Cell membrane
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
What makes the ECF, include moth main and sub divisions.
Interstitial fluid (between cells), Intravascular fluid (blood, plasma, lymph), and Tran cellular (stomach, CSF)
What is the function of having a fluid membrane?
Maintains ECF and ICF
Regulation of molecules
Communication
Structure
3 type of proteins found in a memebrane
Integral, peripheral, and lipid anchored.
What are the types of membrane channels and how to distuinish between them?
Channels, pores, carriers, and pumps
Pores: Always open
Pumps: Use ATP
Channels: driven via conc gradients and electric membrane gradient.
Carriers: Only open to one side and dependent on target concentration.
What does Ficks Law apply to and why does it only work at low solute concentrations?
Flicks law pertains to the flux induced by non electrolyte species. This only applies at low concentration since it approaches Vmax as carrier proteins are occupied (like an enzyme).
Directly proportional to the surface areas, permeability, and concentration gradient of solutes.
What are the triggers for ion gated transport?
Ion gated channels can ligand, mechanical, temperature, or voltage dependent. Can either open or close the channels.
What is an example of facilitated transport? Can this be against a concentration gradient?
Carrier proteins are an example of facilitated transport. GLUT transported use this to be able to transport glucose.
Only one side open at a time and movement is dependent on amount of carrier molecules and concentration gradient of solutes.
Has a binding site specifically for the target molecule.
Much slower than ion or pores channels.
What is the difference between facilitated carrier diffusion and ion transport? Relate to a graph.
Facilitated carriers have a Vmax they approach as saturation of the carrier molecules with their target is approached.
Since ion channel do not depend on a limited carrier protein, then they will have a constant rate of diffusion.
What are some types of active transport?
Na/K ATPase, Ca ATPase, H/K ATPase
What is secondary active transport? What drives this process?
This is when ATP is not directly used but rather used to establish a concentration gradient. Through this gradient then we can couple the transport of molecules using this energy. This can be done through symport or anti port means.
If SGLT is deficient in Na gradient then what happens? Where is SGLT found?
Na drives the movement of glucose via SGLT, thus the transport will decrease if no concentration gradient is established.
SGLT is found in the kidney and intestinal epithelium for glucose transport.
How can we alter cell permibiltity with membrane proteins>
We can change them ie conformational change or we can degrade them.
If something is going through the paracellular route then what forces is it driven by?
The paracellular route is between the cells thus will be depends on the osmotic and hydrostatic pressure of the surround fluid
What is an example of trans cellular transporter?
trans cellular is within a cell thus will use channels such as aquaporins.
What is the term used for both glycolipids, and glycoproteins? What are these used in ?
Glycocalyx; used for call recognition
Describes how the protein to lipid ratio can change as we go from he mitochondria to the myelin sheaths?
Mitochondria will need more proteins for transportation and myelin sheets will need more lipid for their inusltative qualities.
What are the derivatives of arachindonic acid? What do we think when we see these). What are these made from originally.
Eicosanoid synthesis can make Leukotrines, prostaglandins, prostacyclins, and thromboxanes.
We think inflammation when we see these
Lipids act as resivoirs of signaling molecules as we see above.
Name all the polar heads in phospholipids
Choline, serine, ethanoamine, inositol, glycerol
What is the composition of phospholipids?
Glycerol, FA (C1 or 2), phosphoric acid (C3), polar head (to phosphoric acid)
What is the difference between he backbone of sphinogolipids and phospholipids
Sphingolipids - sphingosine
Phospholipids - glycerol
What phospholipids does choline make?
Dipalmitoylphophatidlcholine
Lecithin:sphingomyelin - indicator for fetal lung maturity (>2 is good)
Surfactant
What phospholipid does ethanolamine? What is the pathogenesis?
Phosphatidylethanolamine , inner leaflet, plasmalogens
Ex: rhizomelic chondrodysplasia punctata(RCDP)
Symptoms: skeletal abn, facial features, retardation, resp issues
What phospholipid does serine make? What pathway can we see this in and thus where can we find this?
Phosphatidylserine is made, usually in inner leaf let but externatized when a apoptosis signal is sent —>detected via Annexin V assay
What phospholipid does inositol make
Phosphatidlinositol , req for synthesis of 2nd messanger ie PIP2
Cleaved by phospholipase C into DAG and IP3 signal molecules.
What type of phospholipid does glycerol make?
Phosphotidylglycerol, pulmonary surfactant ie avoioli will stick together, also used for fetal lung development
If a patient is unable too make the cis configuration of unsaturated fatty acids, what will we see?
We will decreased membrane fluidity thus inhibiting memebrane transport.
Where are sphingolipids degraded?
In the lysosome
Cholesterol is in what 2 forms in the body?
Can be in the free form or esterffied with FA side chain of a phospholipid —→cholesterol esterase+ completely hydrophobic
What makes cholesterol and what things can cholesterol make?
Acetylcholine Coa is make into cholesterol.
Cholesterol makes membranes, bile salts, and steroid hormones,
What is an example of a ether glycerolipid?
Plasmogens
What proteins do prions bind to
Lipid binded proteins
What are 2 examples of transporters which present as a disease?
Ex1: RBC transport proteins —→Spectrin, band3, ankyrin (usually allow for flexibility of RBCs)
Without these we will see overly rigid blood cells and hemolysis(Armenia)
Caused by SPHEREPCYTOSIS
Ex2: Defificeny in GLUT 1 —> decreased glucose in CSF —>seizures and mental retardation
What is an example of a channel mutation which presents as a disease?
Mutations in the CFTR caused CF —> via disrupted Cl channels.
What is an example of peripheral proteins?
Non covalently bound, examples include reg subunits of ion channels, cyc c, and Falvoproteins
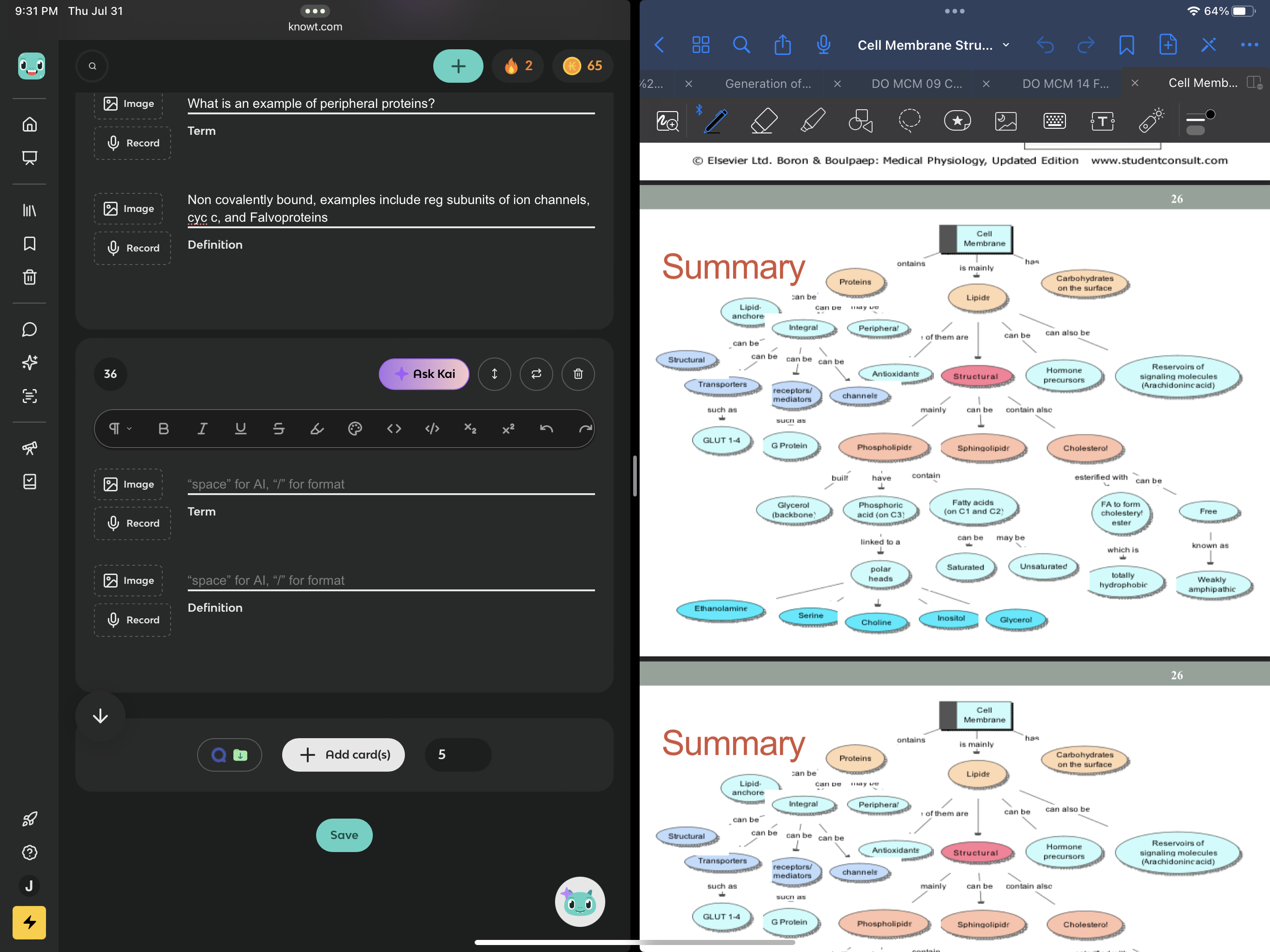
Visualize a map for the interconnected topics
'