Histo 4 | Cartilage & Bone
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
47 Terms
What is cartilage?
A solid form of connective tissue with varying degrees of solidity ranging from the firmness of a rubber eraser to that of a silicon gel
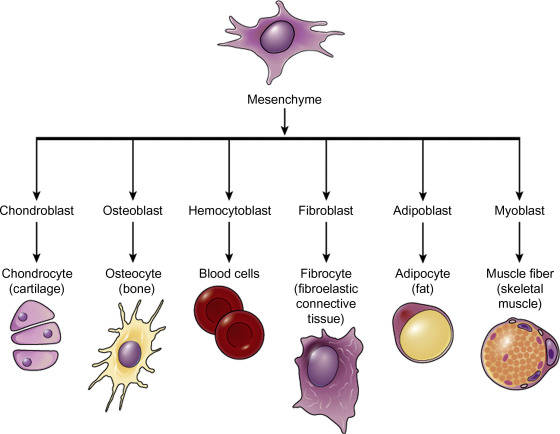
What does cartilage develop from?
From mesenchyme
What are the functions of cartilage in adults?
Provides smooth joint surfaces and structural support (e.g., tracheal rings, ears).
What are the functions of cartilage in from fetus to puberty?
Acts as a model for long bone development and growth.
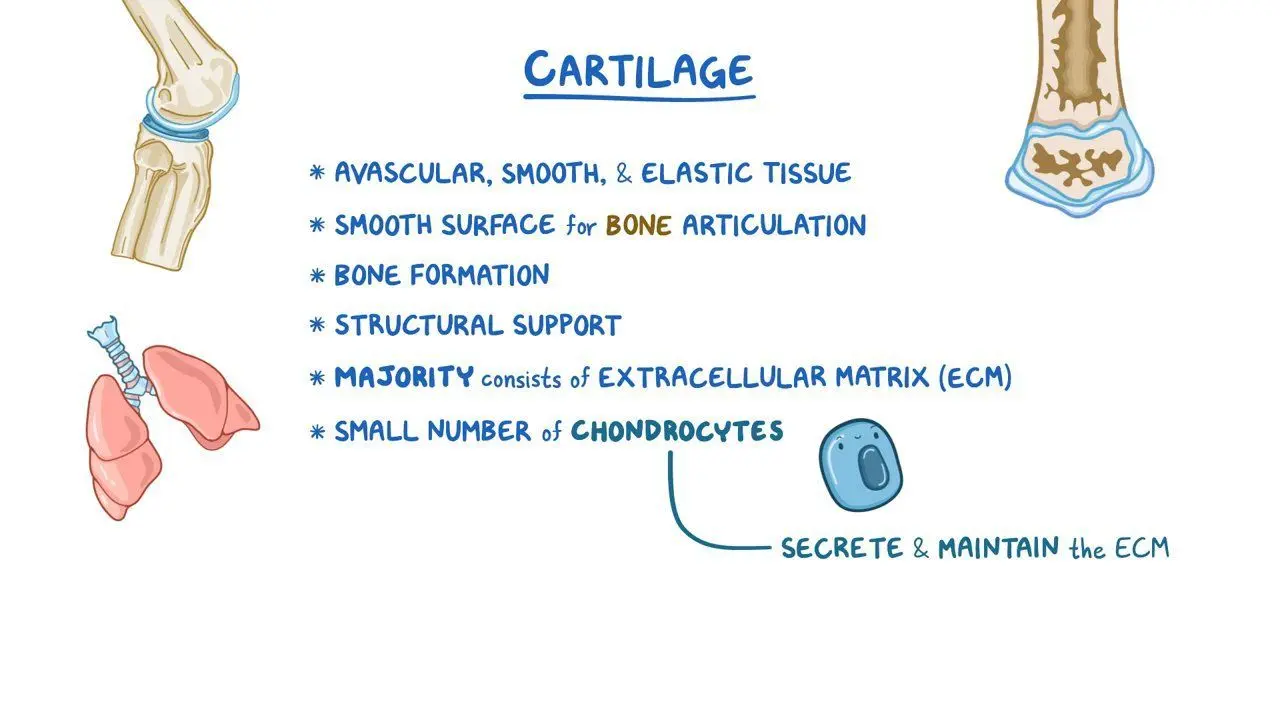
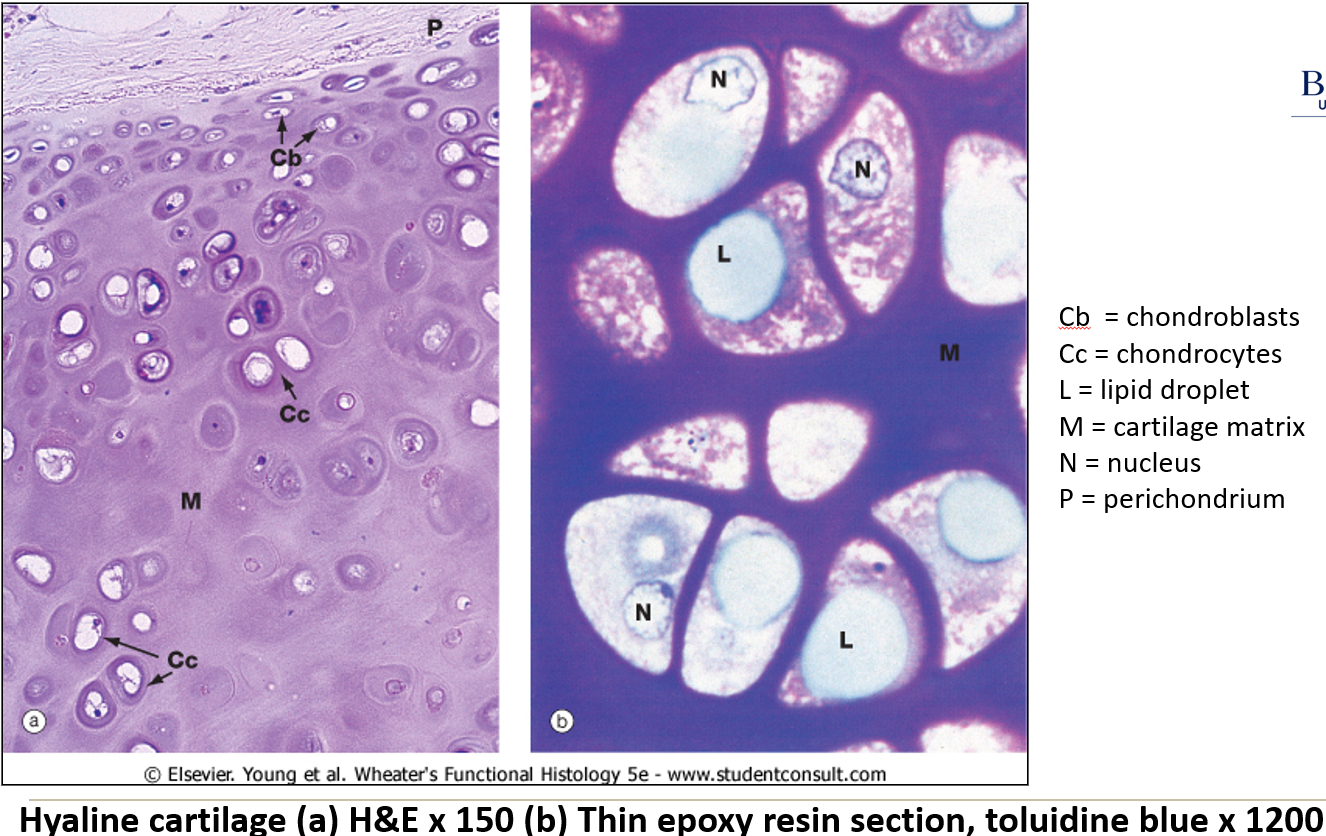
What are the characteristics of cartilage?
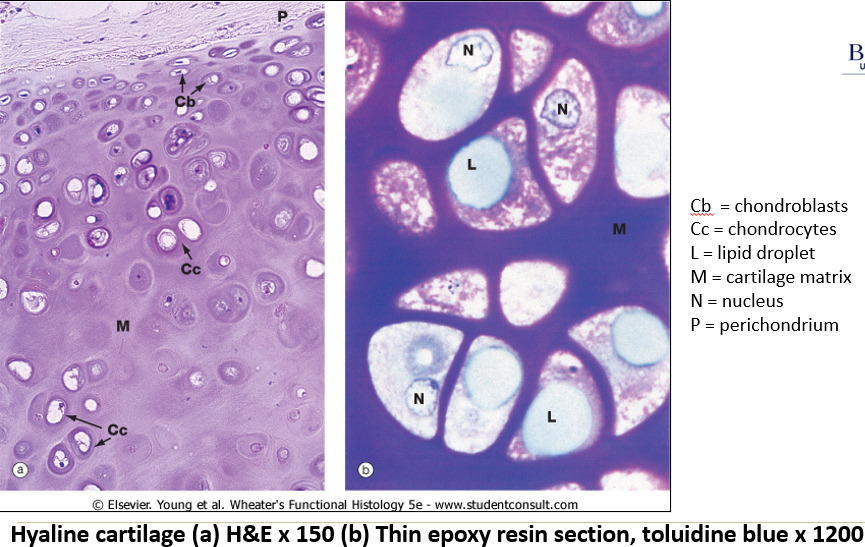
Chondrocytes: Cells located in lacunae, often with lipid droplets or vacuoles.
Avascular: Lacks blood vessels, so oxygen diffuses through the matrix.
Perichondrium: Dense connective tissue layer around cartilage with flat reserve chondroblasts.
Is cartilage vascular or avascular?
Avascular. Lacks blood vessels, so oxygen diffuses through the matrix. This means that cartilage is susceptible to degeneration; hardens and becomes brittle with age.
How does cartilage grow?
Via appositional growth and interstitial growth
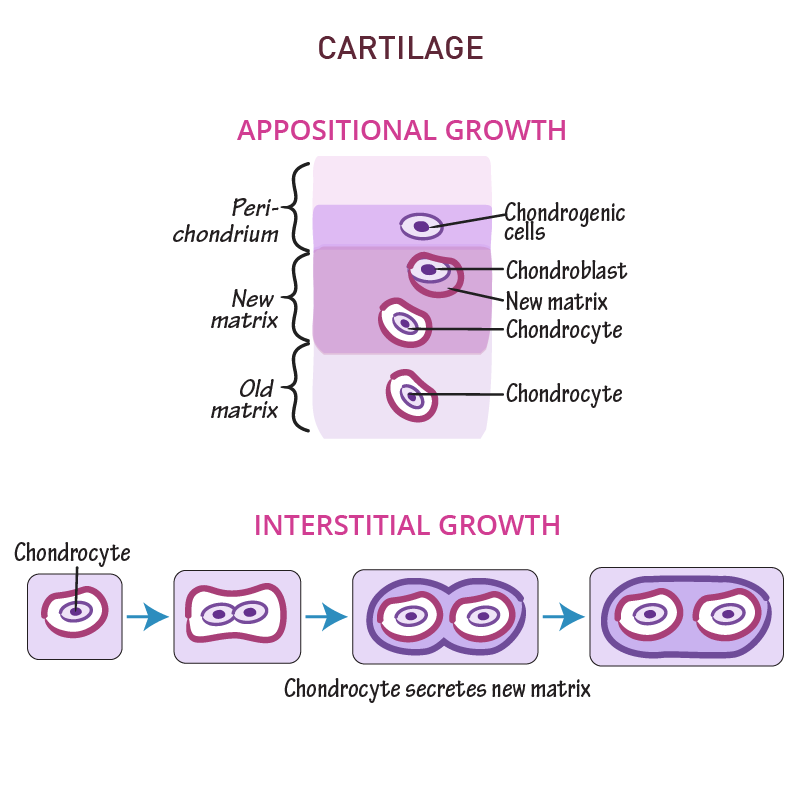
What is appositional growth?
A type of growth which increases the bone width or diameter. This growth occurs as a result of depositing new bone tissue on the endosteal and periosteal surfaces. New layers are formed on the surface of pre-existing bones, increasing the thickness of the bone.
What is interstitial growth?
A bone growth which results in the lengthening of the bone. This growth occurs within the lacunae. It happens due to the cell division in the proliferative zone and the maturation of cells in the zone of maturation. Cartilage lengthens and is replaced by bone tissue during interstitial growth.
Tiny amount of growth
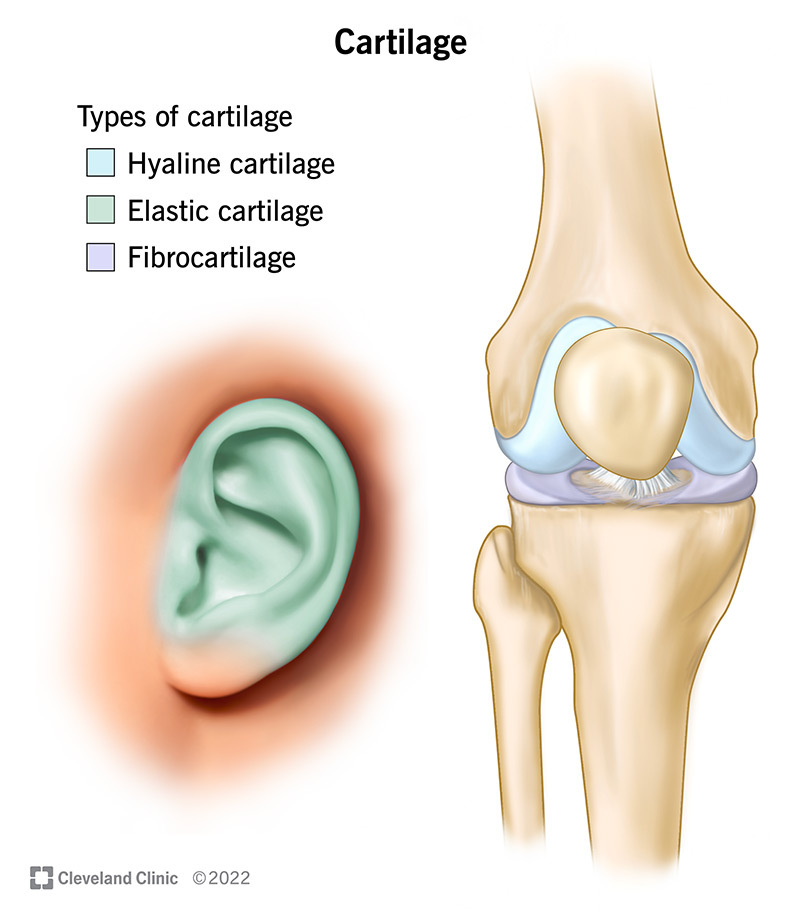
What are the types of cartilage?
Hyaline cartilage
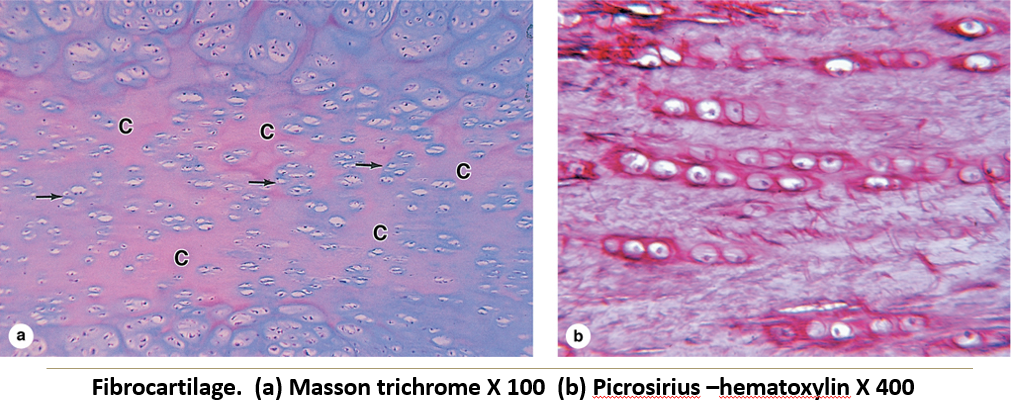
Fibrocartilage
Elastic cartilage
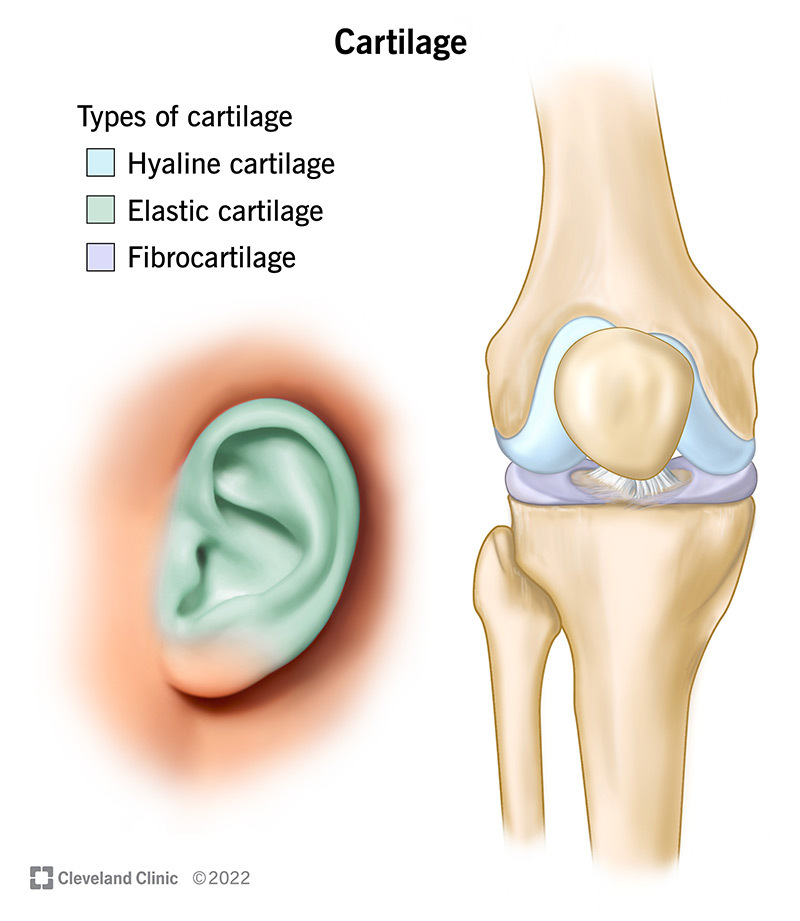
What type of cartilage is the hardest and most abundant; contains fine collagen fibers. Found in joints, trachea, nose, etc.
Hyaline cartilage
What type of cartilage is more pliable; rich in collagen for tensile strength. Found in intervertebral discs, menisci, etc.
Fibrocartilage
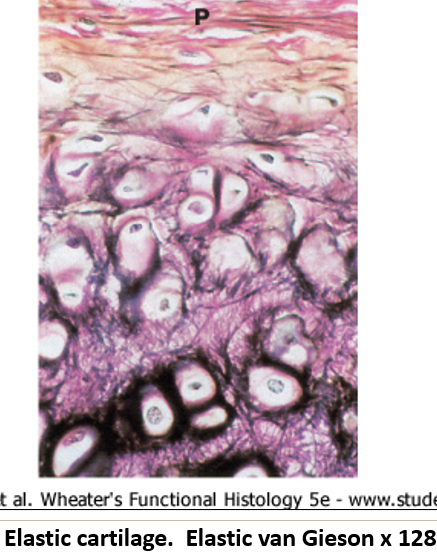
What type of cartilage that is the most flexible; contains elastic fibers. Found in ears, epiglottis, and larynx.
Elastic cartilage
What makes bone unique?
Bone is rigid due to inorganic salts and is richly supplied with nerves and blood vessels.
What are the functions of bone?
Healing capability (vascular) and constant remodeling throughout life.
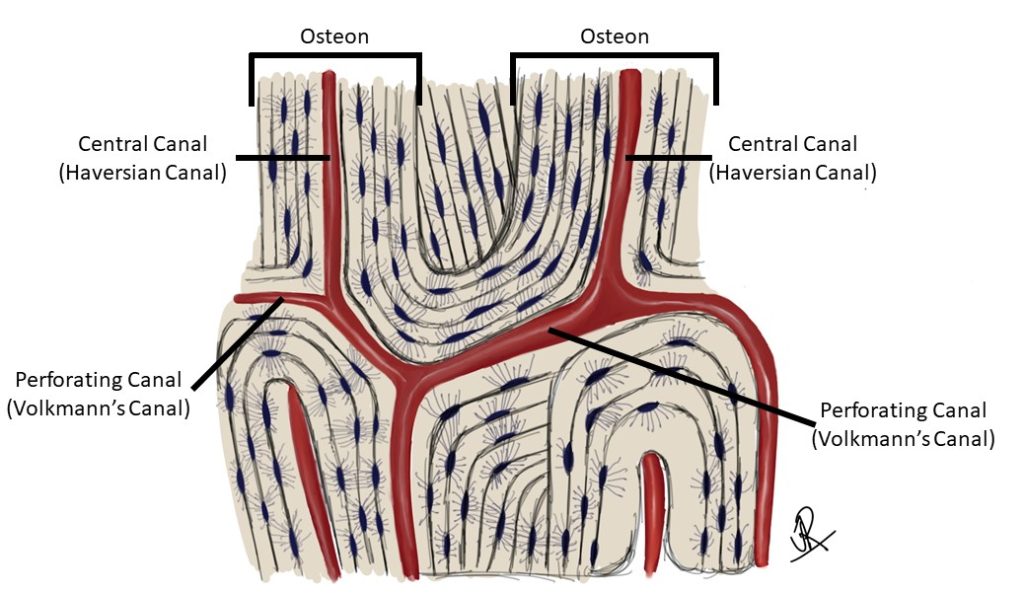
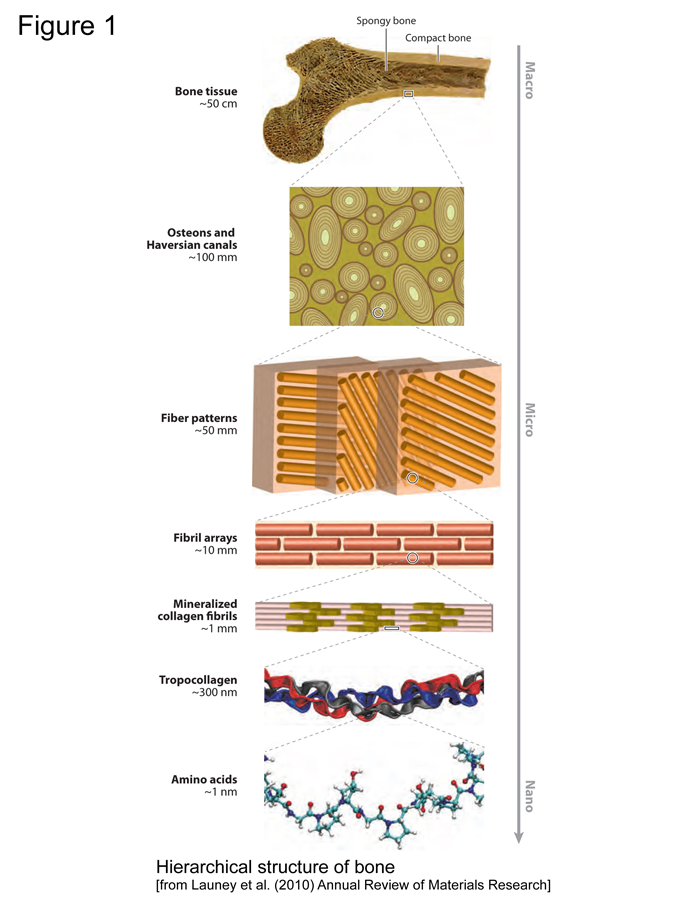
What are the structural components of bone?
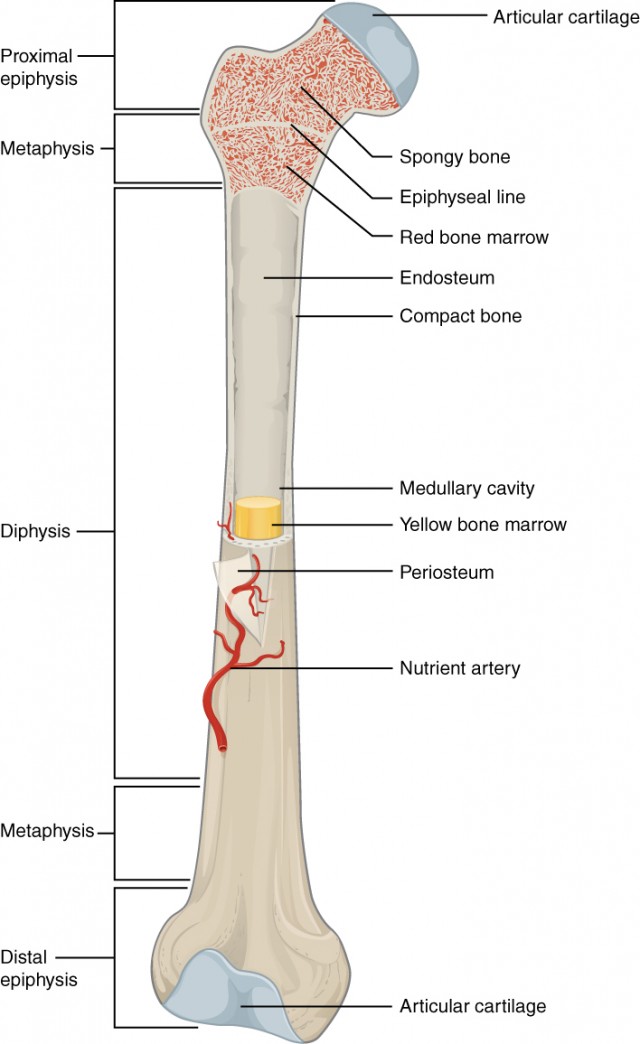
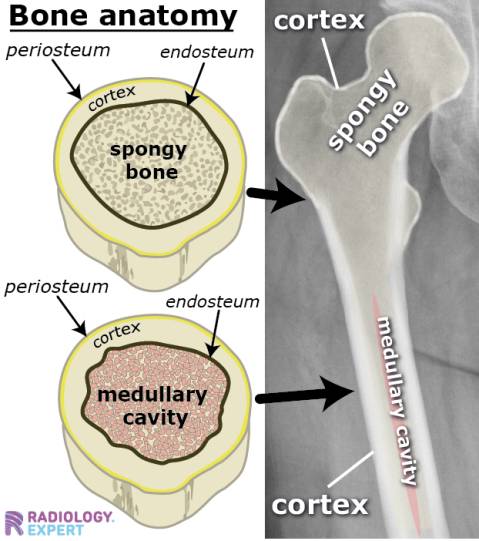
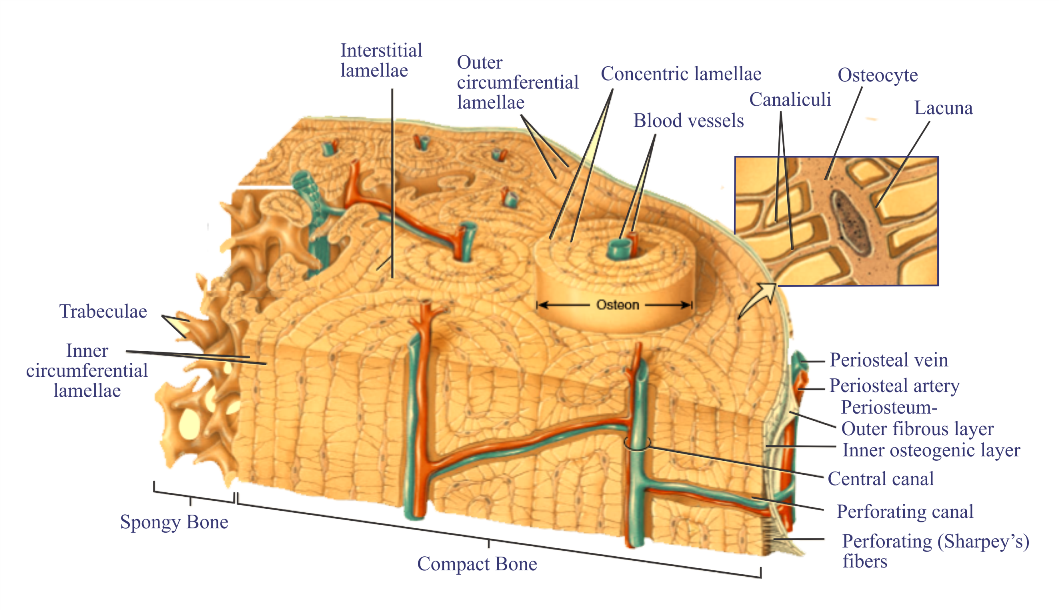
Cortex (Compact bone): Solid outer region.
Medullary (Marrow) cavity: Contains blood cell progenitors (in children) or fat (in adults).
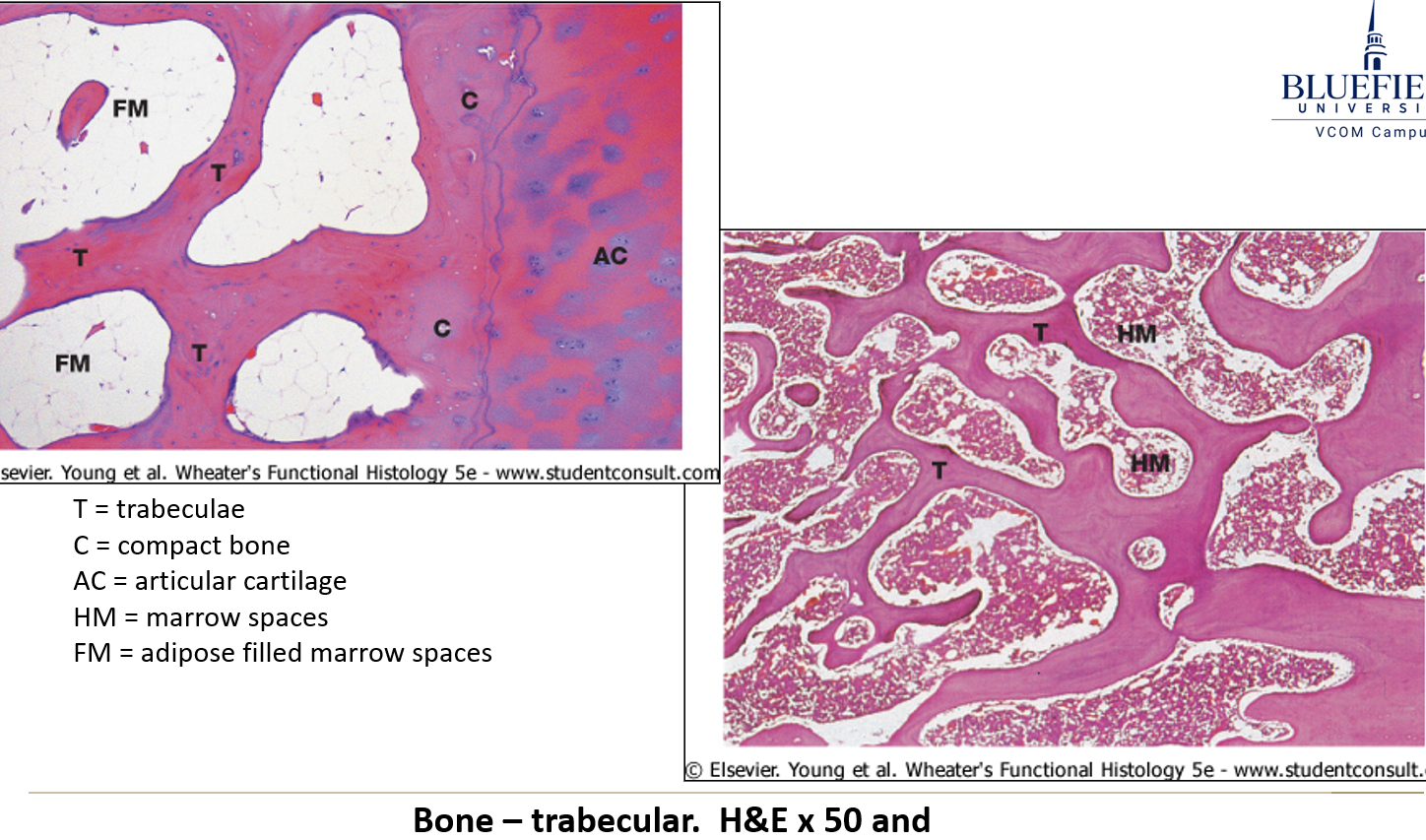
Spongy bone: Contains trabeculae that withstand stress and house blood cells or fat.
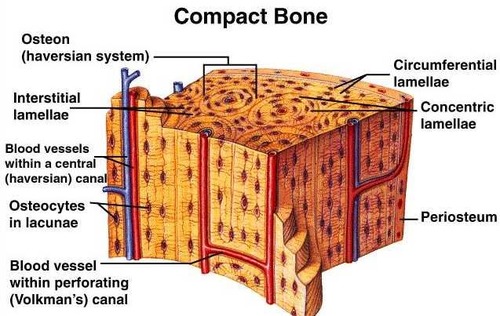
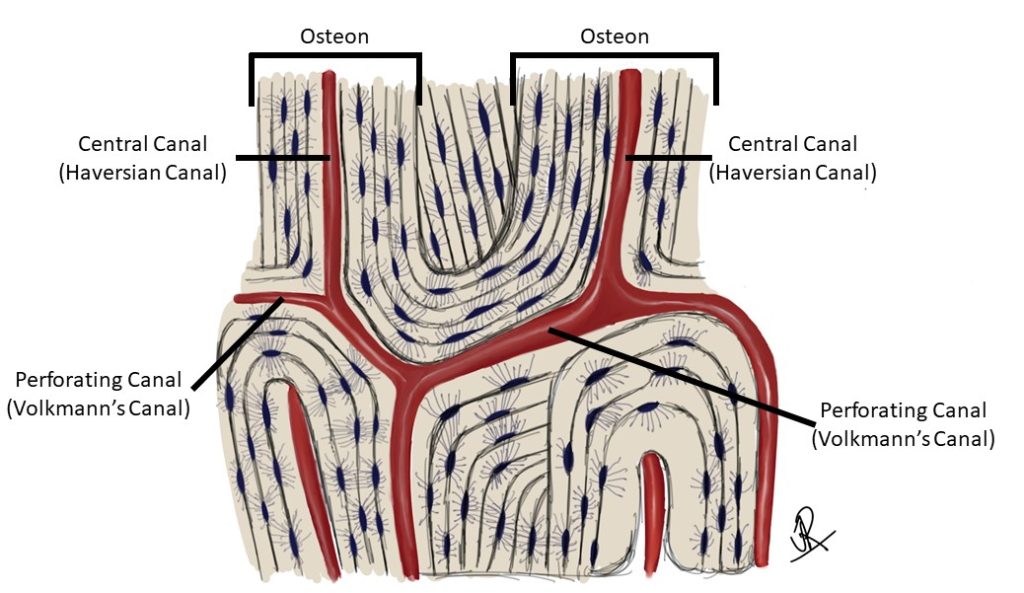
What structural features of compact bones contribute to their strength and nutrient supply?
Osteons (Haversian systems) and Volkmann’s canals found in the compact bone.
What is the initial material deposited before compact bone forms?
The initial material is osteoid, a soft, unmineralized bone matrix that later hardens into compact bone.
What are osteons, and what structures do they contain?
Osteons are cylindrical structures in compact bone. They contain:
Lamellae (layers of bone tissue)
Haversian canal (carries blood vessels and nerves)
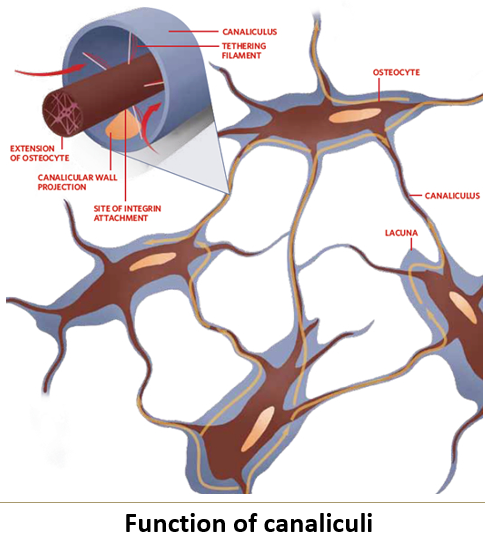
Lacunae (spaces housing osteocytes)
Canaliculi (tiny channels that connect osteocytes for nutrient exchange)
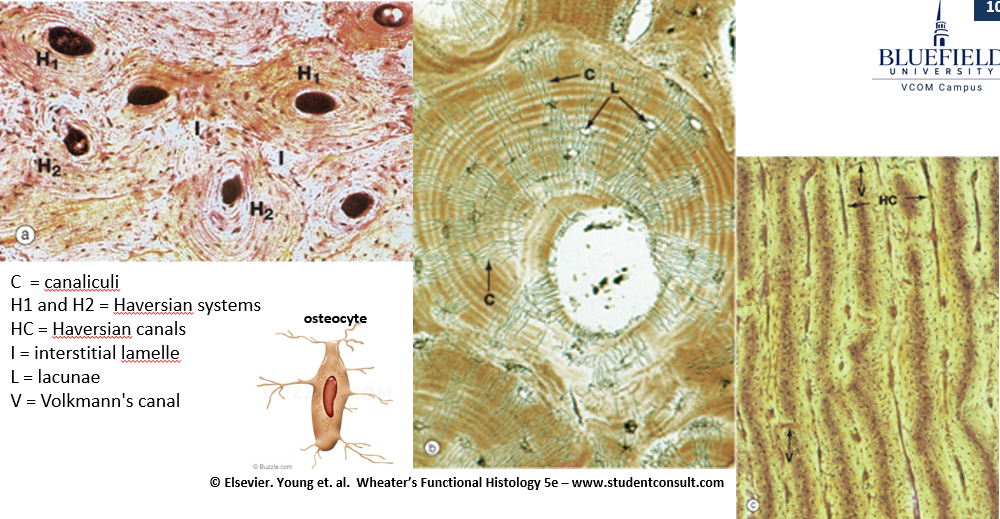
What is interstitial lamellae?
Remnants of old osteons found between newer osteons in compact bone. They help maintain bone structure and fill spaces between osteons
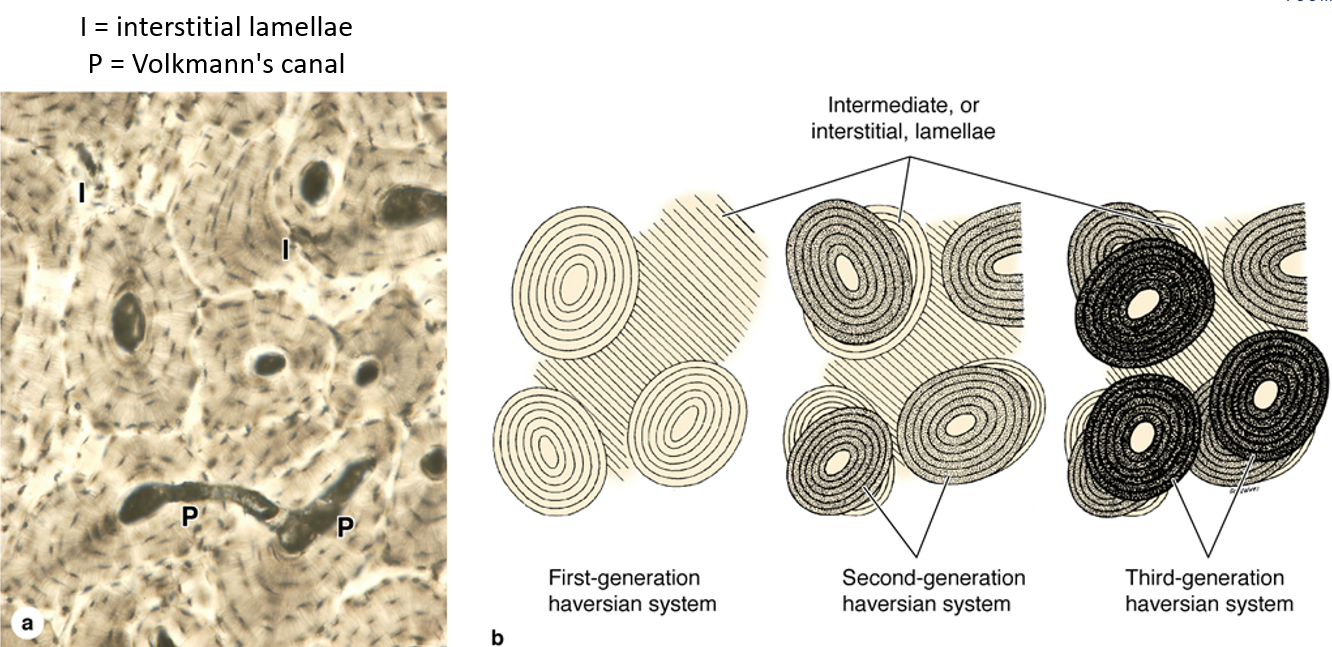
What is the function of Volkmann’s canals in compact bone?
Volkmann’s canals run perpendicular to osteons, connecting different Haversian canals to help blood and nutrients reach all areas of the bone.
Where is spongy bone found?
In the epiphyses and around the marrow cavity.
What connects Haversian canals?
Volkmann’s canals.
Function of osteons?
Provide structure and contain blood vessels and nerves.
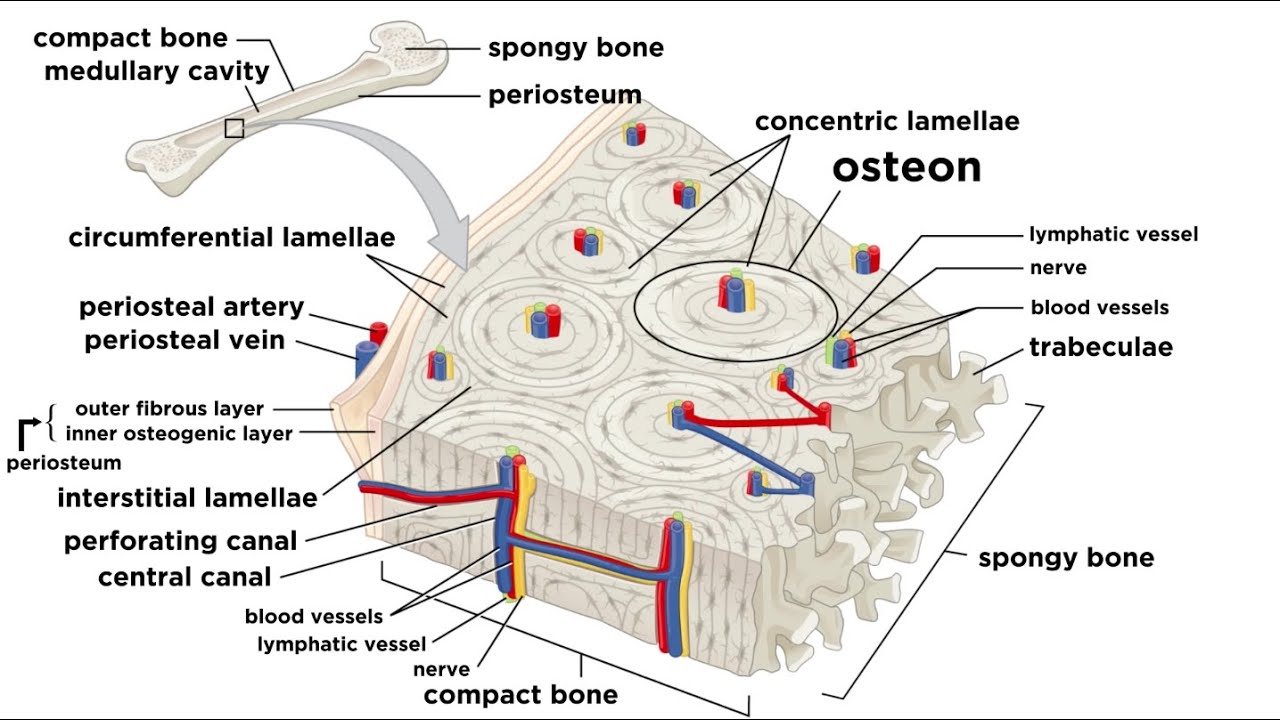
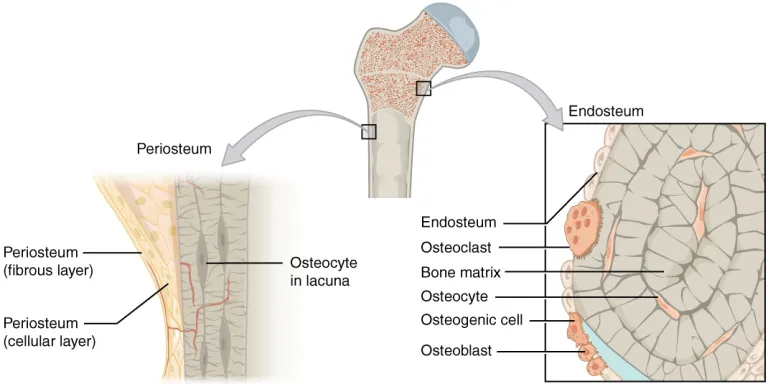
Function of osteoprogenitor cells?
These are stem cells that can turn into osteoblasts. They help in bone growth and repair.
Do osteoprogenitor cells exist in adult bones?
Yes, a few exist and are found on the bone surface.
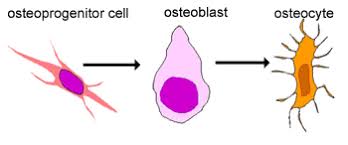
Function of osteoblasts?
Osteoblasts are bone-building cells. They produce proteins and substances to form osteoid (the soft, unmineralized bone material), which later hardens into bone.
Function of osteocytes?
Mature bone cells. They start as osteoblasts but get trapped inside the bone matrix, where they help maintain bone strength and send signals for bone remodeling.
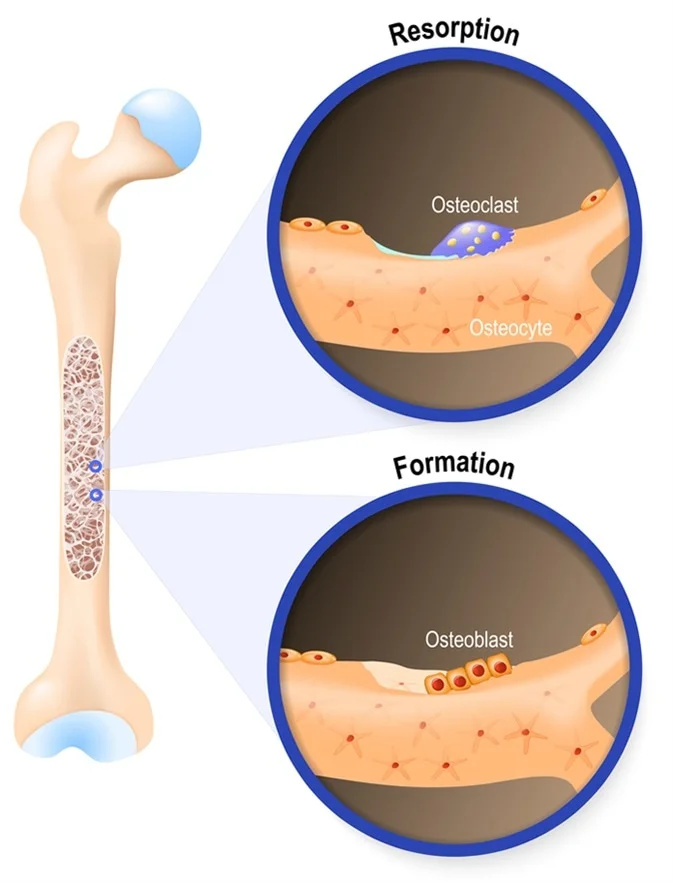
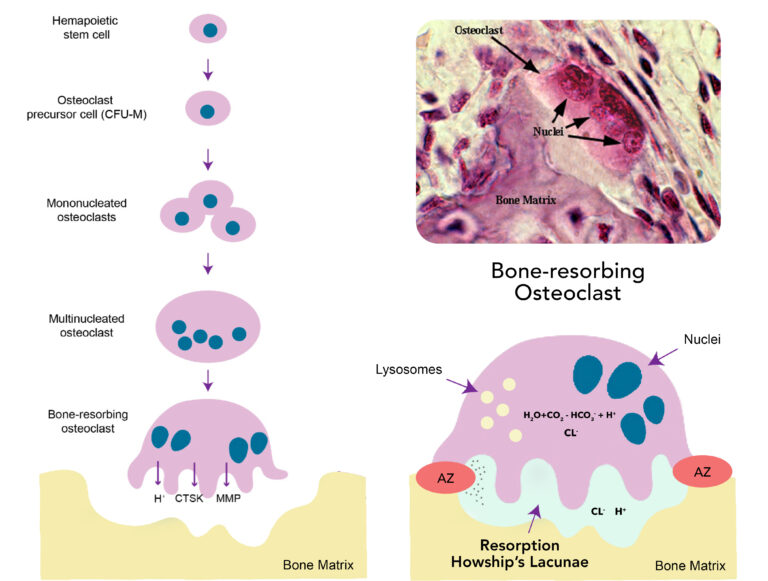
What are osteoclasts?
Large multinucleated cells that degrade bone matrix. These large cells dissolve old or damaged bone to help with bone renewal and calcium balance in the body
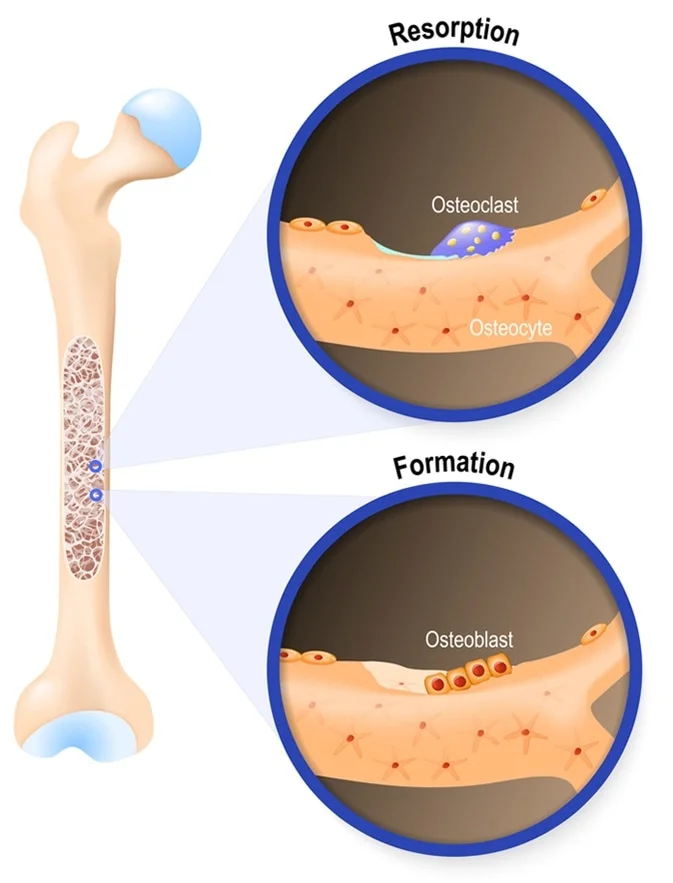
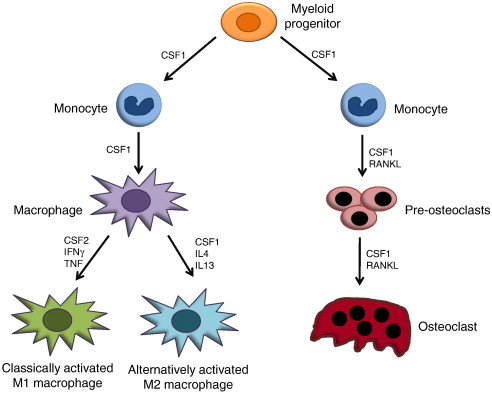
What is the origin of osteoclasts?
They are derived from blood monocytes.
Where are osteoclasts often found?
In Howship’s lacunae (aka resorption pit), indentations in compact bone caused by their reabsorption activity.
What gives the bone matrix its strength?
Highly ordered collagen fibers.
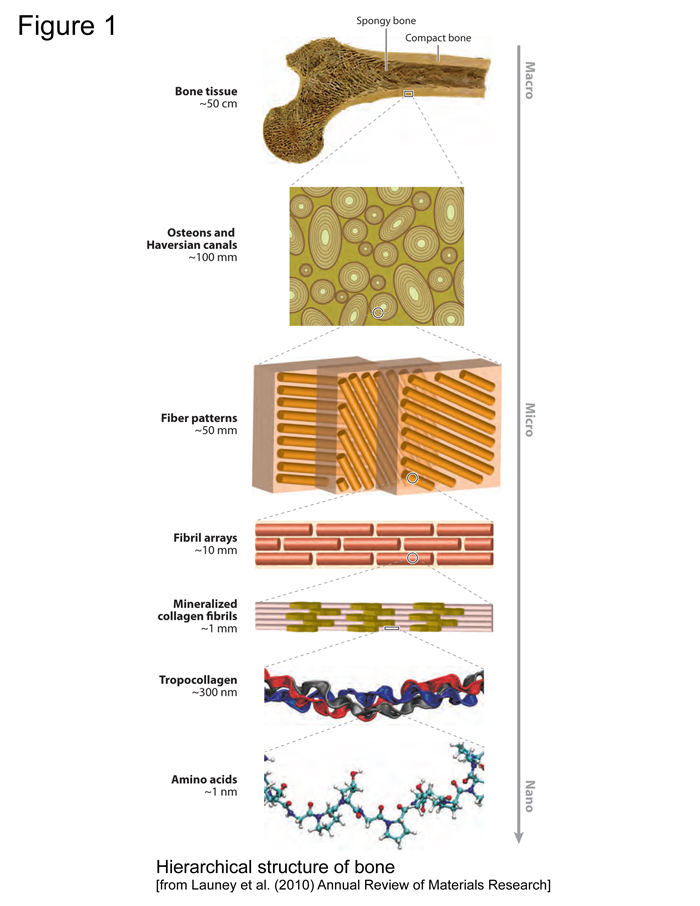
What gives the bone matrix its rigidity?
Minerals, primarily calcium hydroxyapatite.
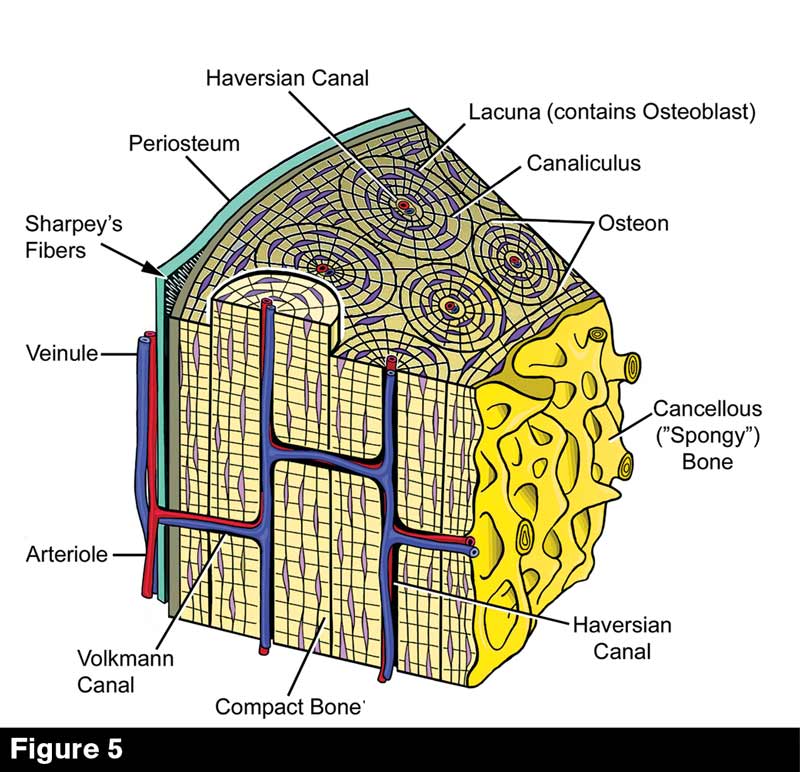
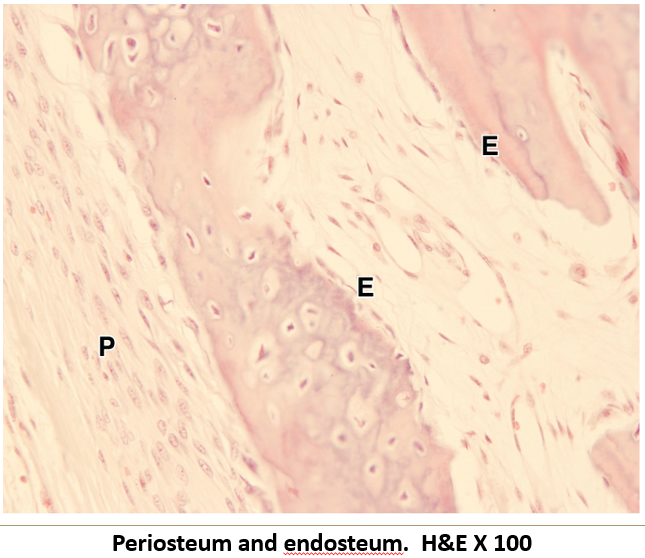
What is the periosteum?
The outer lining of the bone, attached by Sharpey fibers.

What is the endosteum?
The inner lining of the bone.
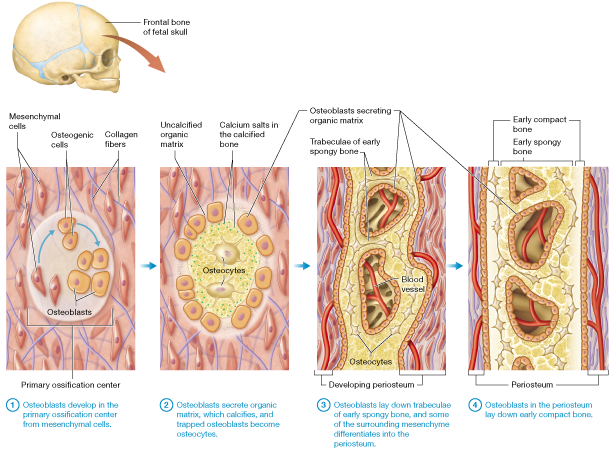
What type of bones form through intramembranous ossification?
Flat bones
What type of bones form through endochondrial ossification?
Long and Short bones
Describe Intramembranous Ossification (Flat Bones)
Formation of a starting tissue: Mesenchymal (connective) tissue becomes full of blood vessels and rapidly grows.
Osteoblast formation: Some cells in the tissue turn into osteoblasts (bone-forming cells) and start creating osteoid (soft bone material).
Bone hardening: The osteoid is replaced by hard, lamellar bone over time.
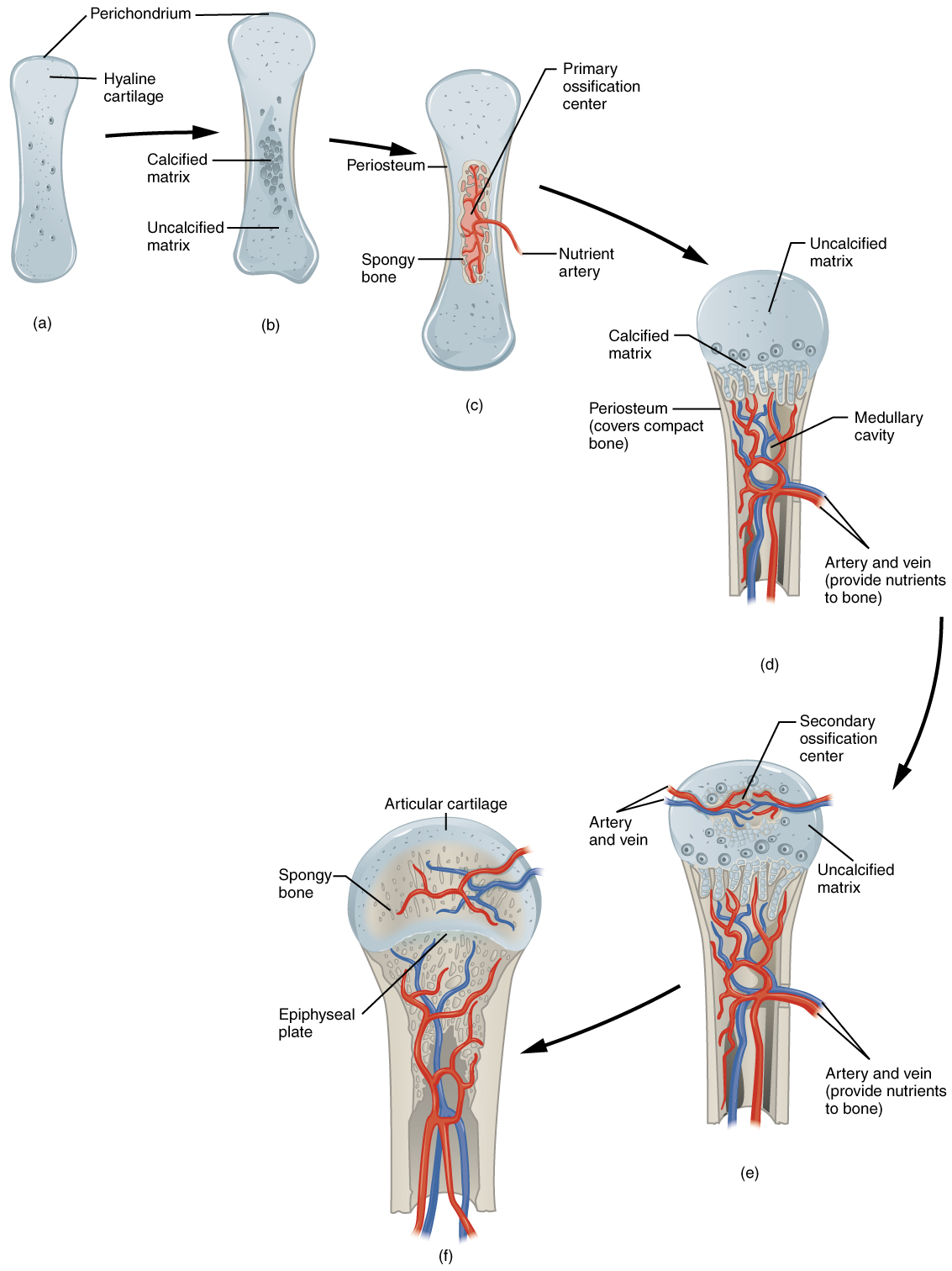
Describe Endochondral Ossification (Long/Short Bones)
Start with cartilage: A model made of hyaline cartilage forms the shape of the future bone.
Cartilage growth: Cartilage cells grow larger (hypertrophy) and multiply.
Calcification begins: Lime salts make the cartilage hard but not yet bone.
Bone-forming cells appear: Cells beneath the outer layer (perichondrium) turn into osteoblasts, forming a thin layer of bone (bony collar).
Blood vessels invade: Blood vessels grow into the bone, bringing nutrients and creating space for bone marrow.
Replace cartilage with real bone: Minerals like calcium replace the lime salts, turning the hard cartilage into bone.
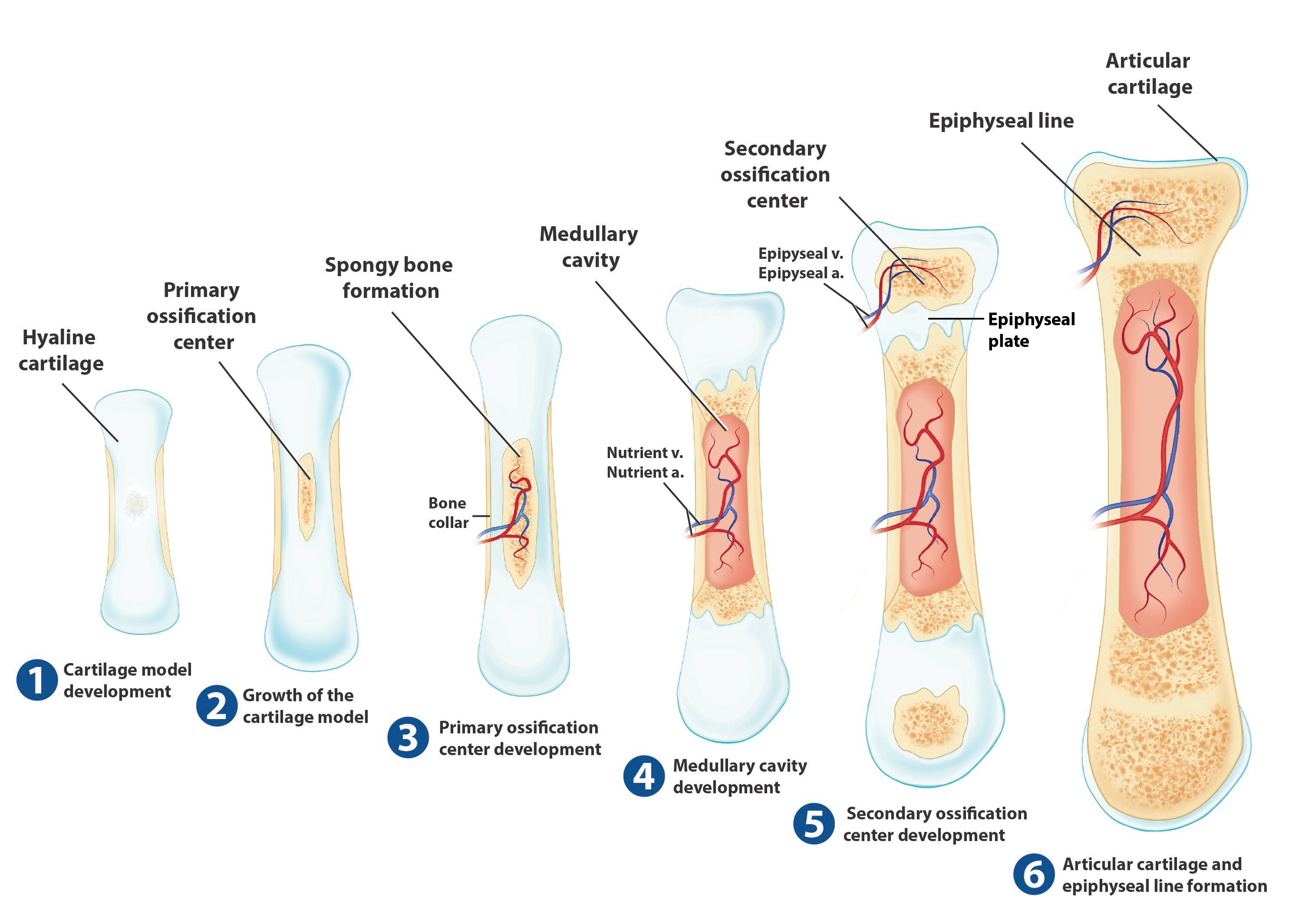
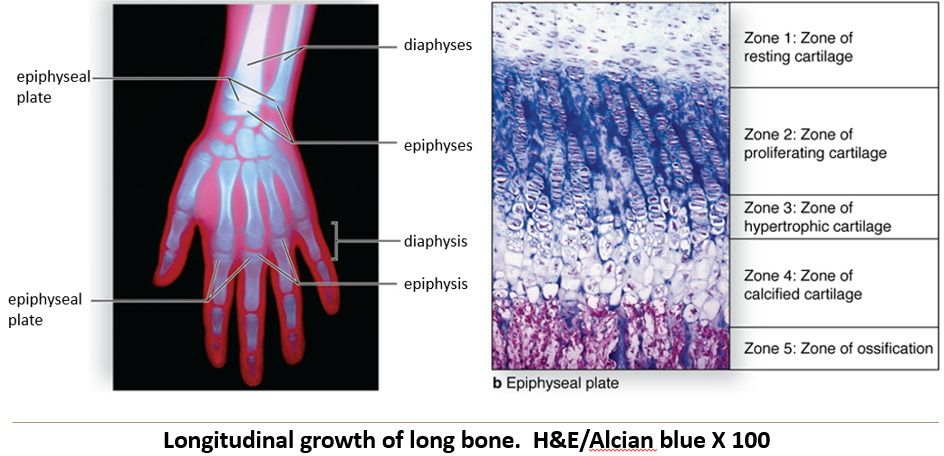
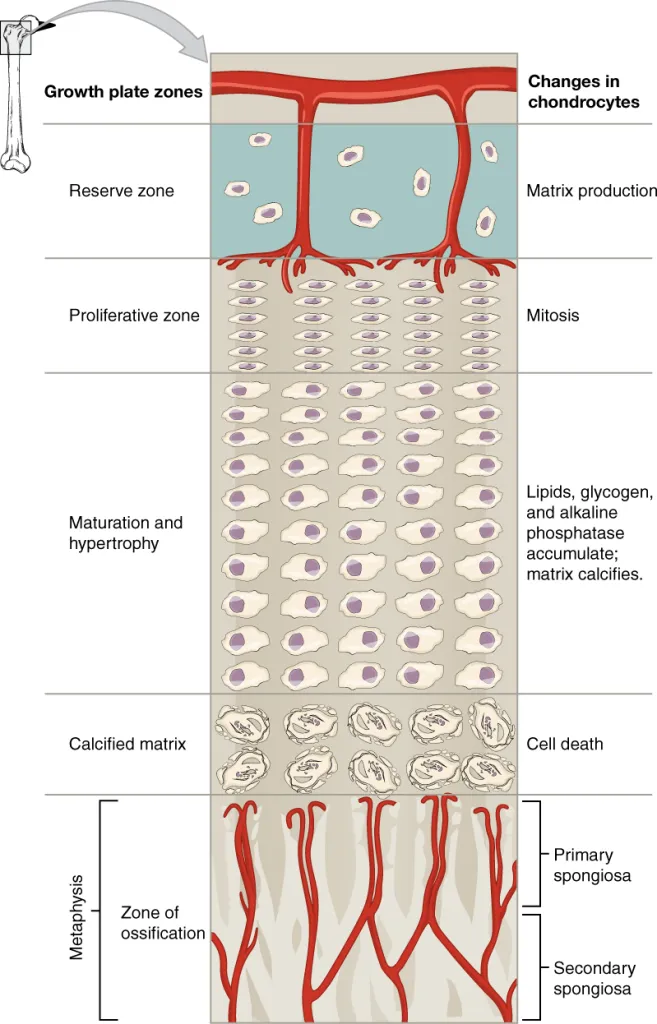
Where does primary ossification occur?
In the diaphysis (shaft of the bone).
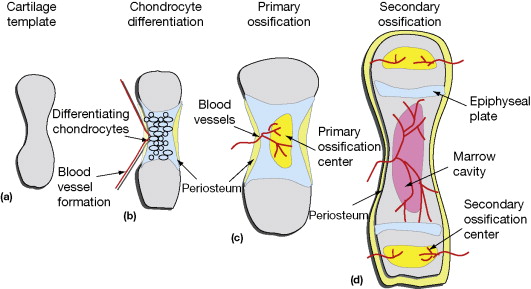
Where does secondary ossification occur?
In each epiphysis (ends of the bone).
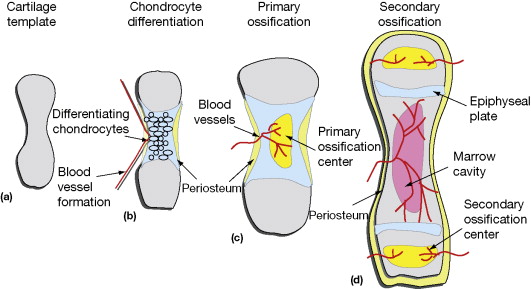
Where does cartilage remain after endochondral ossification?
At the ends as articular cartilage and between the diaphysis and epiphysis as the epiphyseal plate.
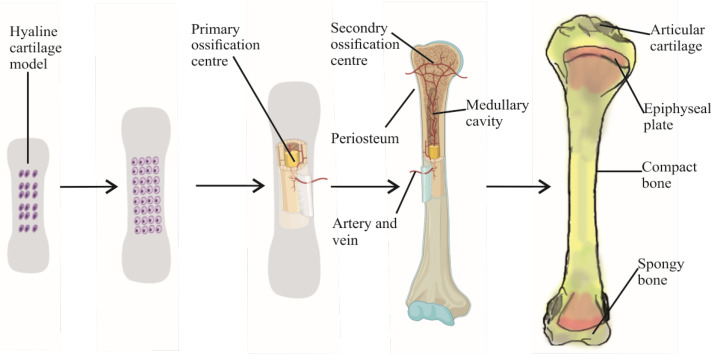
What is bone reformation?
The constant remodeling process that includes both growth and reabsorption.
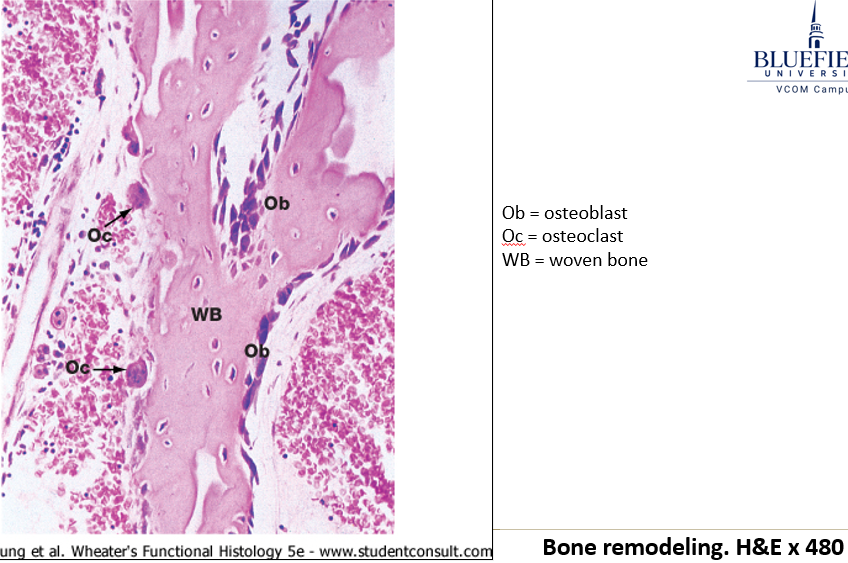
How do flat bones and long bones grow differently?
Flat bones grow by adding bone on the outside and removing bone from the inside (intramembranous ossification)
Long bones grow longer by replacing cartilage with bone at the growth plate (endochondral ossification).
How do flat bones grow without getting thicker?
Osteoblasts add new bone on the outside, while osteoclasts remove bone from the inside to maintain balance.
What are the two types of long bone growth?
Appositional growth makes bones wider, while longitudinal growth makes them longer at the growth plate.
How does longitudinal bone growth occur at the growth plate?
Longitudinal growth happens in different zones:
Reserve Cartilage – Acts as the base for growth.
Proliferation – Cells divide and expand cartilage.
Maturation & Hypertrophy – Cells grow larger.
Calcification – Cartilage hardens with minerals.
Ossification – Bone replaces the hardened cartilage, making the bone longer.