NURS 261 Exam 1: Key Terms on Health Equity & Culture
1/79
Earn XP
Description and Tags
NURS 261 Exam 1
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
80 Terms
health
a dynamic balance of physical, emotional, social, spiritual, and intellectual health.
wellness
a conscious, self-directed, and evolving process of achieving full potential. multi-dimensional and holistic, encompassing lifestyle, mental and spiritual well-being, and the environment. positive and affirming.
wellness dimension: occupational
personal satisfaction and enrichment in one's life through work; attitude about one's work.
wellness dimension: emotional
express feelings freely and manage feelings effectively. forms an interdependent relationship founded on mutual commitment, trust, and respect.
wellness dimension: spiritual
action consists of beliefs, values, and tolerance of others' beliefs.
wellness dimension: intellectual
actively striving to expand and challenge the mind with creative endeavors.
wellness dimension: social
willful choices to enhance personal relationships and important friendships. build a better living space and community.
wellness dimension: physical
striving to achieve a healthy body through exercise, nutrition, sleep, etc.
quality of life
a concept aiming to capture the well-being (population or individual) regarding both positive and negative elements within the entirety of their existence at a specific point in time. a younger patient's QOL is different than an older patient's QOL.
physical well-being
functional ability, strength or fatigue, sleep and rest, overall physical health, and fertility.
social well-being
family distress, roles and relationships, affection/sexual function, appearance, enjoyment, isolation, finances, and work.
psychological well-being
control, anxiety, depression, enjoyment/leisure, cognition/attention, fear of recurrence, and distress of diagnosis and treatment control.
spiritual well-being
meaning of illness, religiosity, hope, uncertainty, inner strength, and transcendence.
clinical model of health
the absence of the disease and the presence of signs and symptoms of the disease. prevention not emphasized. focus on disease and provider.
holistic model of health
the sum of all dimensions. evaluated by how it impacts the whole functioning. multiple disciplines to address health. prevention emphasized. focus on the whole person (person-centered approach).
primary prevention
precedes disease or dysfunction; health promotion/protection; prevention!!

secondary prevention
avert or delay consequences of advanced disease; early diagnosis (screen), prompt treatment, and disability limitation.

tertiary prevention
defect or disability is permanent and irreversible; restoration and rehab; treatment.

culture
languages, customs, beliefs, rules, arts, knowledge, and collective identities and memories developed that make their social environments meaningful.
culture examples
a shared system of beliefs, values, and behavioral expectations, provides social structure for daily living, defines roles and interactions with others and in families and communities, apparent in the attitudes and institutions unique to the culture, and can have subcultures with characteristics not common to the larger culture.
cultural competence
cultural awareness, cultural knowledge, and cultural skills.
cultural competence examples
developing self-awareness, demonstrating knowledge and understanding of a patient's culture, accepting and respecting cultural differences, etc.
literacy
the ability to understand, evaluate, use, and engage with written texts to participate in society, achieve one's goals, and develop one's knowledge and potential.
literacy examples
reading (word recognition), readability (the ease with which written material can be read), and comprehension (the degree to which one understands what they have read).
health literacy
the degree to which individuals can obtain, process, and understand basic health information needed to make appropriate health decisions.
reasons for low literacy
low educational skills, cultural barriers to health care, health conditions require a high level of complicated self-care, not familiar with medical terms or how the body works, and scared and confusion when diagnosed with serious illness.
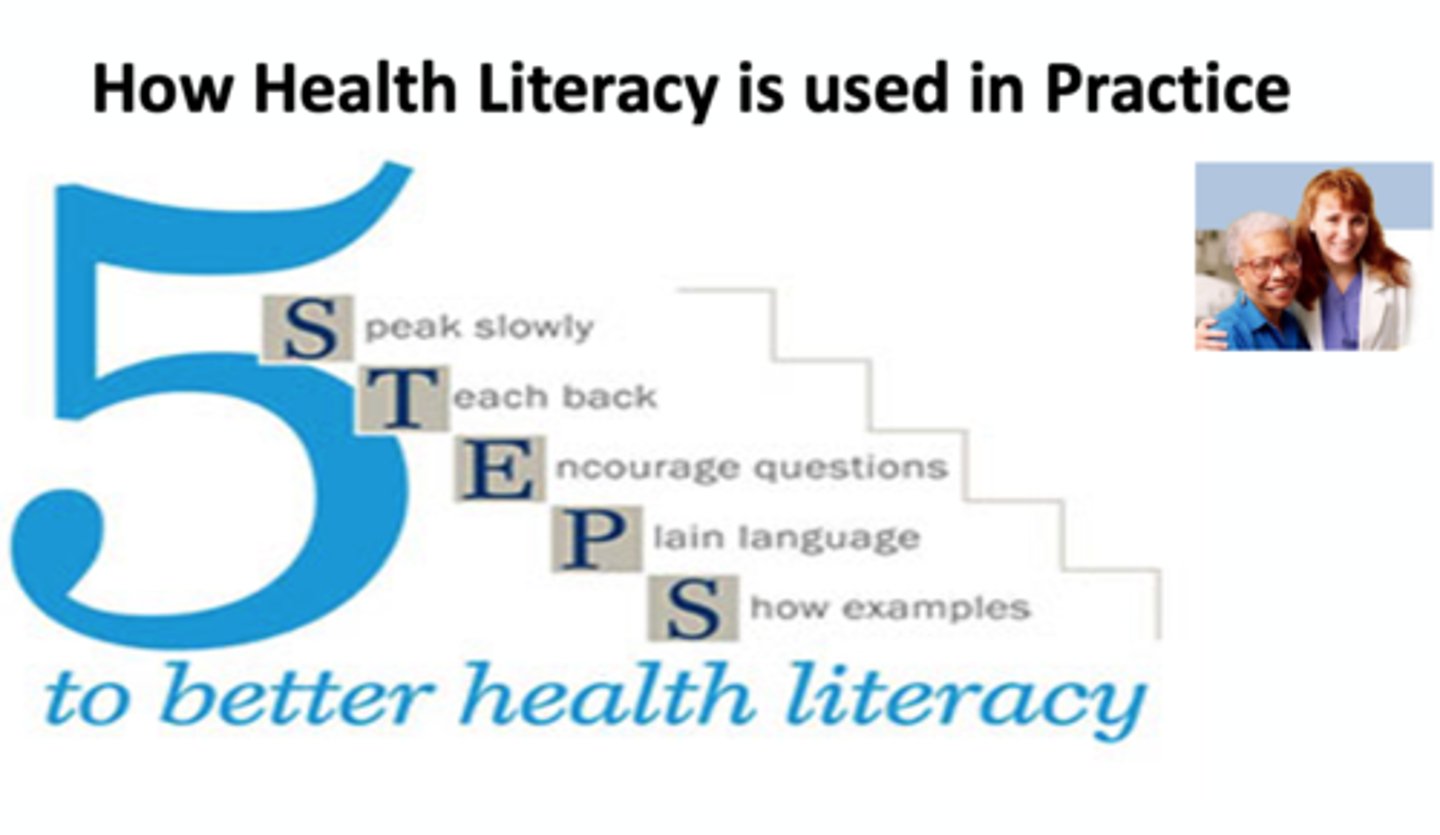
client literacy needs (5 steps)
speak slowly, teach back, encourage questions, plain language, and show examples.
health disparities
differences in the health status of groups of people that are closely linked to social, economic, and/or environmental disadvantages.
health disparity determination
disease incidence, disease prevalence, morbidity, and life expectancy.
health disparity populations
race/ethnicity, sex, sexual identity, age, disability, socioeconomic status, and geographic location.
health disparity examples
heart disease, cancer, infant mortality, obesity, smoking, diabetes, chronic disease, access to health care, and quality of care.
vulnerable populations
chronically ill or disabled, LGBTQ+ population, low-income and/or homeless individuals, women (very young or old), and certain geographical communities (rural and inner city).
emerging populations
homeless, LGBTQ+, and minorities.
health equity
attainment of the highest level of health for all people. promoted through full and equal access to healthy living opportunities.
education access and quality
the connection of education to health and well-being. includes graduating from high school, enrollment in higher education, educational attainment in general, language and literacy, and early childhood education and development.
economic stability
the connection between the financial resources people have (income, cost of living, and socioeconomic status). includes poverty, employment, food security, and housing stability.
health care access and quality
the connection between people's access to and understanding of health services and their own health. includes access to healthcare, access to primary care, health insurance coverage, and health literacy.
neighborhood and built environment
the connection between where a person lives (housing, neighborhood, and environment) and their health and well-being. includes quality of housing, access to transportation, availability of foods, air and water quality, and neighborhood crime and violence.
social and community context
the connection between characteristics of the contexts within which people live, learn, work, and play, and their health and well-being. includes civic participation, discrimination, incarceration, and social cohesion.
autonomy
the right or condition of self-government.
confidentiality
the ability to maintain privacy in one's life (patient information is private unless consent to release the information is provided by the patient).
veracity
truth-telling; supports health-promotion activities.
nonmaleficence
enjoins people to not harm other people; this principle constrains people from autonomous actions that are likely to harm others.
justice
an ethical principle of major importance in health-promotion settings.
kohlberg's moral reasoning: level one - preconventional
0-6 years; obeys to avoid punishment.
kohlberg's moral reasoning: level two - conventional
7-11 years; naive. conforms to get rewards and have favors returned; good boy/girl. conforms to avoid disapproval or being disliked.
kohlberg's moral reasoning: level three - postconventional
11 years+; conforms to avoid censure by authorities. individual principles or conscience. emphasis on individual rights.
gilligan's moral reasoning: preconventional
individual survival (selfishness).
gilligan's moral reasoning: conventional
self-sacrifice is goodness (social morality).
gilligan's moral reasoning: postconventional
principled morality.
descriptive theory
describes people's actual behavior, explains why people behave as they do, and the behavior exhibited defines the person.
normative theory
sets a standard for how people ought to act, justifies why people ought to behave as outlined by the standard, and conscious choices of action define the person.
consequentialism
focuses on the consequences of actions.
deontology (duty-based)
focus on adherence to moral duties and rights.
virtue ethics (character-based)
focuses on character.
ethical decision-making purpose
examines beliefs and values, examines the influence of beliefs on professional practice, post-situation reflection, willingly revises beliefs to align with professional standards, and does not require compromising personal integrity.
health education
any combination of planned learning experiences based on sound theories. increase knowledge, promote skill development, produce a change in behavior, and facilitate health-related learning and tools.
health promotion
the process of enabling people to increase control over, and to improve their health.
goals of health education
achieve the optimal state of health. change health behaviors and improve health status.
primary health screening
detection of a disease in its early stages in order to treat it and deter its progression.
secondary health screening
reduce the cost of disease management by avoiding costly interventions required at later stages.
advantages of health screening
simplicity, individual and group screening, one or multiple-test screening, and opportunity for health education.
disadvantages of healths screening
false positive and negative results.
newborn screening tests
congenital and genetic disorders; metabolic, endocrine, cystic fibrosis, sickle cell anemia, etc.
infant screening tests
iron deficiency anemia and lead poisoning.
children screening tests
lead, iron deficiency anemia, obesity, and diabetes.
adult screening tests
pap test (>21), mammography (40/45), cholesterol (20), colonoscopy (45), fecal occult blood (45), diabetes or pre-diabetes (35).
physical activity for ages 3-5
encourage children to be active when they play and be physically active throughout the day for growth and development.
physical activity for ages 6-17
60 minutes or more of moderate-to-vigorous intensity physical activity each day. aerobic activity (walking, running), muscle-strengthening (climbing, push-ups), and bone-strengthening (jumping, running).
adult physical activity
150 minutes of physical activity; 30 minutes, 5 days a week. muscle-strengthening activities and aerobic activities.
older adults' physical activity (age > 65)
at least 150 minutes a week (30 min; 5 days). at least 2 days of activities that strengthen muscles and activities that improve balance, such as standing on one foot.
pregnant or postpartum women physical activity
at least 150 minutes (30 min; 5 days) of moderate-intensity aerobic physical activity per week. brisk walking, during and after pregnancy.
adults with chronic conditions physical activity
at least 150 minutes (30 min; 5 days) of moderate-intensity aerobic physical activity a week and at least 2 days a week of muscle-strengthening activities that include all major muscle groups.
stress management interventions
physical exercise, meditation, deep breathing, slowing down, connecting socially, tuning into your body, decompressing, laughing out loud, reducing toxic relationships, healthy diet, consistent sleep, being assertive, connecting spiritually, listening to loud music, and alternative therapy (hypnosis or acupuncture).
primary mental health prevention
identifying high risk
secondary mental health prevention
early detection and intervention
tertiary mental health prevention
advanced recovery and reduction of relapse risk.
meaning of spirituality
comprises feelings, thoughts, experiences, and behaviors that arise from a search for meaning and may include interconnectedness with self, others, nature, and a higher force.
factors affecting spirituality
family, ethical background, formal religion, life events, and developmental considerations.
spirituality needs common to most people
meaning of illness, religiosity, transcendence, hope, uncertainty, and inner strength.