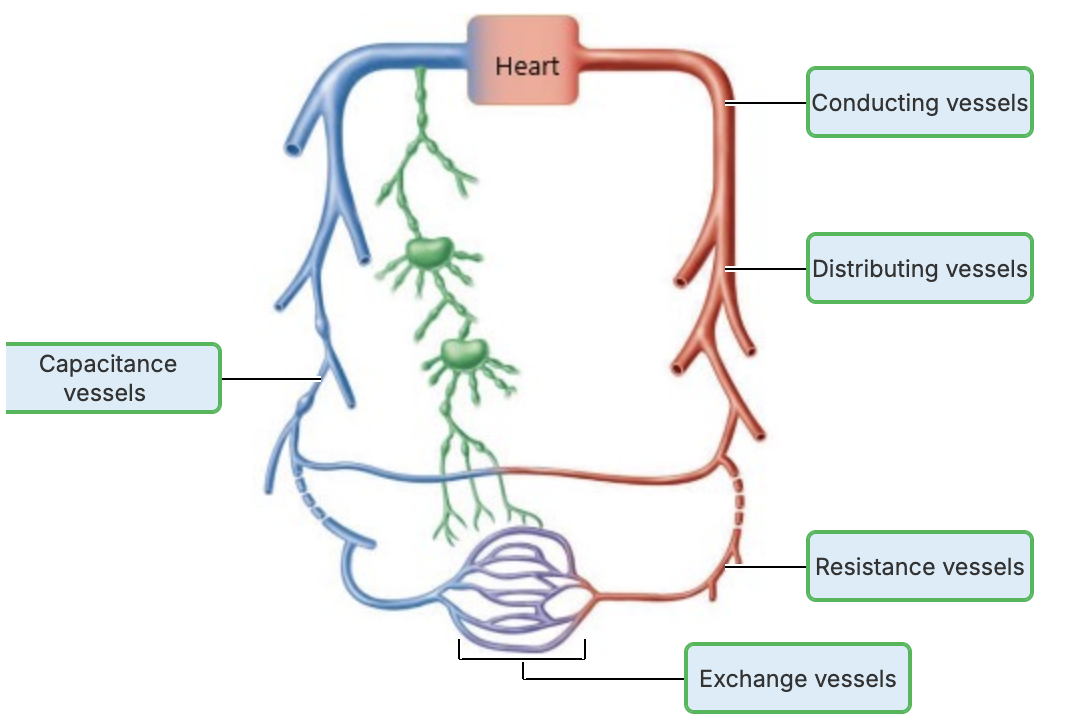
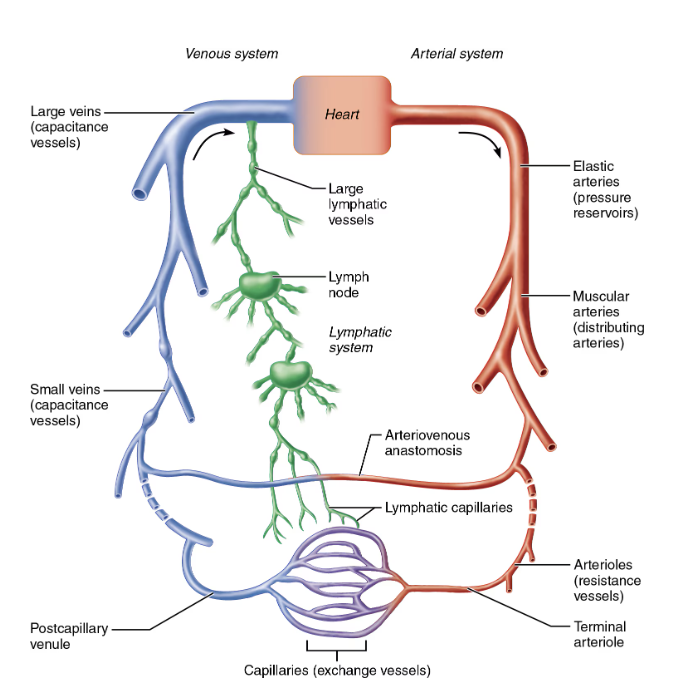
(19.2.3.4.5) Arteries, Capillaries, Veins, Anastomoses
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
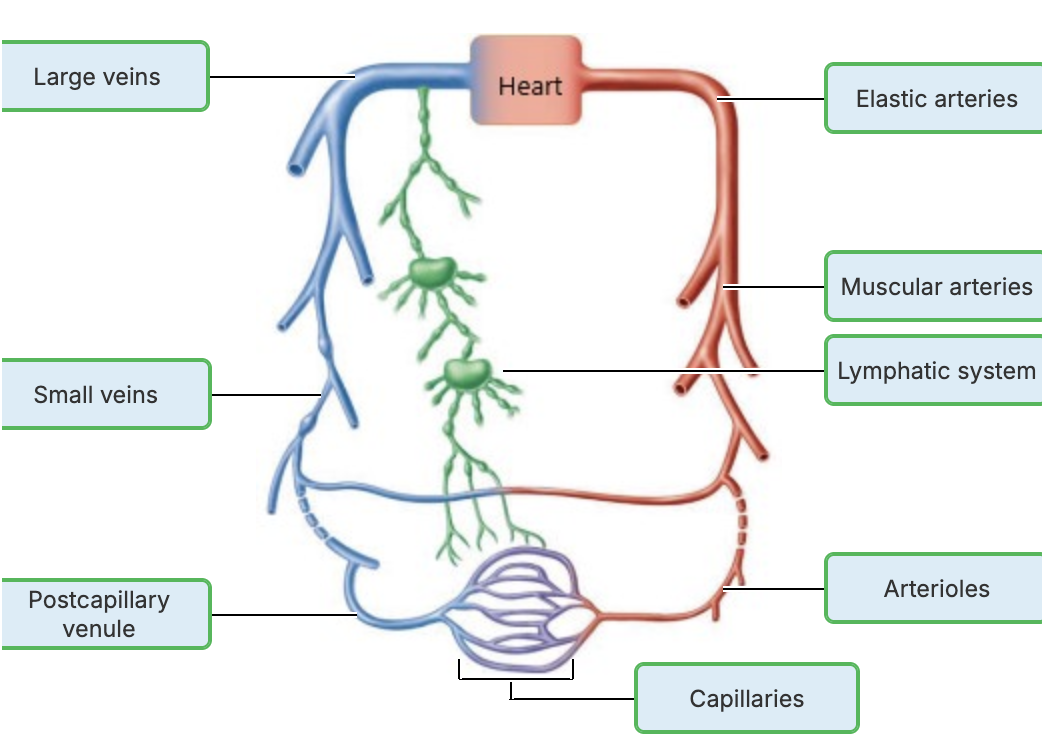
Name the three types of Arteries
Based on size and function
Elastic arteries
Msucular arteries
Arterioles
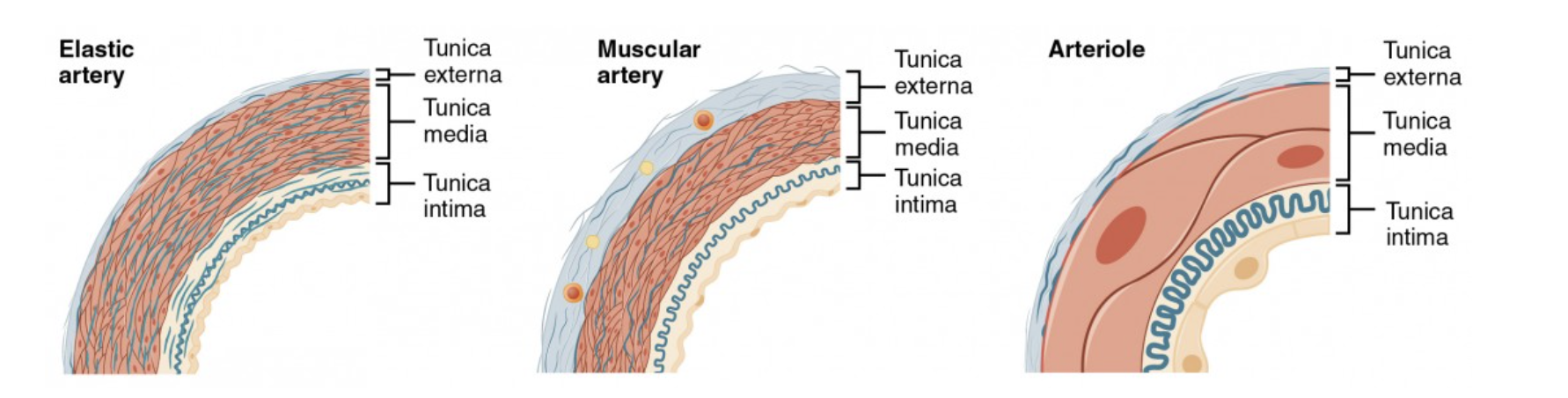
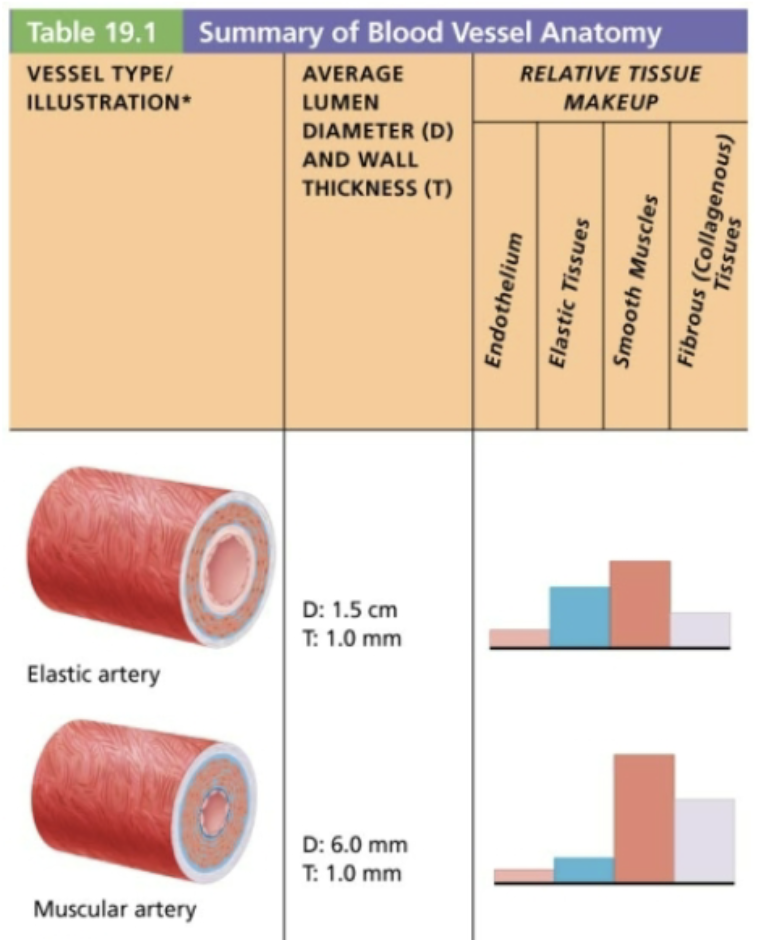
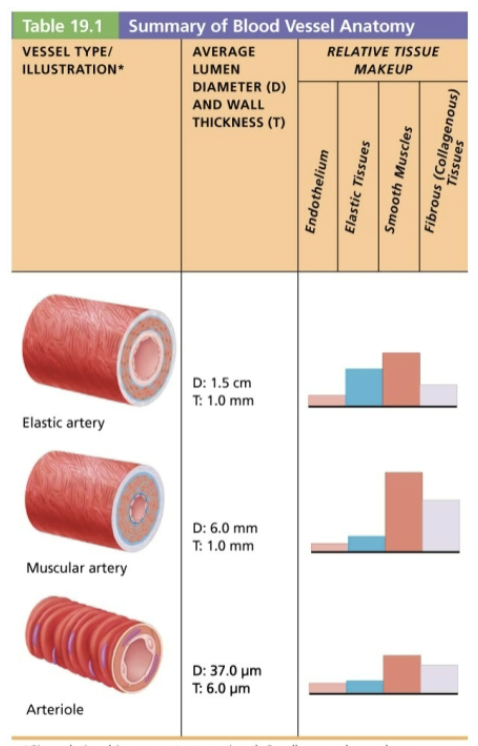
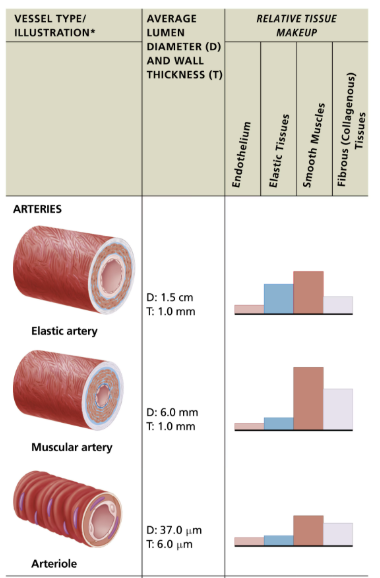
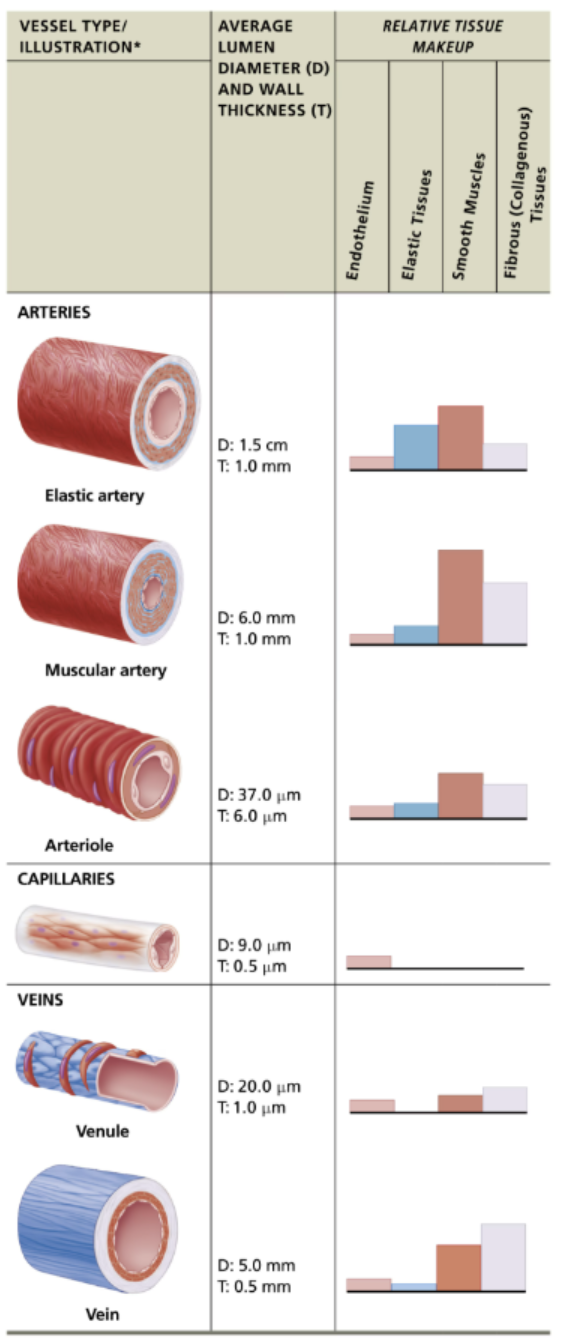
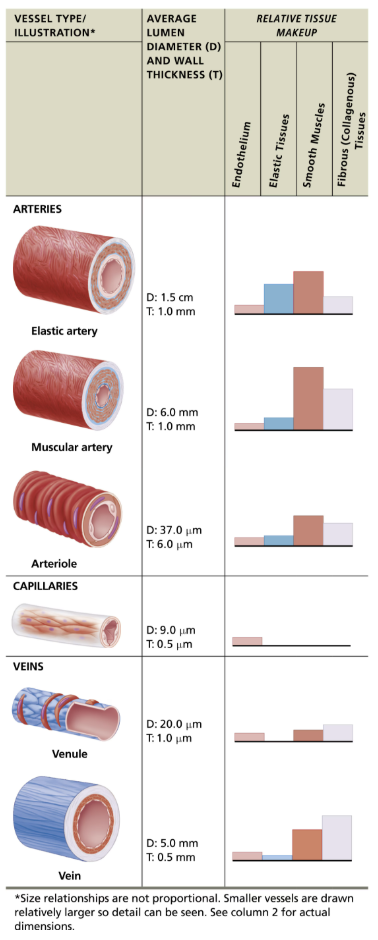
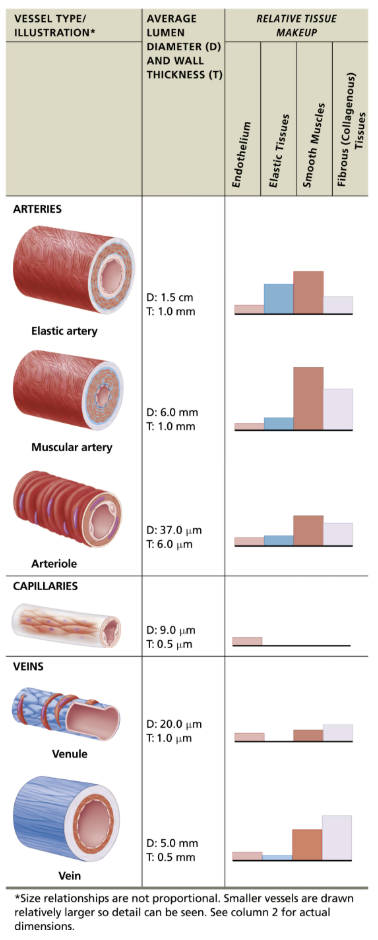
Describe Structure & Function & Example of Elastic Arteries
STRUCTURE
Thick-walled with large LOW RESISTANCE lumen
Elastin found in all three tunics, mostly tunica media
Contain substantial smooth muscle
But INACTIVE in vasoconstriction
FUNCTION
Acts as pressure reservoirs that expand and recoil as blood is ejected from heart
Allows for continuous blood flow downstream even between heartbeats
Also called conducting arteries because they conduct blood from heart to medium sized vessels
EXAMPLE
Aorta and its major branches
Elastic arteries give rise to what?
Muscular arteries
Describe Structure & Function & Example of Muscular Arteries
STRUCTURE
Diameters range from pinky finger size to pencil-lead size
Have THICKEST tunica media, with more smooth muscle, but less elastic tissue
Tunica media sandwich between elastic membranes
ACTIVE in vasoconstriction
FUNCTION
Also called distributing arteries because they deliver blood to body organs (Femoral, brachial, external carotid arteries)
EXAMPLE
Account for most of named arteries
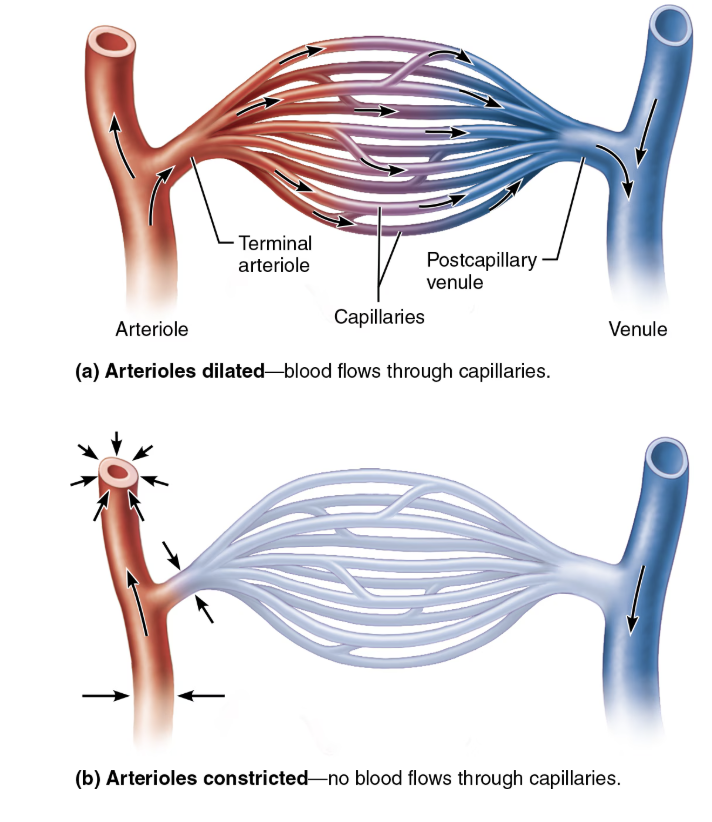
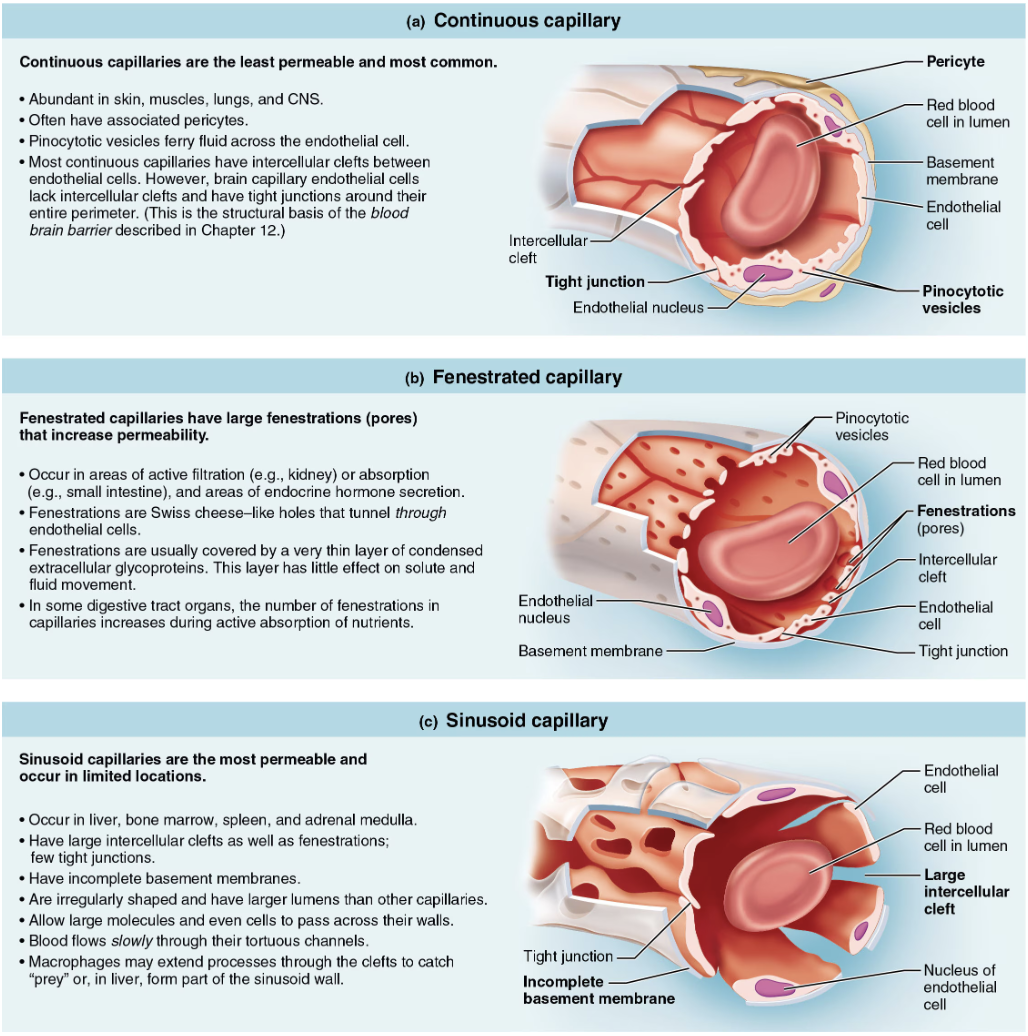
Describe Structure & Function & Example of Arterioles
STRUCTURE
Smallest of ALL arteries
Larger arterioles contain ALL three tunics
Smaller arterioles are mostly single layer of smooth muscle surrounding endothelial cells
FUNCTION
Control flow into capillary beds via vasodilation and vasoconstriction of smooth muscle
Also called resistance arteries because changing diameters change resistance to blood flow
EXAMPLE
Leads to capillary beds
Arterioles lead to what?
Capillary beds
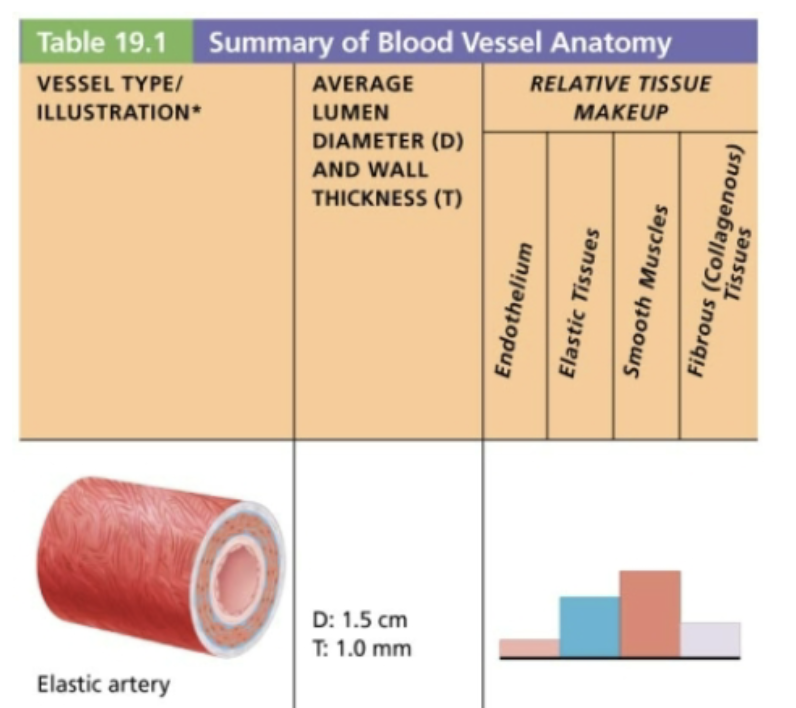
Summary of Artery Anatomy
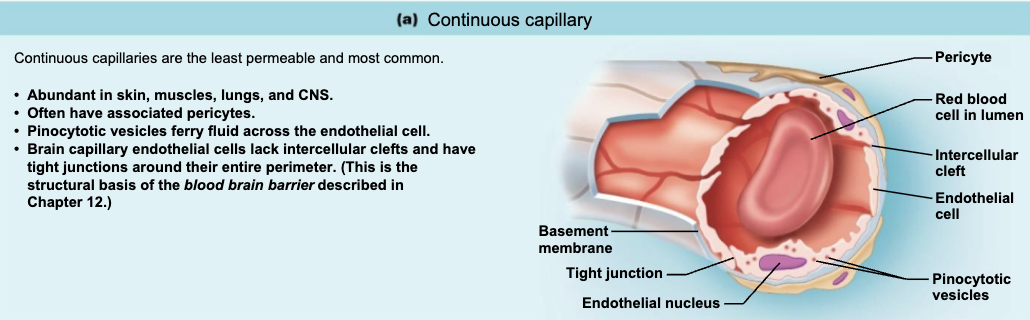
Structure and Function of General Capillaries
STRUCTURE
Microscopic vessels
Diameters so small only single RBC can pass through at a time
Pericytes: spider-shaped stem cells help stabilize capillary walls, control permeability, and play a role in vessel repair
ALL capillary endothelial cells are joined by tight junctions with gaps called intercellular clefts → allows passage of fluids and small solutes
FUNCTION
Supply almost every cell, except for cartilage, epithelia, cornea, and lends of eyes
Exchange of gasses, nutrients, wastes, hormones, etc., between blood and interstitial fluid
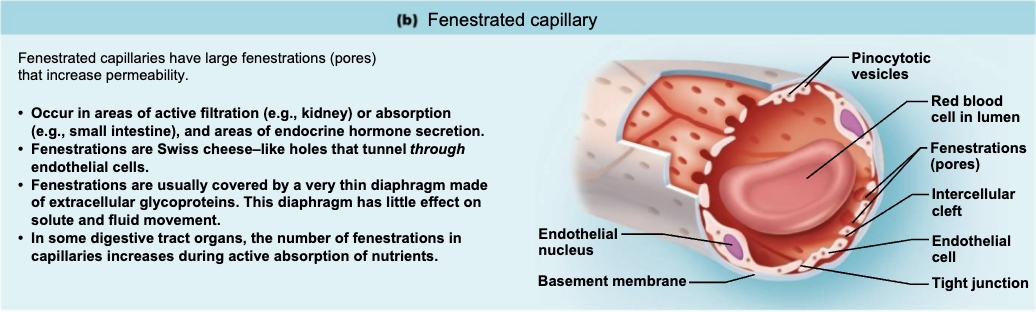
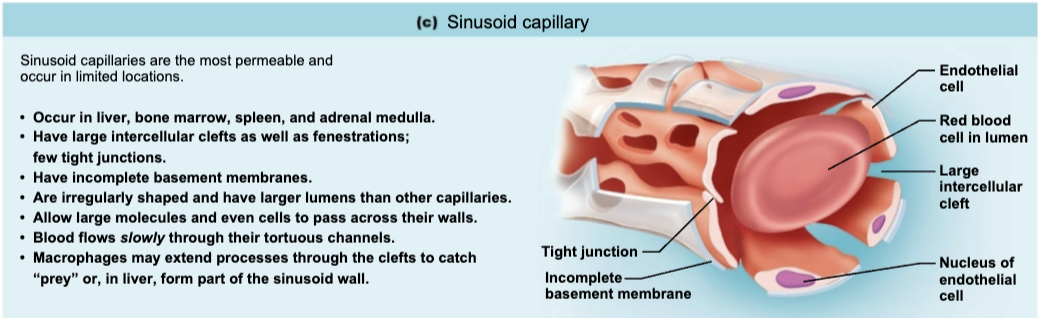
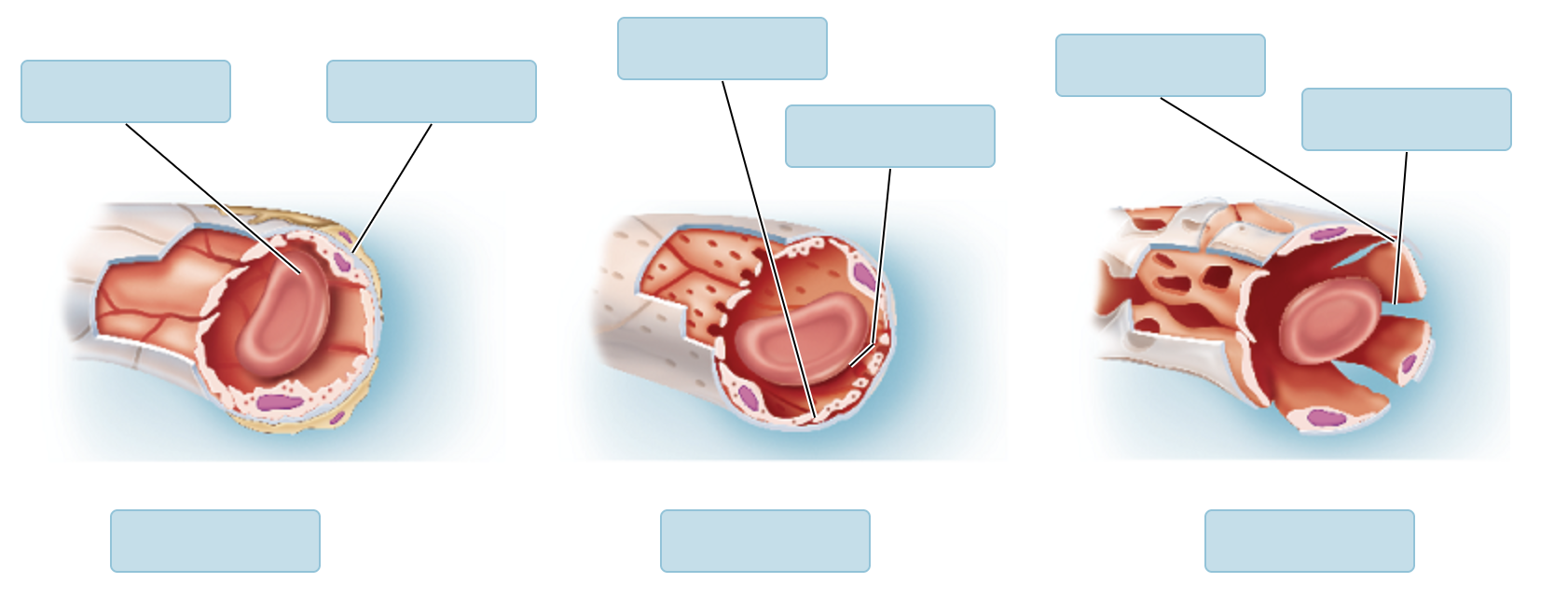
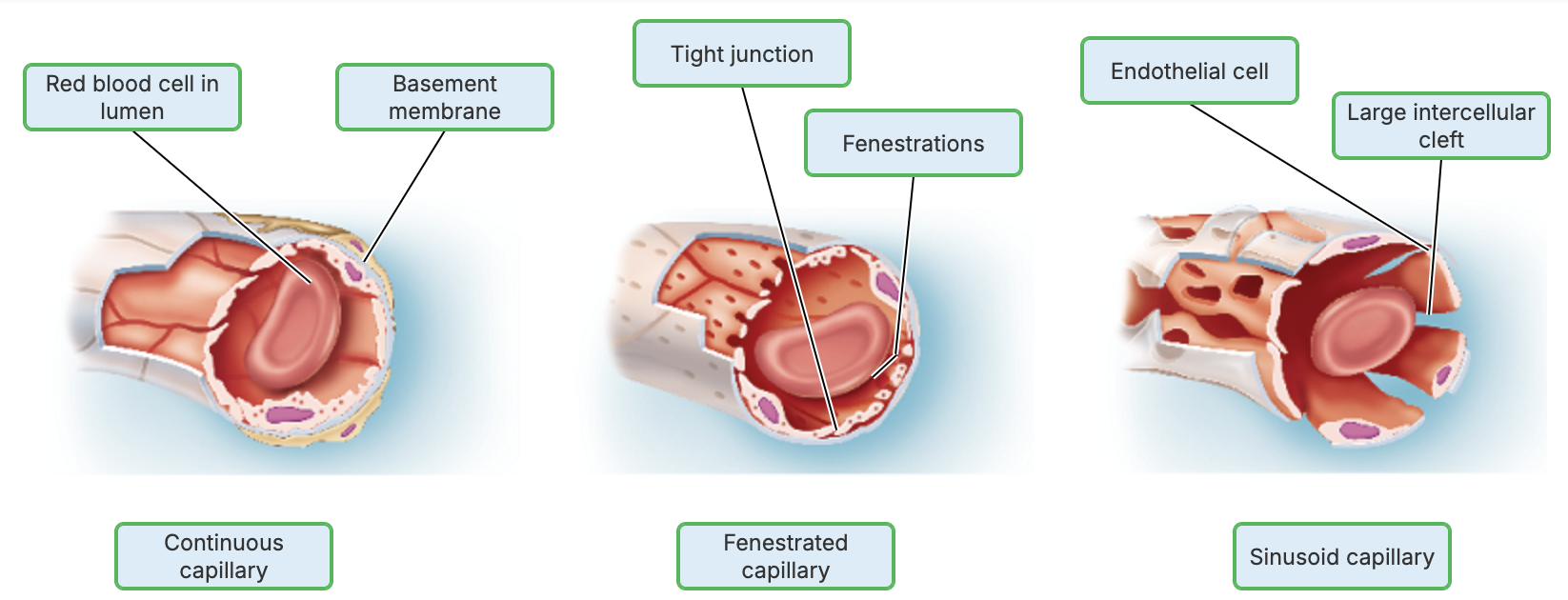
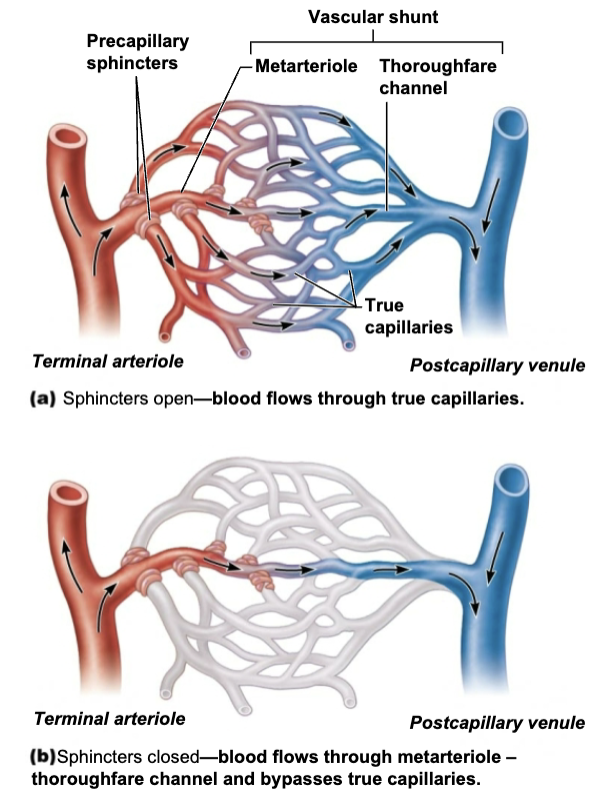
Name the three types of Capillaries
Continuous capillaries
Fenestrated capillaries
Sinusoidal capillaries
Describe Location & Function of Continuous capillaries
LOCATION
Abundant in muscle, lungs, and CNS
FUNCTION
Continuous capillaries of brain are unique → form blood brain barrier, totally enclosed with tight junctions and no intercellular clefts
Describe Location & Function of Fenestrated capillaries
LOCATION
Found in areas involved in active filtration (kidneys), absorption (intestines), or secretion (endocrine hormone)
Describe Location & Function of Sinusoid capillaries
LOCATION
Found ONLY in the liver, bone marrow, spleen, and adrenal medulla
Fewer tight junctions (usually fenestrated with larger inerceullar clefts
Incomplete basement membranes
Usually have larger lumens
FUNCTION
Blood flow is sluggish → allows time for modification of large molecules and blood cells that pass between blood and tissue
Contain macrophages in lining to capture and destroy foreign invaders
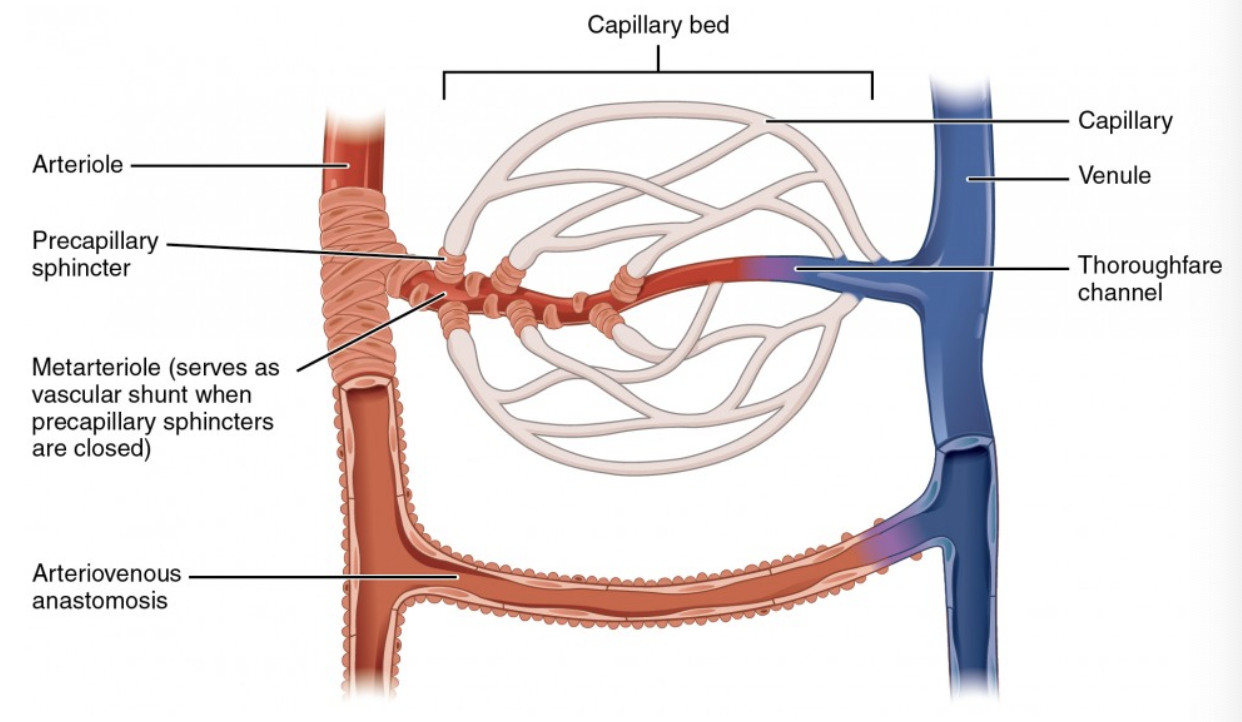
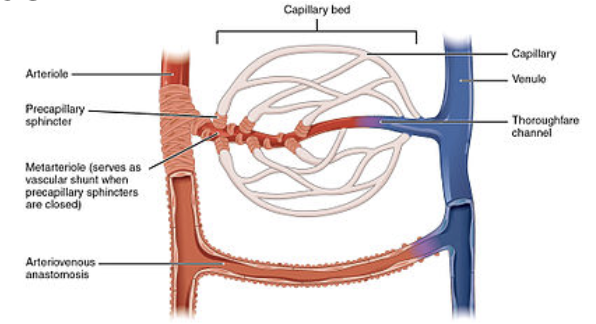
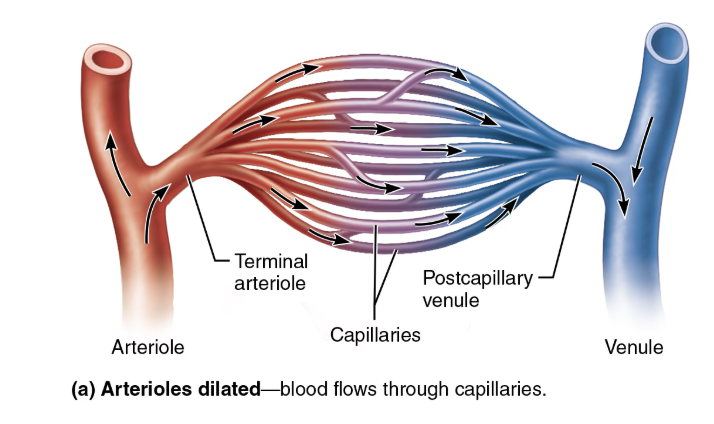
Define Capillary Bed
Interwoven network of capillaries between arterioles and venules
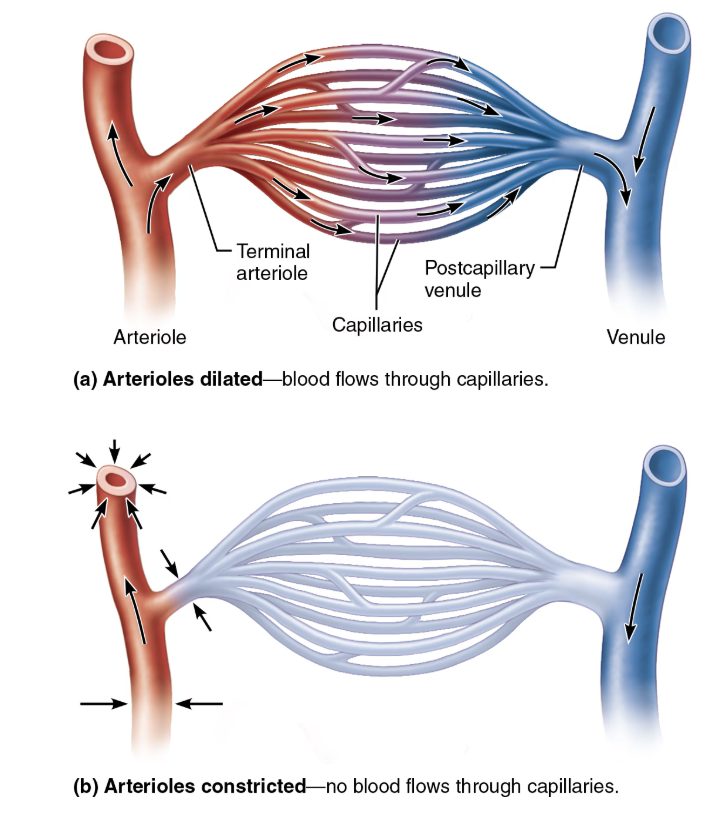
Define Microcirculation
Flow of blood through bed
Name and Describe the Two Types of Vessels in Capillary Beds
Vascular shunt
Channel that connects arteriole directly with venule (metarteriole-thoroughfare channel)
True capillaries
Actual vessels involved in exchange (10 to 100 exchange vessels)
Normally branch from metarteriole and return to thoroughfare channel
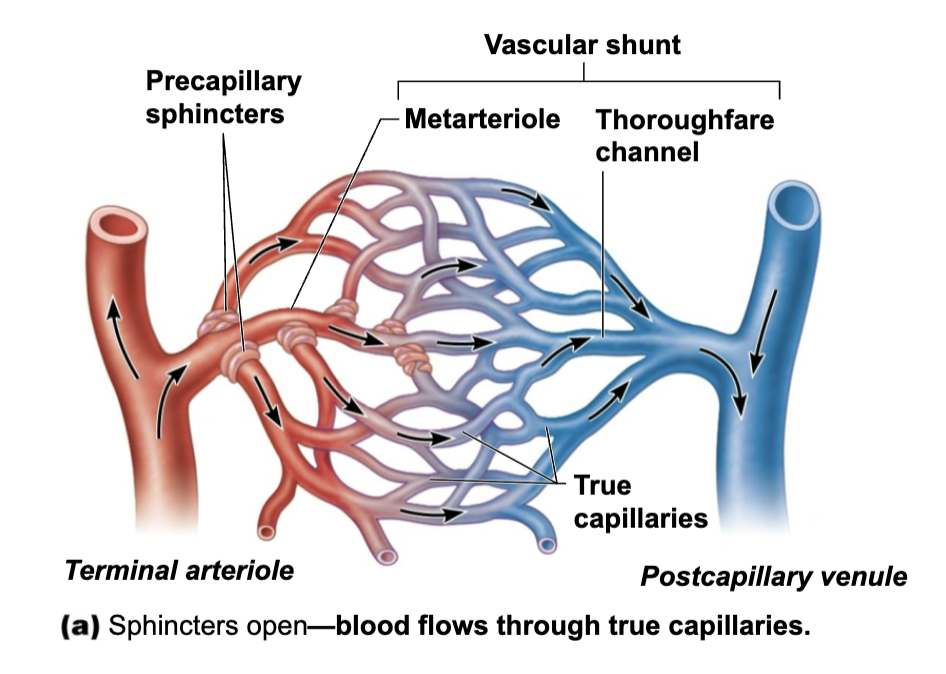
Role of Precapillary sphincters
Regulate blood flow into true capillaries
Blood may go into triw capillaries or to shunt
Regulated by local chemical conditions and vasomotor nerves
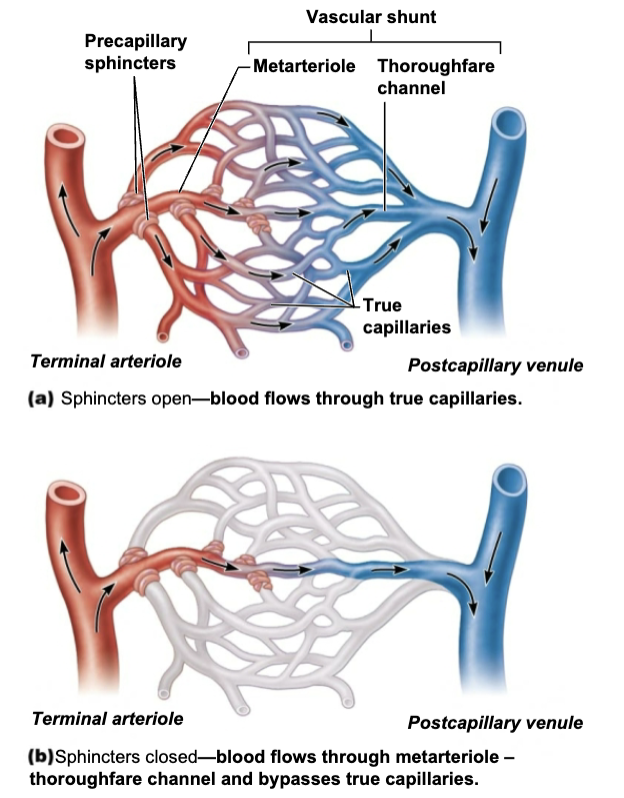
Describe the Pathway Blood takes through Capillary Beds
Arteriole
Blood enters the capillary bed from a terminal arteriole.
Metarteriole
This is a short vessel that links the arteriole to the capillary network.
Precapillary Sphincters
Ring-like muscles at the entrance to the true capillaries that act as valves.
Capillary Bed
A network of interconnected capillaries where exchange with tissues occurs.
Vascular Shunt
A vessel that connects the metarteriole directly to the venule, allowing blood to bypass the capillary network.
Venule: Blood exits the capillary bed and flows into a venule, which merges to form larger veins.
Summary of Capillary Anatomy
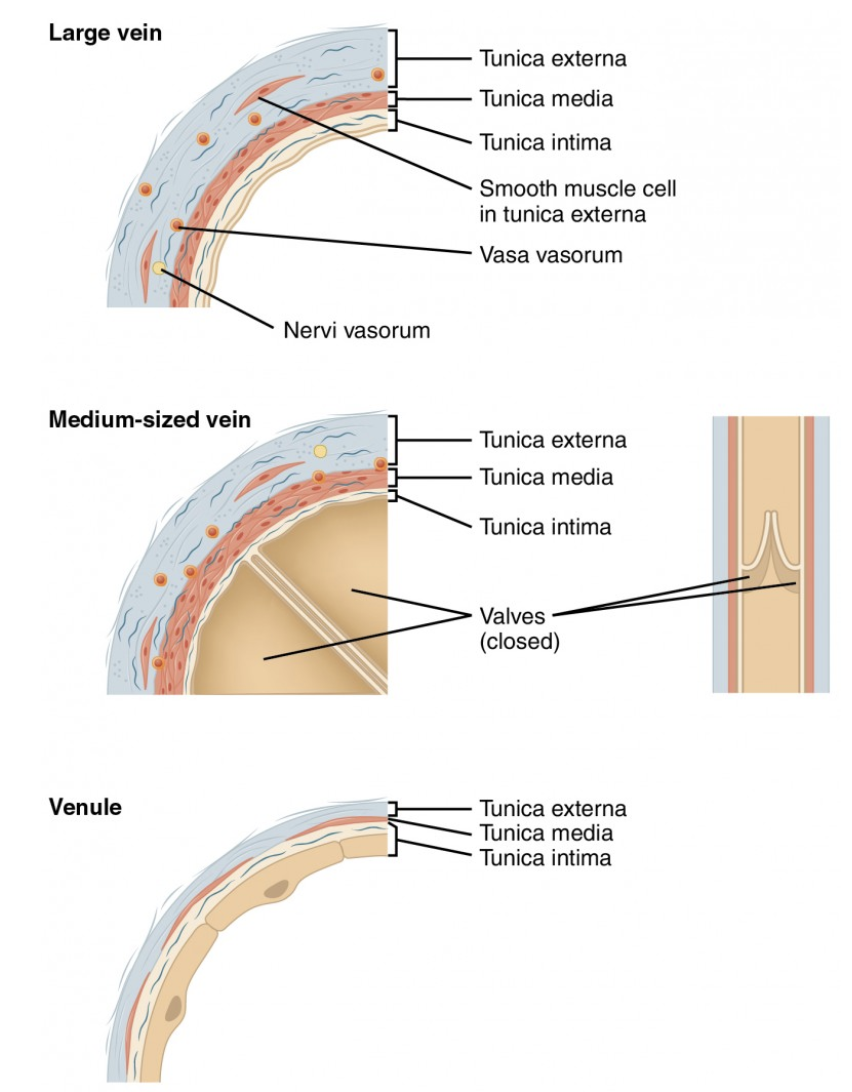
Structure and Function of Veins
STRUCTURE
Formation begins when capillary beds unit in post-capillary venules and merge into larger and larger veins
FUNCTION
Carry blood TOWARD the heart
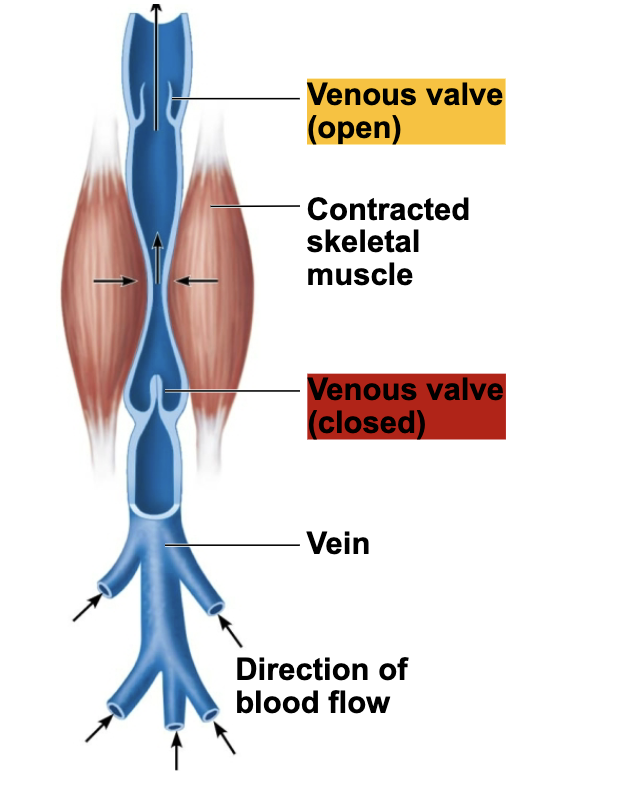
Role of Venous Valves
Folds of the tunica intima of certain veins that prevent blood from flowing backward
Most abundant in the veins of the limbs.
Mechanism of Venous Blood Flow
Veins carry blood from the capillary beds toward the heart
Along the route, the diameter of successive venous vessels increases, and their walls gradually thicken as they progress from venules to larger and larger veins
Name the Two types of Veins
Venules
Veins
Describe Structure & Function of Venules
STRUCTURE
Capillaries unite to form post-capillary venules
Consists of endothelium and few pericytes
Larger venules have one or two layers of smooth muscle cells
FUNCTION
Very porous → allow fluids and WBCs into tissues
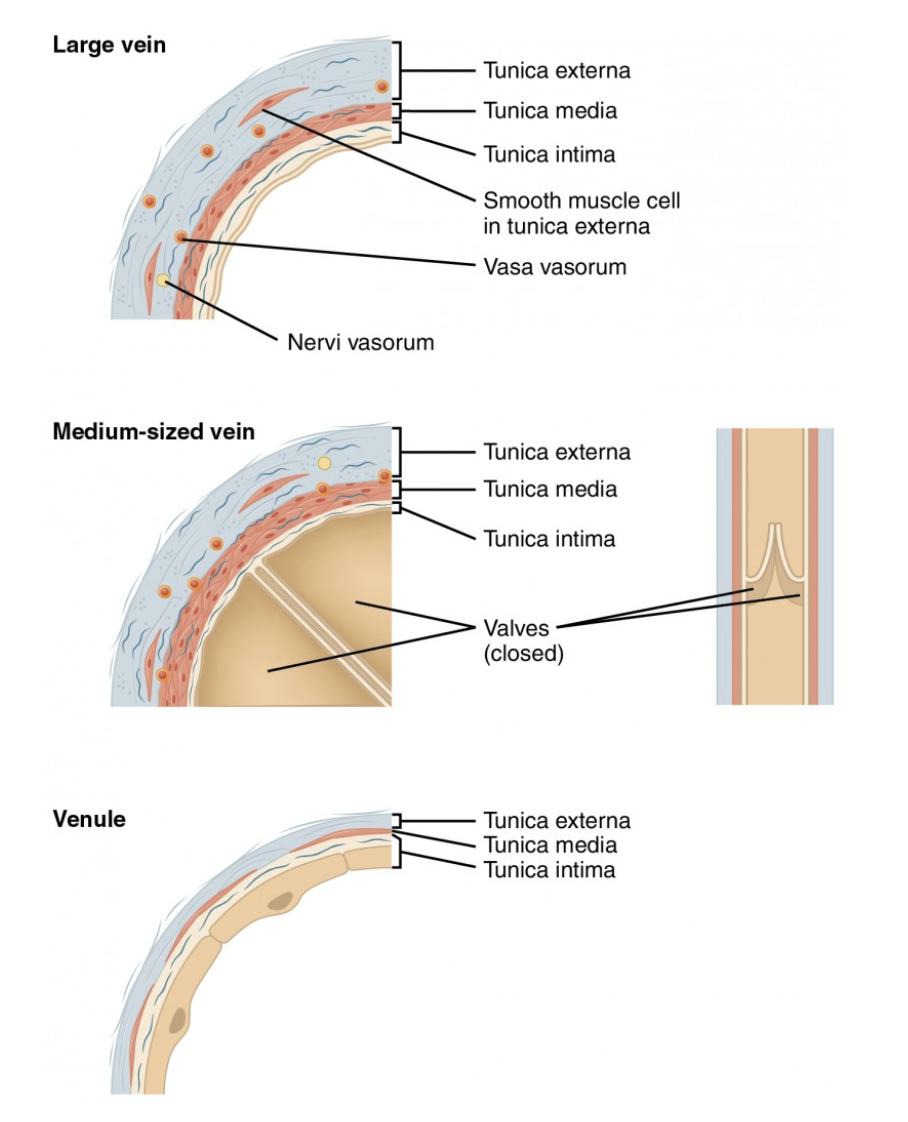
Describe Structure & Function of Veins
STRUCTURE
Formed when venules coverge
Have all tunics, but thinner walls with large lumens compared with corresponding arteries
Tunica media is thin, but tunica externa is thick
Contain collagen fibers and elastic networks
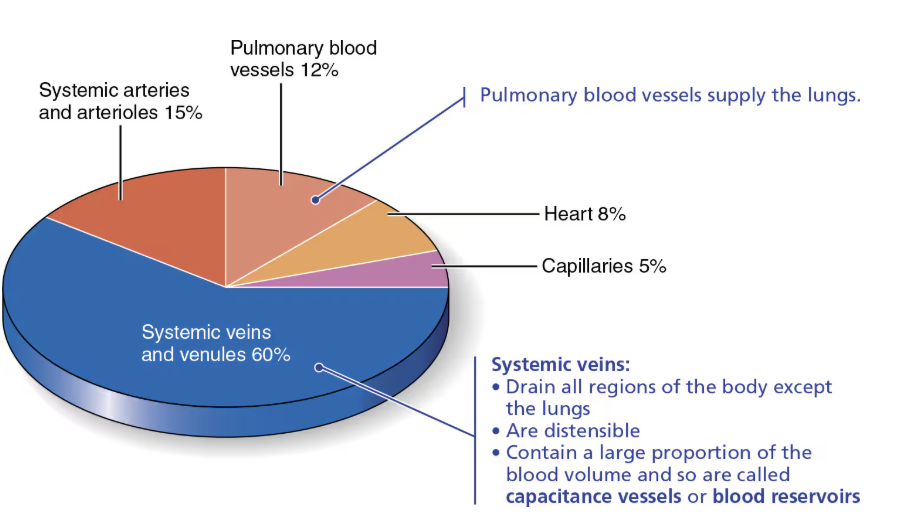
FUNCTION
Large lumen and thin walls make veins good storage vessels → called capacitance vessels (blood reserviors) because they contain up 65% of blood supply
Relative proportion of blood volume throughout the cardiovascular system.
Summary of Veins
T/F: BP lower in arteries
→ TRUE
BP lower in arteries so adaptations ensure return of blood to heart
Large-diameter lumens offer little resistance
Explain Effect and Causes Varicose Veins
EFFECT
Dilated and painful veins due to incompetent (leaky) vavles
CAUSE
Factors that contribute include heredity and conditions that hinder venous return
Prolonged standing, obestity, pregancy
Elevated venous pressure
Straining to deliver a baby or have movement raises intra-abdominal pressure → resulting varicosities in anal veins called hemorrhoids

SUMMARY of Blood Vessel Anatomy
ARTERIES → Directs blood AWAY from the heart
Elastic arteries
Can absorb the most pressure
Responsible for feeling of pulse
Most suited to expanding and recoiling in response to the ejection of blood from the
heart
Muscular arteries
With a thick tunica media and abundant smooth muscle
Responsible for feeling of pulse
Vasoconstriction
Arterioles
Directly controls blood flow to capillaries
Vasoconstriction
CAPILLARIES → Regulated by sphicters
Continuous capillaries
Fenestrated capillaries
Sinusoid capillaries
Most permeable
VEINS
Venules
Directly drains blood from capillaries
Veins
Directs blood one way TOWARD the heart using valve
Name and describe the Two Types of Anastomoses
Venous Anastomoses
Special interconnections of blood vessels that provide alternative pathways for blood to reach a given body region
Arterial Anastomoses
Two or more arteries that connect together in order to provide alternative pathways for supplying blood to a given body region
Role of Anastomoses
These anastomoses provide alternate pathways, called collateral channels, for blood to reach a given body region
Location of the Two Types of Anastomoses
Venous Anastomoses
Abundant
Skin dorsum of hand
Arterial Anastomoses
Around joints where active movement may hinder blood flow
Abdominal organs
Heart
Brain
Arteries that supply the retina, kidneys, and spleen either DO NOT have anastomose or have a poorly developed collateral circulation
Metarteriole–thoroughfare channel shunts are example of what?
Arteriovenous anastomoses