Chapter 15: Psychotic Disorders
1/28
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
29 Terms
Chapter 15: Psychotic Disorders
Psychotic disorders (including schizophrenia) affect:
Thinking
Behavior
Emotions
Ability to perceive reality
Etiology (Causes)
Likely due to a combination of:
Genetic factors
Neurobiological factors
Nongenetic factors (injury at birth, viral infection, nutritional factors)
Onset
Typical age: mid-teens to mid-20s
Can occur:
In young children
In later adulthood
Prodromal Period
Early stage before full disorder develops
Symptoms may include:
Negative symptoms (e.g., anergia = lack of energy)
Reduced positive symptoms (less intense hallucinations/delusions)
Impact
Becomes problematic when symptoms interfere with:
Interpersonal relationships
Self-care
Ability to work
Types of Psychotic Disorders (DSM-5-TR)
Schizophrenia
Psychotic thinking/behavior ≥ 6 months
Significant impairment in work, self-care, relationships
Schizotypal Personality Disorder
Impaired self/interpersonal functioning
Not as severe as schizophrenia
Delusional Disorder
Delusions ≥ 1 month
Functioning not markedly impaired
Brief Psychotic Disorder
Psychotic symptoms lasting 1 day – 1 month
Schizophreniform Disorder
Symptoms like schizophrenia
Duration 1 – 6 months
Social/occupational dysfunction may not be obvious
Schizoaffective Disorder
Meets criteria for both schizophrenia and mood disorder (depressive or bipolar)
Substance/Medication-Induced Psychotic Disorder
Psychosis from intoxication, withdrawal, or medication exposure
More severe than typical substance effects
Psychotic or Catatonic Disorder Due to Another Medical Condition
Psychosis or catatonia caused by a medical condition
Does not meet criteria for another specific psychotic disorder
Psychotic Disorder Expected Findings
Positive Symptoms (things not normally present, easily identifiable)
Hallucinations
Delusions
Alterations in speech
Bizarre behavior (e.g., walking backward constantly)
Negative Symptoms (absence of normal functions – harder to treat)
Affect – Blunted/flat emotional expression
Alogia – Poverty of speech/thought
Anergia – Lack of energy
Anhedonia – Lack of pleasure/joy
Avolition – Lack of motivation (cannot initiate activities without prompting)
Cognitive Findings (thinking/processing difficulties)
Disordered thinking
Poor decision-making
Poor problem-solving
Difficulty concentrating
Short-term memory deficits
Impaired abstract thinking
Affective Findings (emotion-related)
Hopelessness
Suicidal ideation
Unstable or rapidly changing mood
Alterations in thought (delusions)
Alterations in Speech
Alterations in Perception
Personal Boundary Difficulties
Alterations in Behavior
Determine which symptom to drag positive or negative symptoms of schizophrenia. Drag each symptom to the desired image.
Hallucinations
Avolition
Alterations in speech
Delusions
Bizarre Motor movements
Flat affect
Anhedonia
Anergia
Positive
Negative
Positive
Bizarre Motor movements
Delusions
Alterations in speech
Hallucinations
Negative
Anhedonia
Anergia
Flat affect
Avolition
Alterations in Thought (Delusions)
False, fixed beliefs that cannot be corrected by reasoning (often bizarre).
Ideas of reference – Misinterprets trivial events as personal (e.g., others talking about them)
Persecution – Believes others intend harm (e.g., hunted by FBI)
Grandeur – Believes they are powerful/important (e.g., god-like)
Somatic delusions – Believes body is changing unusually (e.g., growing extra limb)
Jealousy – Believes partner is unfaithful without evidence
Being controlled – Believes outside force is controlling their body
Thought broadcasting – Believes others can hear their thoughts
Thought insertion – Believes others’ thoughts are placed into their mind
Thought withdrawal – Believes thoughts are removed by external force
Religiosity – Preoccupation with religious beliefs
Magical thinking – Believes actions/thoughts control events (e.g., special hat makes them invisible)
Alterations in Speech
Associative looseness – Incoherent, rapid shifting of topics (flight of ideas)
Neologisms – Made-up words with meaning only to client
Echolalia – Repeats words spoken to them
Clang association – Rhyming words, often forceful (“fox, box, lox”)
Word salad – Jumbled words without meaning (“Hip hooray, the flip is cast…”)
Circumstantiality – Excessive, unnecessary details before getting to the point
Tangentiality – Wanders off-topic; never returns to original point
Alterations in Perception (hallucinations – no external stimulus)
Auditory – hearing voices/sounds
Command hallucinations – voices instruct actions (e.g., harm self/others → high risk)
Visual – seeing persons/things
Olfactory – smelling odors
Gustatory – experiencing tastes
Tactile – feeling bodily sensations
Personal Boundary Difficulties
Disconnection with body, identity, or perception.
Depersonalization – feeling identity is lost/unreal
Derealization – perceiving environment as altered (e.g., shrinking objects)
Illusions – misinterpretation of real external stimuli
Alterations in Behavior
Extreme agitation – pacing, rocking
Stereotyped behaviors – repetitive, purposeless movements (e.g., sweeping motions)
Automatic obedience – robot-like compliance
Waxy flexibility – maintaining rigid posture for long time
Stupor – motionless, coma-like
Negativism – doing the opposite of requests
Echopraxia – mimicking movements of others
Catatonia – decreased/increased movement; rigid positioning possible
Motor retardation – slowed movements
Impaired impulse control – inability to resist urges
Gesturing/posturing – unusual, illogical expressions
Boundary impairment – inability to see distinction between self and others
Personality Disorder Standardized Screening Tools
AIMS (Abnormal Involuntary Movement Scale) – used to monitor involuntary movements and tardive dyskinesia in clients on antipsychotic medications
Personality Disorder Nursing Care
Therapeutic Approaches
Milieu therapy – structured, safe environment to reduce anxiety & distraction from hallucinations
Assertive Community Treatment (ACT) – intensive case management & interprofessional support for community-living needs
Promote therapeutic communication – reduces anxiety, defensive patterns, and increases participation
Establish trusting relationship with client
Communication for Hallucinations & Delusions
Ask directly about hallucinations (acknowledge feelings without agreeing/disagreeing)
Do not argue with delusions; instead, focus on client’s feelings and provide supportive responses
Monitor for paranoid delusions (risk for violence)
Ensure safety if client has command hallucinations (↑ risk for harm to self/others)
Use reality-based topics in conversation
Identify manifestation triggers (e.g., loud noises can worsen auditory hallucinations)
Be genuine and empathetic
Additional Nursing Interventions
Determine discharge needs (ADLs, ability to live independently)
Promote self-care by teaching/modeling within facility
Link wellness to manifestation management
Teach coping strategies for hallucinations/anxiety:
Music, attending activities, walking, talking with trusted person, directly addressing hallucination (“go away”)
Provide medication education
Involve family when possible
Client Education
Develop social skills and friendships
Participate in group work and psychoeducation
Comply with medications
A nurse is speaking with a client who has schizophrenia when the client suddenly seems to stop focusing on the nurse’s questions and begins looking at the ceiling and talking to themselves. Which of the following actions should the nurse take?
a
Stop the interview at this point, and resume later when the client is better able to concentrate.
b
Ask the client, “Are you seeing something on the ceiling?”
c
Tell the client, “You seem to be looking at something on the ceiling. I see something there, too.”
d
Continue the interview without commenting on the client’s behavior.
Submit
b Ask the client, “Are you seeing something on the ceiling?”
When taking action, the nurse should ask the client directly about the hallucination to identify client needs and monitor for a potential risk for injury.
The nurse should address the client’s current needs related to the possible hallucination rather than to stop the interview.
Avoid agreeing with the client, which can promote psychotic thinking
The nurse should address the client’s current needs related to the possible hallucinations rather than ignoring the change in behavior.
Medications for Psychotic Disorders
Schizophrenia often has acute exacerbations with intervals of semi-remission (symptoms persist but are less severe).
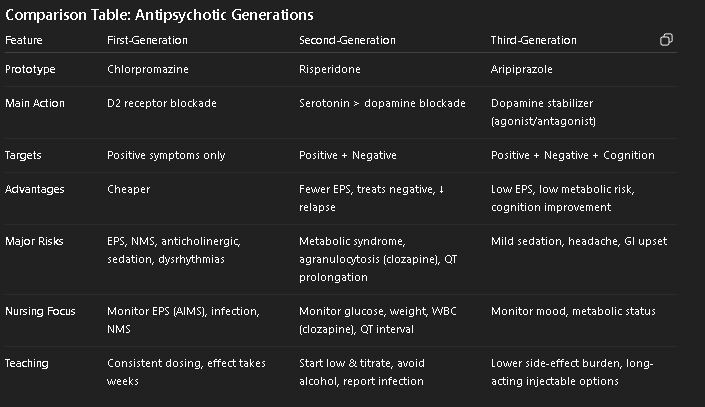
First-Generation (Conventional) Antipsychotics
Used mainly for positive symptoms
Reserved for clients who:
Can tolerate adverse effects
Cannot afford second-generation medications
Potency levels:
Low potency – low EPS, high sedation, high anticholinergic effects
Medium potency – moderate EPS, sedation, anticholinergic effects
High potency – high EPS, low sedation, low anticholinergic effects
Second-Generation (Atypical) Antipsychotics
(Current first-line treatment for schizophrenia)
Advantages:
Relieve both positive and negative symptoms
Reduce depression, anxiety, suicidality
Improve neurocognitive deficits (e.g., poor memory)
Few or no EPS (less dopamine blockade → less tardive dyskinesia)
Fewer anticholinergic effects (exception: clozapine has high incidence)
Lower relapse risk
Third-Generation Antipsychotics
Treat both positive and negative symptoms
Improve cognitive function
Advantages:
Decreased EPS/tardive dyskinesia
Lower risk for weight gain & anticholinergic effects
Goals
Suppress acute episodes
Prevent acute recurrence
Maintain highest possible level of functioning
Health Teaching
Understanding of disorder
Self-care to prevent relapse
Medication adherence & side effects
Importance of support groups
Avoid alcohol/substances
Keep log/journal of feelings & behavior changes (monitor effectiveness)
Nursing Evaluation of Medication Effectiveness
Improvement/prevention of acute psychosis (↓ hallucinations, delusions, anxiety, hostility)
Improved ADLs
Improved social interaction with peers
Better sleep & eating habits
Extrapyramidal Symptoms (EPS) Types (DTAP)
(Acute) Dystonia
Manifestations: Severe spasms of tongue, neck, face, back → crisis situation
Nursing actions:
Monitor 1–5 days after start
Treat: benztropine (antiparkinsonian), diphenhydramine IM/IV
Stay with client until resolved (5–15 min)
Tardive Dyskinesia (TD)
Manifestations: Late EPS (months–years); involuntary movements (tongue, face, arms, trunk)
Nursing actions:
Evaluate at 12 months, then every 3 months
Switch to 2nd-gen antipsychotic if possible
No reliable treatment; instruct client on controlling purposeful movements
Akathisia
Manifestations: Inability to sit still, pacing, agitation
Nursing actions:
Monitor during first 2 months (5–60 days)
Treat with antiparkinsonians, beta-blockers, lorazepam/diazepam
Monitor suicide risk
Pseudoparkinsonism
Manifestations: Bradykinesia, rigidity, shuffling gait, drooling, tremors (pill-rolling), mask-like face
Nursing actions:
Monitor during first month (5–30 days)
Treat with benztropine/trihexyphenidyl
Positive vs Negative Symptoms
Agitation, bizarre behavior, delusions, hallucinations, flight of ideas, loose associations
Social withdrawal, flat affect, low energy, low motivation, anhedonia
Antipsychotics: First-Generation (Conventional) (-azine, -thixene, Loxapine, Haloperidol) Action / Use
Blocks dopamine (D2), acetylcholine, histamine, norepinephrine receptors in brain & periphery
Antipsychotic effects primarily from D2 blockade in the brain
Acute & chronic psychotic disorders
Schizophrenia spectrum disorders
Bipolar disorder (manic phase)
Tourette disorder
Agitation
Nausea/vomiting (blocks dopamine in chemoreceptor trigger zone of medulla)
Antipsychotics: First-Generation (Conventional) (-azine, -thixene, Loxapine, Haloperidol) Complications / Contraindications
Agranulocytosis
Nursing actions: Monitor for infection (CBC, discontinue if WBC < 3,000/mm³)
Anticholinergic Effects
Dry mouth, blurred vision, photophobia, urinary hesitancy/retention, constipation, tachycardia
Extrapyramidal Symptoms (EPS)
D - Benztropine (antiparkinsonian), diphenhydramine IM/IV
T - Switch to 2nd gen, eval every 3 mo., instruction
A - Eval first 2 mo., antiparkinsonians, beta-blockers, lorazepam/diazepam, suicide watch
P - Eval first mo., benztropine/trihexyphenidyl, fall prevention
Neuroendocrine Effects
Manifestations: Gynecomastia, weight gain, menstrual irregularities, galactorrhea
Neuroleptic Malignant Syndrome (NMS)
Manifestations: Sudden high fever, BP fluctuations, diaphoresis, tachycardia, muscle rigidity, ↓ LOC, coma
Nursing actions:
Stop antipsychotic immediately
Monitor vitals, apply cooling, give antipyretics
Administer dantrolene or bromocriptine for muscle rigidity
Treat arrhythmias as prescribed
Increase fluid intake
ICU transfer
Resume therapy only after 2 weeks; consider atypical antipsychotic
Orthostatic Hypotension
Sedation
Seizures
Severe Dysrhythmias
Monitor potassium and avoid concurrent QT-prolonging meds
Sexual Dysfunction (Lower dose or switch to high-potency agent)
Skin Effects (Photosensitivity, contact dermatitis)
Coma
Parkinson’s disease
Liver damage
Severe hypotension
Dementia
Use cautiously in:
Prostate enlargement
Heart disorders
Glaucoma
Paralytic ileus
Liver/kidney disease
Seizure disorders
Antipsychotics: First-Generation (Conventional) (-azine, -thixene, Loxapine, Haloperidol) Interactions / Admin
Other anticholinergic meds – ↑ anticholinergic effects
Client education: Avoid OTC sleep aids, antihistamines
Alcohol, opioids, antihistamines – additive CNS depression
Client education: Avoid alcohol, CNS depressants, driving/hazardous activity
Levodopa/dopamine agonists – counteract antipsychotic effects
Client education: Avoid concurrent use
Use AIMS to monitor for EPS
Differentiate between EPS vs worsening psychosis
May administer anticholinergics, beta blockers, benzodiazepines for EPS
Depot injections (haloperidol decanoate, fluphenazine decanoate) IM every 2–4 weeks
Lower doses with depot preparations reduce risk of adverse effects and tardive dyskinesia
Start with BID dosing → switch to bedtime dosing to ↓ daytime drowsiness
Client Education
Antipsychotics rarely cause dependence
Must take consistently as prescribed
Effects may be noticeable within a few days, but full improvement takes 2–4 weeks (sometimes several months)
Antipsychotics: First-Generation (Conventional) Meds
Prototype
Chlorpromazine
Other Medications
Haloperidol (high potency)
Fluphenazine (high potency)
Loxapine (medium potency)
Thioxthixene (high potency)
Perphenazine (medium potency)
A nurse is discussing manifestations of schizophrenia with a newly licensed nurse. Which of the following manifestations should the nurse identify as being effectively treated by first-generation antipsychotics?
Select all that apply.
a
Auditory hallucinations
b
Withdrawal from social situations
c
Delusions of grandeur
d
Severe agitation
e
Anhedonia
a Auditory hallucinations
c Delusions of grandeur
d Severe agitation
When taking action, the nurse should identify that auditory hallucinations, delusions of grandeur, and severe agitation are positive symptoms of schizophrenia that are effectively treated by first-generation antipsychotics.
A nurse is caring for a client who is currently taking perphenazine. Which of the following findings should the nurse identify as an extrapyramidal symptom (EPS)?
Select all that apply.
a
Decreased level of consciousness
b
Drooling
c
Involuntary arm movements
d
Urinary retention
e
Continual pacing
b Drooling
c Involuntary arm movements
e Continual pacing
Decreased level of consciousness = Neuroleptic malignant syndrome
Urinary retention = anticholinergic
1st vs 2nd vs 3rd Gen Atypical Antipsychotics
Primarily blocks dopamine (D2) receptors
No effect on NT systems (only treats positive symptoms)
Side Effects: Neuroendocrine, Neuroleptic Malignant Syndrome (NMS)
Primarily blocks dopamine (D2) and serotonin (5HT2A) receptors
Treats positive and negative symptoms
Side Effects: Metabolic Syndrome, Elevated Prolactin
Primarily PARTIALLY BLOCKS (partial agonist) dopamine (D2) (stabilizes levels) and block serotonin (5HT2A) receptors
Treats positive and negative symptoms
Side Effects: Metabolic Syndrome, Elevated Prolactin
What is the lead theory in what causes positive vs negative symptoms?
Mesolimbic (brain reward) pathway → TOO MUCH DOPAMINE
Mesocortical (thinking/emotion) pathway → TOO LITTLE DOPAMINE
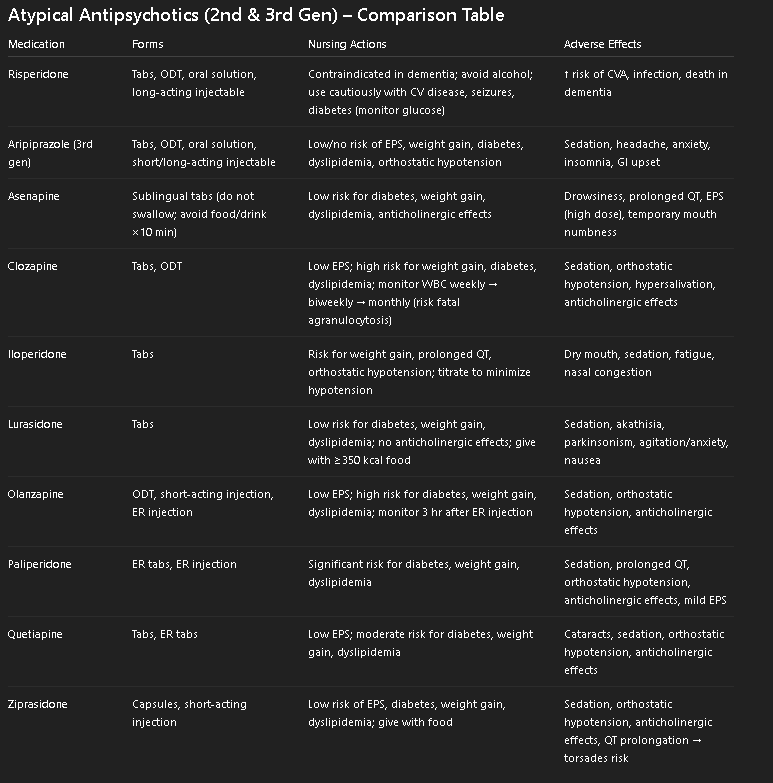
Antipsychotics: Second- and Third-Generation (Atypical) (-apine, idone, -ipra-) Action / Use
Second-gen: Block serotonin (main) and dopamine (lesser degree) receptors
Third-gen: Stabilize dopamine system as agonist + antagonist (partial agonist)
Both block norepinephrine, histamine, acetylcholine receptors
Treat positive & negative symptoms of schizophrenia spectrum disorders
Psychosis induced by levodopa therapy
Relief of psychotic manifestations in other disorders (e.g., bipolar disorder)
Impulse control disorders
Antipsychotics: Second- and Third-Generation (Atypical) (-apine, idone, -ipra-) Complications / Contradications
Agranulocytosis
Nursing actions: Monitor for infection (CBC, discontinue if WBC < 3,000/mm³)
Anticholinergic Effects
Dry mouth, blurred vision, photophobia, urinary hesitancy/retention, constipation, tachycardia
Orthostatic Hypotension
Metabolic Syndrome
New onset diabetes or loss of glucose control
Dyslipidemia → ↑ risk for cardiovascular disease
Weight gain
Agitation, Dizziness, Sedation, Sleep Disruption
Mild EPS (e.g., Tremor) - Use AIMS test
Elevated Prolactin Levels
Client education: Report galactorrhea, gynecomastia, amenorrhea
Sexual Dysfunction
Risperidone
Dementia (↑ risk of cerebrovascular accident, infection, death)
Avoid alcohol
Use cautiously with cardiovascular/cerebrovascular disease, seizures, or diabetes (monitor glucose carefully)
Antipsychotics: Second- and Third-Generation (Atypical) (-apine, idone, -ipra-) Interactions / Admin
Immunosuppressants (anticancer meds) – further suppress immune function
Nursing actions: Avoid with clozapine
Alcohol, opioids, antihistamines, CNS depressants – additive CNS depression
Client education: Avoid alcohol, CNS depressants, driving/hazardous activity
Levodopa & dopamine agonists – counteract antipsychotics
Nursing actions: Avoid concurrent use
Tricyclic antidepressants, amiodarone, clarithromycin – prolong QT interval → ↑ dysrhythmia risk
Nursing actions: Avoid combining with other QT-prolonging agents
Barbiturates & phenytoin – ↓ levels of aripiprazole, quetiapine, ziprasidone
Nursing actions: Monitor effectiveness
Fluconazole – ↑ levels of aripiprazole, quetiapine, ziprasidone
Nursing actions: Monitor effectiveness
Depot/long-acting injections:
Risperidone: IM every 2 weeks
Paliperidone ER injection: every 28 days
Invega Trinza (paliperidone palmitate, generic): every 3 months
Aripiprazole LAI: monthly
Therapeutic effect: 2–6 weeks after first depot dose
Use orally disintegrating tablets if client might “cheek” or has difficulty swallowing
Administer lurasidone and ziprasidone with food for absorption
Monitor cost barriers → may require case management support
Client Education
Start with low dose, titrate gradually (“Start low and go slow”)
Take consistently as prescribed
If taking asenapine → avoid eating/drinking ×10 min after dose
Antipsychotics: Second- and Third-Generation (Atypical) Meds
Prototype
Risperidone
Other Medications
Second-generation: Asenapine, Clozapine, Iloperidone, Lurasidone, Olanzapine, Paliperidone, Quetiapine, Ziprasidone
Third-generation: Aripiprazole, Cariprazine, Brexpiprazole
Adjunct Medications for Psychotic Disorders
Antidepressants (STaMiNA)
Example: Paroxetine
Purpose: Treat depression in clients with psychotic disorders
Nursing actions:
Monitor for suicidal ideation (esp. at start of therapy)
Report worsening depression
Client education: Avoid abrupt cessation (prevents withdrawal)
Mood Stabilizers & Benzodiazepines
Examples: Valproate, Lamotrigine, Lorazepam
Purpose: Treat anxiety, agitation, some positive/negative symptoms
Nursing actions: Use cautiously in older adults
Client education:
Sedative effects possible
Case management & follow-up support
Group, family, individual psychoeducation (problem-solving, social skills, ADLs)
Determine to which category each medication listed below belongs. Drag each medicate to the desired image.
Risperidone
Haloperidol
Quetiapine
Loxapine
Olanzapine
Clozapine
Typical antipsychotics
Atypical antipsychotics
Typical antipsychotics
Loxapine
Haloperidol
Atypical antipsychotics
Clozapine
Olanzapine
Quetiapine
Risperidone