Bone Marrow/Hemic Neoplasia
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
100 Terms
What are differential diagnoses for aplastic pancytopenias?
- Toxin/drug (chemotherapy, some antibiotics, phenylbutazone, griseofulvin, bracken fern in cattle)
- Infection (Parvoviruses, FeLV, E. canis)
- Myelophthisis (neoplastic vs. non-neoplastic (e.g., myelofibrosis))
What are common causes of secondary myelodysplasias in dogs?
- IMHA, IMTP, lymphoma, chemotherapy
What are primary myelodysplasias? What is their prognosis?
- Myelodysplastic syndromes (MDS) are clonal disorders which are basically neoplastic diseases so the prognosis is generally poor
What is a clinical feature of all forms of MDS?
- Non-regenerative anemia
What are the categories of hemic neoplasia?
- Lymphoma
- Leukemia (lymphoid vs. myeloid)
- Histiocytic
- Mast cell
- Plasma cell
- Transmissible venereal tumor (dogs only)
What is the most common types of leukemia in most species?
- Chronic lymphocytic leukemia
What are the two primary differential diagnoses for a small animal patient with marked neutrophilia?
- Severe inflammation
- Paraneoplastic response
What are the primary differences between acute and chronic leukemias?
- Acute leukemias have more immature ("blast-like") cells are more aggressive clinical disease than chronic leukemias
How are different types of leukemias differentiated?
- Almost always requires immunophenotyping
Lymphocytic "leukemia" can arise not only in the bone marrow, but also in the ____________. Which type of leukemia arises here?
- Spleen
- Leukemia of granular lymphocytes in dogs (common form of canine CLL)
How is FeLV associated with lymphoma?
- FeLV+ cats have a high risk of mediastinal lymphoma (especially in younger cats)
How is the leukemic phase of lymphoma different from acute lymphoblastic leukemia (ALL)?
- Both cause large immature lymphocytes in circulation but lymphoma originates in the lymphoid tissues, not the bone marrow, the prognosis for lymphoma is usually much better than that for ALL, and the neoplastic cell count is generally under 75000 per microliter in lymphoma but can be up to 100,000 to 300,000 per microliter in leukemia.
How is the leukemic phase of lymphoma different from chronic lymphocytic leukemia?
- The cells are larger with immature nuclear features while CLL cells are smaller lymphocytes with mature nuclei
What are some types of indolent lymphoma in dogs?
- Follicular (B cell) lymphoma of the spleen/LN
- T-zone lymphoma/leukemia
What are some types of indolent lymphoma in cats?
- Small-cell (aka low grade) lymphoma of the intestinal tract -> Common
How is lymphoma categorized in horses? Indicate which is most common.
- Multicentric - Most common (widespread lymph node involvement)
- Generalized
- Alimentary
- Splenic
- Mediastinal
- Thymic
- Cutaneous
What are the three possible outcomes of BLV infection in cattle?
1) Asymptomatic infection (~2/3 of cattle)
2) Persistent lymphocytosis (~1/3 cattle; >7,500 per microliter)
3) Lymphoma (~5% cattle)
What are common signs of lymphoma secondary to BLV infection in cattle?
- Peripheral and/or internal lymphadenopathy, dyspnea, bloat, fever, jugular vein distention, tachycardia, brisket edema, weight loss
- Rarely cause uterine tumors (Specific if present)
Cutaneous plasmacytoma make up ___________ of all canine skin tumors. They are rare in other species and generally ___________ in all species.
- 1.5%
- Benign
Non-cutaneous plasmacytomas are ________% of all canine oral tumors and are generally ______________. They are can also occur in the _________________ and are again often ____________.
- 5
- Benign
- Rectum/anus
- Benign
What are diagnostic criteria for multiple myeloma?
- At least 2 of the 4:
1) >20% plasma cells in bone marrow
2) Monoclonal gammopathy
3) Multifocal osteolytic lesions or osteopenia
4) Light chain (Bence-Jones) proteinuria
What are some clinicopathologic abnormalities in multiple myeloma?
- Hypercalcemia (osteolysis, hypercalcemia of malignancy)
- Cytopenias: Normal blood cells crowded out by plasma cells in bone marrow
What are the types of histiocytic disorders in dogs and their cellular origin?
- Cutaneous histiocytoma (Langerhans cell)
- Cutaneous histiocytosis (Langerhans cells)
- Reactive histiocytosis (Dendritic cells)
- Histiocytic sarcoma (Dendritic cells or macrophages)
What are the two types of reactive histiocytosis? Which is common in Bernes Mountain Dogs?
- Cutaneous
- Systemic (Bernes Mountain Dogs)
What breeds are predisposed to histiocytic sarcoma?
- Bernese Mountain Dogs
- Rottweilers
- Golden Retrievers
- Flat-coat retrievers
Which type of histiocytic sarcoma is more common?
- Histiocytic sarcoma of dendritic cell origin
Where does histiocytic sarcoma (of dendritic cell origin) commonly occur (nodular/mass formation)? It makes up ~50% of _____________ tumors in dogs.
- Spleen, lymph node, lung, skin, around joints, DNS, bone marrow
- Synovial
Where does histiocytic sarcoma (of macrophage origin) originate? Describe its distribution in these organs.
- Spleen or bone marrow
- Diffuse in that organ, can spread
What is the "hemophagocytic" form/syndrome of histiocytic sarcoma (macrophage origin)?
- RBCs and platelets are destroyed leading to hemolytic anemia and/or thrombocytopenia
What is the most common malignant skin tumor of dogs?
- Mast cell neoplasia
Where do mast cell tumors arise in dogs?
- Cutaneously, subcutis, visceral organs, mucocutaneous tissues
How common are mast cell tumors in cats? Are they typically benign or malignant?
- Second most common skin cancer (majority are benign but 20-25% will metastasize to lymph nodes and/or viscera)
- Most common neoplasm of spleen (splenectomy usually curative but can spread to other sites, especially liver and lymph nodes)
- Intestinal mast cell tumors can occur
How common is mast cell neoplasia in ferrets?
- ~45% of all skin or subcutaneous tumors
What signs/lesions are associated with TVT?
- Hemorrhage and/or secondary infection (especially UTI) is common
Describe the typical progression of TVT.
- 4-6 months of progression, then most but not all tumors spontaneously regress
- Metastasis is rare (<5%) but can go to lymph nodes and internal organs
TVT cells are of what origin? What is particular about them?
- Myeloid (possibly macrophage)
- Different chromosome number than normal dog cells (59 rather than 78); High mitotic rate is common
Describe the typical biologic behavior of amelanocytic melanoma.
- Often metastasizes to draining lymph node(s); Difficult to distinguish from other round cell neoplasia
What are some indications for bone marrow sampling?
- Persistent cytopenias (including non-regenerative and poorly regenerative anemia)
- Suspicion of hematopoietic neoplasia
- Suspicion of infectious or neoplastic marrow disease
- Fever of unknown origin
- Persistent hypercalcemia (dogs)
- Persistent hyperglobulinemia (especially if monoclonal)
What are some reasons one may suspect hematopoietic neoplasia?
- Unexplained leukocytosis (especially lymphocytosis)
- Abnormal cells in circulation
- Staging of lymphoma
What are the two primary infectious diseases that involve the bone marrow?
- Ehrlichia canis
- Leishmaniasis
What are the two types of bone marrow samples?
- Biopsy for histology
- Aspiration for cytology
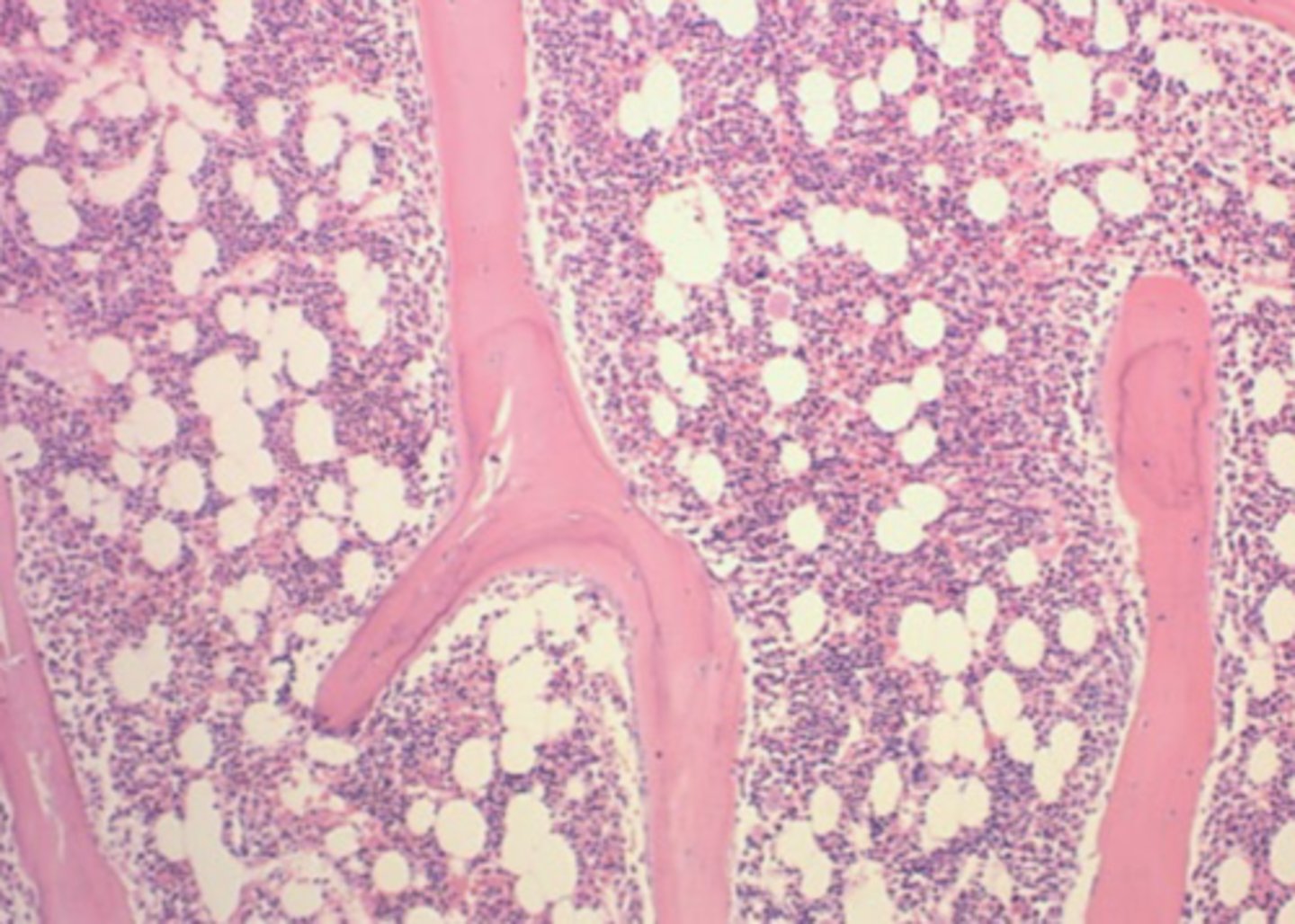
How are biopsies for histology processed?
- Processes like all biopsies: Embedded in paraffin, sectioned, stained with hematoxylin/eosin
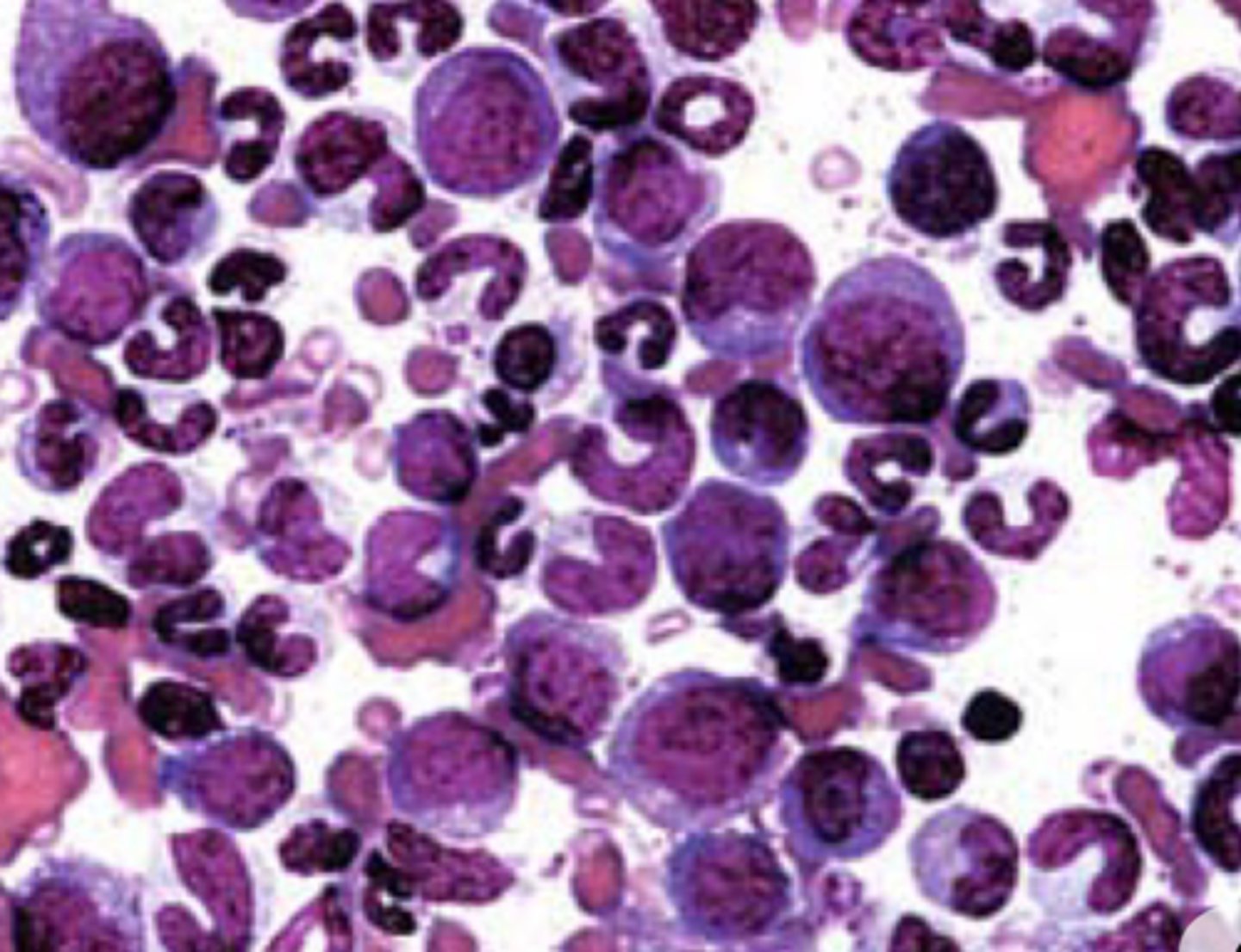
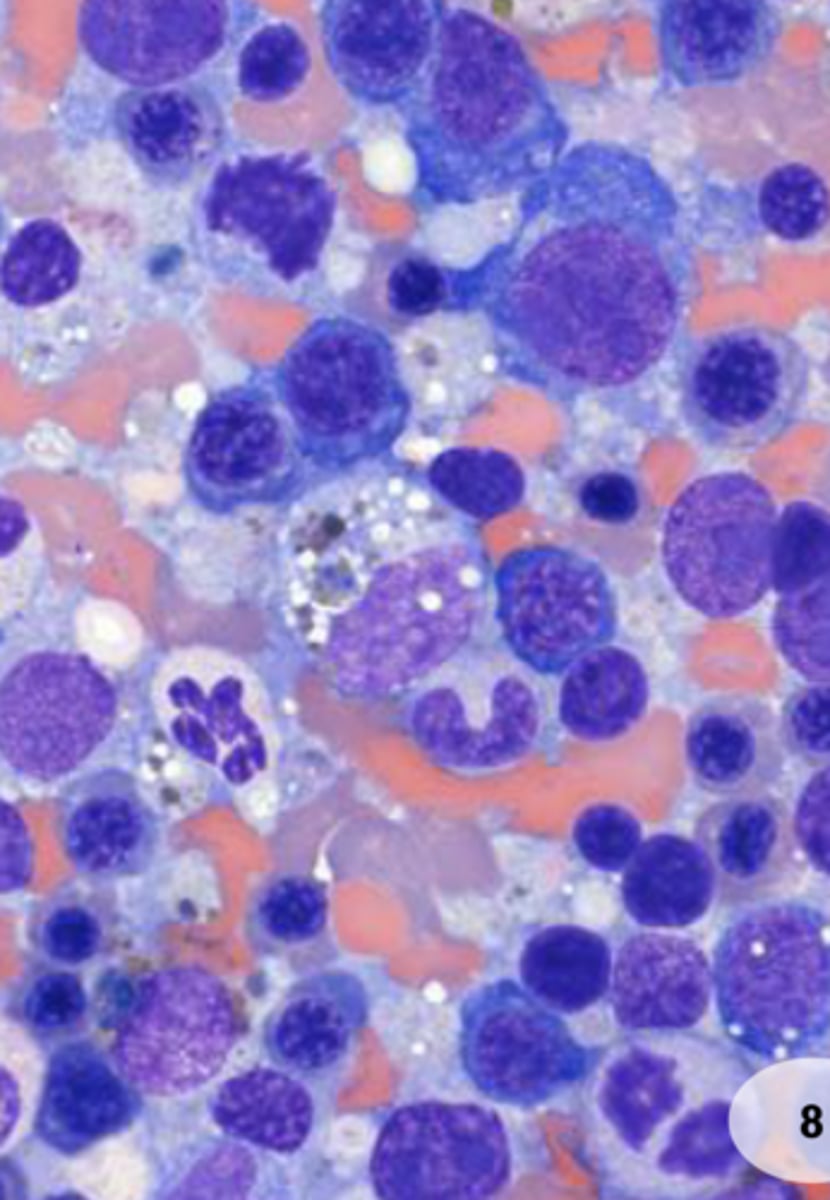
How are aspirations for cytology processed?
- Smears are prepared and stained with Wright's stain like blood/cytology smears
What sort of information does a bone biopsy provide?
- "big picture" and architecture: degree of cellularity, fibrosis, necrosis, large pockets of neoplastic cells
What sort of information does a bone cytology provide? What is the limitation of cytology?
- Individual cell detail, maturation, dysplastic and neoplastic changes to cells
- Limited in that the sample must be representative (e.g. not just peripheral blood)
In what ways do bone marrow biopsies and cytologies complement each other?
- If one sample is poor, the other can still provide info.
- The types of information they provide are different and useful in varying ways
What are the categories of marrow disease?
- Hypoplasia/aplasia
- Dysplasia
- Hyperplasia (appropriate vs. inappropriate)
- Degeneration or necrosis
- Myelofibrosis
What additional diagnostic test is required (within 48 hours) in order to properly interpret a bone marrow sample?
- CBC
For postmortem collection, bone marrow must be the first sample collected. Why?
- It autolyzes within an hour as it is a hypoxic environment
What questions are considered an a bone marrow sample interpretation?
- Is the marrow responding appropriately given the CBC data?
- Are any cells abnormal (dysplastic, neoplastic, etc.)?
- Is abnormal tissue (e.g. fibrosis) or necrosis present?
If an 11 year old patient with non-regenerative, normocytic, normochromic anemia presented and the bone marrow interpretation was erythroid hyperplasia with "maturation arrest" at metarubricyte stage, what would be your clinical diagnosis?
- Precursor Immune-Mediated Anemia (PIMA)
What is the "level of immune attack" for each of the following immune-mediated hematologic diseases?
A. IMHA
B. PIMA
C. Pure red cell aplasia (PRCA)
D. IMN
E. IMTP/ITP
F. Aplastic pancytopenia
A. Mature RBCs
B. Any immature erythroid stage
C. Earliest erythroid precursor
D. Segmented +/- band neutrophils
E. Platelets +/- mekakaryocytes
F. Early hematopoietic precursors
What are the CBC/bone marrow findings for each of the following immune-mediated hematologic diseases?
A. IMHA
B. PIMA
C. Pure red cell aplasia (PRCA)
D. IMN
E. IMTP/ITP
F. Aplastic pancytopenia
A. Regenerative anemia with erythroid hyperplasia
B. Non-regenerative anemia with "maturation arrest" at a specific erythroid stage
C. Non-regenerative anemia; Absence of erythroid cells in bone marrow
D. Neutropenia +/- left shift; myeloid hyperplasia
E. Thrombocytopenia; megakaryocyte hyperplasia
F. Pancytopenia; Hypocellular bone marrow (all blood cel types absent)
Aplastic pancytopenias are caused by what types of syndromes?
- Bone marrow failure syndromes
What blood cell types is unaffected by aplastic pancytopenia?
- Lymphocytes
What is the mechanism by which FelV causes aplastic pancytopenia?
- Usually causes non-regenerative anemia +/- dysplasia; Pancytopenia can result from neoplasia or myelodysplastic syndrome
What is myelodysplasia?
- Abnormal formation of blood cells; Cells often cannot fully mature and cytopenias (anemia, etc) result
Which is more common, primary or secondary myelodysplasia?
- Secondary myelodysplasia
What are secondary myelodysplasias?
- Secondary dysmyelopoiesis due to underlying diseases, drugs, or toxins which can resolve if the underlying diseases is treated or the drug is withdrawn.
What is the number one cause of MDS in cats? What is the classic CBC picture of this disease process?
- FeLV infection
- Non-regenerative anemia with macrocytosis and increased/abnormal NRBCs
What suffix is used to refer to benign tumors of surface epithelium? What about malignant ones?
- "oma"
- Carcinoma
What types of neoplasia are those arising from the neural crest/neuroectoderm? How are they named?
- Epithelial tumors
- Not named with the same convention as other epithelial tumors (i.e. surface epithelium); Variable naming (e.g. melanoma vs. melanocytoma)
What suffix is used to refer to benign tumors of connective tissue? What about malignant ones?
- "oma"
- Sarcoma
Are melanocyte tumors a form of hemic neoplasia?
- No; they are sometimes called round-cell tumors due to their appearance but they are not hemic neoplasia
What is a leukemia?
- A hemic neoplasia originating in the bone marrow
How are leukemias classified?
- Lymphoid or myeloid
- Acute or chronic
What type of leukemia is important in humane medicine but extremely rare in veterinary medicine?
- Chronic myelogenous leukemia
What is CD34?
- A biomarker for hematopoietic stem/progenitor cells which is positive in most acute luekemias
Where does lymphoma originate? In what species does it occur?
- Lymphoid tissues or other organs/tissues
- Reported in many vertebrate species (e.g., frogs) and is common in mammals (dogs, cats, pigs, cattle, horses, etc.)
What are the different types of lymphomas?
- Large/immature cell ("high grade" lymphoma)
- Small/mature cell ("indolent" or "small cell" lymphoma)
In lymphoma, does cell size correlate with biologic behavior?
- Not always; Staging and phenotyping are needed to determine.
What is the best way to characterize the behavior/type of T cell lymphoma? What about B-cell lymphoma?
- Flow cytometry (also histology of lymph nodes in cats as biomarkers are not well developed)
- Histology of the lymph node
How is lymphoma categorized?
1) By cell morphology/biologic behavior (high grade vs. indolent/small cell)
2) By phenotype: B cell, T cell or NK cell (immunophenotyping used)
3) By patient stage (dogs) or distribution (i.e. multicentric, nasal, CNS, renal)
What are the stages of lymphoma in dogs?
- I-V (single LN, regional LN, generalized LN, spleen/liver, blood/bone marrow)
- a (healthy) vs b (clinically ill)
How is FIV associated with lymphoma?
- FIV+ cats have 6 times the risk of developing lymphoma
How is the leukemic phase of lymphoma (lymphoma involving the bone marrow) diagnosed?
- Usually diagnosed by finding neoplastic cells in blood smears (confirm with bone marrow sample)
Is lymphoma always biologically aggressive?
- No; Indolent lymphoma is common in dogs and cats; neoplastic cells/nuclei are often small (often called small-cell lymphoma)
What is small-cell lymphoma of the intestinal tract difficult to distinguish from in cats?
- IBD
- Large-cell (high grade) GI lymphoma is also common in cats
What is the most common hematopoietic neoplasm of horses?
- Lymphoma
What is the prevalence of lymphoma in horses? At what age does it generally occur?
- 2-5%
- Any age
What is the most common tumor of goats? Which form?
- Lymphoma
- Multicentric form
How is bovine leukemia virus spread?
- Iatrogenic methods (e.g., surgical/tattooing equipment)
- Biting flies
- Natural breeding
Lymphoma secondary to BLV infection is most common in cattle of which age?
- 4-8 years old; rare if under 2 YO
What are the two types of plasmacytoma?
1) Cutaneous
2) Non-cutaneous
Cutaneous plasmacytomas commonly occur at which locations on the body?
- Ears
- Head
- Paws
- Trunk
If a non-cutaneous plasmacytoma is not cutaneous or oral, there is a higher risk of what? If found in the internal organs/tissues or lymph nodes, it is considered more _____________.
- Systemic spread and/or multiple myeloma
- Aggressive
In which species does multiple myeloma occur? What is the primary site of infiltration?
- Dogs, cats, horses
- Bone marrow
Sites other than the bone marrow can be affected by or an origin of multiple myeloma. What are these sites and why is this particularly pertinent in cats?
- Spleen and liver
- This is an additional diagnostic criteria in cats because it is so common and cats rarely get osteolytic lesions
What are some clinical signs associated with multiple myeloma which can be nonspecific and insidious (weakness, anorexia)?
- PUPD: Hypercalcemia and/or myeloma-related renal disease
- Lameness, paresis, paralysis and pain: Osteolysis and/or spinal cord compression
- Bleeding diatheses: epistaxis, gingival bleeding, intraocular hemorrhage, melena/hematochezia, retinal hemorrhage, and/or venous dilation (due to hyperviscosity syndrome (high globulin levels) +/- platelet dysfunction
- CNS signs: Seizures due to hyperviscosity syndrome or severe hypercalcemia
What types of lesions does cutaneous histiocytoma result in? What types of dogs are commonly affected? Describe their typical progression.
- Solitary lesions
- Young dogs
- Spontaneously regress
What types of lesions does cutaneous histiocytosis result in? Is it metastatic?
- Multiple skin lesions
- Occasionally metastatic
What forms of histiocytic neoplasia occur in cats? How common are they?
- Histiocytic sarcoma
- Feline Progressive Histiocytosis
- Pulmonary Langerhans cell histiocytosis
- All three are rare
What are some breeds commonly affected by mast cell neoplasia?
- Boxers
- Bull terriers
- Pit bulls
- Boston terriers
- Labradors
How is mast cell neoplasia diagnosed/graded?
- Diagnosed easily via cytology (FNA)
- Graded via histopathology (biopsy) -> 3 tier Patnaik or 2-tier Kiupel systems
High grade mast cell tumors are more likely to do what?
- More likely to locally recur and/or metastasize
How is TVT spread?
- By coitus; rarely via licking/grooming
- Can be transmitted to/from coyotes and other wild dogs
How is TVT treated?
- Highly responsive to vincristine chemotherapy or radiation therapy
- Immunotherapy can help, e.g., IL-2 injection into tumors
What is the origin of melanoma? Describe its morphology.
- Neuroectoderm origin
- Can appear cohesive (as epithelial tissue), spindloid (as mesenchyma tissue), or all 3 at once
When is melanoma particularly difficult to differentiate from round cell tumors?
- When poorly differentiated (with few or no melanin granules; Amelanocytic melanoma)
Still learning (99)
You've started learning these terms. Keep it up!