Organisms response - Control of blood water potential
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
What is osmoregulation?
The control of water potential of body fluids
What are osmoreceptors?
They detect decreases in osmotic pressure of body fluids and inform the brain we are thirsty
How can the normal water pot of the blood be affected?
It depends on the conc of solutes like glucose and proteins etc. A rise in solute conc can lower water pot
What can cause a rise in solute levels in the blood?
- Not drinking enough water
- Sweating a lot
- Eating a salty meal
Where are osmoreceptors located?
In the hypothalamus
Where is ADH secreted from?
Posterior pituitary gland
How do the osmoreceptors respond to low water potential? (general)
1. They send a nerve impulse along a sensory neurone to the posterior pituitary gland
2. The gland then releases antidiuretic hormone (ADH)
3. This enters the blood and travels around the body to the kidneys
4. They also send signals to the thirst centre of the brain
5. When we drink more water, they detect this and send fewer signals to the pituitary gland to make ADH so less ADH is produced
How does the kidney respond to the release of ADH?
1. ADH effects the permeability to water of the cells in the distal convoluted tubule and collecting duct
2. ADH binds to specific cell-surface receptors which activates enzyme phosphorylase
3. This enzyme phosphorylates vesicles containing aquaporin molecules which exist in the collecting duct
4. This causes the aquaporins fuse with the cell-surface membrane making the cells more water permeable
5. More water thus leaves the collecting duct via osmosis
6. More concentrated urine is produced
7. When we drink and less ADH is produced, the permeability of the collecting duct returns to normal and more dilute urine is produced
Diagram to show how ADH affects aquaporins.
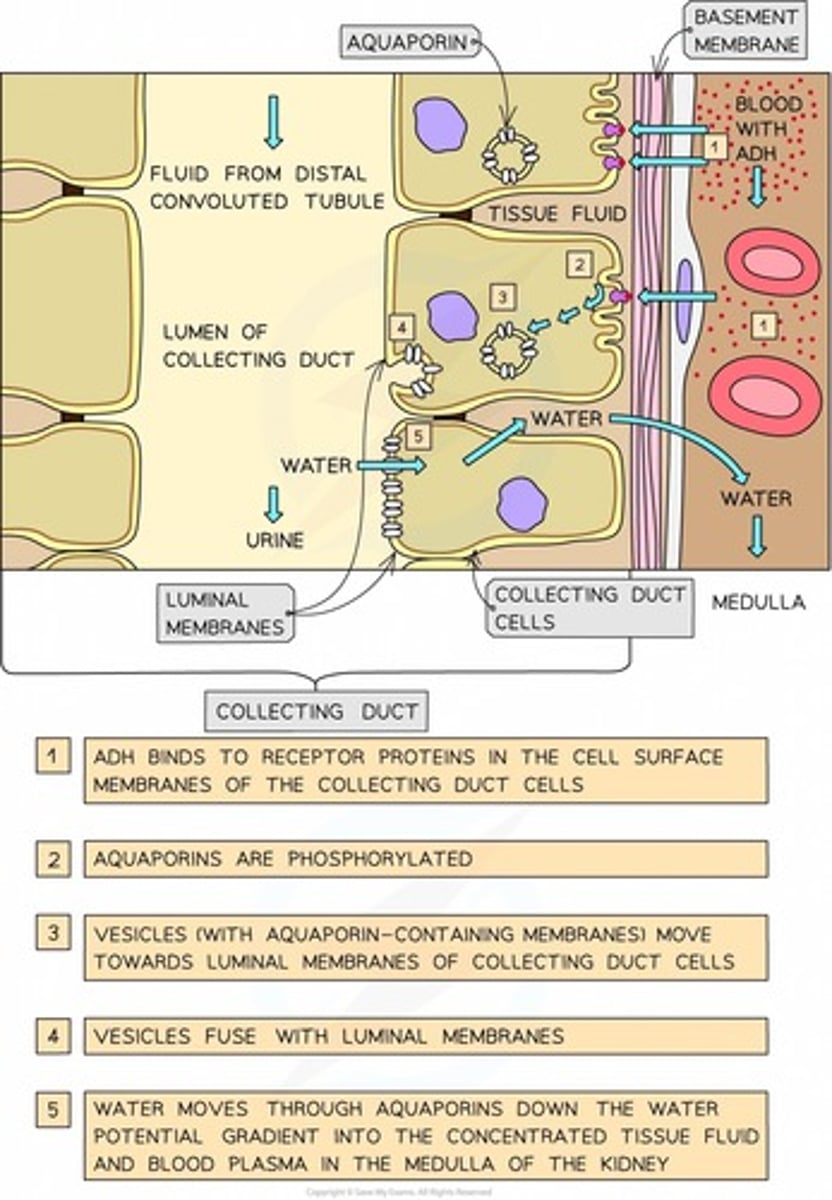
What is ADH?
Anti-diuretic hormone - it controls the concentration of urine and is released into the bloodstream by the pituitary gland
Which membrane does ADH cause to become more permeable?
The luminal membrane on the collecting duct (those facing the lumen of the nephron)
What are aquaporins?
Water permeable channels
What functions do the kidneys perform?
- Involved in osmoregulation
- Act as an excretory organ
How do the kidneys act as an excretory organ?
They excrete toxic waste products of metabolism such as urea and substances in excess of requirements such as salts
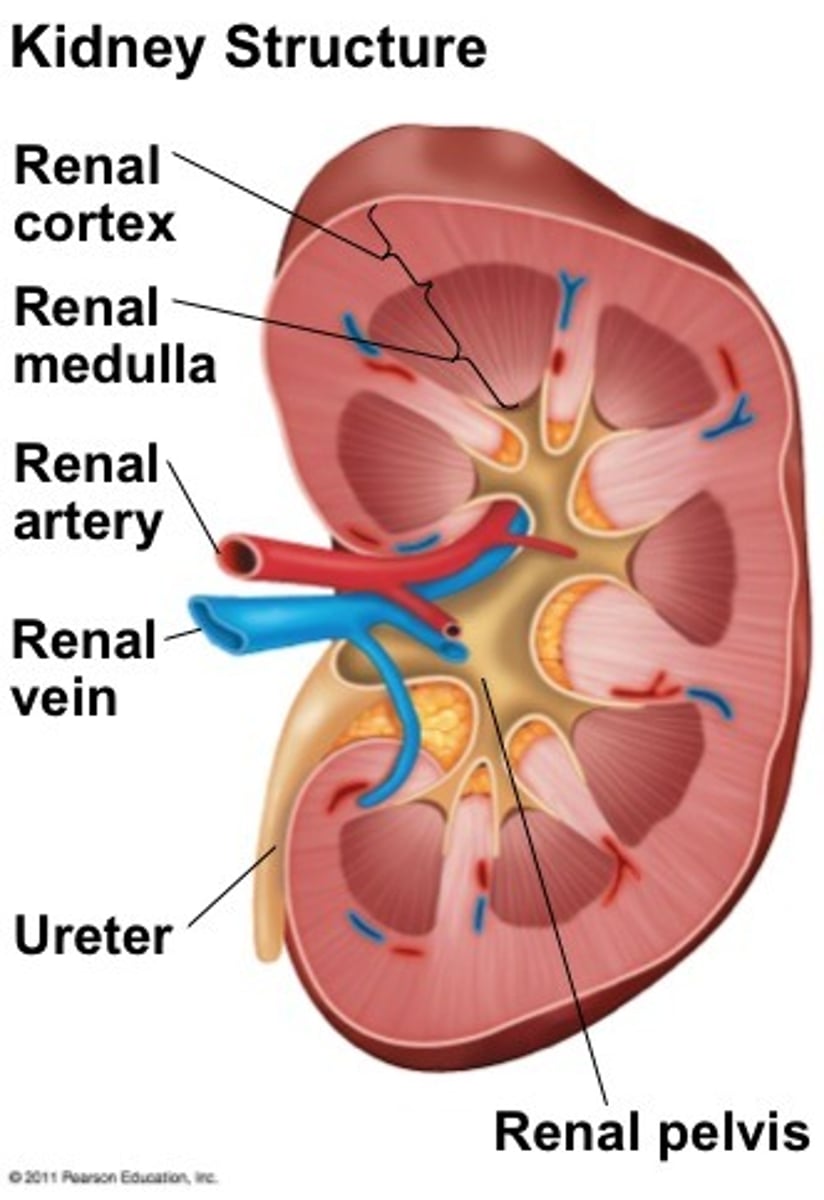
Describe the outer layer of the kidneys.
This is a tough membrane called the fibrous capsule
What are the three main parts within the kidney?
- Cortex
- Medulla
- Reval pelvis
Describe the structure of the cortex.
It contains glomerulus, bowman's capsule, proximal convoluted tubule and distal convoluted tubule of the nephrons
Describe the structure of the medulla.
Contains the loop of Henle and the collecting duct of the nephrons
Describe the structure of the renal pelvis.
It is where the ureter joins the kidney
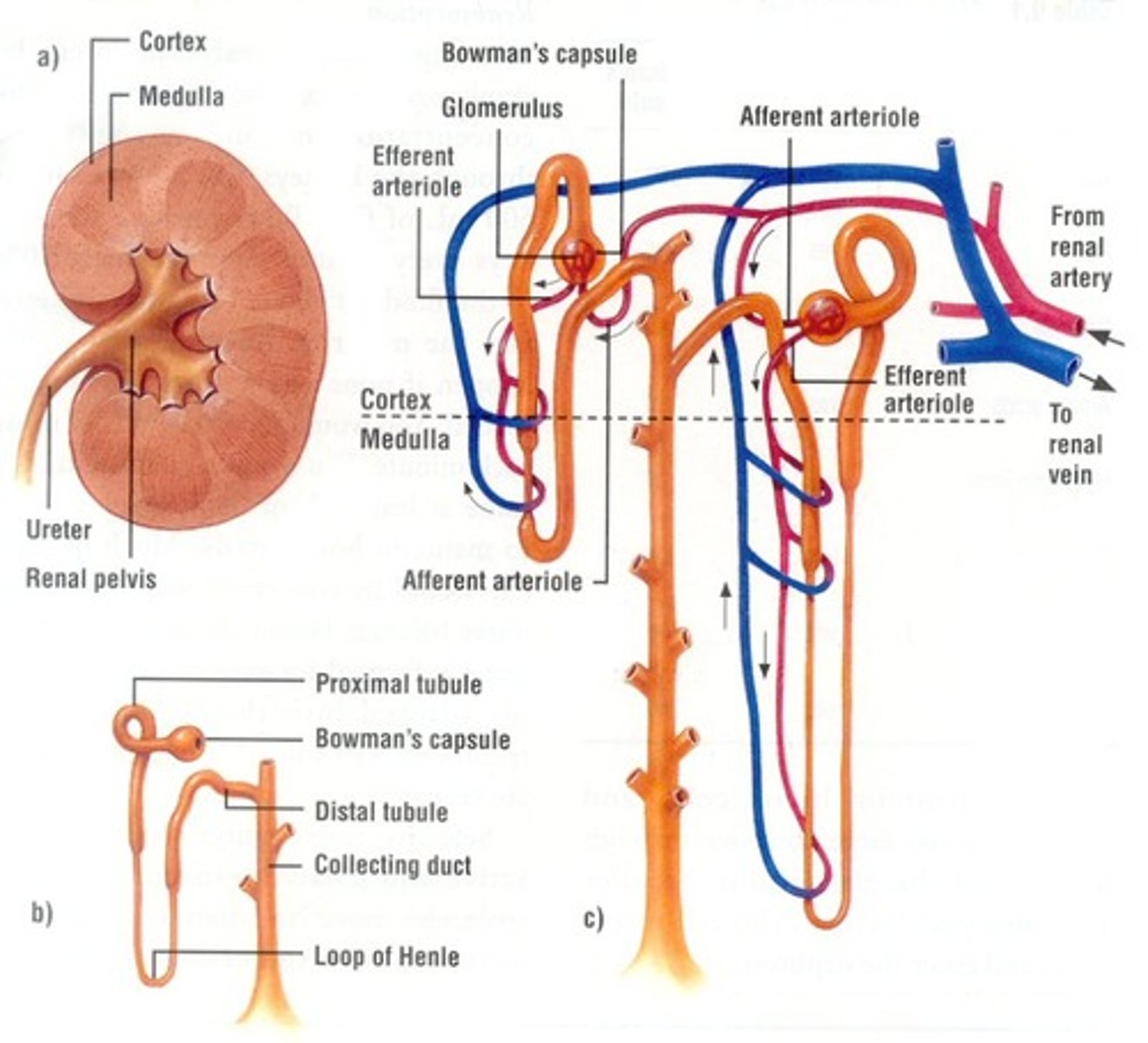
Structure of the kidney.
What are nephrons?
Functional filtration units in the kidneys
Location of nephrons in the kidney.
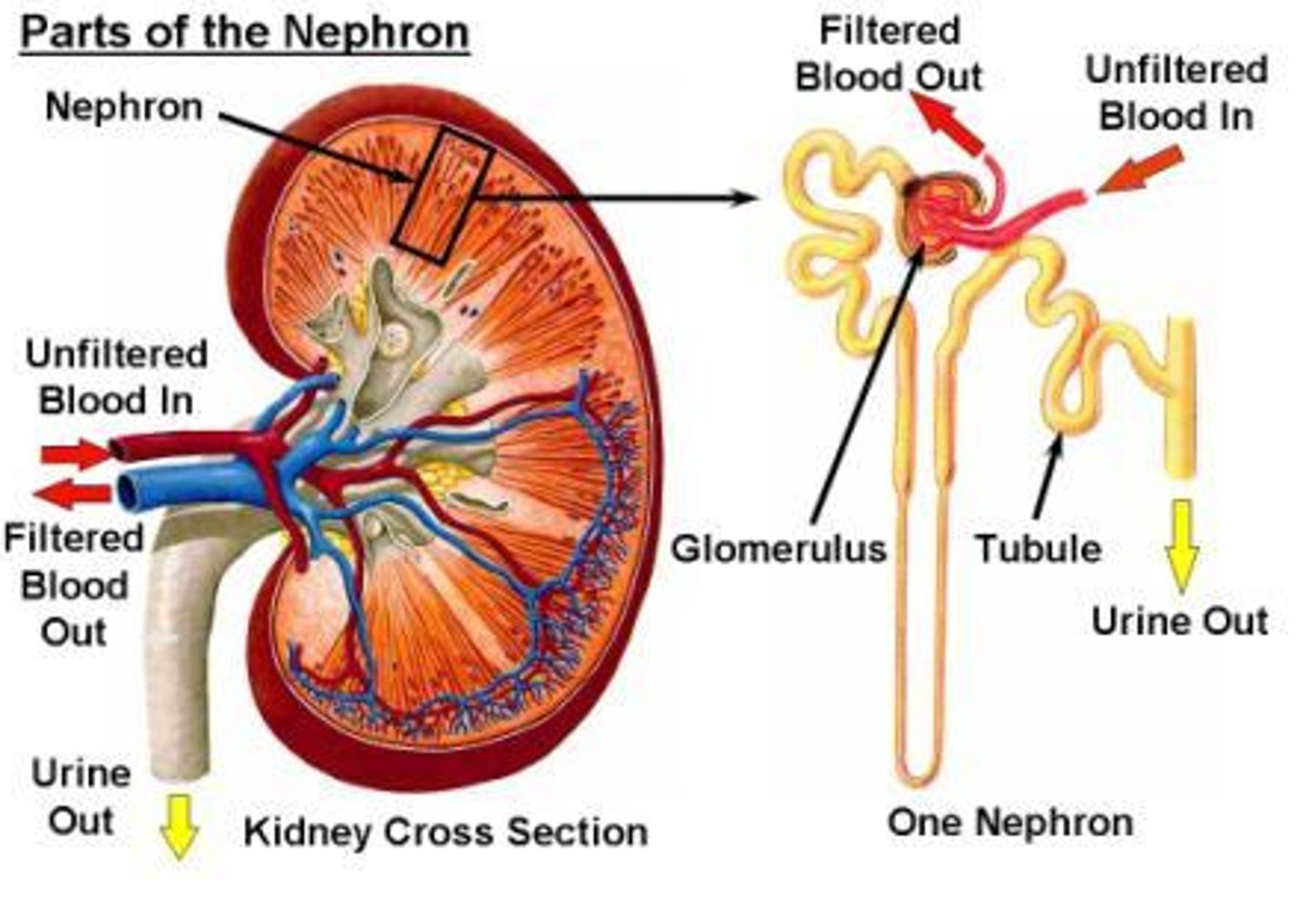
List the parts of a nephron.
- Glomerular
- Bowman's capsule
- Proximal Convoluted Tubule
- Loop of Henle
- Distal Convoluted Tubule
- Collecting duct
Labelled nephron.
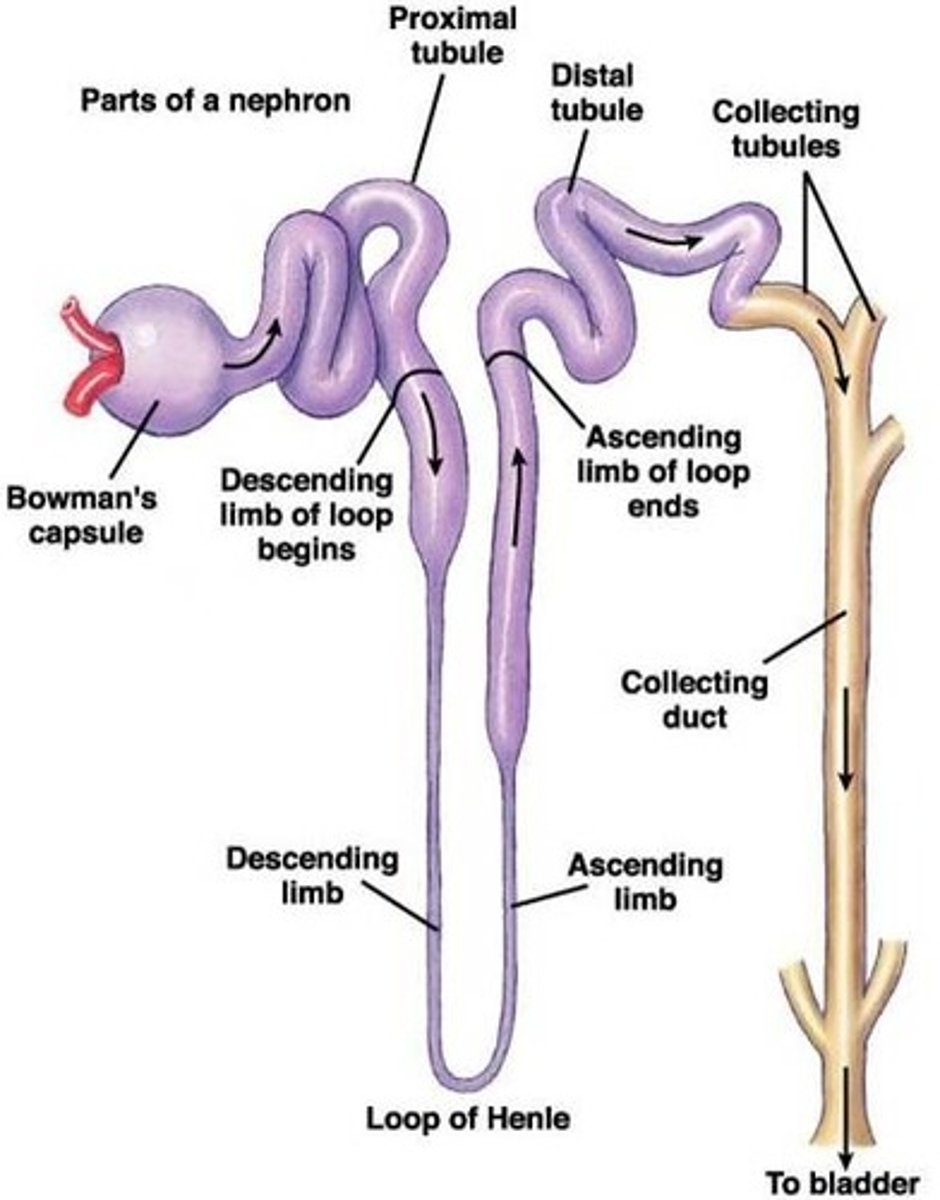
What parts of the nephron are located in the cortex?
- Distal Convoluted Tubule
- Glomerular
- Bowman's capsule
- Proximal Convoluted Tubule
What parts of the nephron are located in the medulla?
- Collecting duct
- Loop of Henle
Describe the golmerulus.
Cluster of capillaries
Describe the journey of the blood around the kidney.
- Blood starts from the renal artery
- Travels through the arterioles to the capillaries (glomerulus)
- After the glomerulus the blood enters an efferent arteriole
- Blood then enters the renal vein
What are the nephrons responsible for?
The formation of urine
What are the four stages in the formation of urine?
1. Ultrafiltration
2. Selective reabsorption
3. Maintaining of an Na+ gradient in the loop of henle for the reabsorption of water
4. Reabsorption of water from the collecting duct
What is ultrafiltration?
Filtration of the blood at a molecular level under pressure
Where does ultrafiltration take place?
Bowman's capsule
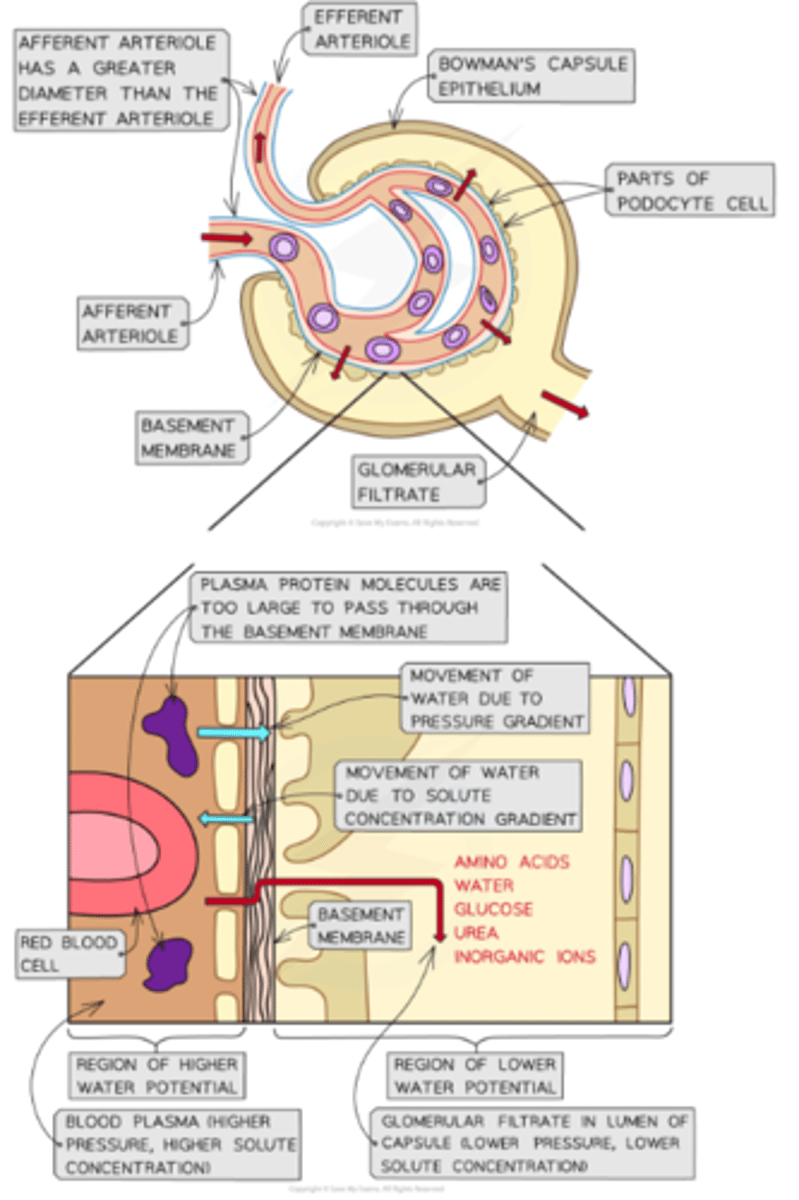
What separates the blood in the glomerular capillaries from the bowmans capsule?
A 2 cell thick layer with a basement membrane in between them
Describe the layers of the membrane between the golmerular capillaries and the bowmans capsule.
- First layer is the endothelium of the capillary
- Next layer is the basement membrane
- Final layer is the epithelium of the bowmans capsule
Describe the epithelial cells on the bowmans capsule.
They have many villi like projections with gaps between them called podocytes
What characteristics of the podocytes, endothelial and epithelial cells allows substances dissolved in blood plasma to enter the bowmans capsule?
All of these structures either have holes in them or holes between them to allow these substances to move through
What is the fluid that enters the bowmans capsule from the blood called?
The golmerular filtrate
What are the main substances in the glomerular filtrate?
- Amino acids
- Water
- Glucose
- Urea
- Inorganic ions
Why do a lot of elements in the blood not pass into the bowmans capsule?
They are too large to fit through the holes
What element of the barrier between the blood and the bowmans capsule prevents the large molecules getting through?
The basement membrane
Why does ultrafiltration occur?
Due to the differences in water potential between the plasma in the glomerular capillaries and the filtrate in the bowman's capsule
What are the two factors that effect water potential in the bowmans capsule?
- Pressure
- Solute concentration
How does pressure impact the movement of water between the golmerular capillaries and the bowmans capsule?
- BP high in capillaries
- This raises water pot in the capillaries to above that in the bowmans capsule
- As a result water moves into capsule
How does solute concentration impact the movement of water between the golmerular capillaries and the bowmans capsule?
- Solute conc in blood is higher than in capsule
- As a result water moves from capsule into capillaries
What factor that impacts movement of water between the golmerular capillaries and the bowmans capsule is most influential?
Pressure. This means the net movement of water is from the blood into the bowmans capsule
Diagram to show movement of water between bowmans capsule and capillaries.
What is selective reabsorption?
The uptake of specific molecules and ions from the glomerular filtrate in the nephron back into the bloodstream
Why does selective reabsorption occur?
Many substances that end up in the glomerular filtrate actually need to be kept
Where does selective reabsorption occur?
In the proximal convoluted tubule
What substances are usually reabsorbed during selective reabsorption?
- Glucose
- Water
How does the selective reabsorption occur?
1. There are Na+/K+ pumps in the basal membrane
2. This moves Na back into the blood lowering the conc of Na inside the epithelial cells
3. This causes the Na ions from the glomerular filtrate to diffuse into the epithelial cells through cotransporter proteins
4. These cotransporter proteins also bring with them another molecules such as amino acids, vitamins, inorganic ions and glucose
5. Once inside the epithelial cells, the molecules diffuse into the blood down their concentration gradient
What is the basal membrane?
Sections of the membrane closest to the blood capillaries
How much glucose should be reabsorped?
All glucose. There should be none in the urine
What does selective reabsorption do to water potential?
It increases the water potential of the filtrate and decreases it in the capillaries (as more ions etc are moving back into the blood). This results in water moving into the blood via osmosis
Diagram to show selective reabsorption in the proximal convoluted tubule.
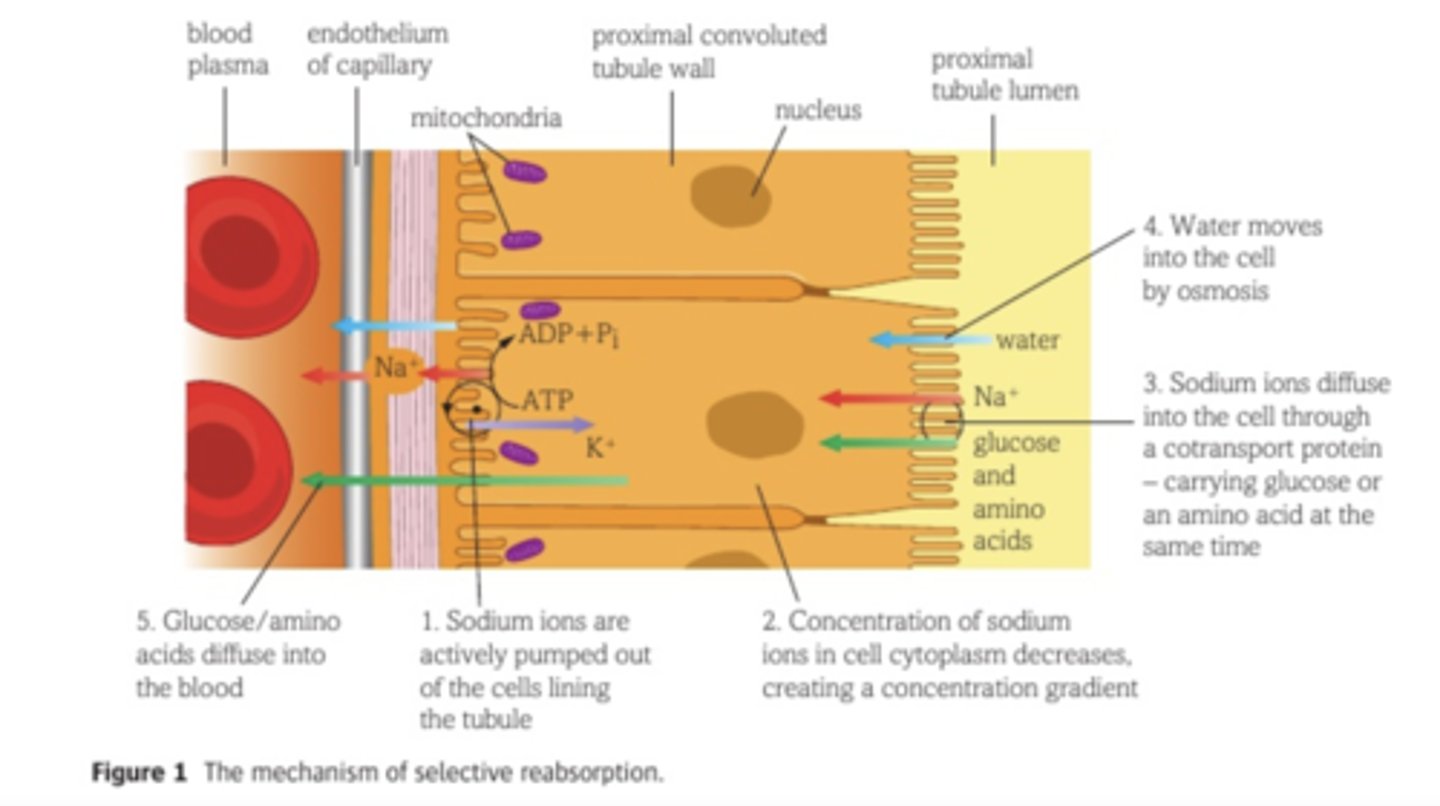
Why is the lining of the proximal convoluted tubule adapted to selective reabsorption?
- Microvilli - high SA
- Cotransporter proteins - to transport specific solute
- High number of mitochondria - energy for Na+/K+ pumps
- Tightly packed cells - no fluid can pass between cells
Where does the maintaining of an Na+ gradient occue?
In the loop of henle
What does maintaining of an Na+ gradient in the loop of henle result in?
The net movement of water out of the loop of henle - reabsorbing water
What is countercurrent multiplication?
Process by which a progressively increasing osmotic gradient is formed in the interstitial fluid of the renal medulla as a result of countercurrent flow
What is the interstitial fluid?
Fluid between cells
How does countercurrent multiplication work to build up an osmotic gradient?
1. Na is actively transported out of the tubular fluid in the thick ascending limb into the interstitial fluid
2. This means there is lower water pot in the interstitial fluid so water moves in (or out of henle) until equilibrium is reached
(These steps are called the single effect)
3. As urine is constantly being produced, new tubular fluid enters the descending limb
4. This pushes fluid down the tube so the cycle continies
(These steps are called fluid flow)
What effects the size of the osmotic gradient in the loop of henle?
The longer the loop, the larger the gradient
Where does the reabsorption of water in the final stage of urine formation take place?
- Distal convoluted tubule
- Collecting duct
Water can be reabsorbed down the entire lengths of the collecting duct. Why?
Because the water pot in the interstitial space gets more and more -ve so water wants to move in
Give the steps of reabsorption of water in in the collecting duct.
1. Na+ ions actively transported out of ascending limb of loop of henle using ATP from mitochondria
2. This creates low water pot in the interstitial space
3. Water does not pass out the ascending limb as it is too thick but it does pass out the thinner descending limb into interstitial space
4. This water then enters the blood capillaries and is carried away
5. The filtrate in the loop loses water and decreases in water pot as it moves down the descending limb
6. At the base of the ascending limb, Na+ ions diffuse out the filtrate and actively transport out as it moves up ascending limb
7. This then raises the water pot of the filtrate
8. This has resulted in water potential steadily decreasing the further into the medulla you go
9. The collecting duct is impermeable to water so as the filtrate moves down it, water leaves via osmosis
10. This water then enters the blood by osmosis and is carried away
11. Because of the movement of water into the blood from the interstitial space, the water keeps moving out of the collecting duct (countercurrent multiplication) and the cycle continues
Describe the movement of filtrate through the loop of henle.
1. Down the descending limb
2. Up the ascending limb
What happens to the filtrate after it leaves the nephron?
Once all the desirable substances have been reabsorped, the remaining fluid flows out the kidney through the ureter and enters the bladder