Sleep Apnea Self Study
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
21 Terms
use this case for the following questions
44 y/o man presents to PCP complaining of snoring that is affecting his life. not aware of how he sounds at night, but wife needs to sleep in another room bc snoring is so loud, and has intermittent grunts/snorts.
HPI: pt has noticed increased daytime somnolence for 3 years which has worsened in the past 3 months. he has difficulty remaining awake in the afternoon at work (accountant). he was frightened several weeks ago when he nodded off at the wheel of his car on the way home. he regularly falls asleep while watching TV with his wife in the early evenings and takes naps on most weekends. he wakes with headaches and does not feel refreshed in the mornings.
past med hx: has not seen a PCP in over 5 years; no meds; no known chronic med problmes
social hx: does not exercise regularly, does not smoke, drinks 3 times/month
ROS: slow weight gain of 15 pounds over 3 years; denies chest pain, dyspnea, or lower extremity edema
PE: HR 82, BP 149/87, RR 12, BMI 30; appears healthy
based on the info above, what disorder are you suspicious this patient may have? which findings in his hx make you suspicious of this disorder?
his hx suggests a sleep related breathing disorder. he specifically sounds as though he has episodes of not breathing in his sleep, which is called apnea.
sleep related breathing disorders can be broken down into 3 categories, what are they
1) obstructive sleep apnea: physical obstruction to breathing regularly while sleeping
2) central sleep apnea: apnea that results from a problem in the neural control of breathing; a problem in the brain
3) simple snoring without apnea
simple snoring (not due to an illness or medication) is likely on the spectrum of OSA, what does this mean
snoring may progress to OSA if the conditions allow
what are suggestive symptoms for OSA in this patient?
1) snoring, grunts, snorts, gasps while sleeping
2) waking without feeling refreshed
3) difficulty remaining awake during the day (nodding off)
4) impaired concentration
5) morning headaches
what are other symptoms of OSA
1) waking with choking sensation or gasping for air
2) nocturnal symptoms of dyspnea, restlessness, nocturia, diaphoresis, reflux, waking with a dry mouth
3) daytime symptoms of nasal congestion, impotence, depression
what physical findings might you find during your head and neck and intraoral exams that would be suspicious for obstructive sleep apnea?
EO:
1) neck circumference: >16 inches in women, >17 inches in men
2) elevated BMI: OSA is more common in elevated BMI, but can occur in normal BMI
IO:
1) "crowding" of soft structures
2) enlarged tonsils
3) elongated soft palate/uvula
4) tongue findings: macroglossia, crenation ("scalloping" on sides of tongue), deep central fissure, elevated base of the tongue
the patient is referred for an overnight polysomnogram (sleep study). a short epoch from that study displays the pattern of chest wall and abdominal movements and nasal airflow during sleep is shown below
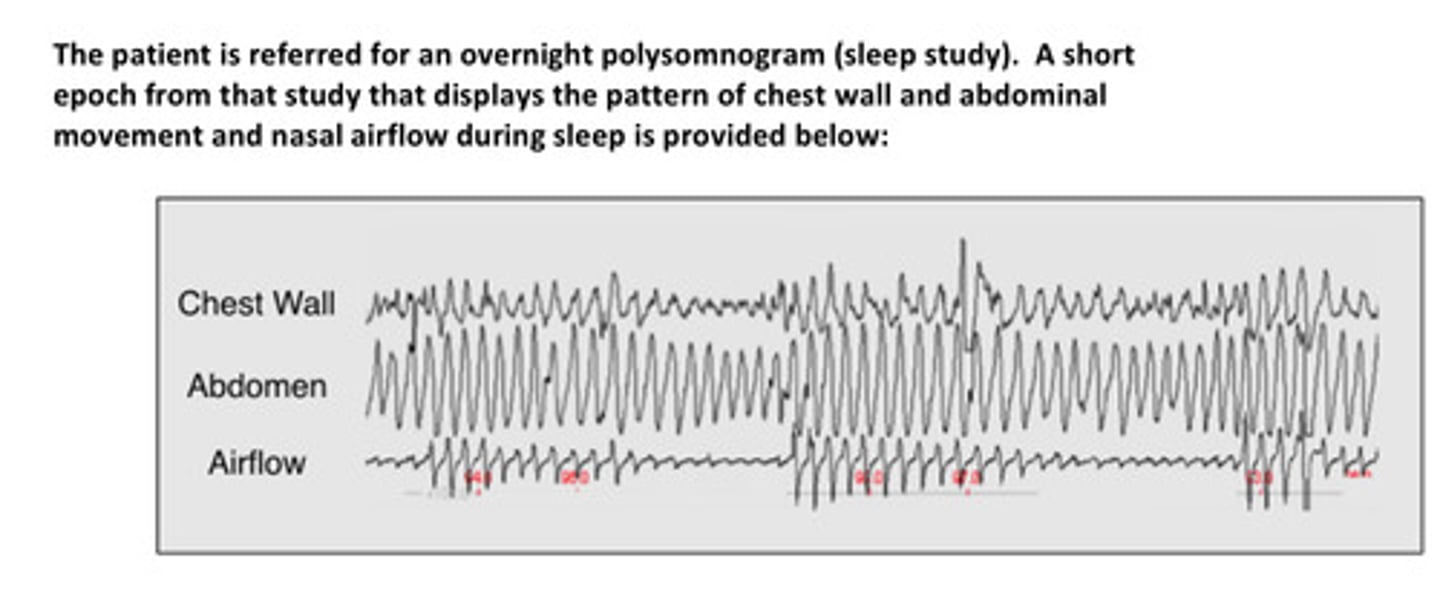
what are the primary findings on this epoch from his sleep study?
we can see that he has episodes of decreased airflow. these can be describe as hypopnea (decreased airflow) and apnea (cessation of airflow). we look at the chest wall and abdominal movements to determine if these are caused by obstruction or by a central (brain) mechanism. if he were to have no chest/abdomen movements, we would conclude that his brain is not telling him to breathe and diagnose him with central apnea. but in this study, we see that his chest and abdomen are moving, but there is decreased airflow —> obstruction!
how do we access the severity of the problem?
severity is graded by counting the number of apneas and hypopneas. this is known as the apnea-hypopnea index (AHI). an AHI >/= 5 events/hr is required for the diagnosis of OSA. the higher the AHI value, the more severe the problem!
describe the pathophysiologic mechanisms that explain OSA
soft tissues and bony structures surrounding the upper airway push inward on the airway. you will remember that as we inhale, the pressure inside the airways decrease and this decreased pressure can narrow the airways. the pharyngeal dilators (genioglossus and palatal muscles) are activated during inspiration. their activation helps to counteract the inward pressure of the tissues and therefore helps maintain airway patency. during sleep, the activity of genioglossus and palatal msucles is decreased, so upper airways have tendency to narrow. and if inward pressure of soft tissues surrounding the airways is greater than the outward pressure of the airway, the airway collapses
explain why OSA is associated with obesity for a couple of reasons now that you understand the pathophysiologic mechanisms
1) volume of soft tissues of the upper airway tends to increase in obesity
2) caudal traction (caudal means "toward the tail") of the lung on the trachea helps to keep trachea open. if lung volumes are decreased, as happens when the diaphragm is displaced upward when supine by obesity, plus the added weight of the thoracic soft tissues, this traction is lost, and the trachea has a greater tendency to collapse
the patient with OSA is at risk for what potential complications if his condition is left untreated
1) pts with untreated OSA have an increased risk of CV disease including hypertension, myocardial infarction, and stroke (main concern)
2) type 2 diabetes
3) pulmonary hypertension and heart failure
4) fatty liver disease
5) neuropsychiatric dysfunction such as depression, cognitive changes, and even psychosis
6) perhaps cancer!
what behavioral changes can the patient make that may help their OSA?
1) weight loss
2) sedative/alcohol avoidance
3) sleeping in a more upright position
4) regular exercise
5) smoking cessation
6) aggressive tx of co-morbidities
what is the most commonly used therapy for OSA
continuous positive airway pressure (CPAP) device! —> consists of a machine which blows air at increased pressure via a face mask (usually tight fitting) or nasal device while the patient sleeps. CPAP raises the pressure inside the airway to help maintain patency. getting used to it is a challenge, but once you do, most people get great relief and feel much better overall with good sleep and have improved health
oral appliances are considered ___________-line interventions for OSA
second-line! CPAP should be tried first since it overall has more success at improving O2 saturation and decreasing AHI.
sometimes surgery is considered as a tx, especially for what?
specific problems like enlarged tonsils or nasal polyps
what devices are newer interventions for OSA and are currently being compared to CPAP devices
hypoglossal nerve stimulation (HNS) devices
this pt presents to your dental office after seeing an ad on the use of dental appliances to treat sleep apnea. what types of oral appliances are available to treat sleep apnea?
oral devices should only be used if a pt is unable to tolerate CPAP as CPAP is best option. the most effective oral appliances are known as mandibular advancement devices (MADs). these protrude the mandible, which opens the airway be repositioning the soft tissues of the tongue. tongue retaining devices (tongue bulbs) are also used in some patients.

in what circumstances should oral appliances not be used?
1) central sleep apnea
2) edentulism for MADs, a tongue bulb could be used instead
3) unstable dentition
4) rapidly progressive caries
5) severe periodontal disease for MAD
6) unstable occlusion for MAD
7) refractory temporomandibular dysfunction
surgical interventions may be useful in rare or specific situations, but typically oral devices are tried prior to surgery
woohoo