kine 326 final #2
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
18 Terms
1. Why is glycolysis activated?
Glycolysis is activated when the demand for ATP increases, such as during exercise, especially high-intensity or anaerobic activity. It provides a rapid source of ATP in the absence of oxygen and also functions in aerobic metabolism by supplying pyruvate for the mitochondria. The pathway is upregulated by:
Low ATP / high ADP or AMP levels
Elevated epinephrine and Ca²⁺, especially in muscle contraction
What happens to the pyruvate?
Fate of pyruvate:
In anaerobic conditions: Pyruvate is reduced to lactate to regenerate NAD⁺, allowing glycolysis to continue.
In aerobic conditions: Pyruvate enters the mitochondria and is converted to acetyl-CoA via pyruvate dehydrogenase, fueling the TCA cycle and oxidative phosphorylation.
2. Blood lactate response to various types of exercise
The blood lactate response reflects the balance between lactate production and clearance:
Low/moderate-intensity exercise: Lactate production is low; clearance matches or exceeds production.
High-intensity exercise: Glycolytic flux increases → lactate production exceeds clearance → blood lactate accumulates.
The point of sharp rise is called the lactate threshold (LT) or onset of blood lactate accumulation (OBLA).
Trained individuals have a higher LT, allowing them to exercise at higher intensities before lactate accumulation impairs performance.
3. ATP yield of glycolysis and why it doesn’t allow sustained ATP supply
From glucose: Net yield = 2 ATP
From glycogen: Net yield = 3 ATP (since it skips the hexokinase step and saves 1 ATP)
Also produces 2 NADH, which can contribute to ATP if O₂ is available (via ETC)
Why it’s not sustainable:
Glycolysis is limited by accumulation of H⁺ ions, which lowers pH and contributes to muscle fatigue.
It’s a short-term energy system, efficient for quick bursts of energy (10s–2min) but inefficient for long-duration activity.
Produces much less ATP per glucose than oxidative phosphorylation (~30–32 ATP), so it's only effective for brief efforts.
1. Where does the carbon that fuels this metabolic pathway (OXIDATIVE PHOSPHORYLATION) come from?
The carbon that fuels oxidative phosphorylation comes from acetyl-CoA, which is derived from:
Pyruvate (from glucose via glycolysis)
Fatty acids (via β-oxidation)
Amino acids (under certain conditions)
Each acetyl-CoA contains 2 carbon atoms, which enter the Krebs cycle and are ultimately released as CO₂ during oxidation.
Define and understand lipolysis,
Lipolysis: The breakdown of triglycerides in adipose or muscle tissue into free fatty acids (FFAs) and glycerol. FFAs enter mitochondria via the carnitine shuttle and undergo β-oxidation to form acetyl-CoA.
Define and understand the Krebs cycle
Krebs Cycle (TCA Cycle): Takes place in the mitochondrial matrix.
plays a key role in aerobic energy production
fully oxidizes acetyl-CoA to generate high-energy electron carriers that feed the electron transport chain for ATP production.
Acetyl-CoA (2C) combines with oxaloacetate (4C) to form citrate (6C). Through a series of steps, it:
Produces 3 NADH, 1 FADH₂, 1 GTP (ATP), and 2 CO₂ per cycle
Runs twice per glucose molecule
Define and understand the electron transport chain (ETC)
Electron Transport Chain (ETC): Located in the inner mitochondrial membrane. NADH and FADH₂ donate electrons, which pass through Complexes I–IV, pumping protons (H⁺) into the intermembrane space. ATP synthase uses this proton gradient to convert ADP + Pi → ATP.
3. What are reducing equivalents and what role do they have in metabolism?
Reducing equivalents are high-energy electron carriers:
Mainly NADH and FADH₂
Produced in:
Glycolysis
Pyruvate dehydrogenase reaction
TCA cycle
β-oxidation
Their role: Deliver electrons to the ETC, enabling oxidative phosphorylation and ATP production.
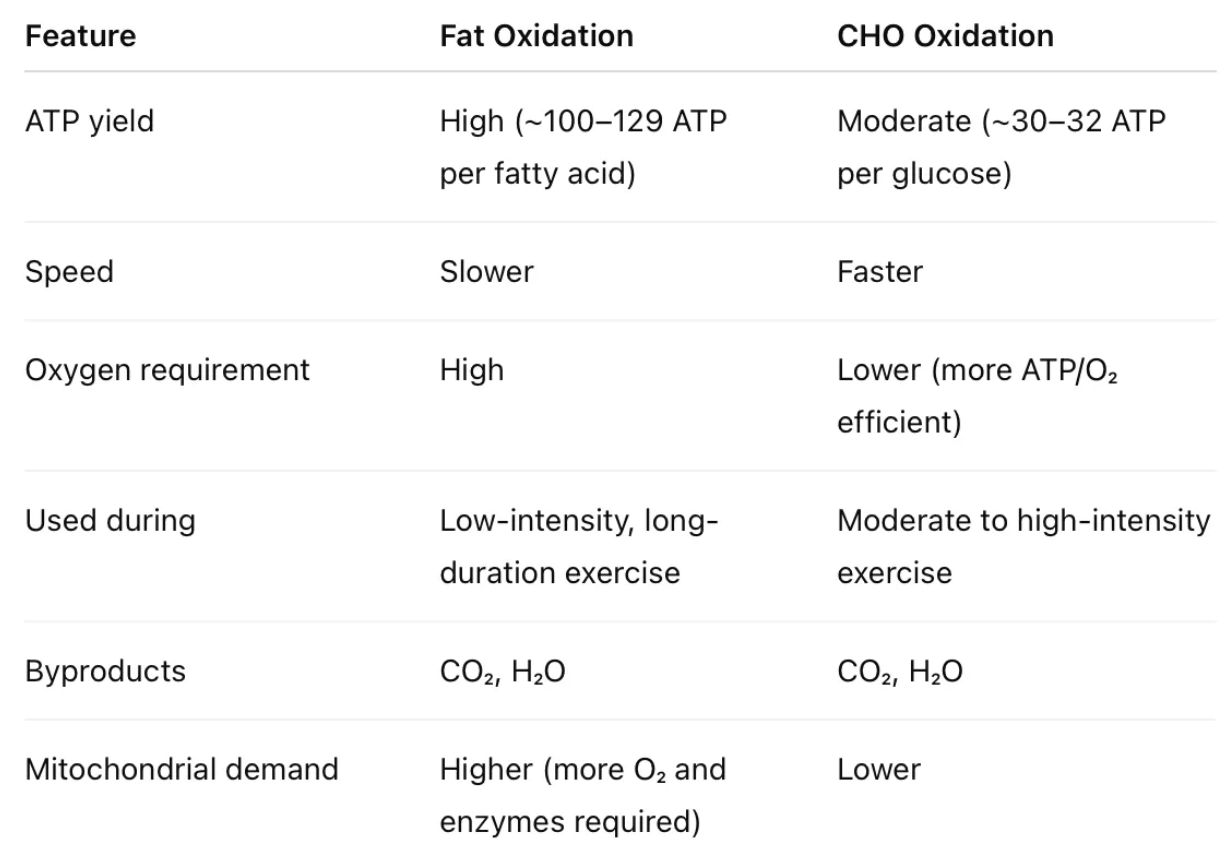
4. Compare and contrast the oxidation of fat and CHO in muscle metabolism
5. How does OXIDATIVE PHOSPHORYLATION metabolic pathway respond to exercise training?
Endurance and interval training lead to:
↑ Mitochondrial density
↑ Enzyme activity (e.g., citrate synthase, cytochrome oxidase)
↑ Fat oxidation capacity (enhanced β-oxidation and reliance on fat at submaximal intensity)
↑ Efficiency of oxygen use
↑ Lactate threshold (delays anaerobic glycolysis reliance)
This allows trained individuals to produce more ATP aerobically, spare glycogen, and delay fatigue.
1. How are the different classes of hormones different, and how does this impact their effects?
Hormones can be grouped into three primary classes, each differing in structure, solubility, and mechanism of action:
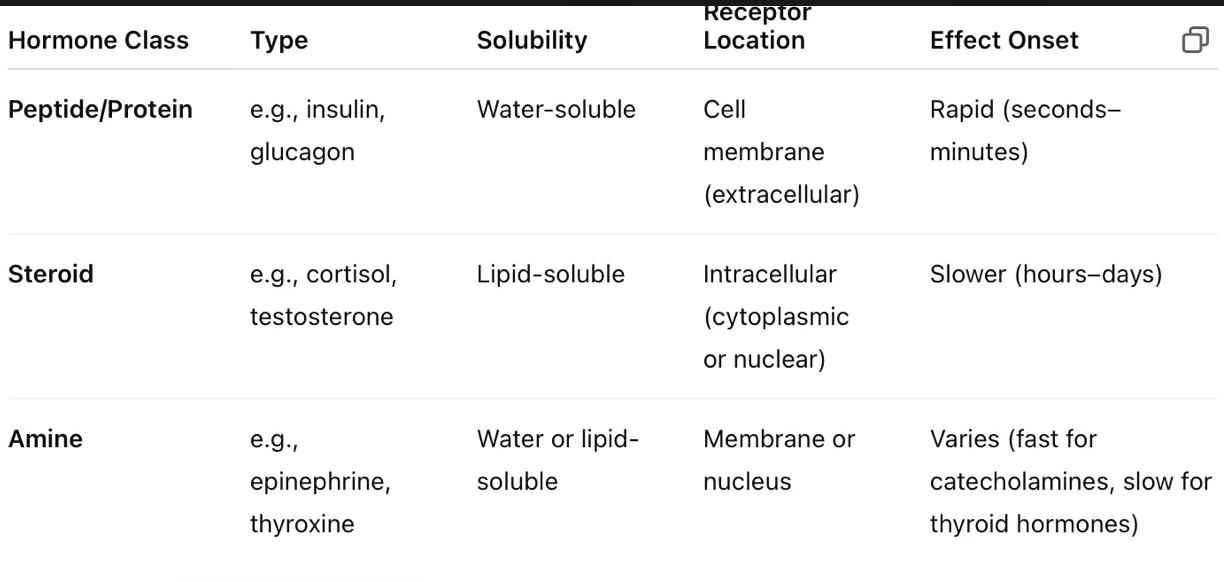
how do the differences in hormones impact their effects?
Impact:
Water-soluble hormones act via second messengers (e.g., cAMP), leading to quick, transient effects.
Lipid-soluble hormones cross membranes, bind nuclear receptors, and alter gene expression, producing slower, longer-lasting effects.
2. Regulation of blood glucose (BG): insulin and glucagon in healthy vs. NIDDM individuals
In healthy adults:
Insulin (from pancreas β-cells): ↓ BG by promoting glucose uptake, glycogen synthesis, and fat storage.
Glucagon (from α-cells): ↑ BG by promoting glycogen breakdown and gluconeogenesis in the liver.
In NIDDM (Type 2 diabetes):
Insulin resistance: Cells don’t respond properly to insulin → impaired glucose uptake.
Pancreas may initially produce more insulin (hyperinsulinemia) but eventually becomes dysfunctional.
Glucagon secretion may be elevated even when BG is high, worsening hyperglycemia.
Result: Poor BG control, especially post-meal, and increased risk for metabolic complications.
3. Regulation of body water and the effects of heat stress
Antidiuretic Hormone (ADH), also called vasopressin, is key to water conservation.
Secreted by the posterior pituitary in response to dehydration or increased blood osmolality.
Promotes water reabsorption in kidneys, reducing urine output.
Aldosterone (from adrenal cortex):
Stimulated by low blood pressure or sodium.
Promotes Na⁺ reabsorption and K⁺ excretion, indirectly conserving water via osmosis.
Under heat stress or prolonged exercise:
Sweating → fluid and electrolyte loss → ↑ plasma osmolality.
ADH and aldosterone levels rise, promoting fluid retention and maintaining blood volume and pressure.
If losses are not replaced, risk of dehydration, heat exhaustion, or heat stroke increases.
hormones to know: pancreatic
Insulin
Secreted in response to high blood glucose (hyperglycemia)
Promotes glucose, amino acid, and fatty acid uptake in skeletal muscle and adipose tissue
Action: Lowers blood glucose
Glucagon
Secreted during low blood glucose (hypoglycemia) and exercise
Promotes glycogenolysis and gluconeogenesis in the liver
Action: Raises blood glucose
hormones to know: Adrenal
Epinephrine (Adrenaline)
Released during stress or intense exercise
Stimulates glycogenolysis, increases heart rate, and supports energy mobilization
Water-soluble: Acts quickly via second messengers like cAMP
Norepinephrine
Supports lipolysis, vasoconstriction, and cardiovascular function during stress/exercise
Also a catecholamine acting rapidly
Cortisol
A steroid hormone released from the adrenal cortex via ACTH
Supports long-term energy availability by promoting gluconeogenesis, protein breakdown, and fat mobilization
Lipid-soluble: Acts slowly by altering gene expression
hormones to know: Anterior Pituitary
Growth Hormone (GH)
Stimulated by exercise and hypoglycemia
Promotes fatty acid mobilization, gluconeogenesis, and conserves blood glucose
Slower-acting with broad metabolic effects