9 - Renal and Digestive Systems
1/101
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
102 Terms
colon
organ that filters out solid waste by reabsorbing water from it → makes feces
liver
organ that filters hydrophilic materials; things that have been absorbed by blood, but too hydrophilic to be absorbed by plasma
kidney
organ that takes plasma out of blood → push it in kidney tubules → modify/filter it
cannot. it can only eliminate hydrophilic waste, such as things eaten, absorbed by blood and dissolved in plasma
if waste products are insoluble in the bloodstream, can it be filtered out by kidney?
regulates BP, ion/water balance, pH
secretes erythropoietin (EPO) to increase RBC production
activates vitamin D
gluconeogenesis (a little bit)
what are some other kidney functions, apart from filtering blood plasma? (4)
erythropoietin (EPO)
a glycoprotein hormone, naturally produced by the peritubular cells of the kidney, that stimulates red blood cell production
colon
liver
kidney
what are the excretory organs? (3)
internal urinary sphincter
structure that sits between the bladder and urethra, made out of smooth muscle (involuntary contraction)
contracts as the bladder fills, relax when bladder empties
external urinary sphincter
structure at the distal urethra, made out of skeletal muscle (voluntary contraction)
relaxes as you pee (you control); normally it stays contracted
contracts, contracts
as the bladder fills, the internal urinary sphincter ___________ (contracts/relaxes) and the external urinary sphincter ___________ (contracts/relaxes).
contraction
voiding urine (not wanting to pee despite needing to) begins with voluntary ______________ (contraction/relaxation) of the external urinary sphincter
contracts, relaxes
when urinating, the external urinary sphincter _________ (contracts/relaxes) to let urine exit. the internal urinary sphincter ____________ (contracts/relaxes) to empty the bladder
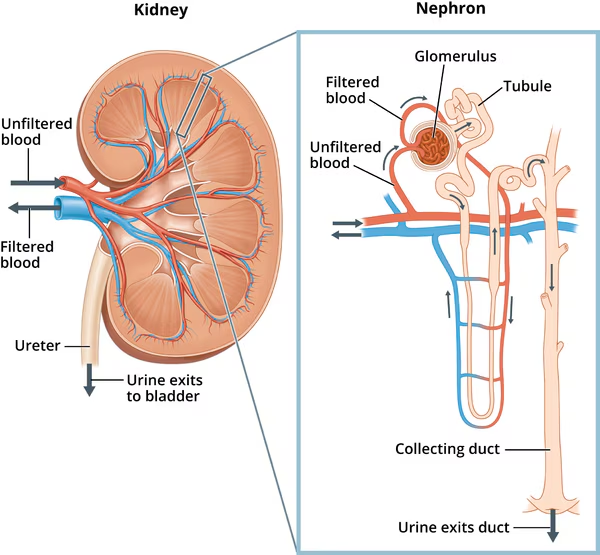
nephron
functional part of the kidney between the cortex and the medulla (where all plasma filtration occurs)
filtration
reabsorption
secretion
what are the 3 processes to which the nephron produces urine?
filtration
the act of the kidney moving a substance (blood plasma) across the membrane (capillary wall) using pressure (BP)
reabsorption
the act of the kidney moving a substrate from blood → filtrate → back to blood (urine to blood again)
glucose, amino acids, water, Na+, HCO3-
what substances are usually reabsorbed by the kidney, given normal conditions?
secretion
the act of the kidneys moving substance away from blood to filtrate (blood → urine) d
drugs, wastes, creatinine, H+, and K+
what substances are usually secreted by the kidneys?
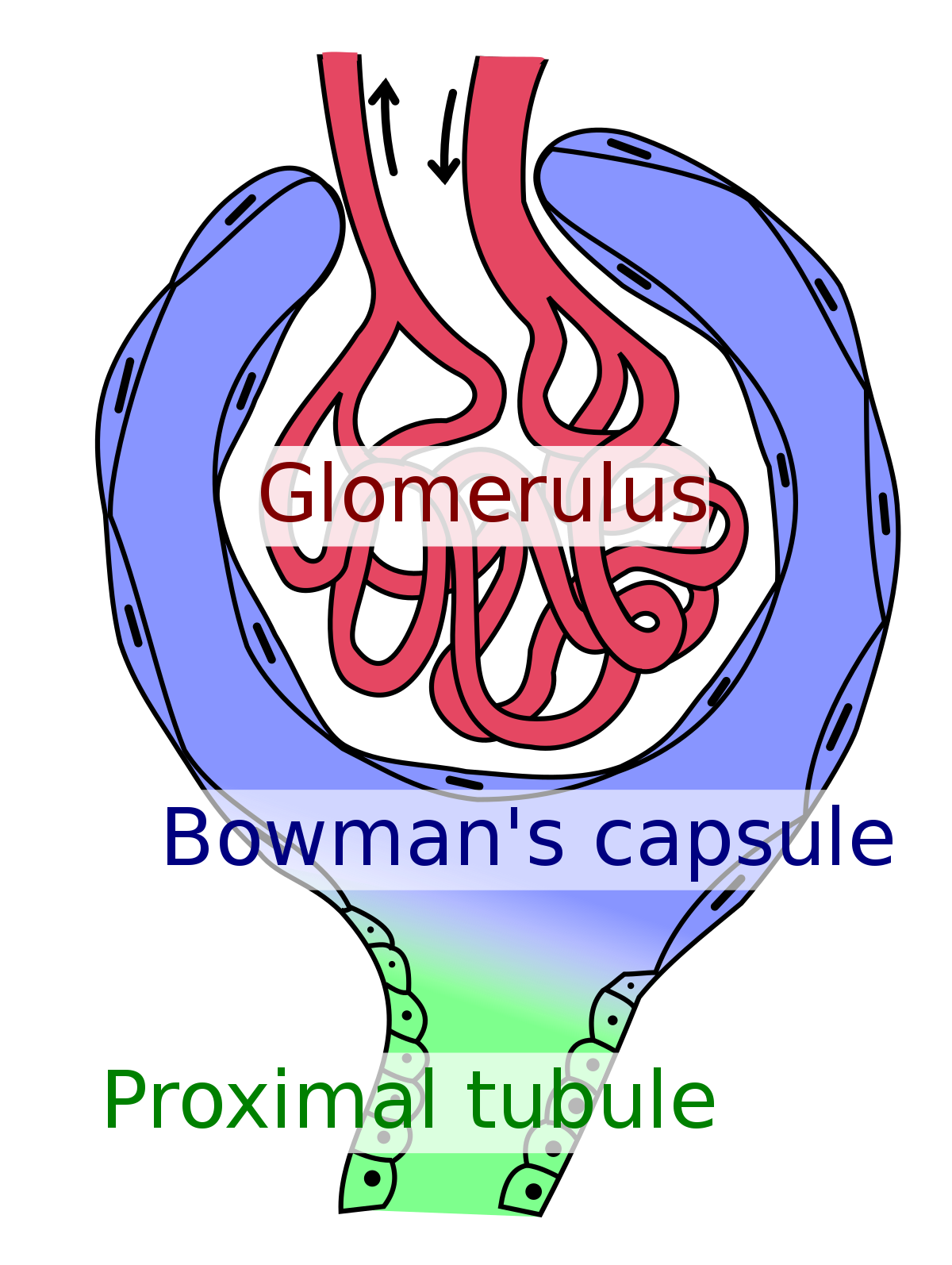
glomerulus
structure in the kidney that contains the capillaries to push plasma out of the bloodstream + does filtration via arterioles
contains afferent and efferent arterioles
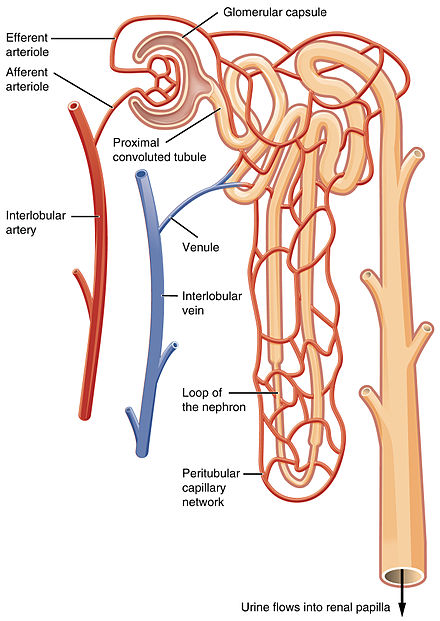
dilate afferent arterioles (let blood in nephron) and constrict efferent arterioles (let blood out)
how to increase GFR (glomerular filtration rate by modifying afferent and efferent arteriole? (should they be constricted/dilated?
proximal convoluted tubule
kidney structure where most reabsorption (Na+, glucose, water) and secretion (H+, K+, creatinine, waste) occurs
microvilli. it’s not regulated babes <3
what does the proximal convoluted tubule reabsorb materials with? how is this regulated?
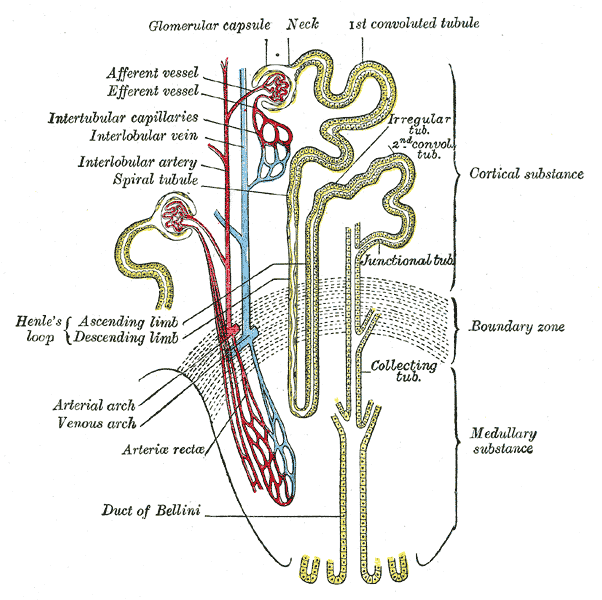
loop of henle
kidney structure that sets up a concentration gradient in the medulla so that the deeper portions of medulla is increasingly salty (increasing osmolarity)
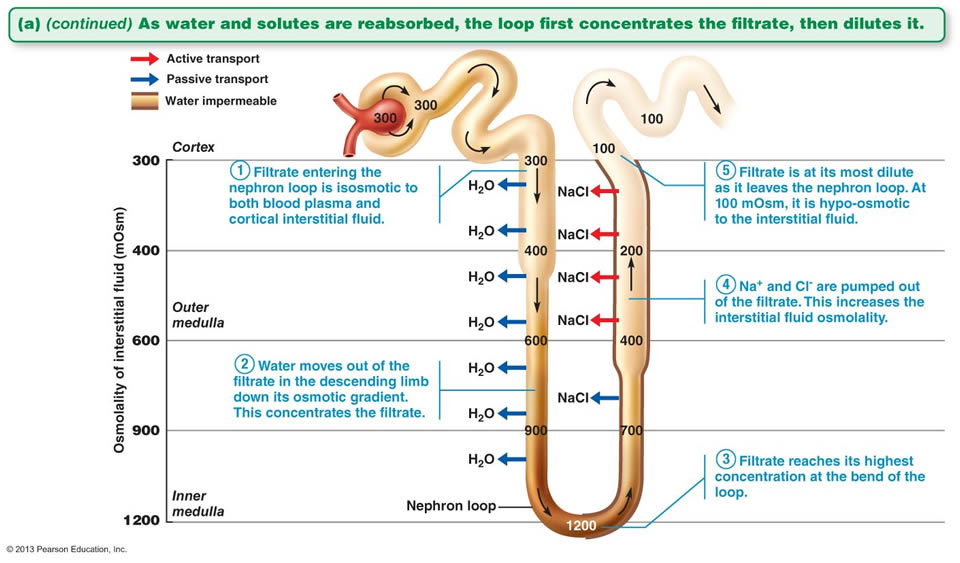
ascending loop of henle
kidney structure that’s impermeable to water, but permeable to salt (Na+ leaves (active transport) but water can’t follow)
descending loop of Henle
kidney structure that is permeable to water, but impermeable to salt
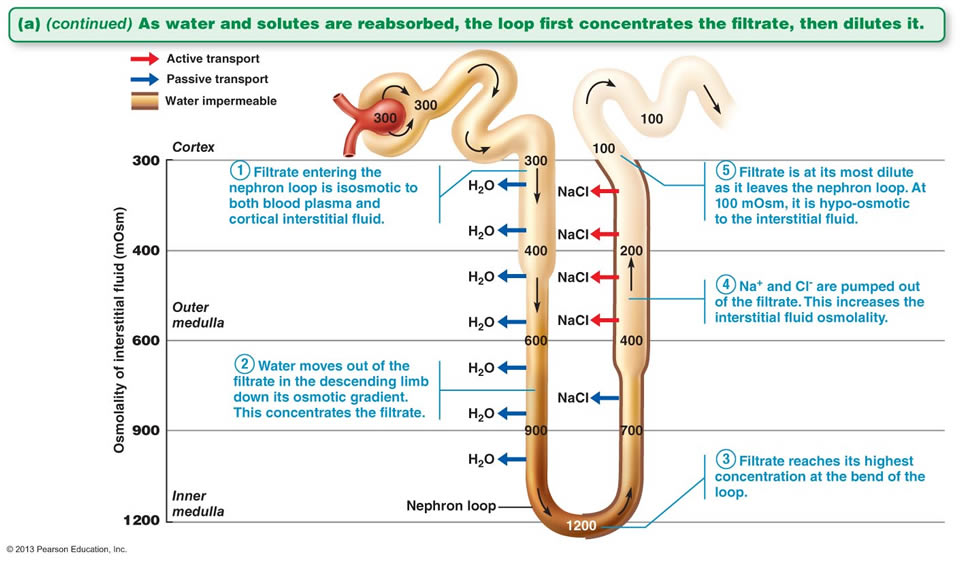
filtrate entering nephron loop is isosmotic to both blood, plasma, and cortical interstitial fluid
water leaves in descending LoH down its osmotic gradient (this concentrates the filtrate)
filtrate reaches the highest concentration at the bend of the loop of henle
Na+ and Cl- are pumped out of the filtrate at ascending LoH → increases the interstitial fluid osmolality
filtrate is at its most dilute as it leaves the nephron loop.
what are the steps of filtrate traveling through the kidney loop of henle?
distal convoluted tubule
kidney structure that’s a specialized reabsorption/secretion center (where aldosterone (Na+ retention), PTH (Ca2+ retention), and calcitonin (Ca2+ secretion) have effects
more selective than its proximal counterpart
collecting duct
kidney structure that picks up water from many different nephrons to perform regulated water reabsorption
has variable permeability to water based on the presence of ADH (water reabsorption)
antidiuretic hormone (ADH)
hormone that allow water to move OUT of the collecting tube to surrounding areas (water is kept)
there woul be no water permeability → water stays in the collecting duct and gets peed out
what happens if there is no antidiuretic hormone (ADH)?
alcohol and coffee. individual pees more because there is no water retention in kidneys
what substances suppress ADH? what happens if that occurs?
hypotension and dehydration. the kidneys retain fluid by reabsorbing water
what conditions/substances activates ADH? what happens if that occurs?
high, high
when urine volume is low, blood volume is _______ (high/low), and blood concentration is ______ (high/low)
low
when urine volume is high, urine concentration is _____ (high/low)
high
when blood volume is low, blood concentration is ______ (high/low)
remember
urine and blood = opposite
volume and osmolarity = opposite
remember
urine and blood = opposite
volume and osmolarity = opposite
systemic vasoconstriction
sodium and potassium reabsorption
ADH secretion (water reabsorption)
increase blood volume and BP
what does aldosterone do?
B.
that’s ADH function
which of these is not a function of aldosterone?
A. vasoconstriction
B. water retention
C. Na+ retention
D. increase blood osmolarity
juxtaglomerular apparatus (JGA)
the contact point between the afferent arteriole and distal convoluted tube
baroreceptors (monitor blood pressure)
JGA cells on the afferent arteriole side act as ______________
JGA cells release renin
what does JGA cells do in cases of hypotension?
angiotensinogen → angiotensin I (by renin) → angiotensin II (by ACE) → aldosterone → systemic vasoconstriction
describe the RAAS system, starting with angiotensinogen and ending with aldosterone
kidney. converts angiotensinogen to angiotensin I in the kidney
where is the enzyme renin secreted from? what is its function?
lungs (endothelial cells). converts angiotensin I to angiotensin II
where is the enzyme ACE released from and what is its function?
chemoreceptors (monitor filtrate osmolarity)
JGA cells on distal convoluted tube act as ______________
stimulate afferent arteriole to release renin
directly dilate the afferent arteriole → increase GFR → more blood in kidney
what do JGA cells on distal convoluted tube do when filtrate osmolarity decrease?
atrial natriuretic peptide (ANP/ANF)
peptide that inhibits renin and aldosterone → vasodilation, decrease Na+ reabsorption → less osmolarity and blood volume → BP lowers
high BP → atria stretch → R atrium releases ANP → vasodilation, inhibition of renin, inhibition of aldosterone
what is the process of high blood pressure regulation in the body?
CO2 + H2O ⇆ H2CO3 + H+ + HCO3-
HCO3- = blood reabsorbed
H+ are secreted (urine - pH of 6)
what is the chemical formula for kidney pH regulation?
CO2 + H2O ⇆ H2CO3 + H+ + HCO3-
[HCO3-] reabsorption increase, [H+] secretion increase
what happens to the renal pH regulation chemical formula when blood pH is too low (acidic)?
CO2 + H2O ⇆ H2CO3 + H+ + HCO3-
[HCO3-] reabsorption decrease, [H+] secretion decrease
what happens to the renal pH regulation chemical formula when blood pH is too high (basic)?
accessory organs
digestive organs with a role, but it’s not part of the alimentary canal
gallbladder
liver
pancreas
salivary glands
name the digestive accessory organs (4)
alimentary canal
muscular tube that goes from the mouth to anus
liver
responsible for:
glucose metabolism (gluconeogenesis, glycolysis, glycogen storage, glycogenolysis)
makes bile
protein regulation (ketogenesis)
toxin breakdown
makes blood clotting protein
lipid metabolism (beta oxidation)
triglyceride synthesis and storage (lipogenesis)
bile
amphipathic molecule that emulsifies fat for easier breakdown (does NOT directly breakdown fat)
gallbladder
digestive organ that concentrates and stores bile
pancreas
digestive organ with endocrine and exocrine role (makes insulin and glucagon)
also makes proteases, lipases, amylases, nucleases (breakdown nucleic acids)
synthesize:
protease
lipase
amylase
nuclease (breakdown nucleic acids)
saliva is NOT the only thing producing amylase!!!!
what are the exocrine functions of the pancreas?
reminder: exocrine means glands that secrete substances through ducts directly (does not secrete into bloodstream)
secretes:
insulin (high glucose)
glucagon (low glucose)
what are the endocrine functions of pancreas?
reminder: endocrine = secrete into bloodstream
endocrine functions (secretes insulin and glucagon)
exocrine functions (synthesize proteases, lipases, amylases, nucleases)
dumps bicarbonate onto things exiting stomach → intestines to neutralize the acidic environment of stomach
what are the 3 functions of the pancreas?
dumps bicarbonate onto things exiting stomach → intestines to neutralize the acidic environment of stomach
why does the pancreas secrete bicarbonate into things exiting the stomach?
lysozyme
amylase
lingual lipase
what are the exocrine enzymes secreted by the mouth/saliva?
lysozyme
enzyme that kills bacteria
amylase
enzyme that digests starch
lingual lipase
enzyme that digests fat
esophagus
muscular tube that brings food into stomach (starts as skeletal muscle, then become smooth muscle)
cardiac sphincter
located at the bottom of the esophagus to prevent reflux of stomach contents
pyloric sphincter
located in the stomach and controls the entry of food into the small intestine
stomach
digestive organ that has very little digestion, absorption. acts as a storage tank for food and secretes acids
gastric glands
located in the stomach, has mucus, parietal cells, and chief cells
parietal cells
in the gastric glands of the stomach and responsible for HCl secretion
chief cells
in the gastric glands of the stomach and responsible for pepsinogen secretion (protease that breakdown pepsin)
pepsinogen
protease that breakdown pepsin in the stomach
parietal cells (secrete HCl)
chief cells (secrete pepsinogen)
what are the exocrine functions of the stomach
G cells (secrete gastrin)
what are the endocrine functions of the stomach?
G cells
located in the stomach and responsible for gastrin secretion (activates gastric glands to secrete gastric acid)
gastrin
hormone produced by G cells in the stomach responsible for regulation of the secretion of gastric acid
duodenum
jejunum
ileum
what are the 3 portions of the small intestine
small intestine
digestive organ where ALL digestive and reabsorption occurs
has a huge surface area due to villi and microvilli folds (plicae = the folds)
plicae
the folds of villi and microvilli in the intestine
enterokinase making enteropeptidase (cleaves off part of trypsinogen → activate trypsin → chain rxn of enzyme activation
brush border enzymes (disaccharidases and dipeptidases are activated)
what are the exocrine functions of the small intestine?
enteropeptidase
enzyme made by enterokinase to cleave off part of trypsinogen → activates trypsin → sets off chain reaction of enzyme activation
brush border enzymes
include disaccharidases and dipeptidases
disaccharidases
enzymes that split disaccharides into 2 monomers for adsorption in the small intestine
dipeptidases
enzyme that splits dipeptides into 2 monomers for adsorption in the small intestine
adsorption
process by which molecules or particles from a gas, liquid, or dissolved solid adhere to a surface.
it is different from absorption (penetration of one substance into the bulk of another)
enterogastrone (reduce stomach motility and emptying)
CCK (increase bile/pancreatic enzyme release
secretin (increase bicarbonate release from pancreas
what are the endocrine functions in the small intestine?
CCK
peptide hormone produced by cells lining the duodenum and jejunum to increase bile/pancreatic enzyme release
triggered by fats and proteins in the intestines
presence of fats and proteins in the intestine
what triggers CCK release in small intestine?
secretin
peptide hormone made by S cells in duodenum to increase bicarbonate release from pancreas
it’s triggered by low pH in the intestine
low pH in the intestine
what triggers the secretin secretion in the small intestine?
large intestine
digestive organ where no digestion/absorption occurs, but water reabsorption and feces storage happen
gives immunity, vision, reproduction, growth, and development
vitamin A function
infections, maternal mortality, blindness
what happens if vitamin A is missing from diet?
help body absorb and retain calcium
vitamin D function
loss in bone density → osteroporosis and fractures
what happens if vitamin D is missing from the body?
helps with blood clotting
vitamin K function
uncontrolled bleeding, osteroporosis, risk of CVD
What happens if vitamin K is missing from the body?