25. respiratory pathogens I (mycoplasmas & rhodococcus)
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
38 Terms
what is special about the structure of mollicutes (mycoplasma spp.)?
lack cell walls → have a single trilaminar membrane rich in proteins and lipids
are mycoplasmas typically found as free-living organisms?
no → obligate parasite
co-evolve with their host
limited host range
what classes of antibiotics are ineffective against mycoplasmas?
all beta lactam antibiotics
sulfonamides
mycoplasma mycoides subsp. mycoides is the causative agent of what disease? what species does it affect?
contagious bovine pleuropneumonia (CBPP)
affects cattle and buffalo
clinical signs of acute contagious bovine pleuropneumonia
respiratory distress
cough
cessation of rumination
anorexia
severe pleuritic pain
is mycoplasma mycoides susbp. mycoides commonly found in the US?
no → eradicated from USA but still a problem in other parts of the world
reportable due to its negative impact on livestock industry
considered the most important bacterial epizootic by WHO
mycoplasma bovis reservoir
mucosal surfaces (respiratory, genital, conjunctiva, mammary gland, alimentary canal, and joints(?))
how is mycoplasma bovis transmitted?
ingestion, possible inhalation, or direct contact
mycoplasma bovis virulence mechanisms
suspect antigenic variation (variable surface lipoproteins)
damage host cells (phospholipases, H2O2, and superoxide radicals)
biofilm formation
can adhere to neutrophils and inhibit respiratory burst activity
how does mycoplasma spread systemically? what are its predilection sites?
hematological spread
predilection sites:
nares
tonsils
eyes
tympanic bulla
meninges
lungs
udder
joints
genital area

what are possible outcomes of mycoplasma bovis infection in calves?
clear infection
chronic colonization of URT & intermittent shedding
increased replication in URT → spread from URT → clinical disease
what are complications associated with mycoplasma bovis infection in calves?
otitis
pneumonia
arthritis
clinical signs of mycoplasma bovis infection in calves
progressive disease
fever & anorexia
otitis → scratching ear, head shaking, ear droop
head tilt ± other neurologic signs indicate otitis interna (CN VIII) ± nystagmus
advanced otitis media-interna → meningitis and/or other cranial nerve deficits
→ spontaneous regurgitation, loss of pharyngeal tone, dysphagia, and aspiration pneumonia
unilateral or bilateral neurologic deficits
purulent aural discharge + ruptured tympanic membrane
arthritis
mycoplasma bovis diagnosis (calves)
based primarily on clinical signs
pharyngeal swabs for culture or PCR
synovial fluid from calves with arthritis can be aspirated for culture or PCR
treatment of mycoplasma bovis infection in calves
antimicrobials are usually unrewarding but may be beneficial in early stage disease
puncturing the tympanic membrane to allow for drainage may alleviate pain from trapped exudate
what age of animal does mycoplasma bovis mastitis affect? how is it transmitted?
affects any age/adults
type of contagious mastitis (spread easily among animals by direct contact and fomites)
clinical signs of mycoplasma bovis mastitis
infection usually subclinical
clinical mastitis usually mild → may have some discharge; affected udders not typically painful
only indicator may be sudden drop in milk production
history of recurrent mastitis is common
clinical/lab findings of mycoplasma bovis mastitis
somatic cell counts usually normal
milk may appear discolored
false negative cultures/PCRs common due to intermittent shedding (need to do repeat sampling)
serology testing individual cow is useless due to high number of false negatives (m. bovis is intracellular)
mycoplasma bovis mastitis treatment
intramammary antimicrobial therapy not effective
if cow spontaneously resolves infection, she can become a carrier
mycoplasma bovis pneumonia source
carrier animals
mycoplasma bovis pneumonia transmission
ingestion or inhalation
mycoplasma bovis pneumonia predisposing factors
all ages affected
stressors (shipment, parturition, weather changes) that affect innate immunity (impaired mucociliary escalator)
what is a gross finding of mycoplasma bovis pneumonia? what is a common sequelae?
lung abscesses
arthritis
mycoplasma bovis pneumonia clinical signs
fever, tachypnea, dyspnea, and decreased appetite ± nasal discharge and coughing
poor weight gain in chronically affected animals
can be accompanied by ear infection and/or arthritis
mycoplasma bovis pneumonia diagnosis
presence of M. bovis in the respiratory tract of healthy animals confound diagnosis
diagnosis will be presumptive and depends on clinical signs and presence of organism in lesion (necropsy) or transtracheal wash
mycoplasma bovis pneumonia treatment
antimicrobials administered early (e.g. tetracyclines) may help + supportive care → unrewarding with advanced disease
what is an important practice to reduce mycoplasma bovis infections?
mycoplasmas are sensitive to disinfection → good farm disinfection & biosecurity practices
rhodococcus gram stain
gram positive rods
rhodococcus equi is the causative agent of what disease? (what age/hosts does it affect?)
pyogranulomatous pneumonia in foals < 6 months of age
uncommon infections in other animals
commonly causes pyogranulomatous pneumonia in immune compromised humans
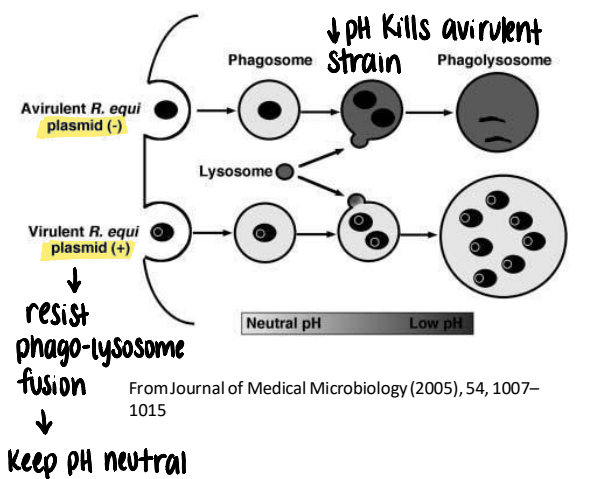
rhodococcus equi virulence factors
plasmid expressing virulence associated protein A (VapA) essential for intracellular survival in foal macrophages
helps resist phagolysosome fusion and keeps pH inside phagosome neutral
lipid rich cell envelope protects from desiccation in environment and supports survival within macrophage
rhodococcus equi source
manure contaminated soils, hays, and sandy stalls (risk factor)
rhodococcus equi transmission
inhalation of organisms
predisposing factors to rhodococcus equi infection
heavy environmental contamination and inadequate colostrum
rhodococcus equi pathogenesis
bacteria engulfed by alveolar macrophages, where it persists → foal macrophages are inefficient at killing bacteria & VapA interferes with lysosome-mediated killing → accumulation of bacteria-laden macrophages → pulmonary pyogranulomas
intracellular → capable of evading host immune response (i.e. no fever)
can cause extensive, irreversible lung damage before foal shows signs of illness
pyogranulomas can be found in other body sites (eyes, joints, intestines)
rhodococcus equi clinical signs
subclinical until advanced disease
based on location of organisms
respiratory: coughing, crackles, tachypnea, flared nostrils
GI: diarrhea with ulcerative colitis and mesenteric lymphadenitis if intestines become infected
osteomyelitis with bone infection (bone swelling, pain/lameness)
rhodococcus equi diagnostics
clinical signs
transtracheal or bronchiolar lavage for culture and cytology
PCR detection of VapA gene is definitive (plasmid only present in virulent strains)
nasal swabs are useless
rhodococcus equi prognosis/treatment
prognosis is good if infection caught early; advanced infections have high mortality rates (40-50%)
sick foals should be isolated and treated with antibiotics (macrolides + rifampin) for several weeks
what is a risk to consider when treating rhodococcus equi with antibiotics? (why should prophylactic antibiotic use be discouraged?)
both mare and foal are at risk for clostridioides difficile associated diarrhea (CDAD)