Traumatic Brain Injury (TBI)
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
Traumatic brain injury (TBI)
Damage to brain tissue caused by an external mechanical force. Results in loss of consciousness, posttraumatic amnesia (PTA), and skull fracture or objective neurological findings that can be attributed to the traumatic event by radiological findings, physical, or mental status examination.
Causes of TBI
1. Falls - major cause of TBI; most common in children and older adults.
2. Struck by or against something
3. Traffic incidents
4. Assault
5. Other
Symptoms of TBI
- Concussion characterized by post-traumatic loss of consciousness.
- Cerebral contusion/laceration/edema accompanied by surface wounds and skull fractures.
- A variety of symptoms can result: 1) Hemiplegia or monoplegia and abnormal reflexes, 2) decorticate or decerebrate rigidity, 3) fixed pupils, 4) coma, 5) changes in vital signs.
Types of brain injuries
Open head injury, closed head injury, and non-traumatic brain injury.
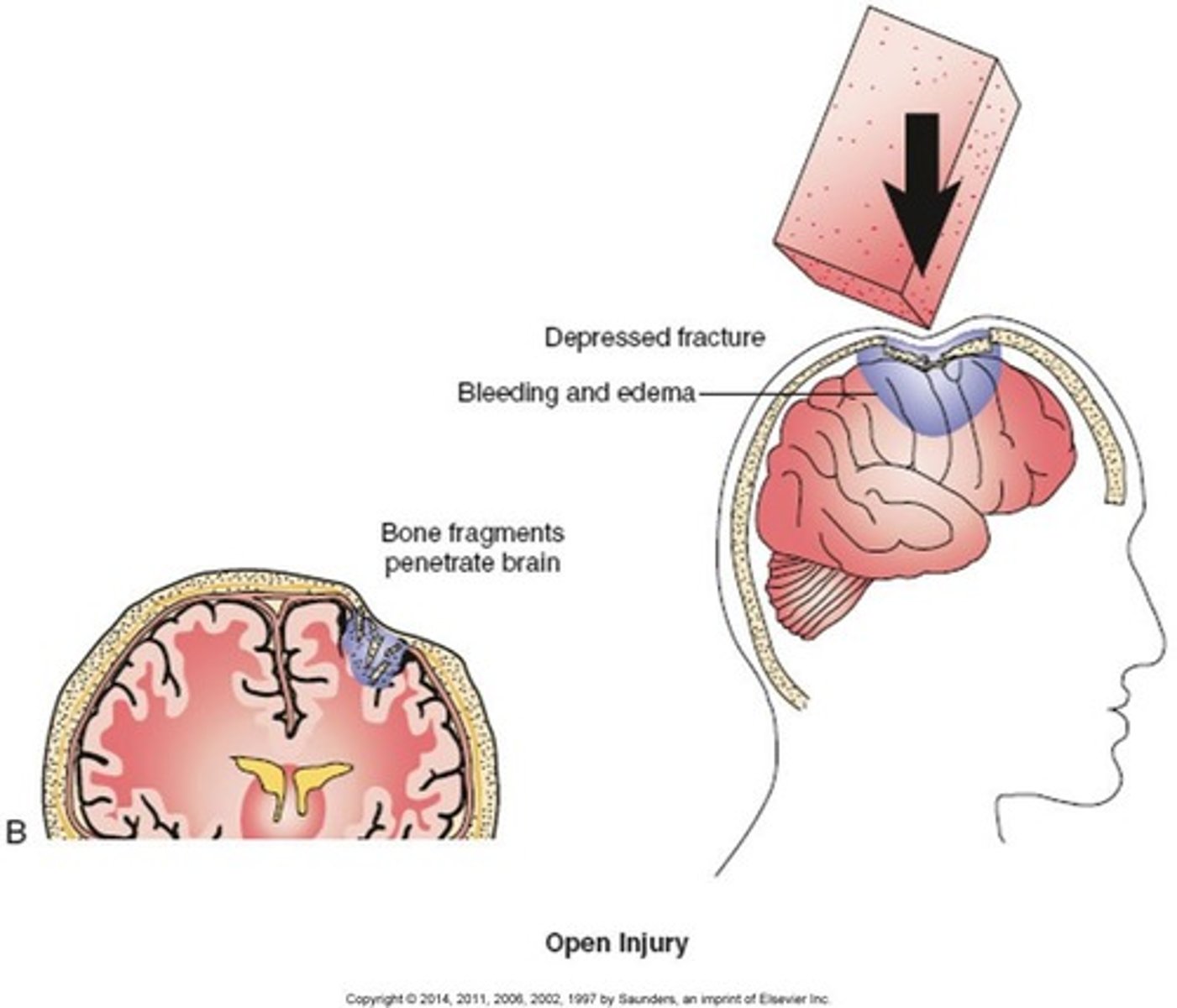
Open head injury
Injury to the brain caused by a foreign object entering the skull. Causes may include firearm injuries or being struck by a sharp object.
Also called focal brain injury.
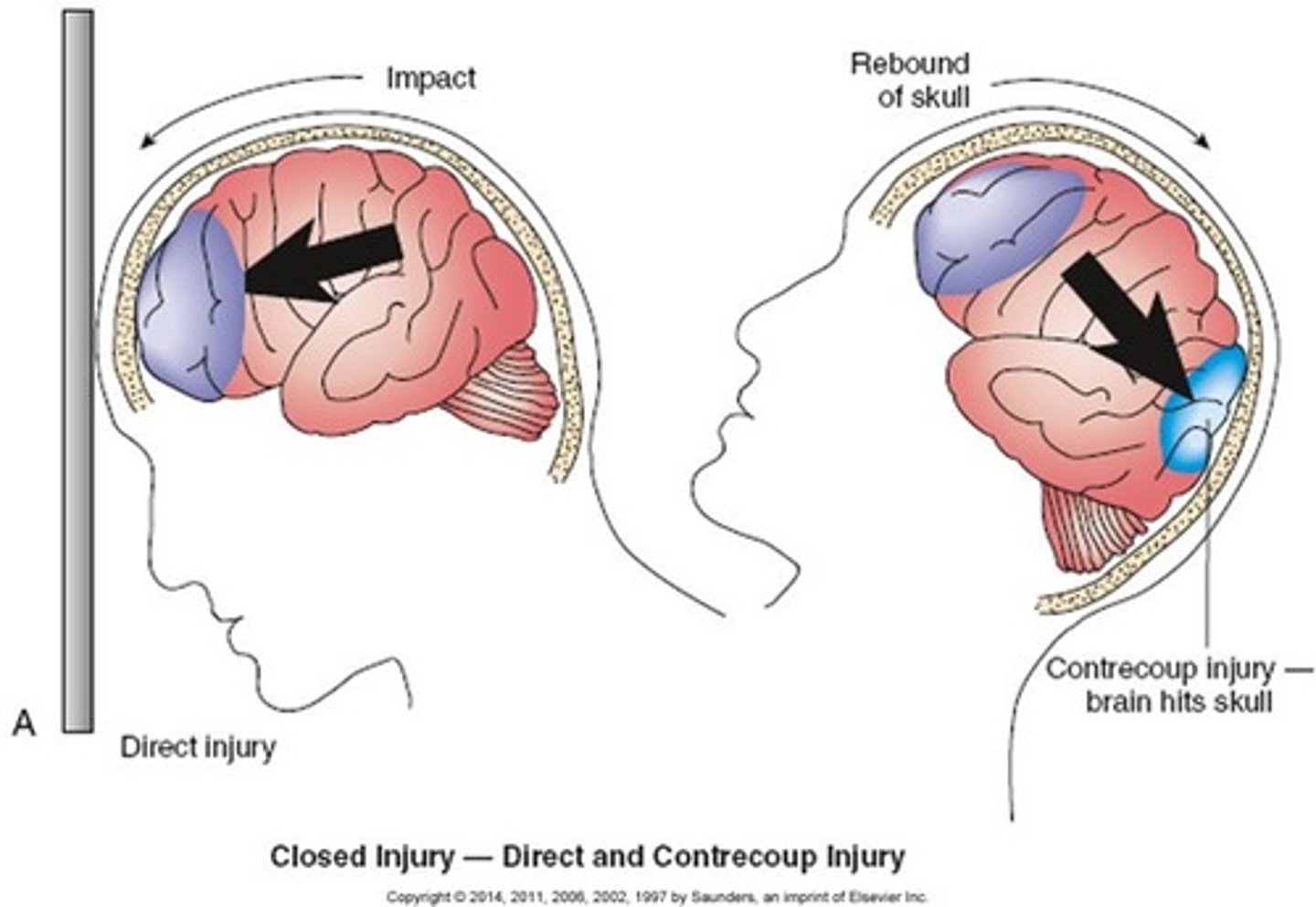
Closed head injury
Injury to the brain caused by movement of the brain within the skull. No penetration of the skull. Cause may include falls, motor vehicle crashes, and being struck by or with an object.
Also called multifocal and diffuse brain injury.
Non-traumatic brain injury
Situations where brain injury can occur without trauma. Includes drug overdose, chronic substance abuse, carbon monoxide, environmental exposure, and anoxia.
Clinical manifestations of TBI (signs and symptoms)
- Abnormal muscle tone and spasticity (decorticate and decerebrate rigidity).
- Primitive reflexes (impaired righting reflexes with midbrain damage; absence of equilibrium reactions and protective extension with basal ganglia damage).
- Muscle weakness.
- Decreased functional endurance.
- Ataxia (abnormal movement resulting from damage to the cerebellum).
- Postural deficits resulting in imbalance in muscle tone throughout the body.
- Limitations in joint motion.
- Changes in sensation (signs of absent or diminished sensation; possible hypersensitivity).
Medical management of TBI
- Resuscitation.
- Management of respiratory dysfunction.
- Cardiovascular monitoring.
- Surgical, pharmacologic, or mechanical means to decrease intracranial pressure.
- Neurosurgery to manage lacerated vessels and depressed skull fractures.
- Pharmacologic interventions - antibiotics, anticonvulsants, sedatives, antidepressants.
Clinical aspects and predictors of outcomes for TBI
Look at the patient immediately when they come in.
Look for:
- Autonomic functions (Visual signs - i.e., pulse, respiratory rate, temperature, blood pressure, diaphoresis.)
- Consciousness - i.e., level of arousal, cognition, length of coma.
- Motor functions - i.e., reflexes, voluntary movements, abnormal postures, decorticate/decerebrate posturing.
- Pupillary response - i.e., depth of coma-pathological signs of coma.
- Ocular movements (Cranial nerves - i.e., abnormalities in pupil size, shape, and light.)
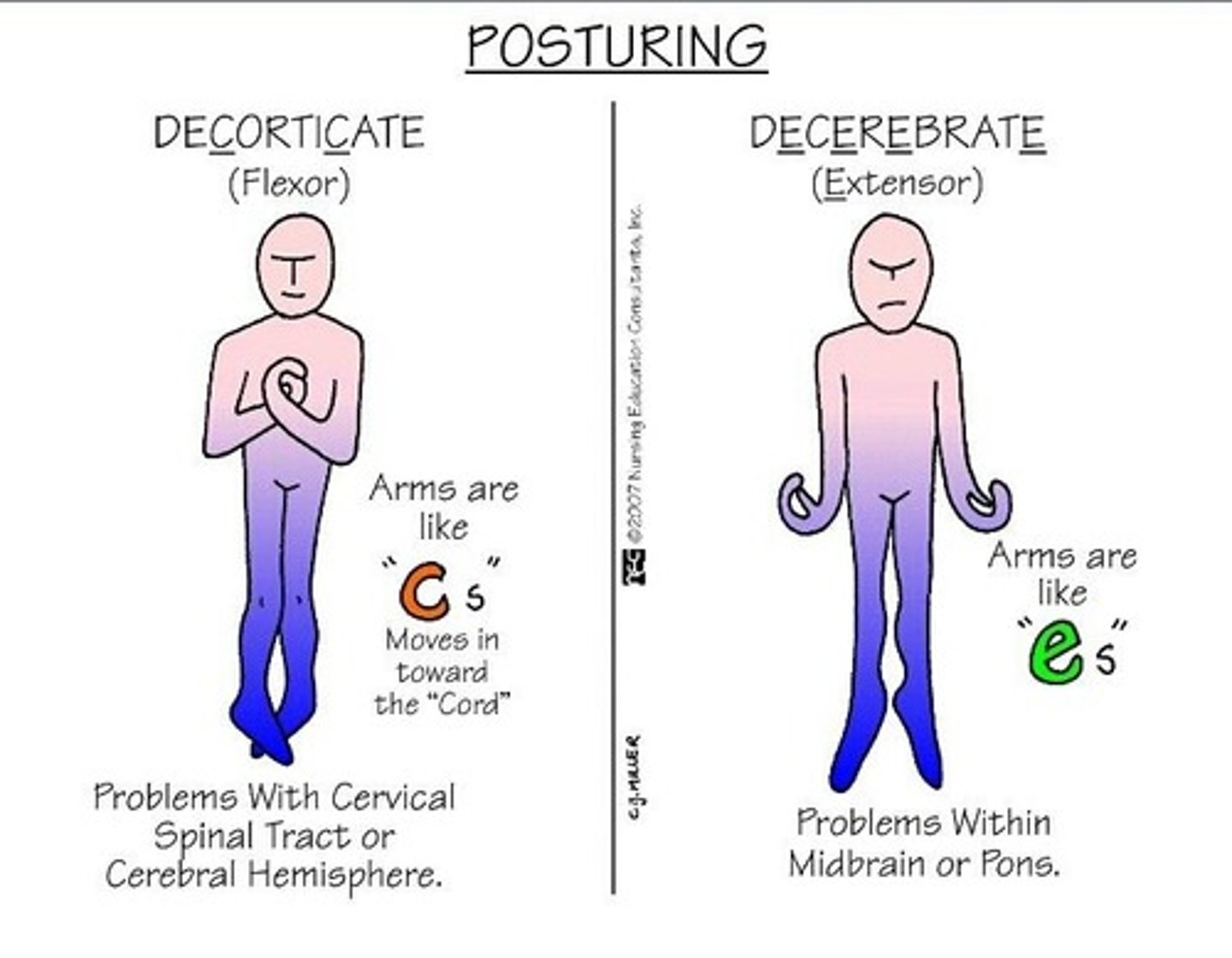
Decorticate posturing
One of the two types of rigidity or posturing that are indicative of where the brain injury has occurred.
UE in a spastic flexed position, internal rotation and adduction. LE spastic extended, internal rotation and adduction.
Lesion at cerebral hemisphere, internal capsule, above the superior colliculus.
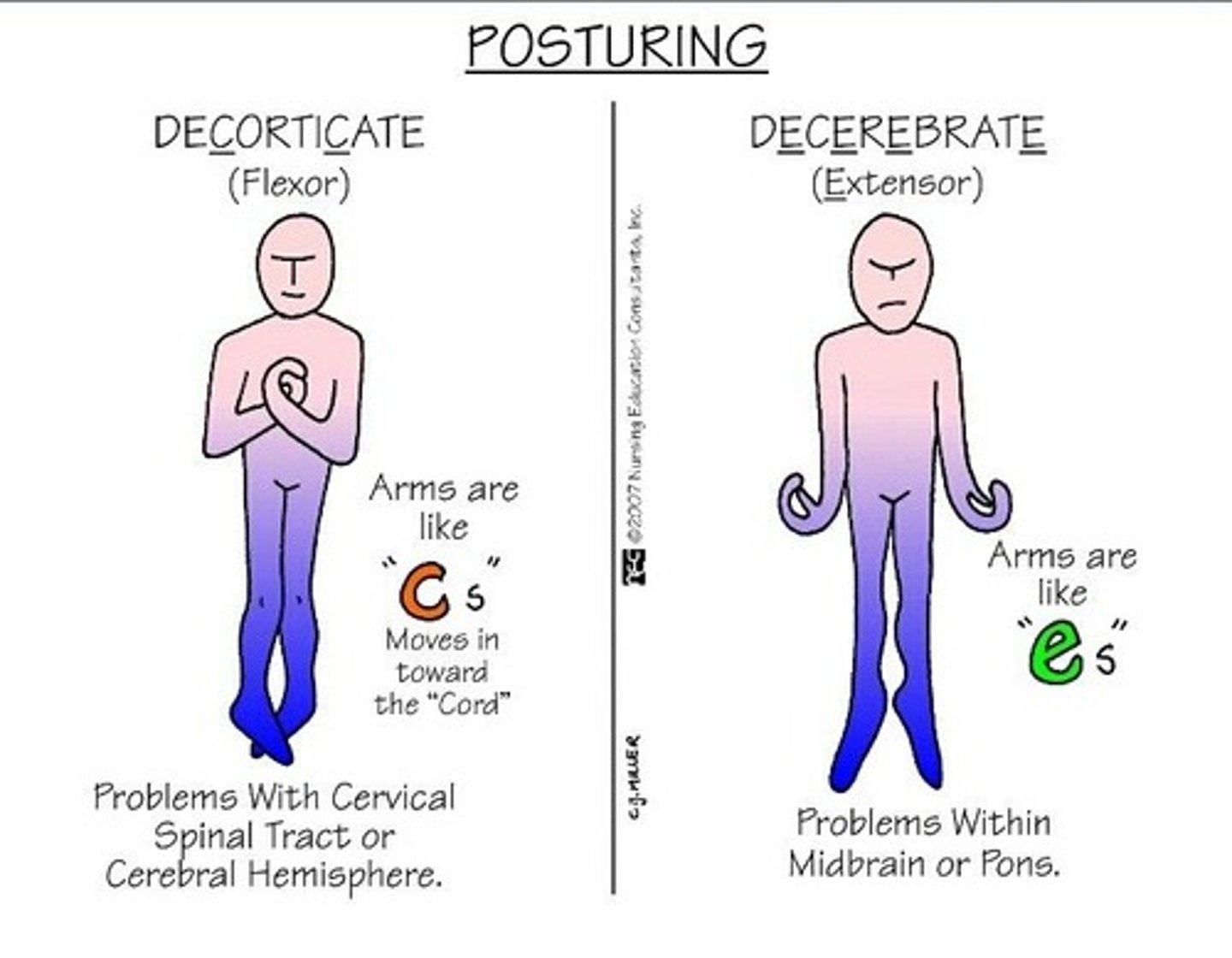
Decerebrate posturing
One of the two types of rigidity or posturing that are indicative of where the brain injury has occurred.
UE and LE in extension, adduction and internal rotation, wrist and fingers in flexion.
Lesion below the superior colliculus, brain stem region.
Poorer prognosis than clients with damage above the superior colliculus.
Retrograde amnesia
Length of amnesia for events prior to injury, unable to remember events due to neurological damage.
Anterograde amnesia
Length of amnesia following impact, injury, unable to consolidate information for storage and retrieval.
Post-traumatic amnesia
Following injury where the patient is confused and seems unable to store and recall new information (can refer to anterograde or retrograde subtype). Length of PTA is an indicator of the outcome or prognosis.
Length of post-traumatic amnesia (PTA) - the time after injury when day-to-day recall returns and full orientation is present.
- Mild: <1 hour
- Moderate: 1-24 hours
- Severe: 1-7 days
- Very severe: 1-4 weeks
- Extremely severe: >4 weeks
Predictors of prognosis for TBI
Age
Lifestyle
Social support system
Premorbid drug and alcohol use
Length of time of coma and/or PTA
OT intervention for TBI
Acute phase
- Effective w/c positioning (prevent skin breakdown and muscle deformity; increase sitting tolerance, respiration, and swallowing ability).
- Proper bed positioning (prevent skin breakdown, facilitate normal muscle tone).
- PROM.
- Splinting and casting UE (indicated for spasticity, ROM deficiencies, and contractures; includes cone or "carrot" splint, resting or functional position splint, anti-spasticity splint, elbow cast).
- Management of agitation (behavioral management strategies).
- Family/caregiver education (sensory regulation, positioning, ROM).
- Neuromuscular re-education.
Inpatient rehabilitation phase
- Optimize motor function through occupation-based activities. Teaching compensatory strategies.
- Optimize visual abilities, visual-perceptual functions, cognitive function, and voice and speech function through compensatory and rehabilitation strategies, environmental adaptations.
- Restore competence in self-maintenance tasks.
- Behavioral and emotional adaptations.
- Supported family caregivers.
Post-acute rehabilitation phase
- Optimize cognitive function, visual and visual-perceptual function.
- Leisure and social participation engagement.
- Work exploration and participation.
- Behavioral and emotional adaptation.
OT evaluation for TBI
- Occupational profile and reviewing medical records. Information may need to be gathered from family members, depending on the client's level of consciousness.
- May include standardized or non standardized assessment of areas of occupation, performance skills, and client factors.
- Assess context for cultural, personal, temporal, and virtual demands.
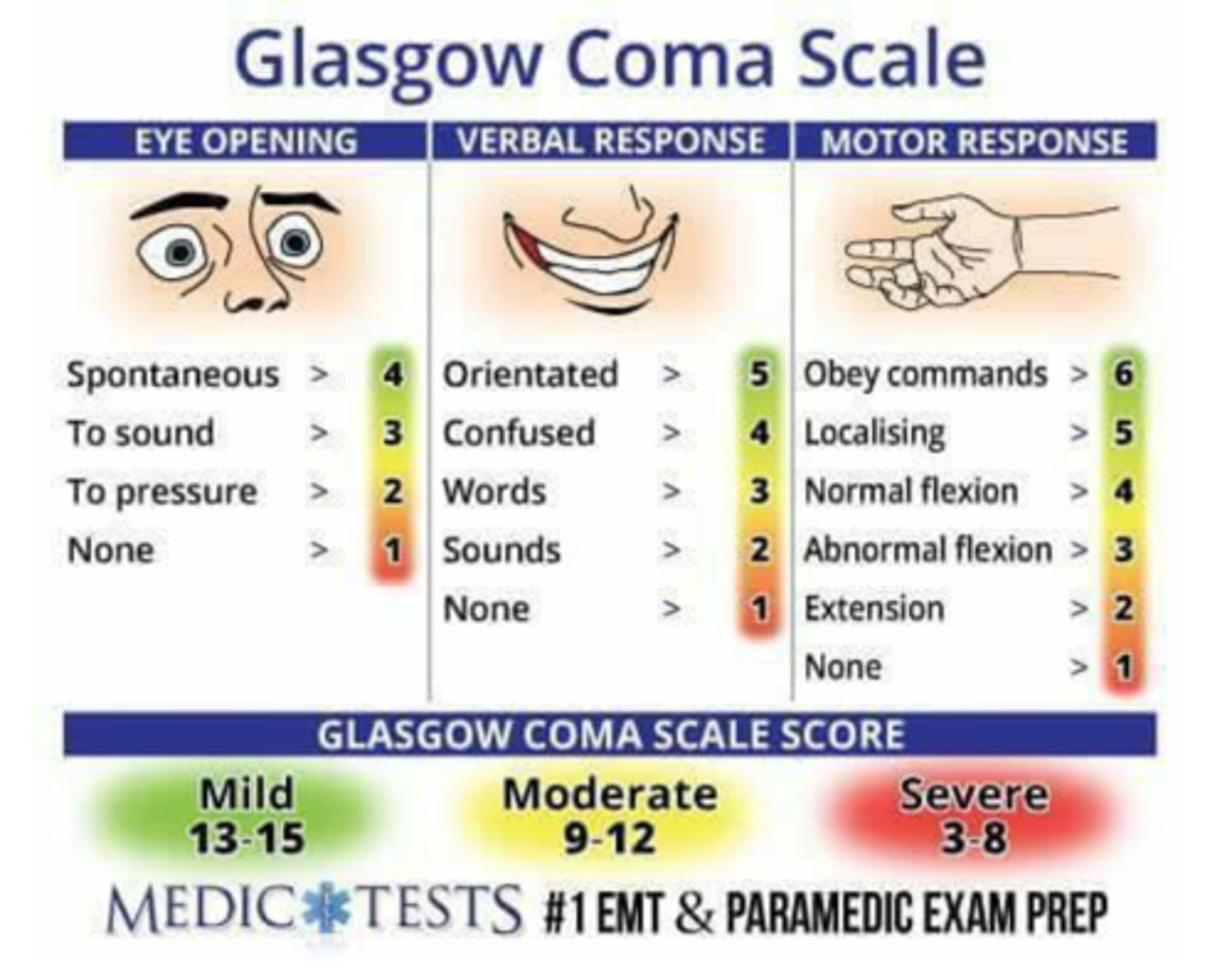
Glasgow Coma Scale (GCS)
A neurological scale which provides an objective method to record the conscious state of a person (assesses severity of coma and impaired consciousness). It is used for initial evaluation and continuing assessment to determine a person's level of consciousness after head injury.
A client is assessed against the scale's criteria which delineate a range of points for three tests: eye, verbal, and motor responses. The resulting total points comprise the Glasgow Coma Score (or GCS). The score sum as well as the three separate values are considered.
Scoring:
The highest total GCS is 15 (i.e., a fully conscious person).
The lowest possible total GCS is 3 (i.e., deep coma or death).
<8 = Severe TBI.
9-12 = Moderate TBI.
> 13 = Mild TBI.
Three aspects of coma are independently observed: 1) eye-opening (E), 2) best motor response (M), and 3) verbal performance (v). An overall coma score is obtained by adding up the total numbers (E+M+V).
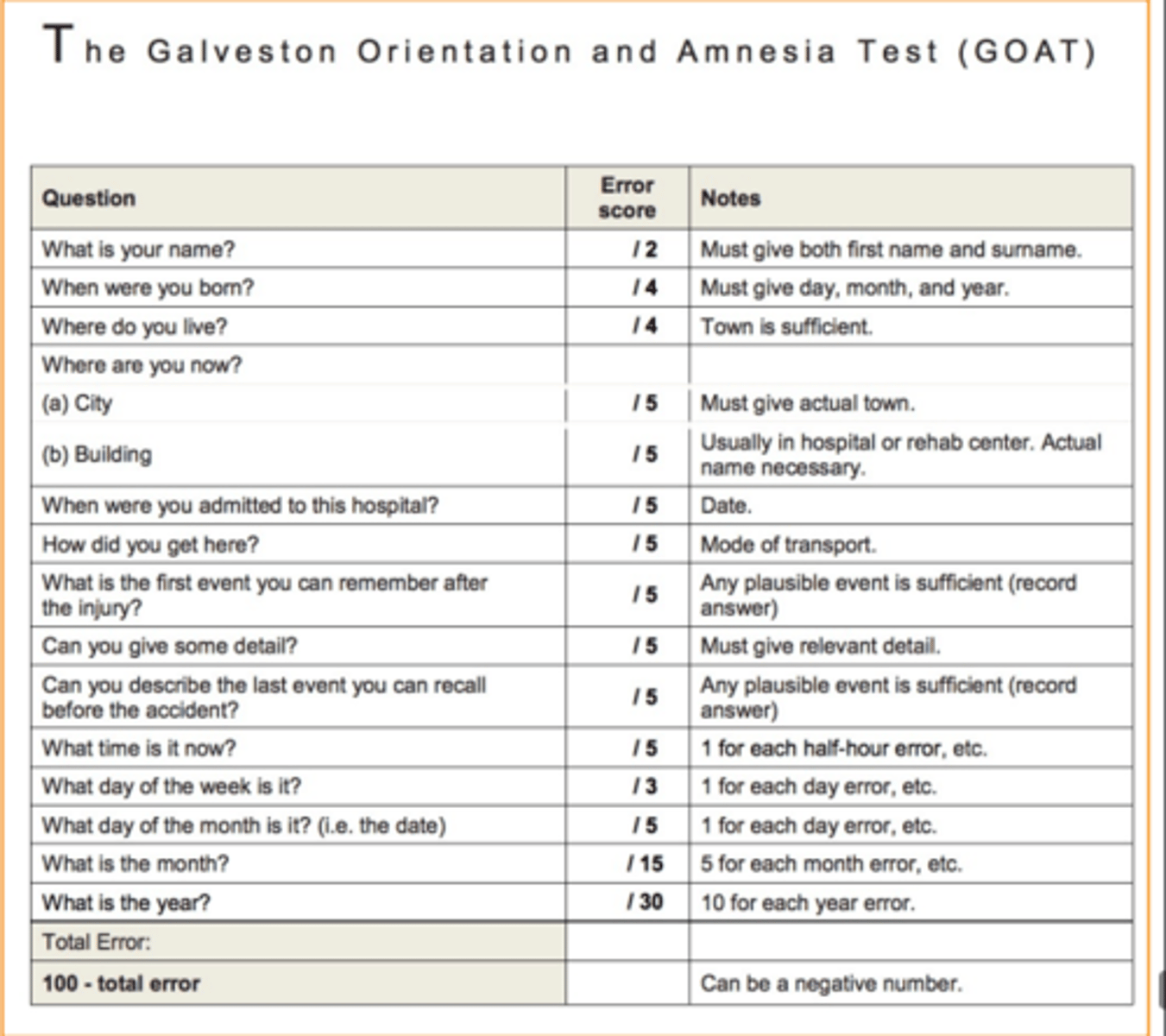
Galveston Orientation and Amnesia Test (GOAT)
Measures cognitive level of patients post-injury so that a more realistic recovery plan can be communicated. Including LOS, rehab therapy plan, and prediction of recovery information for patient’s family.
A low GOAT score usually indicates a longer duration of the post-traumatic amnesic period. An increased duration of the PTA was found in patients with diffuse or bilateral brain injuries. The longer the confused state, the more difficult for the patient to return to pre-injury cognitive levels.
Rancho Los Amigos (RLA) Scale of Cognitive Functioning
Rehab evaluation tool that rates how patients with TBI are recovering. Focuses on client’s abilities and behaviors. Clients move through the stages during the recovery process.
RLA scale:
RLA I (no response/total assist)
RLA II (generalized response/total assist)
RLA III (localized response/total assist)
RLA IV (confused, agitated/max assist)
RLA V (confused, inappropriate, non-agitated/max assist)
RLA VI (confused, appropriate/mod assist)
RLA VII (automatic, appropriate/min assist)
RLA VIII (purposeful, appropriate/stand-by assist)
RLA IX (purposeful, appropriate/stand-by assist on request)
RLA X (purposeful, appropriate/modified independent)
Considerations: Anyone with a TBI can enter this scale at any point; Can start at any level and go through the process of improving and can stop at any process; Rare occasions where clients go through the stages and skip a stage.
RLA I
No response, total assistance.
Coma.
Complete absence of observable change in behavior when presented visual, auditory, tactile, proprioceptive, vestibular, or painful stimuli.
Absence of awareness of self and the environment despite maximum stimuli. No periods of wakefulness in the coma state. When sedating and hypnotic medications are removed, coma rarely lasts more than weeks. Coma rarely lasts >3-4 weeks unless medication induced.
RLA II
Generalized response, total assistance.
Persistent vegetative state (PVS). No awareness of self or environment - cannot attend, follow commands; no intelligible verbal response/communication; no automatic motor response or localizing; incontinence bowel and bladder. Positive signs include sleep/wake cycles, brain stem/autonomic functions (i.e., gag, swallow, cough, temperature regulation), and random vocalizations/movements.
- Demonstrates generalized reflex response to painful stimuli.
- Responds to repeated auditory stimuli with increased or decreased activity.
- Responds to external stimuli with physiological changes generalized, gross body movement, and/or not purposeful vocalization.
- Responds noted above may be same regardless of type and location of stimulation. Responses may be significantly delayed.
RLA III
Localized response, total assistance.
Minimally conscious state. Some awareness with wakefulness. Definite reproductible behavior evidence of some awareness of self or environment.
- Demonstrates withdrawal or vocalization to painful stimuli.
- Turns toward or away from auditory stimuli.
- Blinks when strong light crosses visual field.
- Follows moving object passed within visual field. (Visual tracking.)
- Responds to discomfort by pulling tubes or restraints.
- Responds inconsistently to simple commands.
- Responses directly related to type of stimulus.
- May respond to some persons (especially family and friends) but not to others.
RLA IV
Confused, agitated. Max assistance.
- Alert and in heighted state of activity.
- Purposeful attempts to remove restraints or tubes or crawl out of bed.
- May perform motor activities such as sitting, reaching, and walking but without any apparent purpose or upon another's request.
- Very brief and usually non-purposeful moments of sustained alternatives and divided attention.
- Absent short-term memory.
- May cry out or scream out of proportion to stimulus even after its removal.
- Mood may swing from euphoric to hostile with no apparent relationship to environmental events.
- Unable to cooperate with treatment efforts.
- Verbalizations are frequently incoherent and/or inappropriate to activity or environment.
RLA V
Confused, inappropriate, non-agitated. Max assistance.
- Alert, not agitated but may wander randomly or with a vague intention of going home.
- May become agitated in response to external stimulation and/or lack of environmental structure.
- Not oriented to person, place, or time.
- Frequent brief periods, non-purposeful sustained attention.
- Severely impaired recent memory, with confusion of past and present in reaction to ongoing activity.
- Absent goal-directed, problem solving, self-monitoring behavior.
- Often demonstrates inappropriate use of objects without external direction.
- May be able to perform previously learned tasks when structured and cues provided.
- Unable to learn new information.
- Able to respond appropriately to simple commands fairly consistently with external structures and cues. Responses to simple commands without external structure are random and non-purposeful in relation to command.
- Able to converse on a social, automatic level for brief periods of time when provided external structure and cues.
- Verbalizations about present events become inappropriate and confabulatory when external structure and cues are not provided.
RLA VI
Confused, appropriate. Moderate assistance.
- Inconsistently oriented to person, place, and time.
- Able to attend to highly familiar tasks in non-distracting environment for 30 minutes with moderate redirection.
- Remote memory has more depth and detail than recent memory.
- Vague recognition of some staff.
- Able to use assistive memory aide with maximum assistance.
- Emerging awareness of appropriate response to self, family, and basic needs.
- Moderate assist to problem solve barriers to task completion.
- Supervised for old learning (e.g., self-care).
- Shows carryover for relearned familiar tasks (e.g., self-care).
- Maximum assistance for new learning with little or no carryover.
- Unaware of impairments, disabilities, and safety risks.
- Consistently follows simple directions.
- Verbal expressions are appropriate in highly familiar and structured situations.
RLA VII
Automatic, appropriate. Minimum assistance.
- Consistently oriented to person and place, with highly familiar environments. Moderate assistance for orientation to time.
- Able to attend to highly familiar tasks in a non-distracting environment for at least 30 minutes with minimal assist to complete tasks.
- Minimal supervision for new learning. Demonstrates carryover of new learning.
- Initiates and carries out steps to complete familiar personal and household routine but has shallow recall of what they have been doing.
- Able to monitor accuracy and completeness of each step in routine personal and household ADL and modify plan with minimal assistance.
- Superficial awareness of their condition but unaware of specific impairments and disabilities and the limits they place on their ability to safely, accurately, and completely carry out their household, community, work, and leisure ADL.
- Minimal supervision for safety in routine home and community activities.
- Unrealistic planning for the future.
- Unable to think about consequences of a decision or action.
- Overestimates abilities.
- Unaware of others' needs and feelings.
- Oppositional/uncooperative.
- Unable to recognize inappropriate social interaction behavior.
RLA VIII
Purposeful, appropriate. Stand-by assistance.
- Consistently oriented to person, place, and time.
- Independently attends to and completes familiar tasks for 1 hour in distracting environments.
- Able to recall and integrate past and recent events.
- Uses assistive memory devices to recall daily schedule, recall "to do" lists, and record critical information for later use with SBA.
- Initiates and carries out steps to complete familiar personal, household, community, work, and leisure routines with SBA and can modify the plan when needed with minimal assistance.
- Requires no assistance once new tasks/activities are learned.
- Aware of and acknowledges impairments and disabilities when they interfere with task completion but requires SBA to take appropriate corrective action.
- Thinks about consequences of a decision or action with minimal assistance.
- Overestimates or underestimates abilities.
- Acknowledges others' needs and feelings and responds appropriately with minimal assistance.
- Depressed, irritable. Low frustration tolerance, easily angered. Argumentative, self-centered.
- Uncharacteristically dependent/independent.
- Able to recognize and acknowledge inappropriate social interaction behavior while it is occurring and takes corrective action with minimal assistance.
RLA IX
Purposeful, appropriate. SBA on request.
- Independently shifts back and forth between tasks and completes them accurately for at least 2 consecutive hours.
- Uses assistive memory devices to recall daily schedule, "to do" lists, and record critical information for later use with assistance when requested.
- Initiates and carries out steps to complete familiar personal, household, work, and leisure tasks independently and unfamiliar personal, household, work, and leisure tasks with assistance when requested.
- Aware of and acknowledges impairments and disabilities when they interfere with task completion and takes appropriate correction action but requires SBA to anticipate a problem before it occurs and take action to avoid it.
- Able to think about consequences of decisions or actions with assistance when requested.
- Accurately estimates abilities but requires SBA to adjust to task demands.
- Acknowledges others' needs and feelings and responds appropriately with SBA.
- Depression may continue. May be easily irritable. May have low frustration tolerance.
- Able to self-monitor appropriateness of social interaction with SBA.
RLA X
Purposeful, appropriate. Modified independent.
- Able to handle multiple tasks simultaneously in all environments but may require periodic breaks.
- Able to independently procure, create, and maintain own assistive memory devices.
- Independently initiates and carries out steps to complete familiar and unfamiliar personal, household, community, work, and leisure tasks but may require more than usual amount of time and/or compensatory strategies to complete them.
- Anticipates impact of impairments and disabilities on ability to complete daily living tasks and takes action to avoid problems before they occur but may require more than usual amount of time and/or compensatory strategies.
- Able to independently think about consequences of decisions or actions but may require more than usual amount of time and/or compensatory strategies to select the appropriate decision or action.
- Accurately estimates abilities and independently adjusts to task demands.
- Able to recognize the needs and feelings of others and automatically respond in appropriate manner.
- Periodic periods of depression may occur. Irritability and low frustration tolerance when sick, fatigued, and/or under emotional stress.
- Social interaction behavior is consistently appropriate.
Musculoskeletal problems of RLA I-III
Many musculoskeletal problems that can arise from RLA I-III, including fractures and heterotopic ossification (abnormal bone growth in soft tissue).
Goals for addressing musculoskeletal problems:
- Allow sitting, standing, and positioning
- Allow for functioning and participation in daily activities (ADLs, etc.).
W/c positioning for RLA I-III
- Prevent deformity.
- Tone normalization.
- Pressure management.
- Promote function.
- Increase sitting tolerance.
- Enhance respiratory function.
- Provide proper body mechanics.
- Dynamic head positioning device for w/c, which allows for alignment and freedom of movement and the promotion of function.
Spasticity management for RLA I-III
Goal is to normalize tone with minimal daytime sedation.
- Position in bed, chair.
- Sitting/standing opportunities - two person treatment.
- Neuromuscular blocks plus casting: Phenol - motor points for large muscles, musculocutaneous nerve (biceps), obturator nerve (thigh adductors); Bupivacaine - any nerve, allows immediate casting in a relaxed position; Botulinum toxin - every 3 months, small to medium sized muscles.
Systemic medications to address spasticity includes: dantrolene, baclofen, intrathecal baclofen pump after 4-6 months.
Positioning and casting consume the most time and resources - early tx makes a difference by reducing the need.
Casting for spasticity management
We choose to cast when splinting has failed to control severe tone or contractures from developing.
Positional cast is necessary for continued use (bivalve) - divided into two so you can take out the cast and clean it for maintenance. ROM is decreased and prolonged stretches necessary.
Consequences of lack of intervention for RLA I-III
- Contractures.
- Limited head and trunk control.
- Increased caregiver assistance.
- Limited participation in daily occupations, limited mobility.
- Transportation difficulties.
Behavioral management program for RLA IV
Goals of behavior management program:
- To provide an environment that motivates patients to participate in a comprehensive rehab program at their optimal capacity.
- To integrate family members into the rehab team and tx plan development process.
- To maintain a safe environment through a multifaceted safety program.
- Aggressive and impulsivity expressed.
- To minimize the use of all restrictive modalities.
- To provide education to patients, family, and staff.
- To identify patients with substance abuse disorders and initiate specialized tx.
Sample interventions: Environmental modifications (e.g., reducing noise level, provide consistency and structure) and communication/interaction (e.g., model behaviors for patient; provide choices; give praise and attention for desired behaviors).