Neoplasia 2: Histological Features of Malignancy, Tumour Growth and Evolution
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
20 Terms
List some further cytological criterias of malignancy.
11) Nuclear Moulding
12) Coarse Chromatin
13) Macronucleoli
14) Angular Nucleoli
15) Anisonucleosis
Noone can mail anything alright.
What is nuclear molding?
• Nuclei are deformed by adjacent nuclei
• In the same or adjacent cell(s)
• Reflections of rapid growth/overcrowding
• Cells physically squashed together
What does coarse chromatin tell us?
thickly corded chromatin
Indicates cell is very active, usually dividing
What does macronucleoli tell us?
Nucleoli > 5um (erythrocytes = 5-6um diameter)
What does angular nuclei tell us?
prominant angular nucleoli - more malignant
What does anisonucleosis tell us?
variably sized nucleoli
What are the histological features of malignancy?
1) Enlarged nucleus with prominent nucleolus
Small amounts of cytoplasm
2) Increased mitotic figures
bizarre/abnormal mitoses
3) Multiple nucleoli
4) Bizarre / large nucleoli
karyomegaly
What are some of the biggest markers of differentiation in malignant cells?
• Cell morphology
neoplastic cells often lose any recognisable gross & histological appearance - see Lecture 1
• Cell function
usually lost in malignant tumours
regulatory mechanisms lost
• Cell behaviour
Increasingly aggressive with loss of differentiation and function
What is the parenchyma of the tumour?
What is the stroma of the tumour?
Parenchyma
Neoplastic or transformed cells
Determine biologic behavior
Stroma
Non-neoplastic, host-derived support tissues
Connective Tissue
Blood vessels
Host-derived inflammatory cells
Essential for tumour growth, providing physical support and nutrients
Describe the complex stromal interactions taking place within tumours.
• Complex interaction (2-way)
Signalling molecules - wide variety
» growth factors, cytokines, hormones, inflammatory mediators
• Modulate growth rate, differentiation state, behaviour of both cell groups
e.g. tumour-derived TGF-a (transforming growth factor - a)
» fibroblasts differentiate to myofibroblasts
» pericytes at edge of vessels
e.g. tumour cells release PDGF (platelet derived growth factor)
Scirrhous/desmoplastic responses
Allows new blood vessels to grow in
What percentage of canine cancers are believed to be hereditary?
5 - 10%
What cancer affecting GSDs is hereditary?
- renal carcinoma and nodular dermatofibrosis (RCND)
» autosomal dominant inheritance
» inactivation of tumour suppressor gene
folliculin (FLCN)
What causes heritable alterations in cancer?
Progressive accumulation of genetic and epigenetic abnormalities in cells
• Initial change is due to:
EITHER inherited germline mutation
OR somatic mutation, DNA damage by…
EITHER intrinsic factors
OR extrinsic factors
» by-products of metabolism e.g. Reactive Oxygen Species (ROl)
» a chemical carcinogen, radiation or an oncogenic virus
What is epigenetics?
Epigenetic: reversible, heritable changes in gene expression that occur without mutation
e.g. hypermethylation of promoter sequence -> stop tumour suppressor
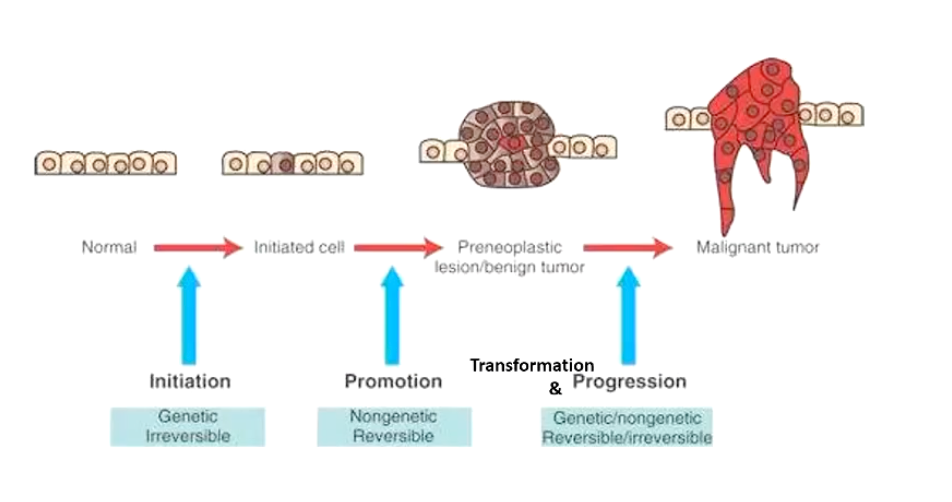
Describe the stepwise tumour development process.
**Best understood in carcinomas
• Stepwise tumour development
1) Initiation
• irreversible GENETIC change introduced
2) Promotion
• specific stimuli cause outgrowth of initiated cells
• the end result is a benign neoplasia
(Transformation)
• neoplastic cells become progressively more malignant
3) Progression
• increased dysregulation
eventually become a malignant tumour
Can be irreversible or reversible
Describe key features of the initiation stage of tumour development.
• Irreversible genetic change induced in basal cells by an initiator
• Initiator = chemical or physical carcinogen
→ DNA lesion introduced
→ DNA lesion mispairing during subsequent replication
→ mutation fixation (Not caught by cytotoxic T cells or NK cells)
• Initiated cells
- morphologically normal
- possibly quiescent for years until triggered to next stage
Describe key features of the promotion stage of tumour development.
- outgrowth of initiated cells in response to selected stimuli
• promoters alter gene expression
• initiated cells have growth advantage over uninitiated cells
• not a mutation, so REVERSIBLE
If stimulus removed, can return to quiescent cells
Describe key features of the transformation and progression stage of tumour development.
Go from benign to malignant to metastatic (If stimulus causes)
Involves genetic and epigenetic changes
Increasingly malignant sub-clones selected
Summarize the stepwise tumour development.
Outline the stepwise development of squamous cell carcinoma (SCC).
• Step 1: epidermal hyperplasia - benign papilloma (A-B)
• Step 2: carcinoma beginning to invade (C)
• Step 3: invasive carcinoma (D)