganglia (input to heart and gut; slows heart and speeds digestion)
- carries general sensory afferents (touch: behind ear, larynx)
- carries special sensory afferents (taste; back of throat)
- carries information about O2 and CO2, and/or blood pressure (sensors in aortic arch)
Sensory System
Used by an organism to monitor the state of it's body and its environment
Sensory systems
Somatosensory, Visceral sensory, special sensory (vision, auditory, vestibular, gustatory, olfactory)
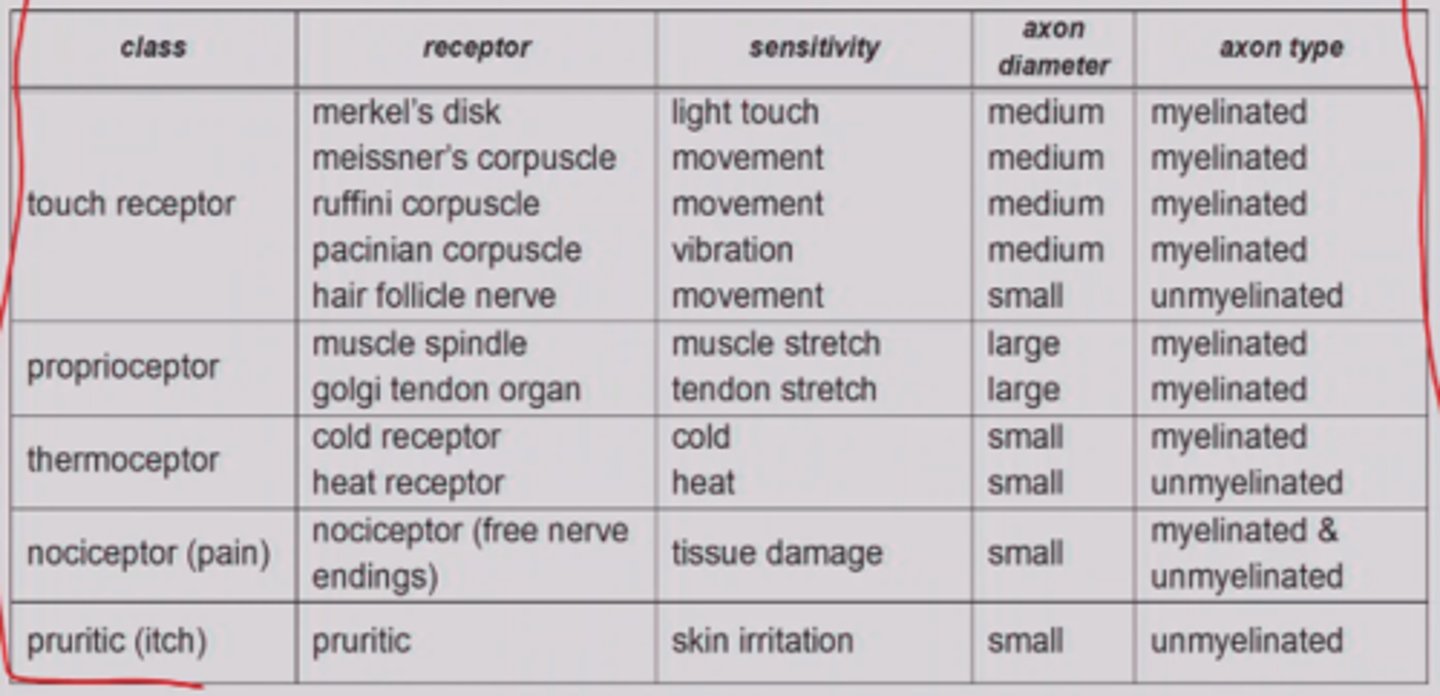
Somatosensory Systems detects
Multiple sensations
- Touch: fine touch, pressure, vibration, hair movement, movement against the skin
- Proprioception: limb and trunk position, limb movement, load
- Thermoception (temperature)
- Nociception (pain--tissue damage)
- Pruriception (itch)
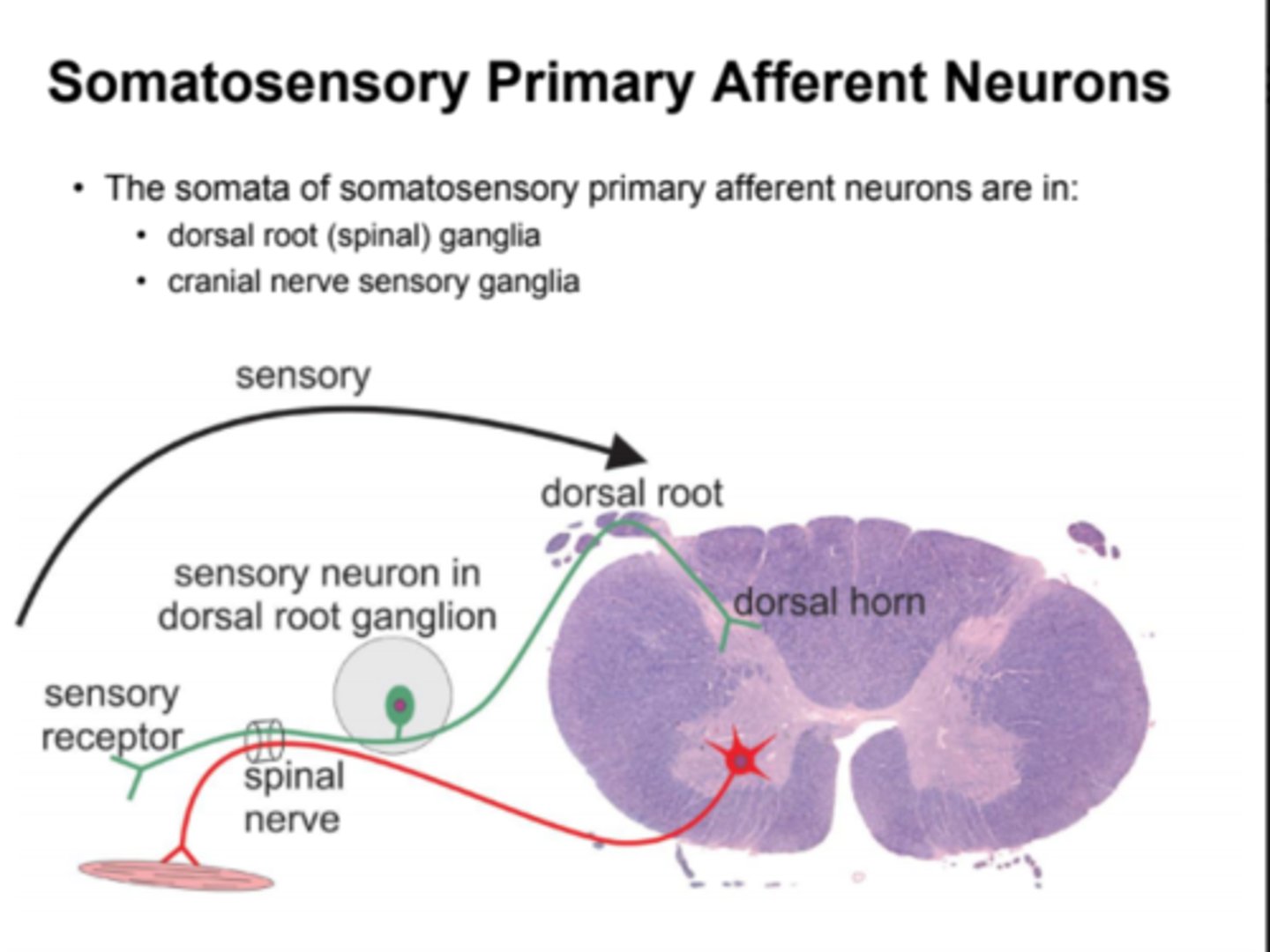
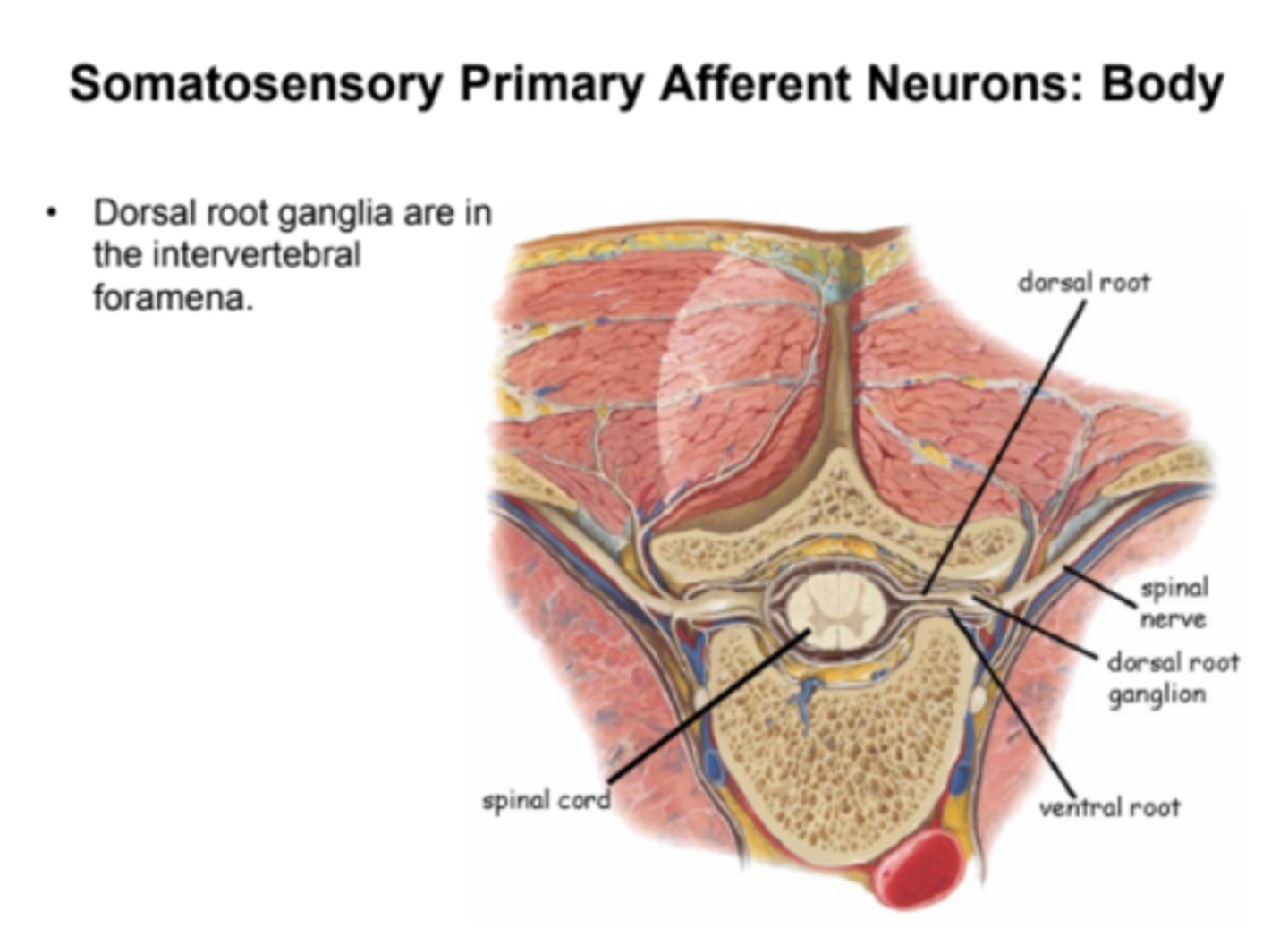
Somatosensory Primary Afferent Neurons
- Peripheral processes of somatosensory primary afferent neurons remain outside the CNS.
- However, their central processes enter the CNS as dorsal rotos
- Dorsal roots only contain axons of sensory neurons
- Peripheral processes of dorsal root ganglion neurons are distributed throughout the body via spinal nerves
- Spinal nerves are composed of a mixture of sensory and motor axons from a single spinal cord segment
- Soma (cell body) of a somatosensory neuron hangs off the middle of the axon in the ganglion. The peripheral processes responds to touch, pressure, or pain by generation of an action potential
- Sensory receptors are found at the ends of the peripheral processes of neuron (each neurons receptors are specialized to respond to particular stimuli)
Somatosensory Primary Afferent Neurons: Body
Somatosensory Primary Afferent Neurons: Head
Peripheral Distribution of Somatosensory Axons
- The peripheral axons of sensory primary afferent neurons innervate body regions that correspond to the spinal cord segments the axon projects to
- These body segments are called 'dermatomes.' Each spinal nerve innervates its own dermatome.
Touch
- Mechanoreception is detection of mechanical force (texture, pressure, vibration, movement)
- Receptors are broadly distributed through the body. They are the most concentrated in the skin
- Touch receptors are encapsulated by non-neuronal cells or are associated with hair follicles
- Encapsulation changes the response properties of the receptor
- Type of encapsulation, depth in the skin, and sensory receptor proteins expressed by neuron determine the stimulus that activates a sensory cell
Sensory Cell (touch)
- Merkel's disk: under each ridge of fingerprint; Merkel cells (capsule) amplifies signal, sensitive to light touch and movement via different axons; mostly in hairy skin
- Meissner corpuscle: encapsulated in layers of Schwann cells; in dermis; sensitive to light touch and vibration, mostly in hairless ksin
- Ruffini Corpuscles: in dermis, capsule is elongated; sensitive to direction of movement across skin and to stretch of skin and other tissues
- Pacinian corpuscle: deep in skin; rapidly responding; sensitive to vibration and deep pressure
- Hair follicle receptor: axons forms a plexus around hair follicle; detects movement of the hair
Density of touch
Density of touch receptors in our skin determines the resolution of our sense of touch in different parts of the body - two point discrimination
Proprioception
Sense of the position, movement, and load of the limbs and trunk
- Proprioceptors are also mechanoreceptors but are specialized for proprioception
- Muscle spindles: sense organs for muscle length. they consist of nerve endings wrapped around a special intrafusal muscle fiber embedded in muscle. Fire when muscle is stretched and provide information required to adjust the strength of muscle contraction in response to external forces
- Golgi tendon organs: embedded in collagen fibers of tendons. they are compressed by tension (sensitive to the force exerted by tendon). Help prevent muscles from exerting more force than they can safely bear
Somatosensory Receptors Table
Somatosensory Receptors
- A stimulus, if sufficiently strong, results in sodium channels
opening and an influx of sodium into the nerve ending. This
results in a graded depolarization of the membrane
potential.
- The stronger the stimulus, the larger the membrane depolarization.
- With sufficient depolarization (i.e., greater than threshold),
voltage-gated sodium channels open in the initial segment of
the axon, and an action potential is generated.
- The frequency of action potentials encodes the strength and
duration of the stimulus.
Functions of somatosensory input
Local (spinal) reflexes and input to brain
Somatosensory spinal reflexes
Require few (e.g. 1 or 2) synapses; all synapses occur
in spinal cord
- Knee-jerk reflex to muscle stretch
• Response occurs in the muscle that was stretched
- Flexor-withdrawal reflex to skin pain (e.g., stepping on a Lego)
• Sensation in skin; response in muscle
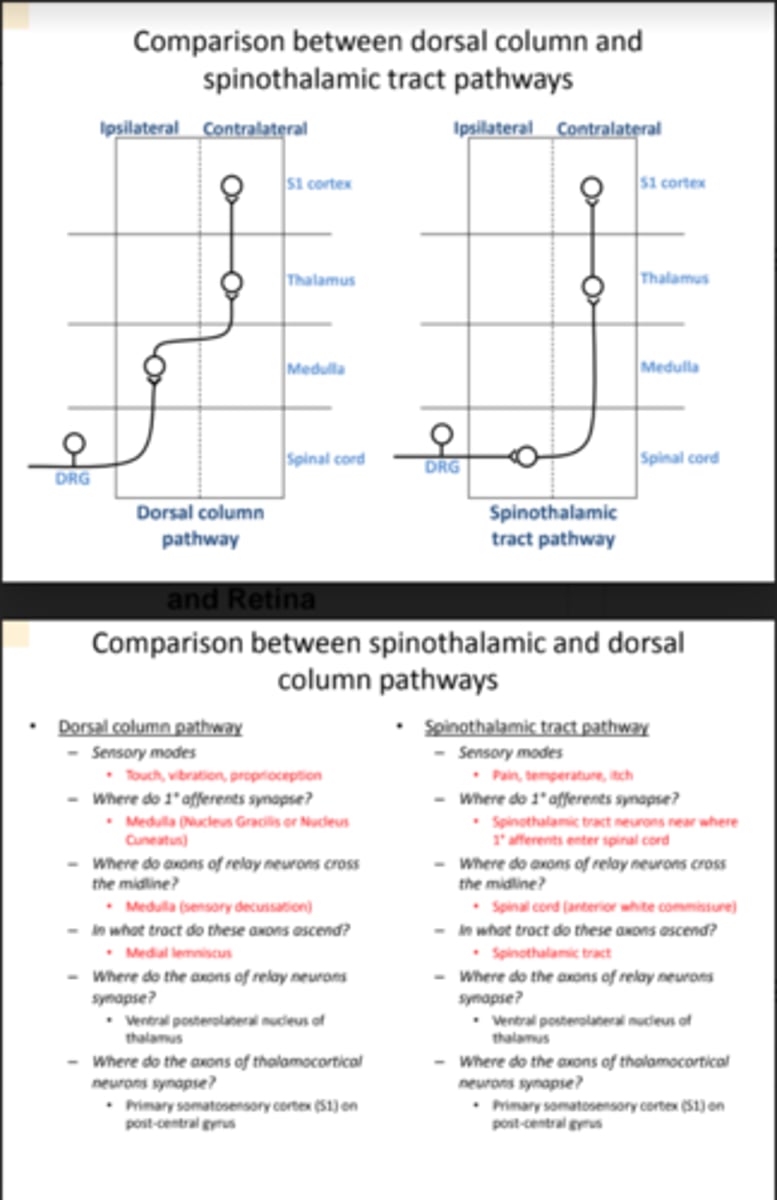
Somatosensory pathways ascending to brain
To (ipsilateral) cerebellum
- Spinocerebellar tract carrying proprioception
• To (contralateral) cerebral cortex
- Dorsal column pathway carrying touch, vibration
- Spinothalamic tract pathway carrying temperature, pain, itch,
some touch
Spinocerebellar pathway
Primary sensory neurons carrying
proprioceptive information synapse
deep in the dorsal horn.
• Second order neurons ascend on both
sides of the spinal cord in the
spinocerebellar tracts.
• These axons synapse mainly on the
ipsilateral side of the cerebellum.
• The cerebellum has important roles in
maintaining balance and coordinating
movements.
- Spinocerebellar tracts are in the lateral funiculus of the spinal cord
Somatosensory Projections to Cerebral Cortex
- Primary afferent neurons carry somatosensory information into the
ipsilateral CNS
- Axons of relay neurons cross the midline to carry somatosensory
information to the contralateral thalamus
- Thalamic neurons project their axons to somatosensory cortex
without crossing the midline again
Two pathways from periphery to cerebral cortex:
- proprioception and most touch via the dorsal columns
- Pain, temperature, itch, and some touch via the spinothalamic tracts
Dorsal Columns Projection to Cerebral Cortex
1. Primary sensory axons for
proprioception and touch enter the
dorsal horn and do NOT synapse.
Rather, they ascend in the
ipsilateral dorsal columns.
2. These axons finally synapse in
nucleus gracilis (from lower body)
and nucleus cuneatus (from upper
body) in the medulla.
3. Axons from these nuclei cross the
midline and ascend to synapse in
the ventral posterolateral nucleus
(VPL) of the thalamus.
4. Axons from VPL neurons ascend
through internal capsule to synapse
in primary somatosensory cortex.
Dorsal columns are in dorsal funiculus
Somatosensory Projection to Cerebral Cortex 1
Axons entering via the dorsal
root join the dorsal column along
the border with the dorsal horn.
• New axons add onto the lateral
edge of the dorsal columns
• Therefore:
• Fasciculus gracilis carries
axons from the lower body.
• Fasciculus cuneatus carries
axons from the upper body.
In the medulla, nucleus
gracilis receives the axons
from the lower body, and
the cuneate nucleus
receives the axons from
the upper body.
• The output axons from
these nuclei cross the
midline and ascend to the
thalamus as the medial
lemniscus.
Axons from neurons in nucleus gracilis and nucleus cuneatus
ascend in the medial lemniscus and synapse in the ventral
posterolateral nucleus of the thalamus.
Somatosensory Projection to Cerebral Cortex 2
Axons from neurons in the
ventral posterolateral
nucleus in the thalamus
project to primary
somatosensory cortex (S1
cortex) in the postcentral
gyrus of the parietal lobe.
• S1 is called "primary"
somatosensory cortex
because it receives
somatosensory information
from the periphery by the
most direct route, and most
densely of all cortical
regions.
Information from the
spinothalamic tract
projects from the ventral
posterolateral nucleus of
the thalamus to primary
sensory cortex (S1
cortex)
• Pain information also
projects to limbic cortex
resulting in motivation to
avoid
For intractable pain,
spinothalamic axons can be cut
surgically as they cross the
midline or as they ascend in the
spinothalamic tract.
Somatosensory Projection to Cerebral Cortex: Spinothalamic projection
Spinothalamic projection:
• Primary sensory axons for pain,
temperature, itch, and some touch
synapse on neurons in the dorsal
horn.
• Axons of these dorsal horn neurons
cross the midline of the spinal cord
and ascend in the contralateral
spinothalamic tract.
• They synapse in the ventral
posterolateral nucleus (VPL) of the
thalamus.
• Axons from the VPL neurons ascend
through internal capsule to synapse
in primary somatosensory cortex.
Somatosensory Projection to Cerebral Cortex: Trigeminal System
Trigeminal sensory
pathways in the brain are
similar to those for the rest
of the body.
• Somatosensory
information from the
trigeminal nerve goes to
the ventral posteromedial
nucleus (VPM) of the
thalamus.
Primary somatosensory
cortex (S1 cortex) for the
trigeminal system (face &
head) is also in the
postcentral gyrus of the
parietal lobe.
• As with the rest of the
body, trigeminal pain
information also projects
to limbic cortex ->
unhappiness & motivation
to avoid
The somatosensory projections to
primary sensory cortex (S1) have a
somatotopic organization throughout
their length
• Primary sensory cortex has a
representation of the body on it,
known as a homunculus (little
person).
Ventral Posteromedial Nucleus
Somatosensory information from the face and head (trigeminal
system) is relayed via the ventral posteromedial nucleus of
thalamus to primary somatosensory cortex.
Somatosensory System: crossed and uncrossed projections
- Somatosensory axons project ipsilaterally to the cerebellum.
--We'll find that a stroke in the right side of the cerebellum is
likely to affect motor control of the right side of the body.
- Somatosensory axons project contralaterally to the cerebral
cortex. --Thus a stroke in the right somatosensory cortex is
likely to affect sensory perception of the left side of the body.
Comparison between dorsal column and spinothalamic tract pathways
Pain
Defined as "an unpleasant sensory and emotional experience associated with actual or potential tissue damage
- Carried into CNS by thin primary afferent axons with slow conduction velocities (myelinated axons: <10 meters/sec / unmyelinated axons: <2 m/sec)
- Sensations are carried to the thalamus by spinothalamic tract neurons
Nociceptors
Nociceptors signal tissue damage or threat of tissue damage
- Mechanical injury (e.g., cutting, scraping, etc.)
- Heat injury (burning)
- Cold (frost-bite)
- Gut distension (e.g., gas pains)
- Chemical injury (e.g., acid)
- Free nerve endings
- Thresholds are usually higher than most other sensory receptors (light-touch receptor threshold: <1 g / painful touch threshold: ~70g)
Mechanical Nociceptors
- High threshold
- Increased force -> increased firing
- Small, point-like receptive fields
Polymodal Nociceptors
- Respond to mechanical, heat, and chemical stimuli
- Thermal thresholds 43-45 C
- High mechanical thresholds
- Respond to algesic agents, e.g., acid
Cold Nociceptors
- Thresholds ~0 C
- No overlap with cooling receptors
Anatomy of nociceptors
- Free nerve endings in superficial skin
- Terminals have transductin proteins sensitive to: heat, cold, acid, pressure, ATP
Sensitization of nociceptors
- Causes decreased threshold and larger response
- Contributes to increased pain after injury
Sensitizers
- Activity: heat, mechanical stimulation, chemical stimulation
- Inflammatory agents: prostaglandins, bradykinin, serotonin, cytokines
Types of pain
- Acute pain ("normal pain"): in response to injury or threat of injury, lasts as long as the stimulus, defines what's safe to explore
- Persistent pain: outlasts the injury/threat of. related to healing, protective during healing process
- Chronic pain: outlasts duration of healing
Inflammatory Pain
- Most common persistent pain (e.g., sunburn)
- Accompanies all injuries: skin, joints, muscle, bones, post-surgery
- Paradox: Inflammation promotes healing; inflammation causes more pain
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDS): blocks production of prostaglandins -> reduced inflammatory pain / effect on healing is uncertain