Integumentary
1/125
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
126 Terms
What percentage of body weight is made up by the skin?
20% of body weight.
What is the primary function of the skin?
Protection.
What does the skin protect the body from?
Micro-organisms, UV radiation, body fluid loss, and mechanical stress.
How does the skin help regulate body temperature?
Through sweating and adjusting blood flow to the skin.
What role does the skin play in immune surveillance?
The skin detects and responds to pathogens and foreign substances.
How does the skin contribute to Vitamin D activation?
The skin activates vitamin D when exposed to UV radiation.
What sensory functions are provided by the skin?
Touch and pressure receptors.
What role do commensal micro-organisms play in the skin?
They help protect the skin from harmful pathogens and maintain skin health.
What are pressure injuries?
Ischemic lesions on dependent areas, usually on bony prominences, caused by prolonged pressure.
What is the appearance of a Stage I pressure injury?
Red, intact skin.
What is the appearance of a Stage II pressure injury?
Skin damage, such as partial-thickness loss of dermis.
What characterizes a Stage III pressure injury?
An ulcerating crater with full-thickness loss of tissue.
What is seen in a Stage IV pressure injury?
Exposed tendon, bone, or muscle.
What causes ischemia in pressure injuries?
Unrelieved pressure that distorts capillaries, microthrombi that occlude blood supply, shearing forces, friction, and moisture.
What characterizes a Stage I pressure injury?
Nonblanchable erythema of intact skin.
What is the appearance of a Stage II pressure injury?
Partial thickness loss, such as erosion or blister.
What does a Stage III pressure injury involve?
Full-thickness loss that can involve subcutaneous tissue, extending to, but not through, underlying fascia.
What defines a Stage IV pressure injury?
Full-thickness loss with exposure of muscle, bone, or supporting structures like tendons. Can also involve tunneling.
What is a keloid?
A type of scar overgrowth where the scar extends beyond the original site of injury.
Who is most commonly affected by keloids?
Typically dark-skinned individuals.
What causes the formation of keloids?
Excessive fibroblast activity and collagen formation.
overgrowth of a scar
When do keloids typically grow?
They grow within 1 year of skin damage.
What is the appearance of a keloid?
A claw-like appearance on flat surfaces.
What do the terms eczema and dermatitis describe?
They describe inflammatory responses to the skin and are often used interchangeably.
What are common characteristics of eczema and dermatitis?
Itching, lesions, skin changes, crusting, oozing, and chronic skin alteration.
What type of hypersensitivity reaction is commonly associated with Allergic Contact Dermatitis?
A T cell-mediated hypersensitivity reaction (Type IV).
Allergic contact dermatitis: caused by an allergic reaction to something the skin touches (e.g., poison ivy, nickel).
What factors contribute to Allergic Contact Dermatitis?
Interaction of skin barrier function, reaction to irritants, and genetic susceptibility.
What are some examples of allergens that cause Allergic Contact Dermatitis?
Poison Ivy and latex allergy.
eyelashes
How does Irritant Contact Dermatitis differ from Allergic Contact Dermatitis?
Irritant Contact Dermatitis involves innate immunity activated by proinflammatory properties of substances, unlike the T cell-mediated response in allergic contact dermatitis.
What are some examples of substances that can cause Irritant Contact Dermatitis?
Detergents and industrial cleaners.
Irritant contact dermatitis: caused by a substance that physically damages the skin (e.g., soap, bleach).
Where does Stasis Dermatitis commonly occur?
It commonly affects the lower legs.
What causes Stasis Dermatitis?
It is caused by chronic venous stasis and edema.
What happens during Stasis Dermatitis due to blood pooling?
Pooling of blood traps neutrophils, leading to erythema and itching.
What are the later stages of Stasis Dermatitis characterized by?
Scales, hyperpigmentation, and lesions.
What is Psoriasis?
An autoimmune skin disease that commonly affects the scalp, skin, and ears.
What is the most common type of Psoriasis?
Plaque psoriasis, also known as psoriasis vulgaris.
When is Psoriasis typically diagnosed?
Around 20 years of age, and it is hereditary.
What causes the rapid turnover of the epidermis in Psoriasis?
A relapsing condition where the epidermis sheds every 3-4 days instead of the usual 14-20 days.
What is the result of rapid epidermal turnover in Psoriasis?
Thickened epidermis that forms white-silver plaques of keratin.
What role do T helper cells play in Psoriasis?
T helper cells secrete cytokines that cause the symptoms of Psoriasis.
What other conditions are Psoriasis sometimes seen in?
It can be seen in persons with IBS, Crohn’s disease, and Rheumatoid arthritis.
What is Acne vulgaris?
An inflammatory disorder of the pilosebaceous unit attached to the hair follicle.
What causes Acne vulgaris during puberty?
Sebaceous glands undergo hypertrophy with increased androgen production.
What is Acne rosacea?
A common condition in middle-aged adults, characterized by chronic inflammation due to an altered innate immune response.
What are the symptoms of Acne rosacea?
Chronic inappropriate vasodilation, causing flushing and sun sensitivity, typically on the middle third of the face.
What is Lupus?
An autoimmune inflammatory systemic disease with skin symptoms.
Where are the most common skin symptoms of Lupus located?
The face, with a butterfly-shaped distribution across the cheeks and nose.
What are some additional symptoms of Lupus?
Alopecia, hives, and Raynaud's phenomenon.
What causes organ damage in Lupus?
Autoimmune complexes, potentially caused by an unknown antigen.
What age and gender group is most commonly affected by Lupus?
Women in their late 30s to 40s.
What type of hypersensitivity reaction is associated with Lupus?
A Type III hypersensitivity reaction.
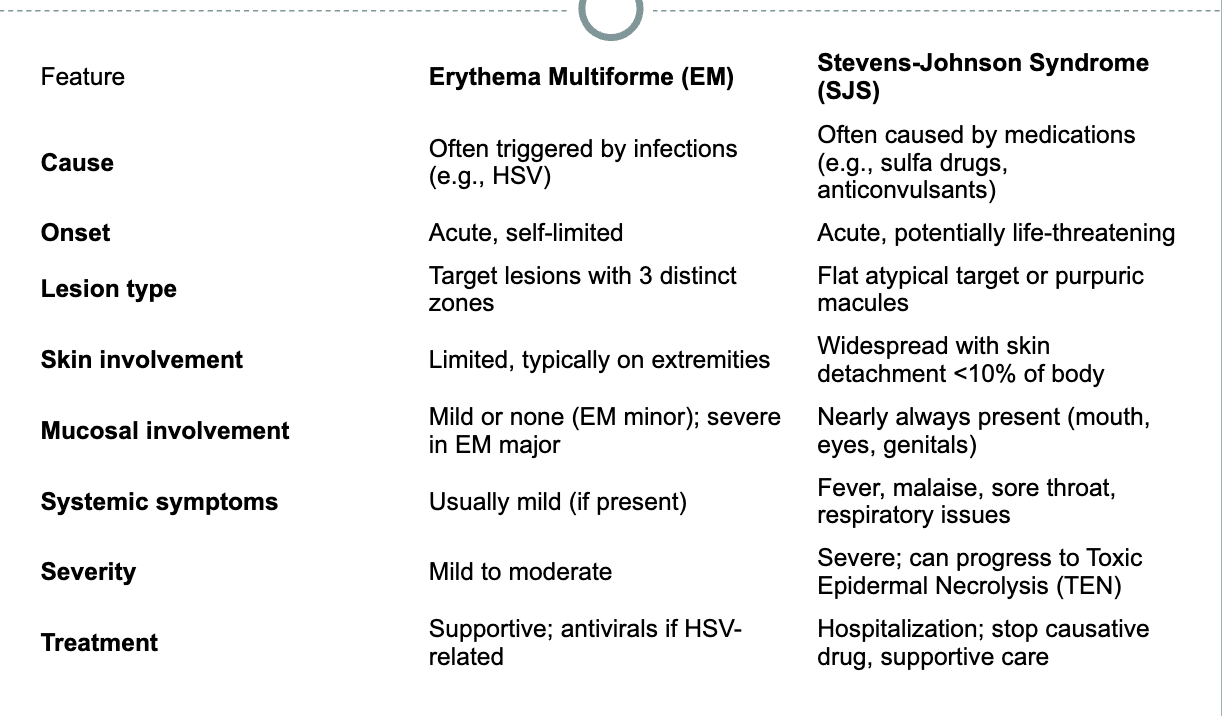
What type of hypersensitivity response is involved in Erythema Multiforme (EM) and Stevens-Johnson Syndrome (SJS)?
Type IV hypersensitivity response to a drug or acquired infection.
What causes Erythema Multiforme (EM)?
Inflammation of the skin and mucous membranes due to an immune response to a drug or microorganism, targeting small blood vessels.
less severe than stevens johnsons
What are the characteristics of the lesions in Erythema Multiforme (EM)?
Edema, vesicles, and bullae form on the skin and mucous membranes, with a "target" lesion shape.
What distinguishes Stevens-Johnson Syndrome (SJS) from Erythema Multiforme (EM)?
SJS involves severe erythematous bullous lesions covering 10% of the body and is considered a medical emergency.
What is the role of the nurse in managing Erythema Multiforme (EM) and Stevens-Johnson Syndrome (SJS)?
Recognize target lesions.
Obtain a medication history (e.g., Penicillin, phenytoin, barbiturates, sulfonamides).
Identify potential infectious causes (e.g., HSV, EBV, Mycoplasma).
Comparison of EM and SJS
You can have EM from drugs as well
What types of bacteria are commonly associated with Bacterial Infections related to Staph and Strep?
Staph (Staphylococcus) and Strep (Streptococcus) bacteria.
What is Folliculitis?
An infection of the hair follicle where bacteria enter through the skin's hair opening.
What is the most common bacterium responsible for Folliculitis?
Staphylococcus aureus.
What is a Furuncle (boil)?
A Furuncle is an infection of the hair follicle where inflammation spreads into the dermis (cellulitis), usually caused by Staphylococcus aureus.
What are the symptoms of a Furuncle (boil)?
A firm, red, painful nodule 1-5 cm in size that may drain pus or necrotic tissue. It is often mistaken for a "spider bite."
What is a Carbuncle?
A Carbuncle is a collection of infected hair follicles, often presenting as a subcutaneous or deep dermis swollen, red, and painful mass.
Where are Carbuncles most commonly located?
The posterior neck, upper back, and lateral thighs.
What is Impetigo?
Impetigo is a superimposed infection that occurs on any skin lesion, typically caused by Staphylococcus aureus or beta-hemolytic Streptococcus.
Who is most commonly affected by Impetigo?
Children are most commonly affected by Impetigo.
What is Cellulitis?
Cellulitis is an infection of the dermis and subcutaneous tissues that can develop following any skin lesion.
What are the symptoms of Cellulitis?
Cellulitis presents as an area of infection that is darker than the surrounding skin, hot to the touch, and swollen.
general term for infection in the skin
What virus causes Measles?
Measles is caused by the Morbilli or rubeola virus, which is a single-stranded RNA virus.
What are the early symptoms of Measles?
The early symptoms of Measles include:
Moderate fever
Cough
Runny nose
Red eyes (conjunctivitis)
Sore throat
What are the later symptoms of Measles?
Later symptoms of Measles include:
Koplik spots (blue-white spots inside the mouth)
Red-brown rash starting at the hairline and spreading down
High fever (can exceed 104°F)
When does the rash appear after exposure to Measles?
The rash usually appears 14 days after exposure to the Measles virus. Some immunocompromised individuals may not develop the rash.
What are some common complications of Measles?
Common complications of Measles include ear infections and diarrhea. Serious complications include pneumonia and encephalitis, especially in children under 5 years of age.
What are the two types of Herpes Simplex Virus (HSV)?
The two types of Herpes Simplex Virus (HSV) are:
HSV-1: Primarily affects the lips, mouth, and eyes.
HSV-2: Primarily affects the genital area.
How is HSV-1 transmitted?
HSV-1 is transmitted through saliva and commonly affects the lips, mouth, and eyes. It can also live latently in the dorsal root ganglion and reactivate through sensory nerve endings.
How is HSV-2 transmitted?
HSV-2 is typically transmitted through mucous membrane contact during viral shedding, and it most commonly affects the genital area. It can also be transmitted vertically (from mother to child).
What viruses cause chickenpox and shingles?
Varicella zoster virus (VZV) causes chickenpox (initial infection) and shingles (reactivation, also called herpes zoster).
Where does the varicella zoster virus remain latent?
It remains latent in the trigeminal and dorsal root ganglia.
it is going to hurt before you see it
What percentage of patients experience postherpetic neuralgia after shingles?
About 20% of patients.
What is the purpose of the zoster vaccine?
To reduce the incidence of shingles and postherpetic pain.
What virus causes warts on the skin and genitals?
Human papillomavirus (HPV).
How is HPV transmitted?
By touch (for skin warts) and sexual contact (for genital warts).
What is verruca vulgaris?
A skin wart caused by HPV.
What is condyloma acuminata?
A genital wart, which is highly contagious and can lead to cancer.
What is another name for fungal infections of the skin?
Mycoses or Tinea (caused by dermatophytes).
What is the most common fungal infection?
Candida albicans.
What are common sites for Candida albicans overgrowth?
Mouth, esophagus, vagina, penis, and skin folds.
What are risk factors for Candida albicans infection?
Moisture, antibiotics, diabetes, pregnancy, steroids, and immunosuppression.
What does Candida albicans look like in the mouth or vagina?
A curd-like white or “cottage cheese” appearance.
What type of hypersensitivity reaction causes urticaria (hives)?
Type I hypersensitivity.
What immune cells and chemicals are involved in urticaria?
B cells, IgE, mast cells, histamine, and prostaglandins.
What are common triggers for urticaria?
Medications, plants, animals, insect bites, or other allergens.
Is urticaria usually acute or chronic?
It can be acute or chronic.
What type of immune reaction can severe insect bites trigger?
Type I hypersensitivity, leading to urticaria or anaphylaxis.
Which insects commonly cause local skin reactions?
Mosquitoes, blood-sucking flies, ants, wasps, hornets, bees, and yellow jackets.
How do stinging insects like bees and wasps cause reactions?
Their stinger implants into the skin and releases venom, triggering a local or systemic response.
What is seborrheic keratosis?
A benign proliferation of cutaneous basal cells.
How does seborrheic keratosis appear?
As flat or slightly elevated lesions that may resemble warts.
When is seborrheic keratosis more common?
It is more common with age.
What is the most common skin cancer in the U.S.?
Basal cell carcinoma.