energy transfer y13
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
What is homeostasis?
The maintenance of constant internal conditions to prevent damage to cells e.g temperature, pH, glucose conc
What organs are involved in homeostasis and how?
muscles - maintain body temp
Liver + pancreas - adjust glucose levels
Kidneys - remove urea, adjust conc of inorganic ions + water potential of blood
Pottery gland - produces hormone controlling water balance by targeting kidneys
Lungs - remove co2, water lost when exhale
Skin - adjusts body temp, water + ions lost when we sweat
What are the components of the blood?
plasma
Rbcs
WBCs
Platelets
What is the collision theory?
Metabolic rate being increased by temp
increased temp=increased rate of reaction=increased kinetic energy of molecules= more successful collisions + reactions
Temp too high= reaction stops due to hydrogen bonds holding enzyme together breaking, causing denaturation
What is meant by core body temperature?
Maintenance of constant temperature of the brain and other internal organs of the chest and abdomen
(Allows mammals to be independent of changes to external temperatures)
Why is pH important in homeostasis?
fluctuation in blood pH causes denaturation of enzymes and proteins= lower rate of reaction
Optimum pH= faster metabolic reactions
How do you calculate pH?
pH=-log10[H+]
H+ means conc of hydrogen ions
Why is blood glucose conc important in homeostasis?
too high=reduced water potential of blood= water moves out of blood by osmosis= cells die
Too low= cells have lack of energy from respiration= normal cell activities unable to be carried out
Unavailable glucose= brain cells can’t function= mammal loses consciousness
What is the purpose of negative feedback?
To restore the system back to its original level e.g regulating blood conc of co2
What does positive feedback do?
Makes changes in the same way the deviation in the norm had, amplifying change e.g release of hormones
Is usually harmful, but useful when body needs to react quickly
What is hypothermia?
The fall in body temp due to prolonged exposure to cold weather, this change is too large to counteract
What is glucagon?
a hormone
A protein
Synthesised by ribosomes
Travels to target organ/ cell in blood where it binds to receptor due to being complementary
What is glucose?
a carbohydrate (disaccharide/ monosaccharide)
Used in respiration for the release of energy
Present in the blood
Contains 38 mols of ATP
Stored in muscles and liver as glycogen
What is glycogen?
Made up of glucose
Stores carbohydrates
Is compact, insoluble and easily hydrolysed
What does insulin do?
Decreases blood glucose levels by binding to hepatocytes (receptors on cell membranes of muscle and liver cells) which increases permeability of membrane to glucose so more glucose taken up by cell
This involved increasing number of channel proteins in cell membrane
Also activates enzymes in muscle and lice cells for glycogenesis
Increases rate of respiration of glucose
What is the normal blood glucose concentration in humans?
90mg of glucose in 100cm³ of blood
How would a fall in glucose effect body cells?
water potential becomes less negative
Water moves out of blood into cells
Rate of respiration slows down
How would a rise in glucose effect body cells?
water potential becomes more negative
Water moves out of cells into blood
Rate of respiration increases
What hormones are involved in homeostasis?
Insulin and glucagon
Where is glucagon and insulin stored?
In the pancreas
How does glucagon increase blood glucose levels?
Causes glycogen to turn into glucose by glycogenolysis
How does the liver regulate blood glucose conc?
Liver receives all glucose absorbed in blood from intestines via hepatic portal vein
hepatic vein transports deoxygenated blood to vena cava
Gall bladder stores bile
Hepatic artery transports oxygenated blood to liver
Hepatic and cystic ducts provided bile to intestines
Hepatic portal vein carries glucose rich blood from intestines (why we don’t go into diabetic coma after meals)
Small intestine turns proteins to amino acids, carbs into monosaccharides, fibre into digestive transit, fat into fatty acid and glycerol
How can glucose be added to the blood?
glycogenolysis - hydrolysing glycogen to glucose by breaking glycosidic bonds
Gluconeogenesis - converting non carbohydrate substances to glucose
How can glucose be removed from the blood?
glycogenesis - condensing glucose and storing it as insoluble glycogen
Converting glucose to fat
Using glucose as a fuel for cellular respiration
How does the pancreas regulate blood glucose conc?
pancreas secretes insulin and glucagon
These hormones have opposite effects on blood glucose levels (negative feedback)
How are hormones created in the pancreas?
By a group of cells called the islets of langerhans
What are the islets of langerhans made up of?
alpha cells in the centre that secrete glucagon to increase blood glucose conc
Beta cells in the centre that secrete insulin to reduce blood glucose conc
How does insulin lower blood glucose concentration?
binds to hepatocytes
This increased permeability of muscle and liver cell membranes
Allows more glucose to be taken up by the cells from the increased number of channel proteins
Insulin also causes glycogenesis (converts glucose into glycogen)
How does glucagon raise blood glucose concentration?
binds to hepatocytes on liver cells
This causes glycogenolysis (hydrolysis of glycogen into glucose)
Glucagon also decreases the rate of respiration in cells so less glucose is needed via gluconeogenesis
What are glucose transporters?
Channel proteins allowing glucose to be transported across a cell membranes by facilitated diffusion
E.g GLUT4 in skeletal and cardiac muscle cells
What does GLUT4 do when insulin is low?
GLUT4 activates from insulin binding to receptors on cell surface membranes
This causes GLUT4 to move to membrane to transport more glucose into the cell
Causes rapid removal of glucose from blood
Why is either storing glucose or using it for respiration important?
To maintain the concentration gradient
What happens due to hyperglycaemia (rising blood glucose conc)?
beta cells secreted insulin into blood
Insulin binds to glycoprotein receptors on cell surface membranes, triggering cell response
Glucose transporters move to cell membrane
Enzymes increase rate of glycogenesis
What happens due to hypoglycaemia (falling blood glucose conc)?
alpha cells secrete glucagon into blood
glucagon binds to hepatocytes on liver cells, triggering cell response
Enzymes speed up glycogenolysis (breaking glycogen)
Glucagon increases rate of gluconeogenesis (making new glucose)
Where is adrenaline produced and when is it secreted?
In adrenal glands in kidneys
when blood glucose conc is low
Stressed
Exercising
What does adrenaline do?
binds to hepatocytes, activating glycogenolysis and inhibiting glycogenesis
This causes glucose conc to increase
Also causes fight or flight due to more glucose being able to be used in respiration for muscles
What is cAMP and how is it activated?
Is a second messenger that causes the breakdown of glycogen to glucose
adrenaline and glucagon binding to specific receptors on cell surface membranes
This activates enzymes that accelerate the production of cAMP
What is diabetes?
A metabolic disorder caused by either a lack of insulin or a loss of responsiveness to insulin, resulting in an inability to control blood glucose levels
What is type 1 diabetes?
usually occurs in childhood
Is an autoimmune response where immune system attacks beta cells in islets of langerhans, resulting in the inability to secrete insulin
What is type 2 diabetes?
occurs later in life
Is a loss of responsiveness to insulin and can be due to insulin deficiency
Caused by poor diet and obesity
How can diabetes be treated?
insulin injections taken 2-4 times a day
Automatic blood glucose metres combined with an insulin pump implanted below the skin (is automatic)
What other health issues can type 2 diabetes cause?
heart attack
Kidney disease / failure
What should be altered in diets to reduce risk of type 2 diabetes?
higher intake of fibre
Reduce intake of carbohydrates, sugars, adults, fats
How have some food companies attempted to make food products healthier?
using sugar alternatives to sweeten foods and drinks
Reducing sugar, salt and fat content of foods
What is the normal glucose level in urine?
Between 0-0.8mM
any higher may indicate diabetes
Why is the main function of the kidneys?
To filter waste products out of the blood (ULTRAFILTRATION) and reabsorb useful solutes (SELECTIVE REABSORPTION)
Regulates water and ion content of the blood to keep water potential and pressure of the blood constant
Where are nephron tubules located?
In the kidneys
Fill in the blank boxes showing the parts of the nephron and what they do
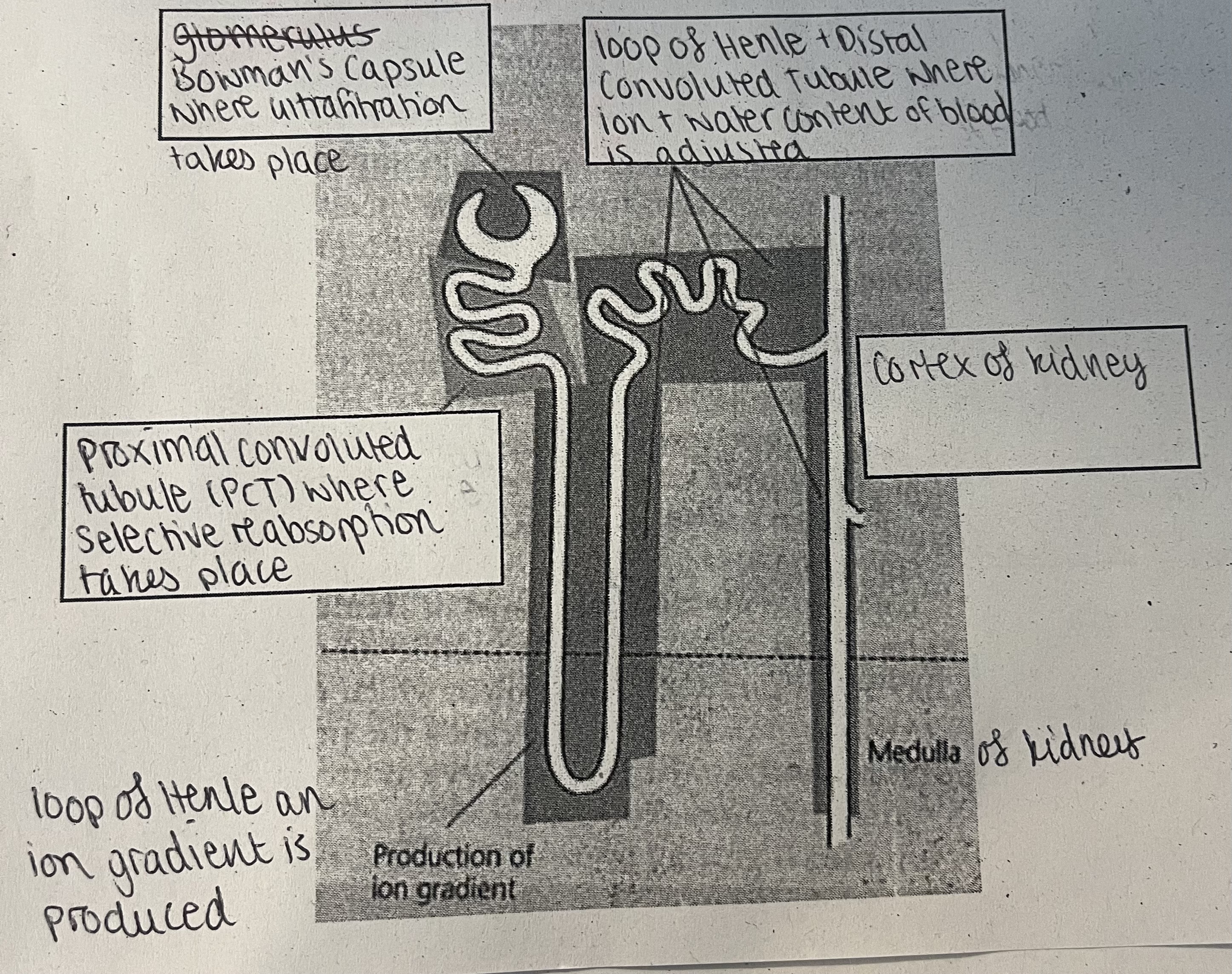
What is the first stage of filtration in the kidneys?
ULTRAFILTRATION in the nephron:
blood enters small arterioles which then splits into a knot of blood vessels called the glomerulus
This creates higher pressure in the glomerulus, causing liquid and small molecules (e.g glucose) to be forced out of the glomerulus from the high hydrostatic pressure and into the bowman’s capsule
What three layers of tissue does filtrate need to pass through to get into the bowman’s capsule?
capillary endothelium
Basement membrane (where filtration takes place)
Epithelium of the bowman’s capsule
What is the second stage of filtration in the kidneys?
SELECTIVE REABSORPTION
Only useful substances in the filtrate are absorbed into the blood in the proximal convoluted tubule (PCT)
How are these useful substances transported into the blood?
ACTIVE TRANSPORT → sodium ions and glucose molecules transported from glomerular filtrate into PCT by symports
Sodium ions actively transported into the blood by a sodium pump, whilst also transporting potassium ions in the opposite direction
FACILLITATED DIFFUSION → glucose transported out of the PCT and into the blood
What is the third stage of filtration in the kidneys?
an ion gradient is produced in the medulla by the loop of henle
At the ascending limb, sodium ions are active pumped out into the medulla → ascending limb is impermeable to water so water potential in medulla is low due to the limb being highly permeable to sodium ions
Water moved out of the descending limb by osmosis as water potential is lower in the medulla than the limb as the limb is highly permeable to water → this limb is slightly permeable to sodium ions so they move out by diffusion
Glomerular filtrate is now more concentrated due to ions being unable to diffuse out because of the descending limb being impermeable to them
The water moved into the medulla is absorbed into the blood through the capillaries
What is the fourth stage of filtration in the kidneys?
adjustment of the water and ion content of the blood to keep internal environment constant
Water moves out of DCT and collecting duct by osmosis, and absorbed into the blood due to the lower water potential in the medulla
The ascending limb is more permeable to salts and less permeable to water causing sodium and chloride ions to move out actively into surrounding tissue
Water passes out of the descending limb by osmosis, causing the filtrate to become more concentrated
This results in the countercurrent multiplier mechanisms where the solute concentration is lower in the ascending limb that the descending limb
What is ADH
A hormone that stops you urinating
How is ADH released?
when osmoreceptor cells in the hypothalamus detect a decrease in water potential, water moves out of the osmoreceptor cells by osmosis which decreases their volume
This send a signal to the posterior pituitary gland which releases ADH to the kidneys through the blood
What happens when ADH reaches the kidneys?
binds to receptors on the plasma membrane of cells in the DCT and collecting duct
This causes channel proteins callled aquaporins to make the DCT and collecting duct more permeable to water
Thus results in water being absorbed into the medulla of the kidney and is to the blood by osmosis
This produces a small amount of concentrate during so less water is lost from the body
What is osmoregulation?
the regulation of water potential in the blood to be kept constant
→ water potential too low causes more water being absorbed into the blood from nephrons = more concentrated urine
→ water potential too high causes less water being absorbed into the blood from nephrons = more dilute urine
this happens in the Loop of Henle and the collecting duct
What is the function of the loop of henle?
to create and area of high concentration in the medulla so water can be absorbed by osmosis so concentrated urine can be produced
What happens when the body is dehydrated?
blood water content is low
Blood volume low so ADH secretion Increases
1. ADH increases permeability of DCT and collecting duct to water
2. Water moves out of tubules into tissue fluid of medulla as the water potential is more negative here due to the sodium ion conc
3. This decreases volume of urine produced and increased conc of dissolved substances in urine making the urine hypertonic to blood plasma
What happens when the body is hydrated?
high blood water content
High blood volume so ADH secretion decreases
ADH decrease permeability of DCT and collecting duct to water
Less water moves out of tubules into tissue fluid of medulla
This increases the volume of urine produced and decreases the conc of the dissolved substances in it
Urine produced it hypotonic to blood plasma
What does hypertonic mean?
More concentrated than blood plasma
What does hypotonic mean?
Less concentrated than blood plasma
What is the chemical and word equation for photosynthesis?
Word: carbon dioxide + water → glucose + oxygen
Chemical: 6co2 + 6h20 → c6h12o6 + 6o2
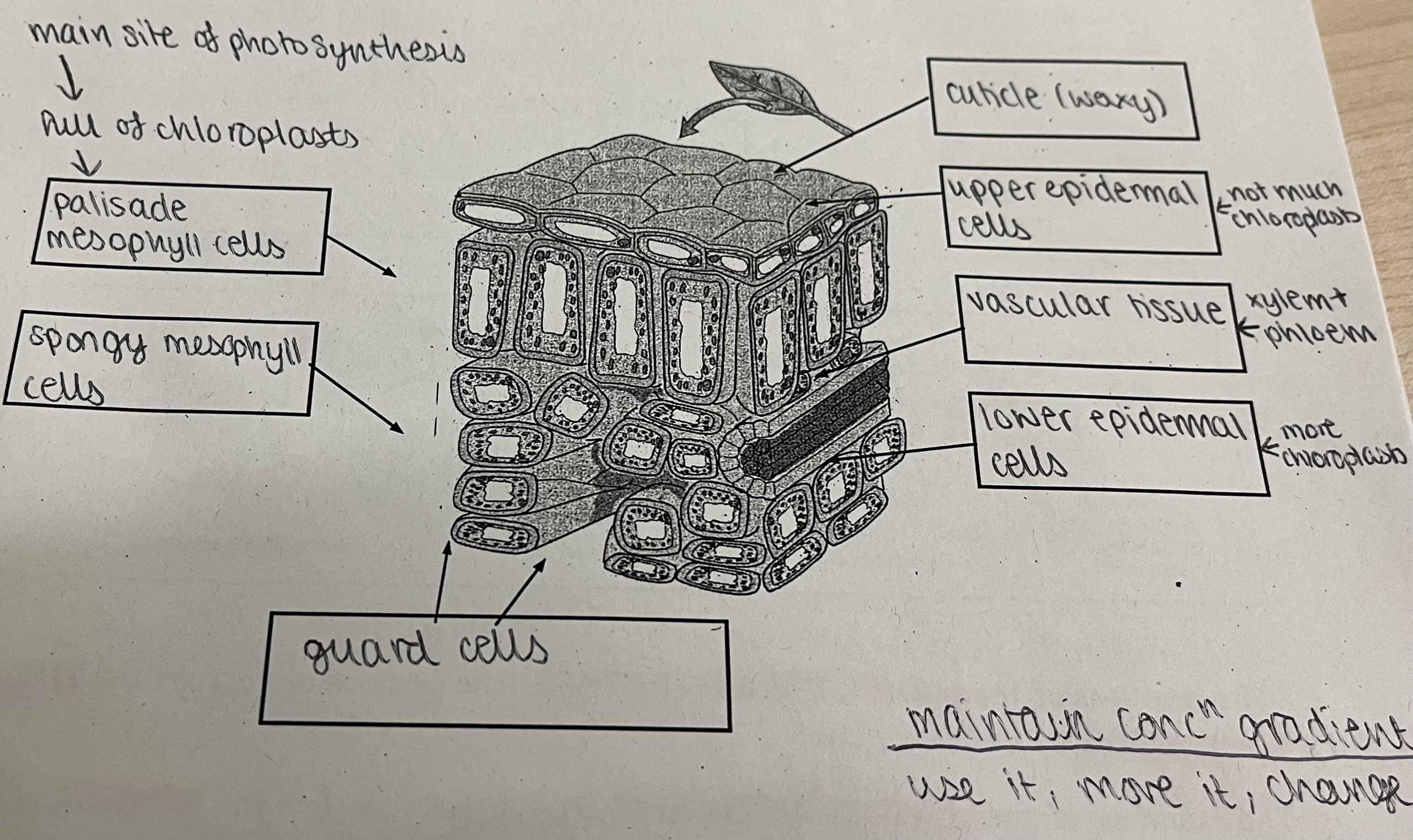
What are the adaptations of a leaf?
large surface area to maximise light capture
Stacks of chloroplasts to maximise light absorption
Stomata and waxy cuticle to deduce water loss
Thin to shorten diffusion pathway, increasing rate of diffusion
What is the structure of a leaf?
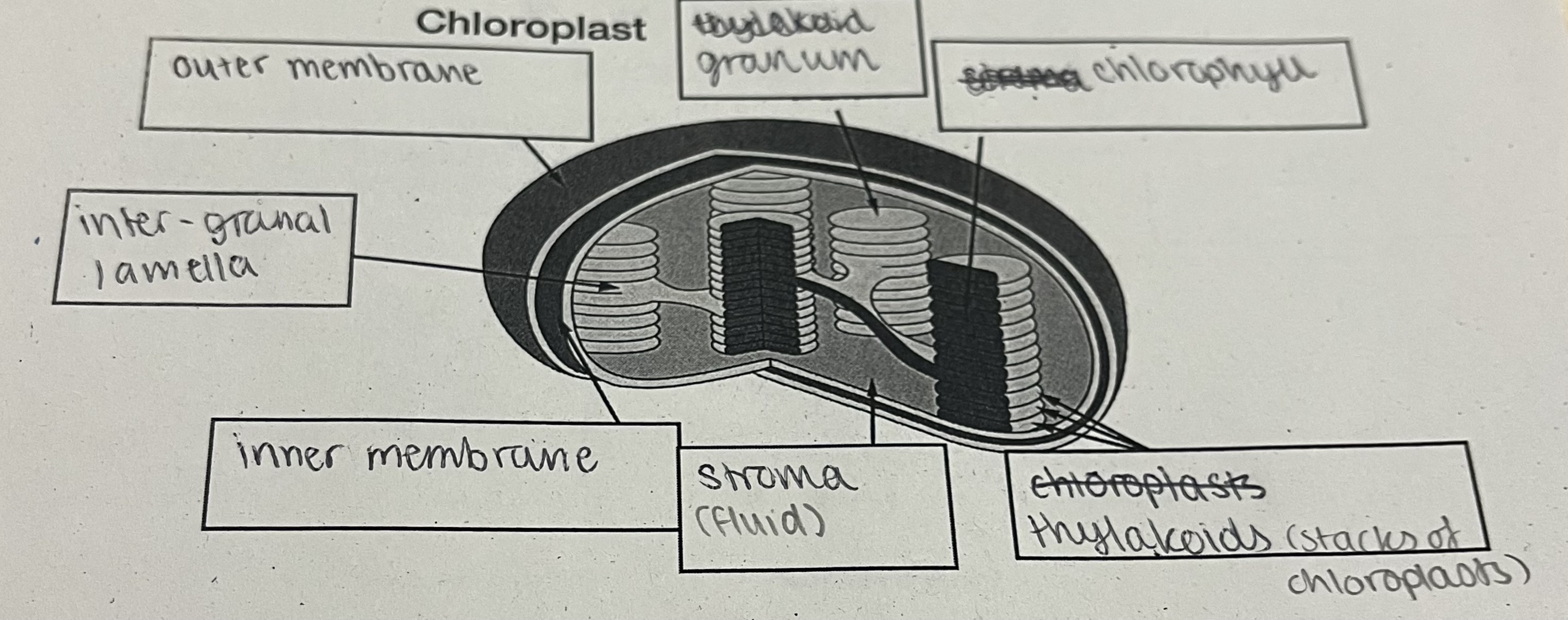
What is the structure of a chloroplast?
What is autotrophic nutrition?
Where organisms make their own food where they use a source of energy to make complex organic molecules from inorganic raw materials
How photoautotrophs make their own food?
e.g green plants and algae
Use light energy to synthesis their own organic materials
What are the two stages of photosynthesis?
light dependant stage - takes place on and across the thylakoid membranes of the chloroplast, producing NADPH and ATP to feed the…
Light independent stage - take place in the stroma of the chloroplast, producing ADP+P and NADP^+
What are photosystems?
The combination of the photosynthetic pigments in chloroplasts and the proteins they are attached to in the thylakoid membrane
What are the two redox reactions?
Oxidation - LOSS
loss of electrons and hydrogen
Gain of oxygen
Reduction - GAIN
gain of electrons and hydrogen
Loss of oxygen Reduction
REDOX REACTIONS HAPPEN DURING PHOTOSYNTHESIS
What are co enzymes?
Molecules that aid the function of an enzyme by transferring a chemical group from one molecule to another
What co enzyme is involved in photosynthesis?
NADP which transfers hydrogen from one molecule to another which reduces and oxidises substances
How do plants use energy during the light dependant reaction in the thylakoid membranes?
PHOTOIONISATION
light is absorbed by the chlorophyll, exciting some electrons in the chlorophyll
This causes the electrons to be released from the chlorophyll
DEHYDROGENATION
Some energy from the released electrons are used to:
PHOTOPHOSPHORYLATE ADP into ATP
NAD into NADPH
During this, water is oxidised to become oxygen as hydrogen is removed (PHOTOLYSIS)
What is the equation for phosphorylation?
ADP + Pi → ATP
What are the 2 ways in which photophosphorylation happens?
Non cyclic photophosphorylation
Cyclic phosphorylation
What is non cyclic photophosphorylation?
Electron has lots of energy from light absorption in the chlorophyll
Electron then goes through a series of electron carriers, losing energy at each one
Hydrogen ions are removed as a result of a loss of energy from electrons
Electrons are now negatively charged
Hydrogen ions reach ATP synthase which produces ATP
The negatively charged electron leaves and meets NADP and a hydrogen ion, producing NADPH
Photolysis splits water to make ½ O² , 2H^+ and 2e^- as waste products of photosynthesis
What is cyclic photophosphorylation?
the electrons released are not donated to NADP but are passed back to PSI via electron carriers
This means the electrons are continuously recycled and flow repeatedly through PSI
This produces small amounts of ATP the same way as non cyclic photophosphorylation (movement of protons across thylakoid membrane)
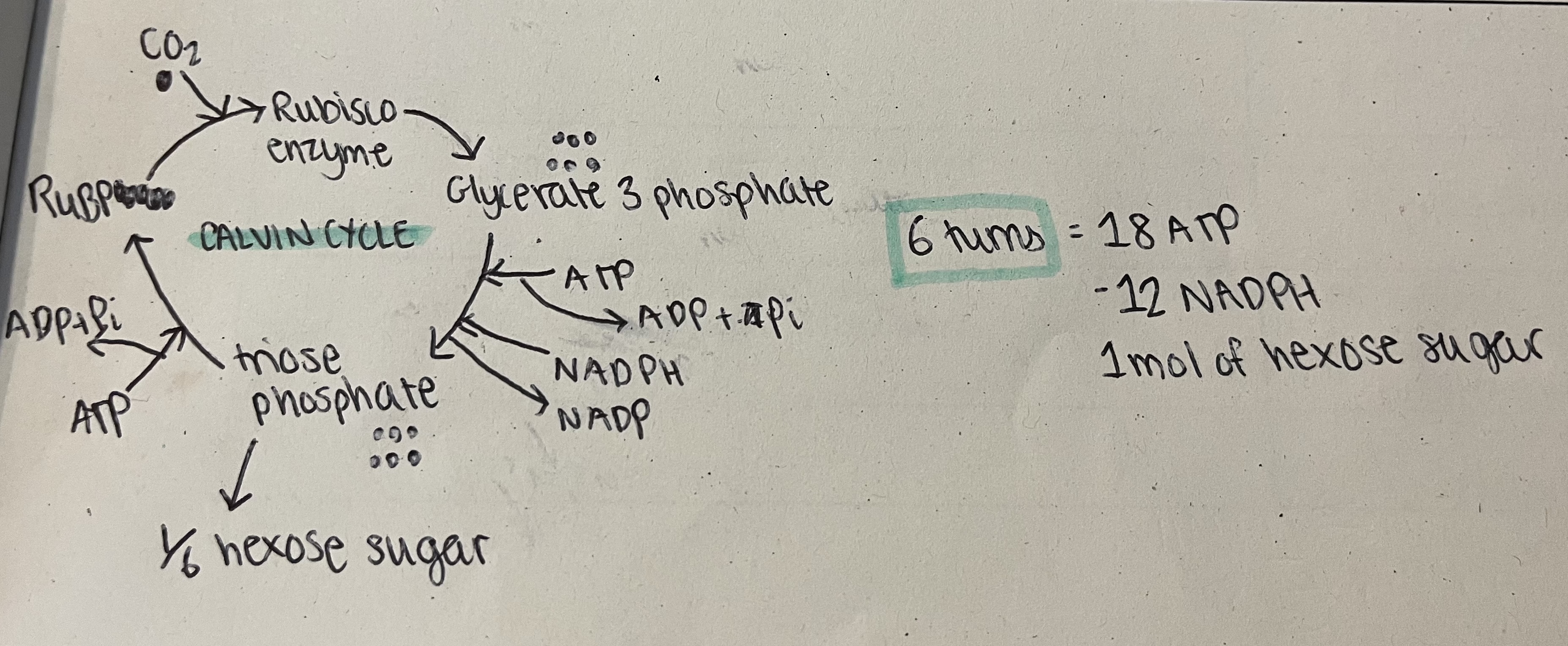
What are light independant reactions? (CALVIN CYCLE)
Co2 combines with ribulose bisphosphate (RuBP) to produce 2 mols of glycerate 3-phosphate (GP), catalyses by the rubisco enzyme
Energy from ATP and NADPH from light dependant reactions used to reduce GP to the sugar triose phosphate (TP)
NADP and ADP and Pi return to light dependant stage to collect more electrons
1/6 TP converted into useful organic substances, meaning the cycle needs to turn six times to make one hexose sugar
5/6 TP used to regenerate RuBP by using some ATP
How can the Calvin Cycle be investigated?
supply a plant with radioactively labelled CO2
Expose leaves for different amounts of time
Remove leaves and analyse them for radioactive substances
What would happen when the plant is deprived of light?
GP increases due to no ATP and reduced NAPD is produced from light dependant reaction used to convert GP into TP
Decreased RuBP as it is converted into GP which is then converted into TP