Adaptive immunity part 2 - Cell Mediated Components of Adaptive Immunity & Allergy
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
18 Terms
How do antigens trigger B-cells to make antibody?
B-cell receptor comes into contact with the antigen and they interact.
-B-cell receptor is the antibody on the surface of the B cell - that is why through clonal selection a certain B cell will only recognise a certain antigen (it is antibody of the same specificity - IgG)
How does the antigen cause the B-cell to make the antibody? What are the two types of antigen?
- Have two types of antigen
- 1- Thymus-independent antigen = very large made up of lots of different epitopes and bind to several antigen
receptors on B-cell surface crosslinking them = critical matrix = cascade to occur within the B cell = turns B cell
on to produce antibodies
- 2-(Note these are also Thymus-independent antigen just smaller) Non-specific activation with proteins (other subset of receptors which are immunoglubulin in origin e.g. CD79) on the B cell surface that are just a part of
the structure like the alpha and beta chains - these will turn B cells on to make antibodies
What would a good vaccine cause B cells to do?
Direct induction of adaptive cell mediated immunity (B-cell differentiation to memory cells to plasma cells) to allow
pathogen (antigen) to be strong enough to be thymus independent to switch on B cell response to make
antibodies (note: not all antigens are strong enough to do this)
Note: - T-cell induction of plasma cells to make antibody key to vaccination success
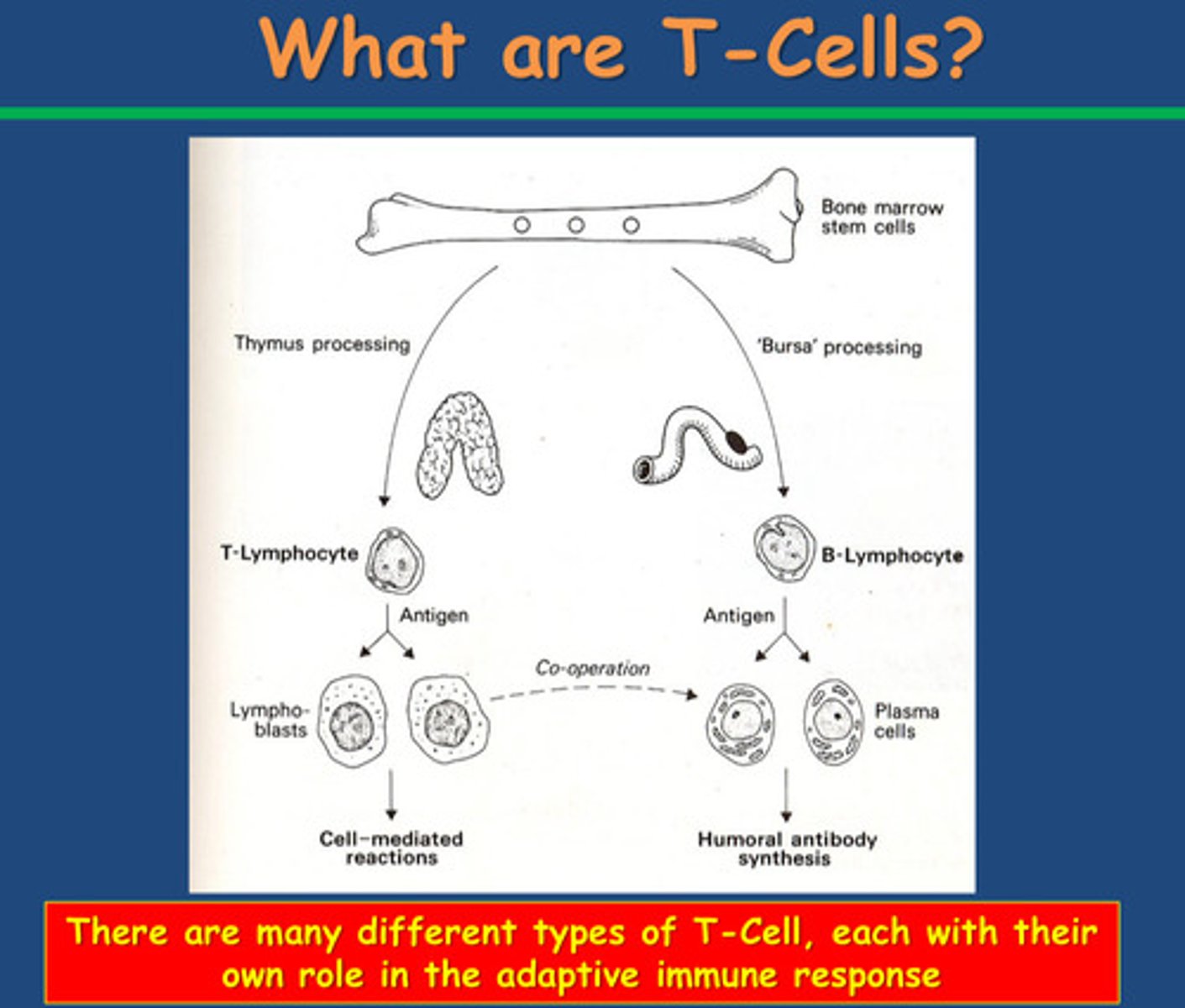
Where do T cells come from?
How do they differentiate and what do they differentiate into?
-The bone marrow also contains the precursors of T cells
-Immature T cells develop in the thymus
-Thymus processing occurs
-T lymphocytes mature and differentiate into two types of cell:
Effector cells and memory cells
What are the 2 important functions of the thymus?
Thymus contains immature T cells and main roles are to give positive
survival signals to immature cells to keep alive and remove cells that
recognise self-cells = auto-immune response
Why are T-cells important?
What are the two type of T cells and what do they do?
-T-Cells help weaker antigens trigger B cells to make antibodies
- T-cells differentiate into effector T cells (Helper T cells (Th) cells are actually a subset of effector T cells) or memory cells
- Effector T cells cooperate with plasma cells to make antibodies
- T-helper cells help trigger B cells to make antibody: Th - T helper cells (aka. T4, CD4+ etc.)
- TH2 (T helper cells type 2) are subset of T helper cells to trigger B cells to release antibodies but antigen must present first - how it works :
- B-cell internalises antigen in phagolysosome and express on surface with MHC II as a complex
- Helper T cell comes and recognises MHC II and antigen and is very specific (cell to cell specificity - only certain clones of TH2 cells will recognise a certain antigen complex of MHC II expressed on the surface of the of the B cell and they will bind through the T cell receptor)
- To strengthen interaction, CD4+ stabilises the bind between the antigen complex of MHC II expressed on the surface of the of the B cell and they will bind through the T cell receptor
- Stimulates T-cell to release cytokines and IL-2,4,5 (interleukins)
- B-cell has IL receptors which then bind = B cell makes antibodies
Note:
- T-cell induction of plasma cells to make antibody key to vaccination success
- Induction of cell mediated immunity in absence of antibody is also key
Relating to T cells - how can we ensure vaccination success
- T-cell induction of plasma cells to make antibody key to vaccination success
- Induction of cell mediated immunity in absence of antibody is also key to amplify the immune response
See below quizlet:
How can we increase the chance that a B cell will come into contact with a T cell?
How can we increase the chance that a B cell will come into contact with a T cell?
-Produce more T cells !!!
How? -Innate immunity communicates with our T cells:
-We have to stimulate the T cells to divide, macrophages cause this.
-Polymorphs and macrophages can phagocytose cells but there will be waste products left over. These present their waste on their surface.
-Our first signal for T cells is the presentation of the antigen complex of MHC II expressed on the surface of the of the B cell which turn on the B cell to produce antibodies as the T cell releases IL-2,4 and 5
-Secondary signal comes from macrophage: Releases IL-1 - stimulate the TH2 molecule to divide and increase its numbers
Note:
-Also TH1 (inflammatory T cells) cells turn on macrophages - they recognise macrophage that are presenting an antigen with a MHII molecule
-This stimulates TH1 cell to release cytokines specifically IFN-gamma (interferon gamma) which will cause macrophage to increase phagocytosis (a way our adaptive immune system can turn on our innate immune system)
-Amplifies the immune response
How can we overcome a particular bacteria that has developed to evade phagocytosis?
-Increase your capacity to phagocytose cells (make it faster)
How:
-TH1 (inflammatory T cells) cells turn on macrophages - they recognise macrophage that are presenting an antigen with a MHII molecule
-This stimulates TH1 cell to release cytokines specifically IFN-gamma (interferon gamma) which will cause macrophage to increase phagocytosis
Functions of TH1 Cells
1. TH1 (inflammatory T cells) cells turn on macrophages - they recognise macrophage that are presenting an antigen with a MHII molecule
-This stimulates TH1 cell to release cytokines specifically IFN-gamma (interferon gamma) which will cause macrophage to increase phagocytosis
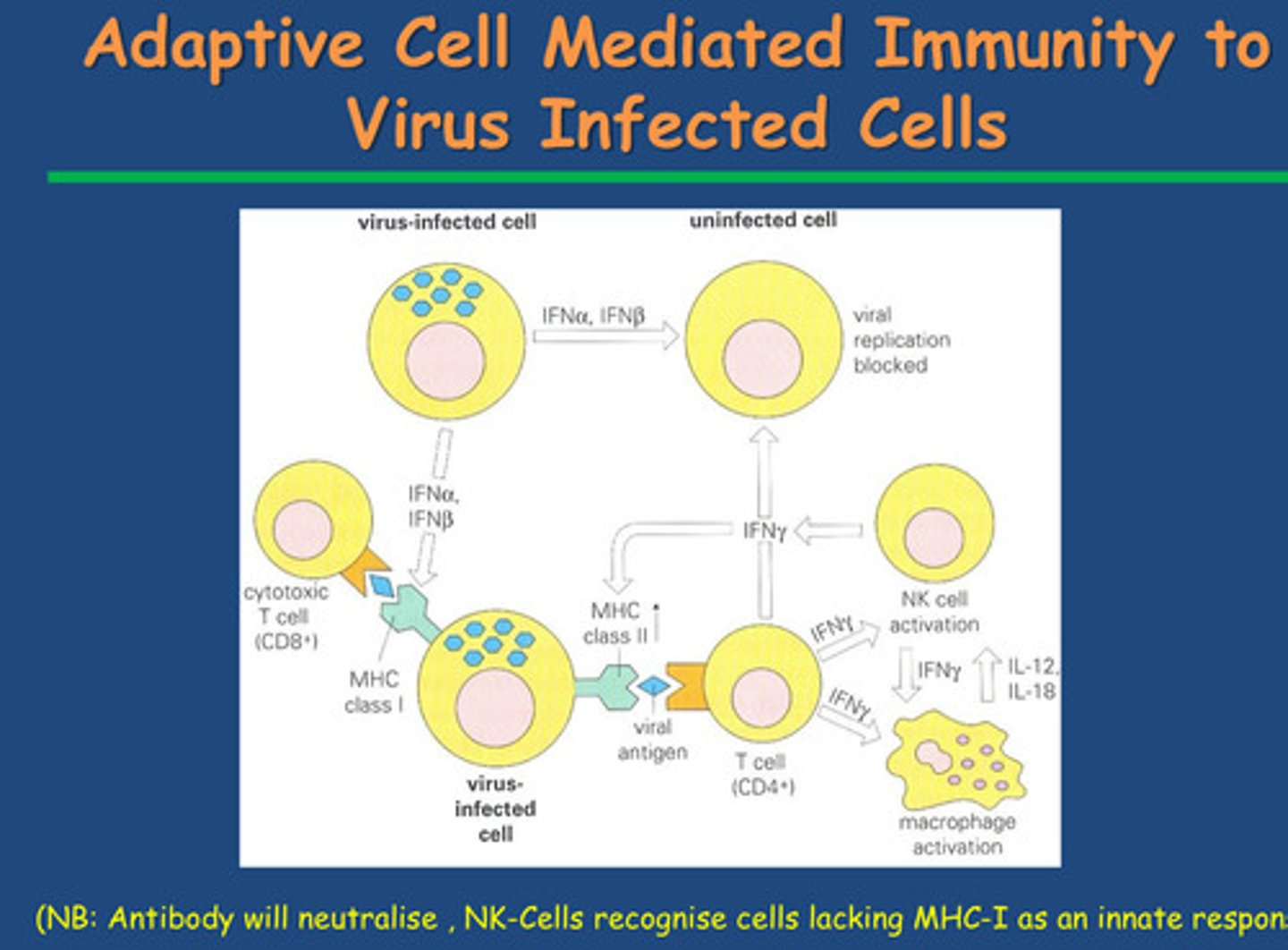
2. Cooperate with Cytotoxic T cells: CD8+ cells aka T8 cells or killer cells
Identification:
Cytotoxic T cells (also called CD8+ T cells) identify infected or abnormal cells by recognizing antigens presented on the cell surface by MHC Class I molecules.
-Activation:
When they encounter an infected or cancerous cell displaying a foreign or abnormal antigen, they become activated.
-Killing Mechanism:
Release Perforin and Granzymes: Cytotoxic T cells release perforin, which creates holes in the target cell's membrane. They also release granzymes, enzymes that enter through these holes and induce the cell to undergo apoptosis (programmed cell death).
Result:
The infected or cancerous cell self-destructs without causing inflammation, helping to contain infection or prevent tumor growth.
Removal:
After killing, cytotoxic T cells detach and move on to find and destroy other infected or abnormal cell
Summary slide of antiviral defences
Note: NK cells (innate immunity) will recognise virally infected cells that aren't expressing MHC molecules at all
Summary: What makes a good vaccine?
-Induction of antibody is key to vaccination success
-Induction of memory cells to provide a secondary antibody response is key to vaccination
-Induction of memory cells to provide a secondary antibody response is key to vaccination success
Key points:
1. Direct induction of adaptive cell mediated immunity (aka differentiation of memory cells to plasma cells) is key to vaccination success
2. T-Cell induction of plasma cells to produce antibody is key to vaccination success
3.Induction of Cell mediated immunity via innate (macrophage) & adaptive (T-helper cells) arms to produce antibody is key to vaccination success
4. Induction of cell mediated immunity (innate arm) in the absence of antibody is also key to vaccination success
5. Induction of cell mediated immunity (adaptive arm) in the absence of antibody is also key to vaccination success
USE SLIDES TO GET INFO
What is hypersensitivity?
- Exaggerated response damaging tissue after 2nd contact with antigen
- Immediate or delayed
What is Type 1 hypersensitivity?
- Anaphylactic
- IgE antibody produced to allergen
- Allergic reaction immediately after second allergen
- B cells stimulated into plasma cells into IgE helped by T cells
- Hereditary predisposition for production
- IgE binds to Fc receptor of mast cells e.g., basophils/eosinophils and
sensitises them
- Second exposure = allergen attaches to IgE of sensitised mast cells =
degranulation = histamine, LT, PG, PAF, ECFA release = muscle
contraction, vasodilation, increased vascular permeability and mucus
secretion = anaphylaxis
- Hayfever rhinitis = atopic allergy
What is Type 2 hypersensitivity?
- Cytotoxic = destroys host cells by lysis or toxic mediators
- IgE or IgM directed against tissue antigens
- Stimulate complement pathway
- Antibodies interact with C1Q by Fc
- Damage mechanisms part of normal processes of immune
- E.g., blood transfusion of different blood group
What is Type 3 (III) hypersensitivity?
- Complex mediated hypersensitivity
- Formation of complexes removed by monocytes usually
- Excess antigens = not removed = accumulate = reaction
- Vasculitis, glomerular nephritis and arthritis and skin
- 1- persistent viral/bacterial/protozoal = chronic complex formation and
deposition in tissues
- 2- continued production of auto antibodies = prolonged complex formation
SLS
- 3- lungs = repeated allergen inhalation
What is Type 4 (IV) hypersensitivity?
- Cell mediated / delayed
- T-cells
- Time required for delayed T cells to migrate and accumulate near
antigens takes a day or more
- Antigens binding to tissues are phagocytosed and presented to receptors on
delayed cell surface
- Antigen and delayed t cell contact = proliferates releasing cytokines
attract lymphocytes, macrophage and basophils = tissue damage
- TB skin test, allergic contact dermatitis, transplantation, cancer
killing
- Tuberculin injected into forearm = tuberculin + response in 8 hrs = red,
hard
- Size of hardness = amount of antigen introduced and degree of
hypersensitivity
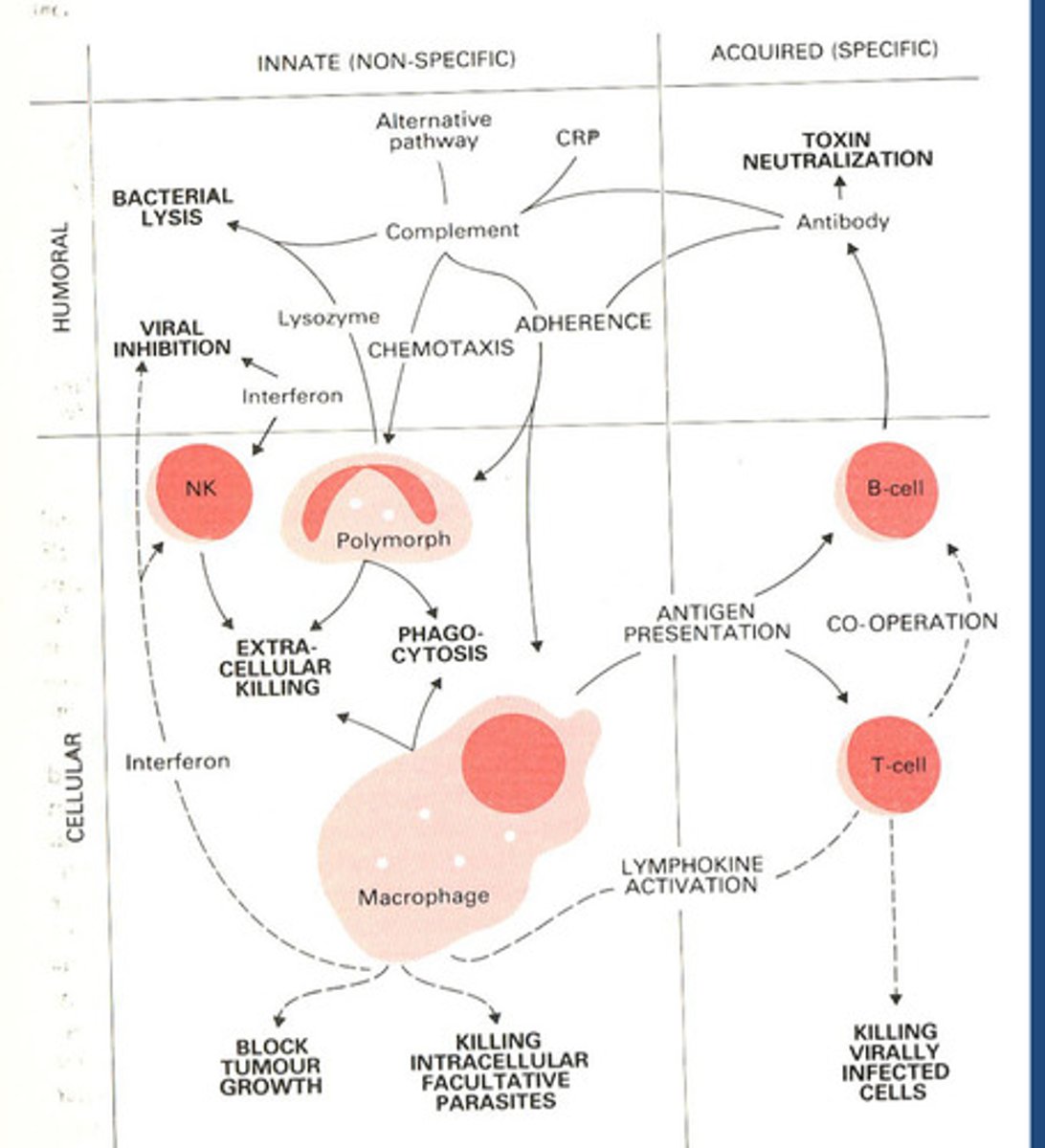
Summary innate and acquired immunity and how they overlap?