DSA24/27L - Diarrhea and Constipation
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
44 Terms
Soft or liquid stool > 3 times in 24 hrs; caused by infex, IBD, or meds
Define Diarrhea
If it lasts > 4 wks
When is Diarrhea considered chronic?
> Rib Raising & Suboccipital Inhibition (SNS vs PNS)
> Thoracic inlet and TAD release for Infex Diarrhea (R-C)
> Ganglion Inhibition (SNS)
What OMT can be done for Diarrhea?
Unsatisfactory defecation characterized by infrequent stools and/or difficult stool passage
Define Constipation
>2 of the following for 3 mo:
–straining during ≥ 25% of defecations
–lumpy or hard stools during ≥ 25% of defecations
–feeling of incomplete evacuation during ≥ 25% of defecations
–feeling of obstruction or blockage during ≥ 25% of defecations
–manually facilitating defecation during ≥ 25% of defecations
–< 3 bowel movements/week
How is Constipation defined as per the Rome III criteria?
> Rib raising/soft tissue to T10-L2/Suboccipital Inhibition (Vagus)/Sacrum Tx [SNS vs PNS]
> Ganglion Inhibtion (SNS)
> Mesenteric Release (R-C)
> Colonic Stimulation
What OMT can be done for Constipation?
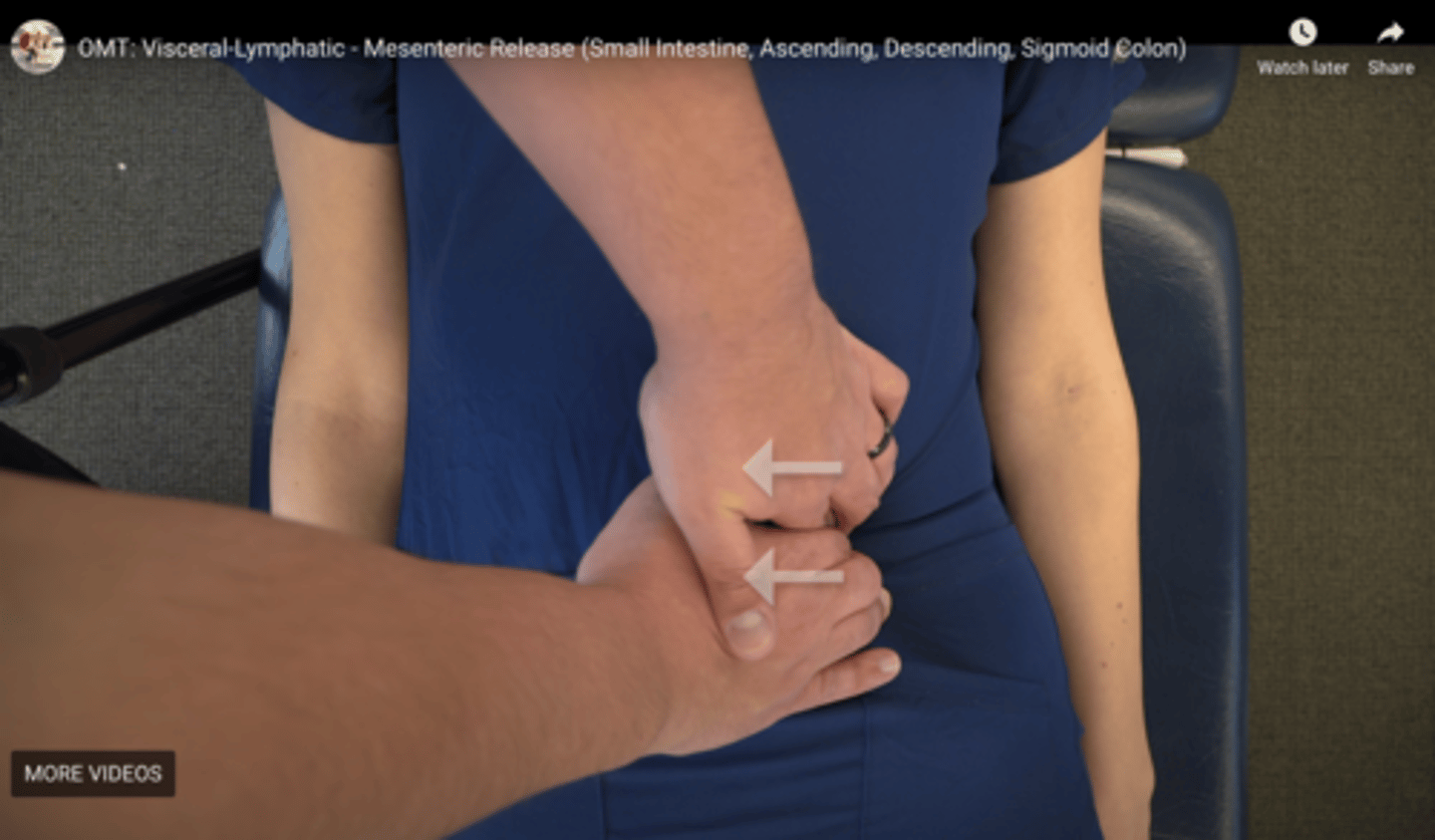
Place hand at left border of mesenteric region (to left of midline) w/ fingers curled --> push into RUQ
Where should the physician's fingers gently push posteriorly to engage tissues for Small Intestine Mesenteric Release?

Place hand at right border of mesenteric region (to right of midline) w/ fingers curled --> push into left side
Where should the physician's fingers gently push posteriorly to engage tissues for Ascending Colon Mesenteric Release?
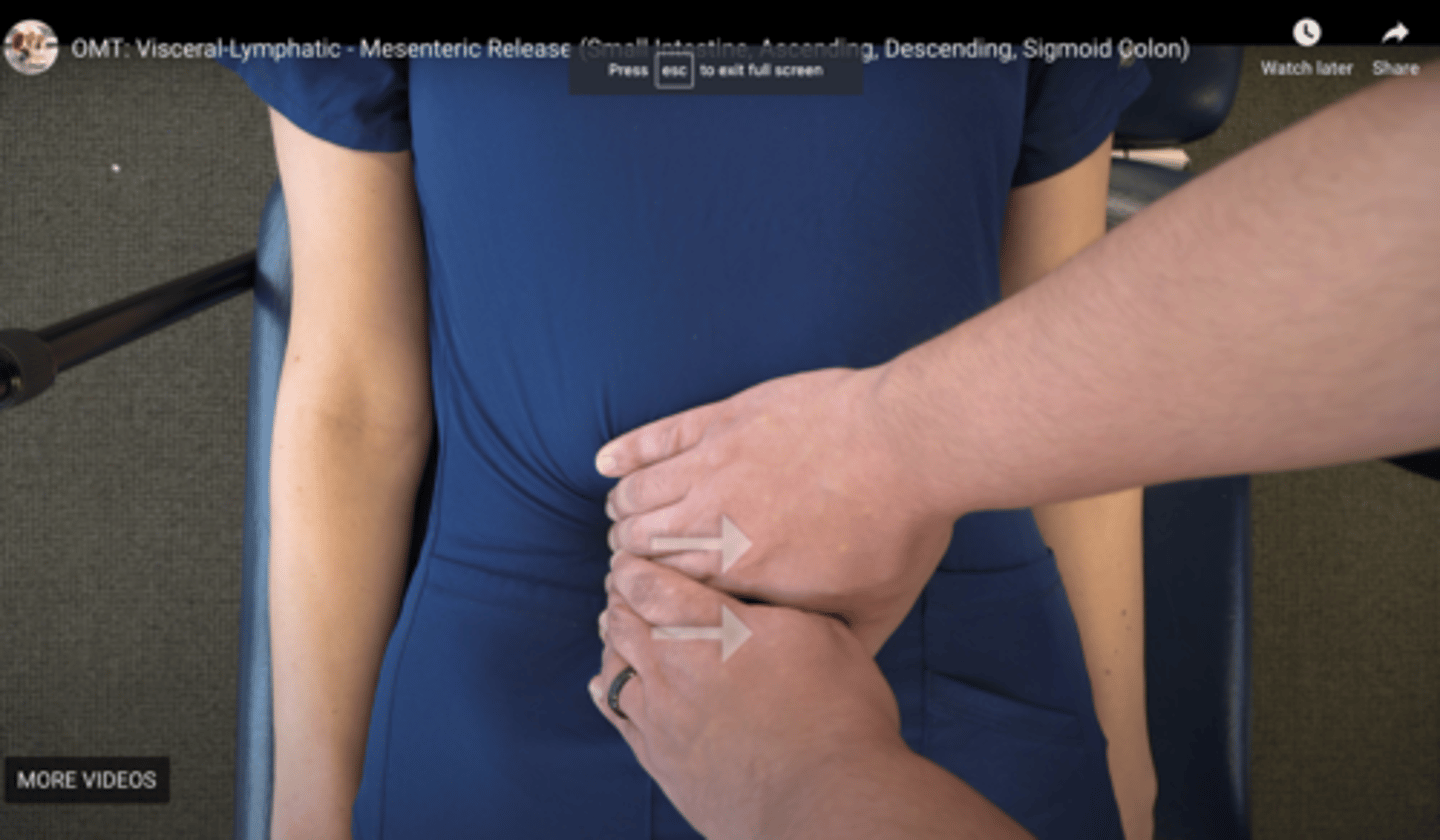
Place hand at left border of mesenteric region of ascending colon (to left of midline) w/ fingers curled --> push into right side
Where should the physician's fingers gently push posteriorly to engage tissues for Descending/Sigmoid Colon Mesenteric Release?
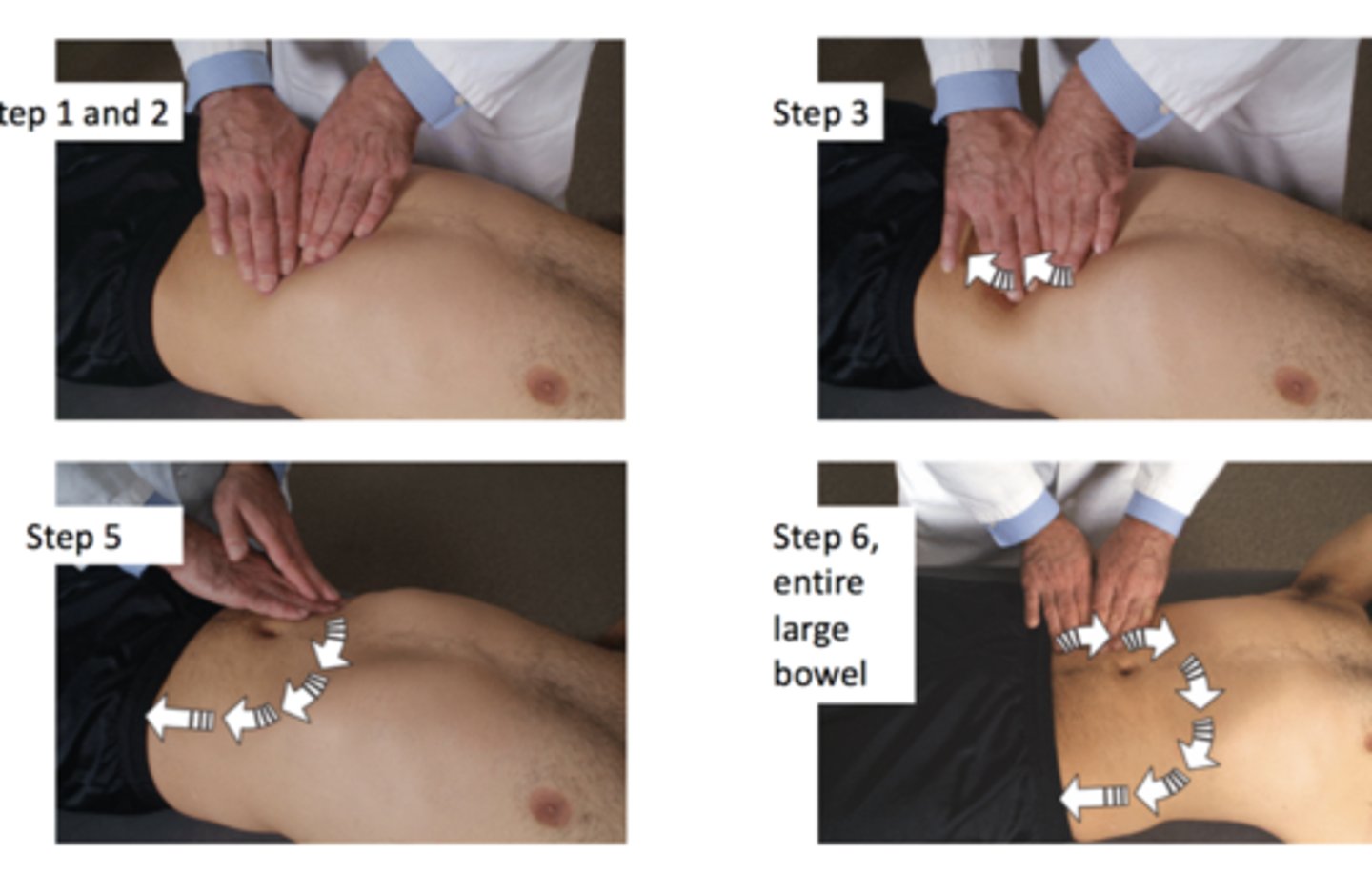
Put fingers over sigmoid colon & roll fingers along bowel in direction of colonic flow to left inguinal area --> release pressure and reposition hands along colon toward descending colon --> reposition hands at splenic flexure then work down the descending/sigmoid colon --> reposition hands at hepatic flexure then across transverse colon, then back down descending/sigmoid colon --> reposition hands to cecum, then work along ascending, transverse, then descending colon
Describe how Colonic Stimulation should be performed
Normal-transit constipation
Define Constipation Type:
Incomplete evacuation;
-Sx: (+/-) Abdominal pain
-Dx: Normal Results
Slow-transit constipation
Define Constipation Type:
Infrequent stools (e.g., ≤1/wk)
-Hx: Young Women
-Sx:
> Lack of urge to defecate
> Poor response to fiber and laxatives
-PE:
> Malaise
> Fatigue
-Dx: Retention in colon of >20% of radiopaque markers five days after ingestion
Defecatory disorders (pelvic floor dysfunction, anismus, descending perineum syndrome, rectal prolapse)
Define Constipation Type:
Incomplete Evacuation
-Hx: Young Women
-Sx:
> Frequent Straining
(need for manual maneuvers to facilitate defecation)
-Dx: Abnormal balloon expulsion test and/or rectal manometry
Irritable Bowel Syndrome
Define Condition:
Recurrent abdominal pain on average at least 1 day per week in the last 3 months, associated with 2 or more of the following:
1) Related to defecation
2) A/w change in stool frequency
3) A/w a change in form (appearance) of stool
Diarrhea, Constipation and IBS if there NO ORGAN RUPTURE, SEVERE BLEEDING, and IF TOLERATED
In what cases can OMT be safely performed for GI issues?
OMT directed at viscerosomatic reflexes
What should be done in terms of OMT if a patient is experiencing abdominal/intestinal cramping?
> If Acutely Ill (until pt is stabilized)
> If stabilized, only use it to address viscerosomatic reflexes
When should OMT NOT be used on pts?
> TAD musculature
> Abdominal musculature
> Pelvic floor musculature
What structures are needed to function for Defecation to occur?
Appropriate increase in intraabdominal pressures can be produced and excessive straining prevented to allow for better defecation
How might correcting abdominal and pelvic floor musculature improve defecation?
> Sacrum
> L5 innominates
> Iliopsoas
> Pelvic Floor Musculature
Somatic dysfunction of what structures can affect the position of the colon (ex: descending, sigmoid colon, rectum), thus impairing normal peristalsis and defecation?
Strains the pelvic floor musculature --> pelvic floor/innominate/sacral somatic dysfunction ==> Organ Prolapse
How is constipation (and thus straining during BM) a risk factor for pelvic floor dysfunction?
Piriformis syndrome
What might occur from severe/recurrent straining from constipation?
1) Thoracic Inlet Release
2) Tx TAD
3) Assess Mesenteries for somatic dysfunction (since the main channels for circulation for intestines is in mesenteries)
How should the intestines be treated according to the Resp-Circ Model?
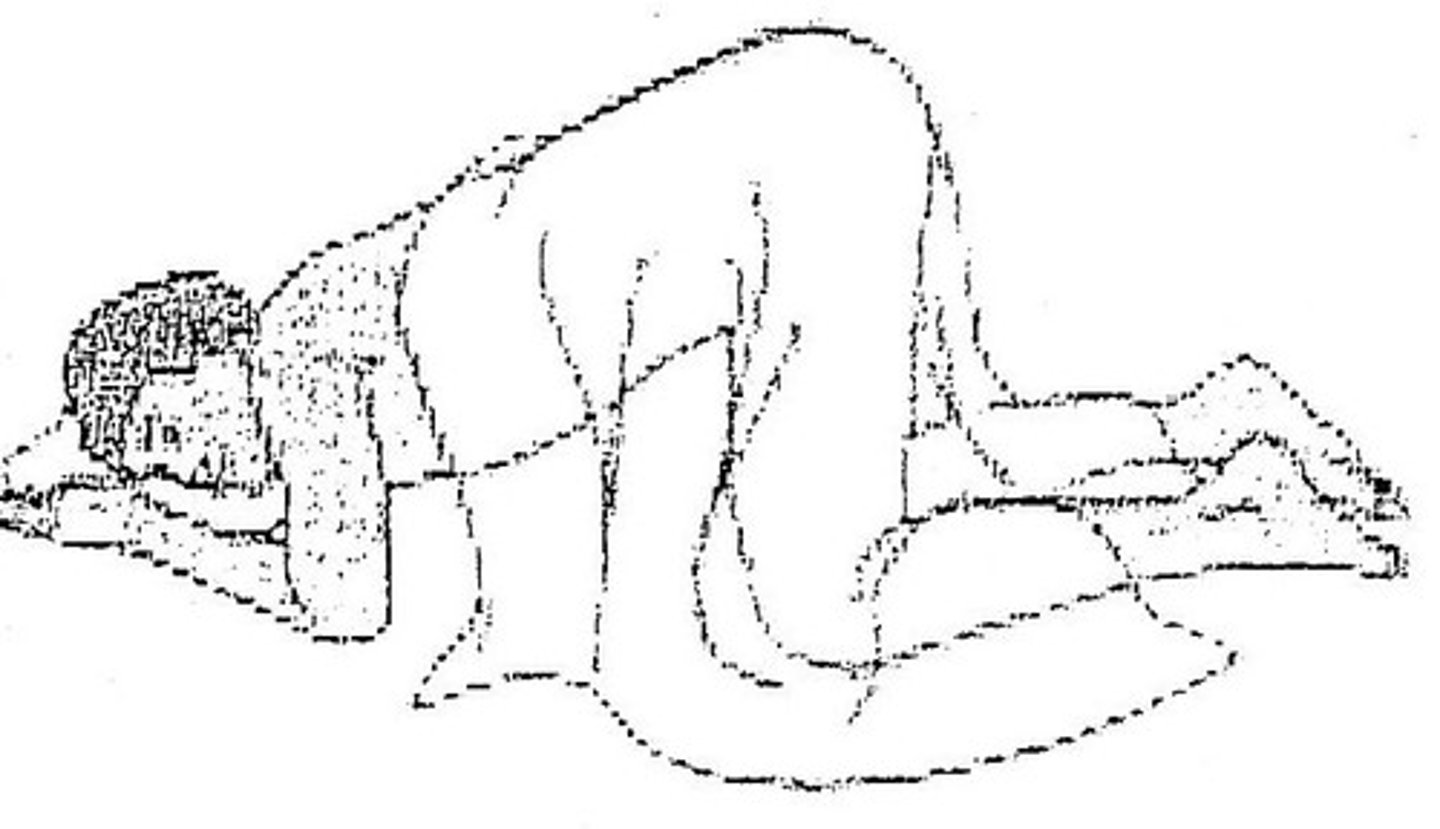
Knee-Chest Position:
In this position, gravity draws abdominal and pelvic contents out of pelvis to help reposition and reduce strain upon those organs as well as drain contents
What is a method to treat the Intestines via the Resp-Circ Model that pts can do at home (esp for those with Constipation, Dysmenorrhea, or other Pelvic "Congestion" Issues)?
- Decreased motility in the gut = constipation, distention
- Contraction of the rectal sphincter
- Vasoconstriction
- Decreased mucosal defenses in the stomach
Stimulation of the SNS of the GI system causes what to occur?
T10-L2
What structures can be treated to REDUCE SNS (ex: Constipation from reduced peristalsis)?
- Increases motility and peristalsis
- Increases secretions
- Vasodilation
- Relaxation of sphincters
Stimulation of the PNS of the GI system causes what to occur?
Vagus for Proximal Intestines, Sacrum for Distal Colon
What structures can be treated to REDUCE PNS (ex: Constipation from reduced peristalsis)?
Right medial 5th and 6th intercostal spaces
Ant CR of Liver
Right medial 6th intercostal space
Ant CR of Gall Bladder
Right medial 7th intercostal space
Ant CR of Pancreas
Medial 8th-10th intercostal spaces near the cartilages
Ant CR of Small Intestines
Upper edge of the tip of rib 12 on the Right
Ant CR of Appendix
Anterior iliotibial bands from greater trochanter to distal lateral condyle, 1-2" wide band corresponding to large intestines flipped over thighs
Ant CR of Colon
Between the Right T5 and T6 transverse and spinous processes
Post CR of Liver
Between the Right T6 transverse and spinous processes
Post CR of Gall Bladder
Between the Right T7 transverse and spinous processes
Post CR of Pancreas
Between the transverse and spinous processes of T8-T10
Post CR of Small Intestines
T11 transverse process
Post CR of Appendix
Triangular area from the L2-L4 transverse processes to the crest of the ileum
Post CR of Colon
Constipation can lead to abdominal bloating, cramping (pain), and decreased appetite, leading to a worsening nutritional status (slowed growth in children)
How does constipation affect the pt from the Metabolic-Energy Model?
To encourage bowel motion and movement after intestines have been still for too long (to avoid effects of poor nutrition and lack of gut activity)
Why are pts encouraged to walk soon after surgery?
Leads to loss of electrolytes can lead to metabolic disorders, such as hypokalemia which has multiple effects on the body, or dehydration
How can diarrhea affect the pt from the Metabolic-Energy Model?
Profoundly affects the gut flora --> More illnesses (ex: common cold)
How can IBS affect the pt from the Metabolic-Energy Model?