Spermatogenesis
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
73 Terms
what species have inguinal testis?
bull, ram, stallion, camel
what species have perineal testis?
boar, dog, tomcat
what are the reproductive components in the scrotum?
testes, epididymmis, vas deferens
T/F: testis develop outside the body
false, inside
cryptorchidism
failure of testes to descend into scrotum
phases of testicular descent
1. transabdominal phase- attached to gubernaculum. Cells of peritoneum infiltrate gubernaculum so it becomes fused. Which then tells gubernaculum to grow through inguinal ring into vaginal cavity of scrotum
2. inguinal scrotal phase:
testis enters scrotum and gubernaculum regresses which pulls testis down to bottom of vaginal cavity. Gubernaculum keeps testis attached to bottom of scrotum
where are testis typically retained if they fail to descend?
abdomen or inguinal canal
Dogs with cryptorchidism are 9-14x more likely to develop testicular cancer. Why?
testosterone and growth factors are aberrant = irregularity driving cancer
T/F: spermatogenesis occurs at the same temp of the body
false, needs temps 4-6 degrees cooler than body
What are the three structures that help achieve a cooler temperature of the testes?
pampiniform plexus
cremaster muscle
scrotal skin
function of pampiniform plexus
warm arterial blood from body is cooled on way to testis because surrounding veins are returning cooler blood from testis
function of cremaster muscle
contracts and relaxes to promote venous return of testicular blood
-cannot facilitate long term contractions
how does the scrotal skin help keep the temperature of the testis lower than the body?
1. sweat glands innervated with sympathetic nerves
2. thermosensitive nerves that tell body to increase RR to induce panting
How does heat stress effect sperm production and motility?
decrease drastically
which species have retroperitoneal testis ?
birds, elephants, sloths, armadillos, whales, dolphins
________ is the primary reproductive organ in the male. They produce what?
testes
spermatozoa, hormones and proteins, fluids
what is contained within the testicular parenchyma?
seminiferous tubules
leydig cells
capillaries
lymphatic vessels
Ct
where does spermatogenesis occur?
seminiferous tubules
T/F: the compartments of the seminiferous tubules are basal, adluminal, and interstitial
false, only basal and adluminal
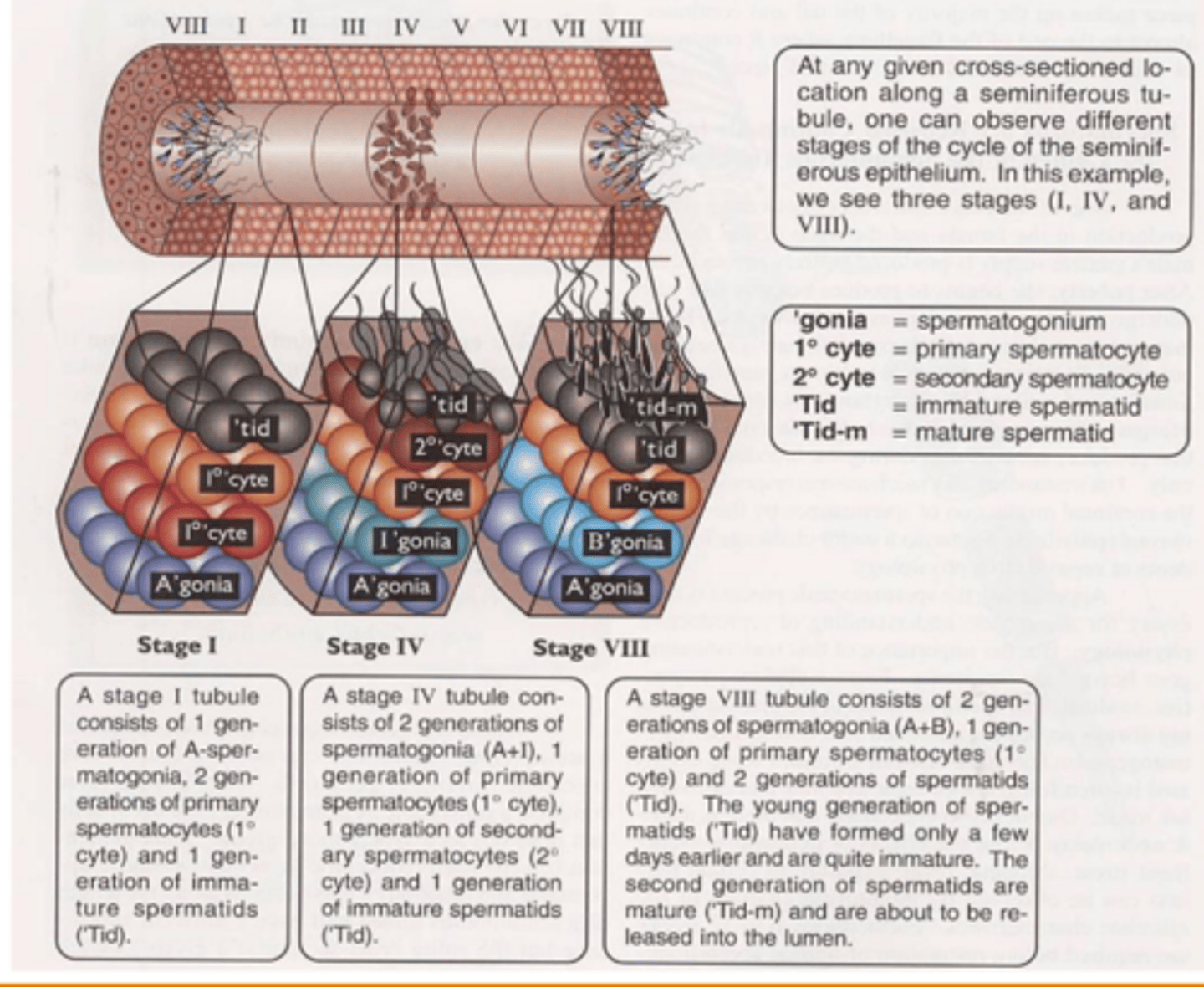
What is housed in the:
a. basal compartment
b. adluminal compartment
spermatogonia, primary spermatocytes
maturing spermatocytes/ spermatids
what separates the basal and adluminal compartments? aka blood testis barrier
tight junctions of sertoli cells
What is the purpose of separating the basal and adluminal compartment?
creates immune-privileged site in testicular epithelium to allow for meiosis of spermatocytes
ALSO protects post-meiotic germ cells from cytotoxic agents
OVERALL: protection from male immune system and toxins
goals of spermatogenesis
1. Provide continual supply of male gametes through stem cell renewal.
2. Provide genetic diversity.
3. Provide billions of sperm daily for maximum reproductive ability.
4. Provide an immunological site for developing germ cells so they are not destroyed by males immune system
what are the phases of spermatogenesis?
Where does each phase occur?
proliferation- basal
meiosis- adluminal
differentiation- adluminal
proliferation phase aka _____________________
a. what occurs during this phase?
b. when does it begin?
c. What is produced from this phase and where do 'they' go?
spermatocytogenesis
mitotic divisions
puberty
spermatogonia B
cross BTB
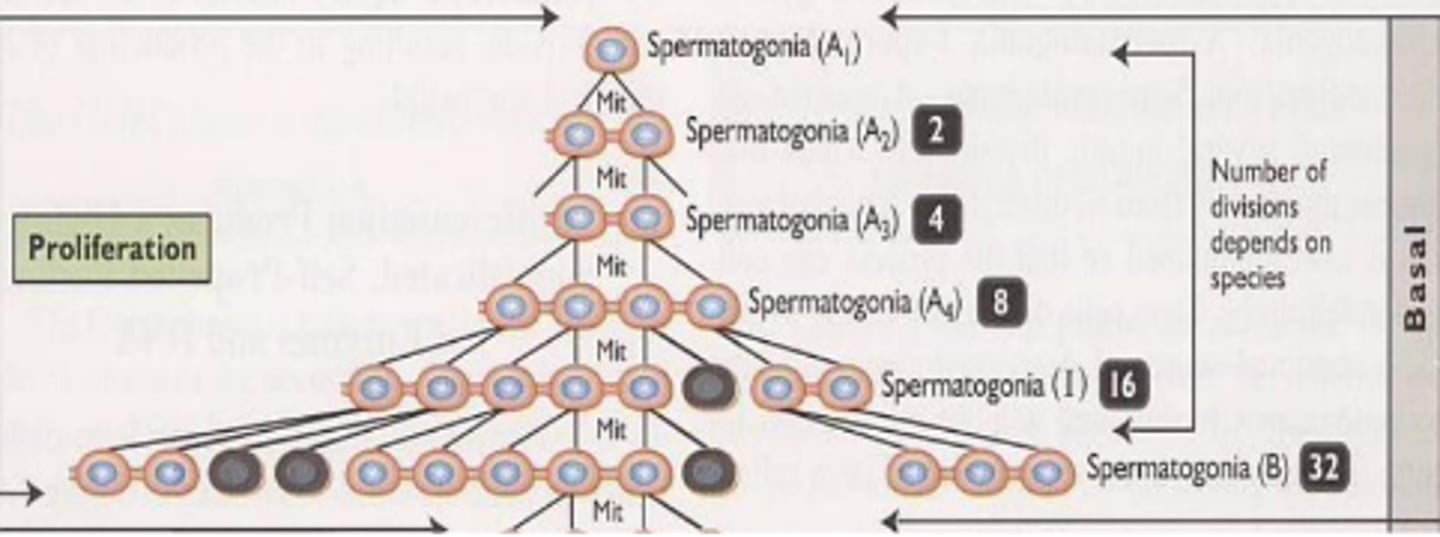
T/F: all species undergo 5 rounds of mitosis in the proliferation phase
false
Meiotic phase
a. what occurs during this phase?
b. when does it begin?
c. What is produced from this phase and where do 'they' go?
meiosis I
when primary spermatocytes enter adluminal compartment
Differentiation phase aka _____________ has an end result of?
spermiogenesis
creating a sperm cell potentially capable of traveling to and fertilizing an egg.
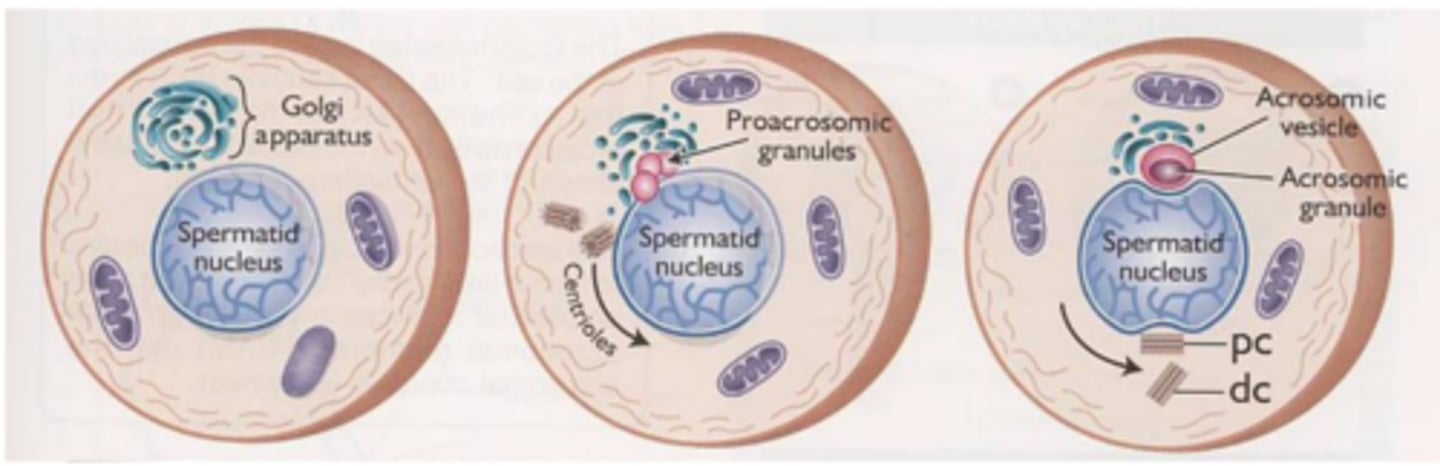
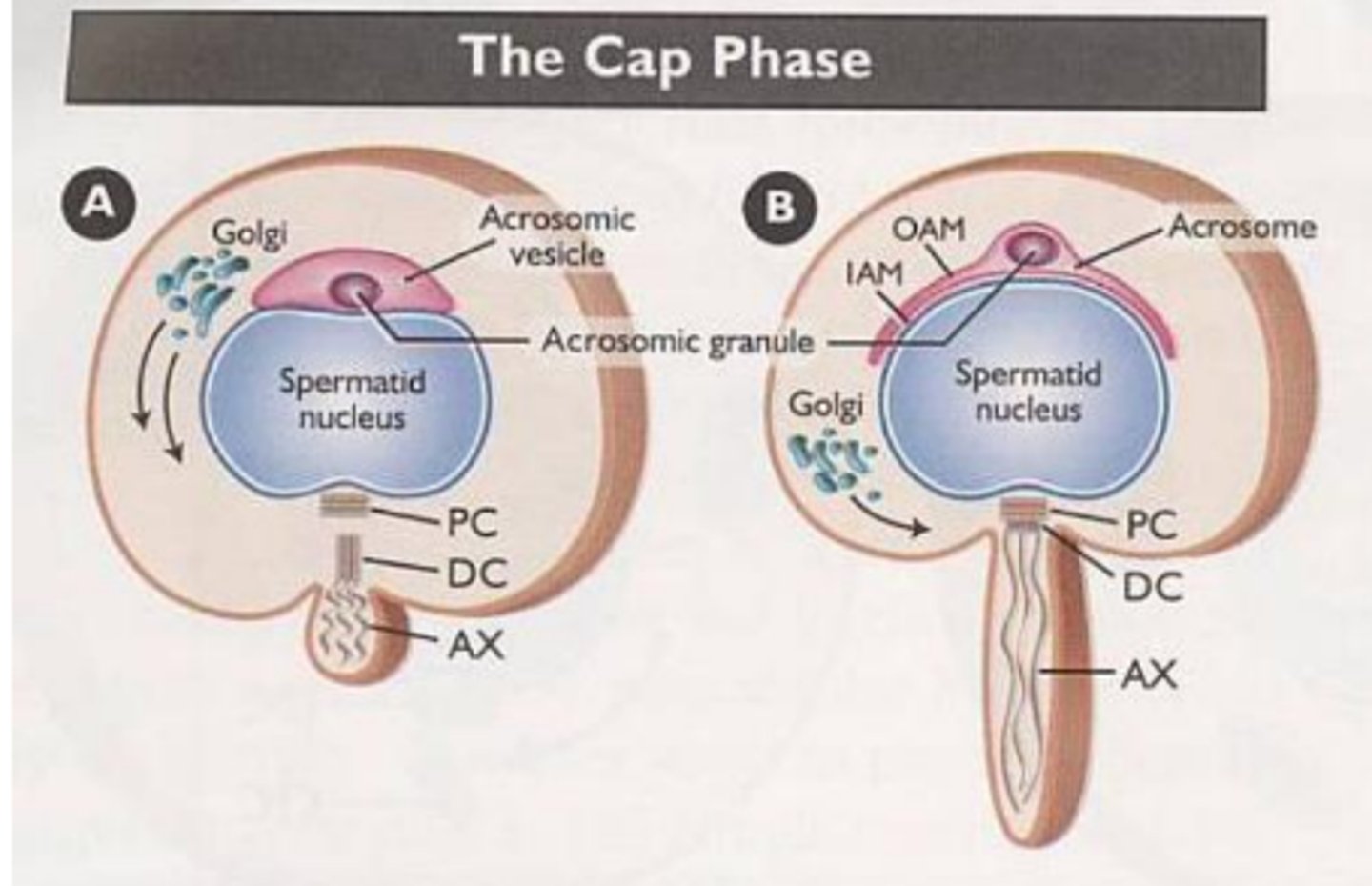
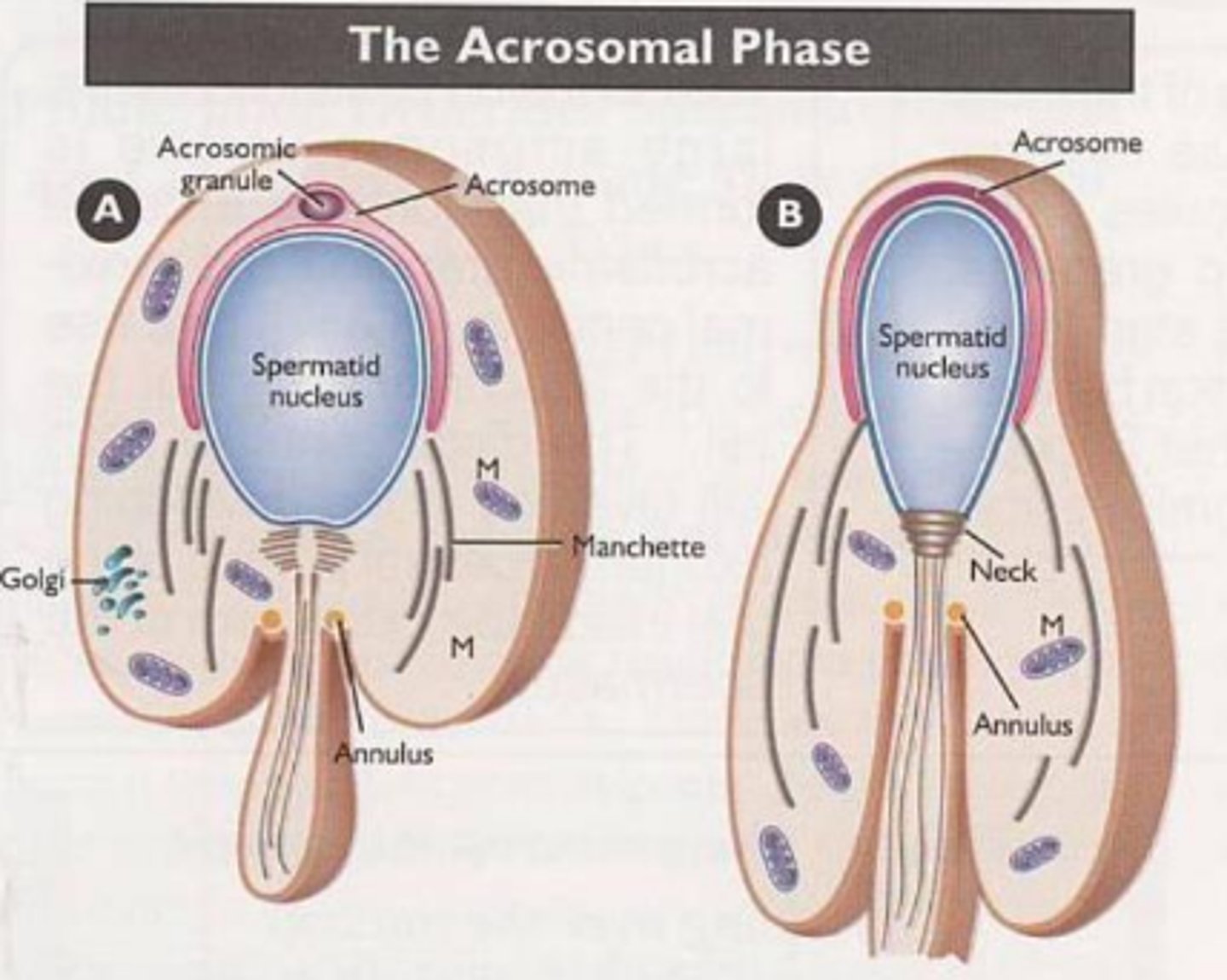
what are the phases of differentiaiton
golgi
cap
acromoal
maturation
The golgi phase begins with a golgi apparatus. what else is occuring?
vesicles of golgi fuse and create pro-acrosomic granules until a large acrosomic vesicle is formed
Cap phase is where the _________ forms a distinct cap over the nucleus. What happens to the golgi? what is the end result?
acrosome
disappears
primitive flagellum begins to project
What occurs during the acrosomal phase?
acrosome spread across nucleus and eventually forms neck filled with proteinsq
The maturation phase forms the middle piece of sperm. How?
mitochondria accumulate around flagellum
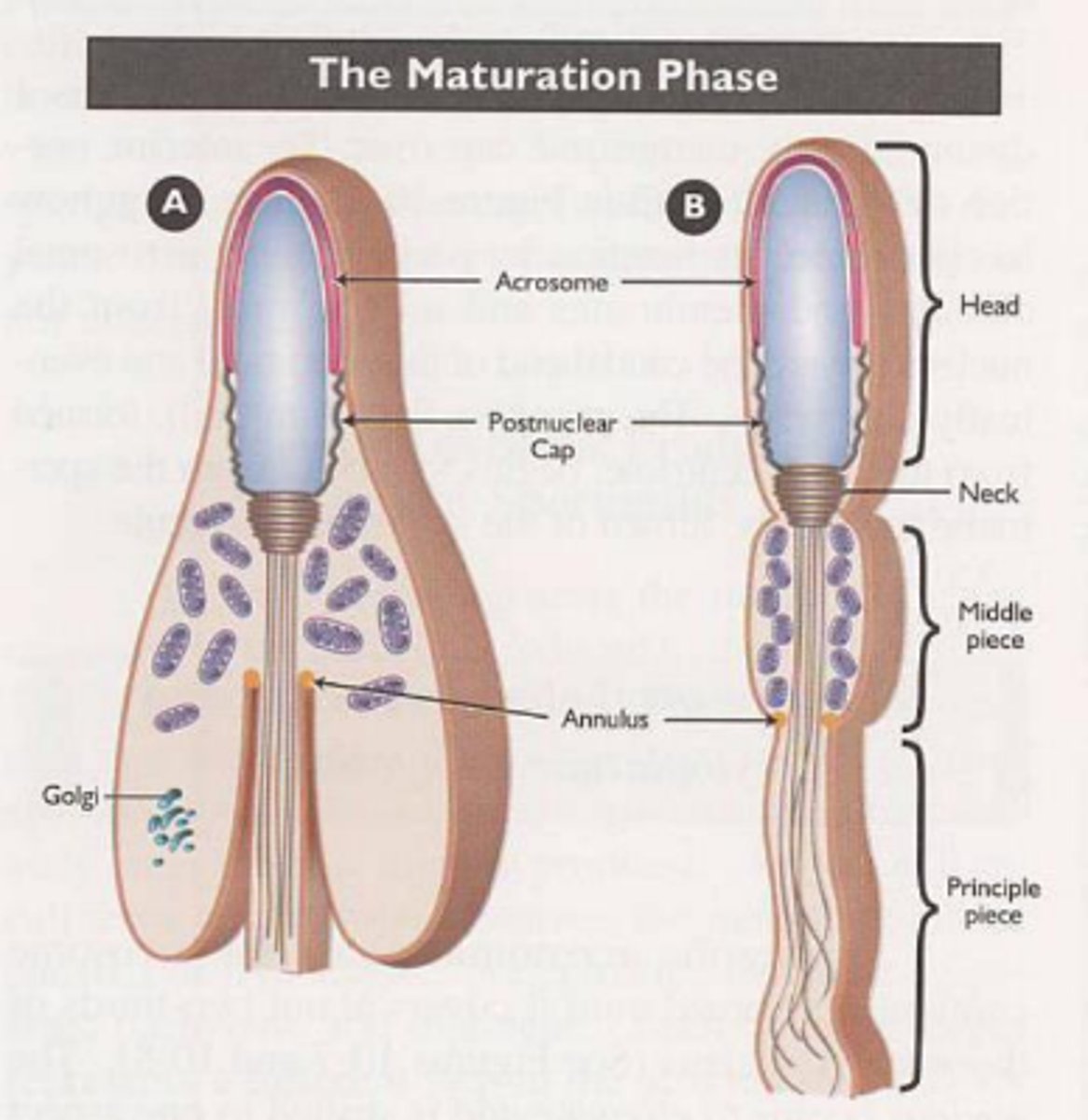
Mature sperm is composed of a head and tail. What is found in the head? the tail?
the head consists of nucleus, acrosome, and post-nuclear cap
the tail consists of a middle piece, principle piece, and terminal piece
______ is the release of spermatozoa from _________ cells into lumen of seminiferous tubules
spermiation
sertoli
T/F: after spermatozoa is release it can fertilize an egg
FALSE, chromatin is compacted meaning transcription and translation of DNA have been stopped
what compacts chromatin in the nucleus of spermatozoa?
keratin, disulfide bonds
what is the acrosome filled with? why?
hydrolytic enzymes to penetrate oocyte
T/F: mitochondria is rapidly degraded after fertilizaiton
true
Even though spermatozoa are continually released spermatogenesis occurs in cycles. Explain
many stages are occurring at different locations
T/F: length of spermatogenesis varies by species
true
What hormones does spermatogenesis require?
GnRH -> LH, FSH -> gonadal steroid (testosterone and estrogen)
Is GnRH secretion pulsatile or continous? what is the effect on LH and FSH?
pulsatile
LH pulses immediately after GnRH but has a short half life which allow for periodic testosterone production
FSH also follows but at lower concentration for longer periods
LH acts on __________ cells which convert progesterone to ________________ which is then transported to _______ cells to do what?
leydig
testosterone
sertoli
maintain spermatogenesis
_________ tells sertoli cells to initiate spermatogenesis but eventually theses cells become less responsive
FSH
When sertoli cells are still responsive to FSH what do they do after initiating spermatogenesis?
convert testosterone to estradiol for negative feedback
What else do sertoli cells secrete?
inhibin, to suppress FSH secretion
What is the effect of using exogenous testosterone/ anabolic steroids on the HPT axis?
GnRH decreases -> decreases LH and FSH -> less testosterone produced by leydig cells = inability to maintain spermatogenesis
T/F: when spermatogenesis is over and spermatozoa are secreted into the lumen of seminiferous tubules they are now able to fertilize an egg
FALSE
Explain passageway of spermatozoa from lumen of seminiferous tubules to head of epididymis
rete testis -> efferent duct -> epididymal duct
What are the 3 sections of the epididymis
caput (head)
corpus (body)
cauda (tail)
How does sperm concentration change when they enter the caput as compared to when they move further through the epididymis?
originally have low concentration due to high levels of rete fluid which is then absorbed by efferent ducts and caput to concentrate sperm number
The location of __________ _______ can help identify sperm maturation issues
cytoplasmic droplet
T/F: when sperm reach the tail of the epididymis they are mature
true
Why is contraction decreased in tail compared to body and head of epididymis?
conserve sperm until sexual excitation and ejaculation
what occurs to the old sperm if no sexual release occurs?
periodic contractions to move old sperm to ductus deferens and urethra to be flushed out during urination
Purpose of accessory sex glands
nourish spermatozoa
activate spermatozoa
clear female repro tract
produce secretions that assist in transport
plug to help retain spermatozoa in female repro tract (some species)
_________ is the enlargement of the ductus deferens that open into pelvic urethra
ampulla
which glands empty directly into pelvic urethra?
vesicular
Prostate gland location varies based on species. It can be corpus or disseminate. Explain
corpus is outside urethralis muscle and disseminate is along walls of pelvic urethra
which glands produce the viscous secretion that causes seminal plasma to coagulate following ejaculation?
bulbourethral
what do the vesicular glands secrete? why?
what does the prostate gland secrete? why?
what does the bulbourethral glands produce? why?
what are the two types of penises?
musculocavernosus
fibroelastic
T/F: the musculocavernous penis have limited erectile tissue so it is encased in tunica albuginea
false, fibroelastic
parts of the penis
glans
shaft
base
the dog has two distinct regions: bulbus glandis and pars longa glandis. what runs through these structures?
os penis
mechanisms of erection
1. erotogenic stimuli
2. activate repro behavior center in hypo
3. stimulate parasym nerves
4. which also release NO
5. NO initiates cascade that causes erection
what is the role of nonadrenergic noncholingeric parasympathetic neurons in erection?
when stimulate they fire and release NO leading to vasodilation
Musculocavernous has a (slow/fast) erection compared to fibroelastic penis
slow
mechanism of ejaculation
intromission
sensory stimulation of glans penis
vontraction of muscles and accessory glands
expulsion of semen
what is a good estimator of sperm producing ability?
scrotal circumference