Acute Inflammatory Skin Disorders
1/69
Earn XP
Description and Tags
LO : (1) Describe the typical clinical presentation, pathophysiology, risk factors, diagnostic features, and treatment of allergic contact dermatitis.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
Acute inflammatory skin diseases
immune reactions against the skin that are short-term, lasting for days to weeks;
Chronic conditions persist for months to years
Many acute inflammatory skin conditions are triggered by a(n)
allergen
Allergic reactions are an overresponse of the immune system to common elements in our environment, like foods or plants.
3 types of acute inflammatory skin disorders are
contact dermatitis, urticaria and erythema multiform
urticaria is an allergic reaction while contact dermatitis is type 4 hypersensitivity
Contact dermatitis
inflammatory skin condition caused by exposure to an exogenous agent, characterized by erythema and pruritus
Redness and itchiness
skin lesions of contact dermatitis are
localized to the site of contact without systemic involvement
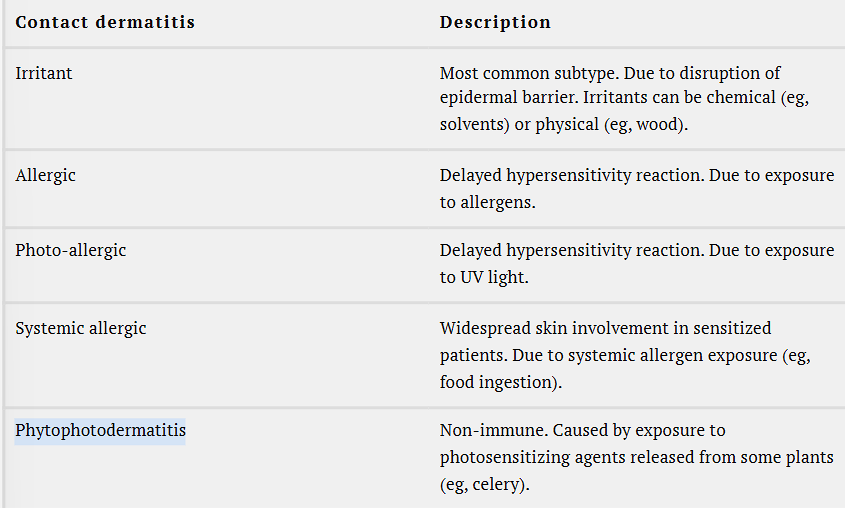
5 types of contact dermatitis
Irritant - most common, disrupts epidermal barrier and can be chemical or food irritants
Allergic - delayed hypersensitivity reaction due to allergen exposure
Photo-allergic - delayed hypersensitivity reaction to UV light
Systemic allergic - widespread skin involvement to sensitized patients, which is due to systemic allergen exposure like food ingestion
Phytophotodermatitis- non-immune, caused by exposure to photosensitizing agents released from plants
Clinical Presentation of allergic contact dermatitis (ACD)
ACD presents with erythematous, pruritic rash at the site of contact, rash is either linear or geometric
ACD lesions are indurated with distinct borders or edges
Develop vesicles or bullae (>1cm)
Patients complain of burning sensation at site of lesion
Initial rash spreads as papules, vesicles and bullae

ACD progresses to a chronic form if
allergen exposure is continued
Pathophysiology
caused by an environmental trigger in a genetically predisposed individual.
Allergens are environmental elements that trigger an allergic reaction when they come in contact with the skin.
Examples of such allergens include plants (eg, poison ivy, poison oak), metals (eg, nickel, gold), topical medications (eg, antibiotic), and others (eg, latex, rubber, fragrances, hair care products).
________ and certain _________ play a role in allergic skin reactions; increased ____ is also associated with increased ACD
Genetics and certain occupations can put individuals at risk for exposure to allergens
Increased age due to repetitive exposure to allergen
Allergic contact dermatitis is a type ____
4 hypersensitivity reaction, also known as delayed hypersensitivity reaction, a type of cell-mediated hypersensitivity reaction.
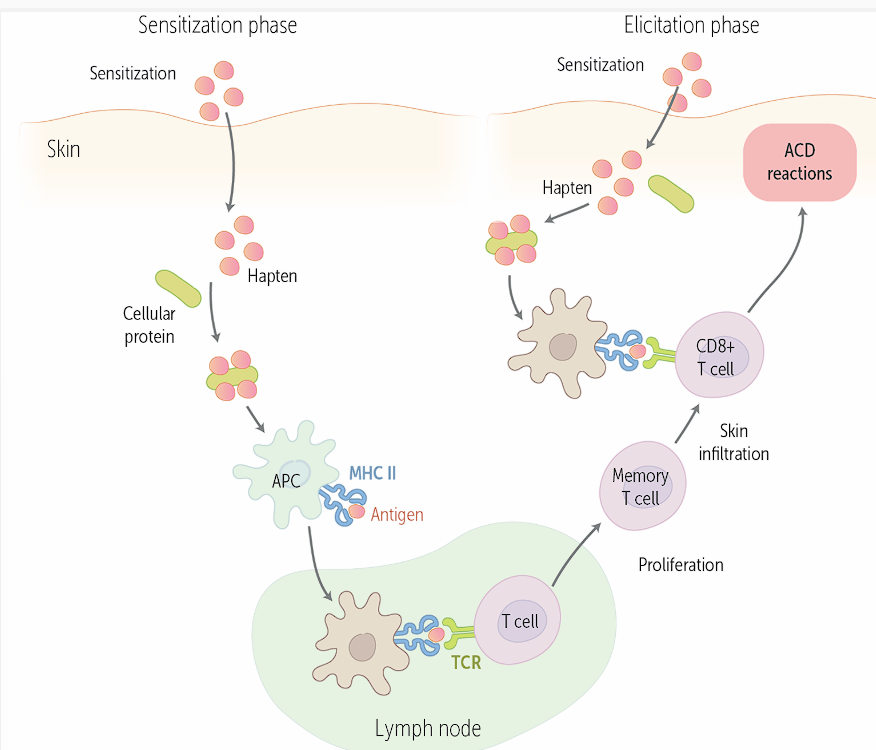
Reaction has the sensitization and elicitation phase
Two main phases of ACD/type 4 hypersensitivity
Sensitization — body takes in the allergen and it will be presented on APC’s membrane through MHC
The midpoint is lymph node, where APC presents antigen to T cell
T cell will bind with TCR and cause proliferation of memory T cells which infiltrate the skin, and become CD8 T cells that when interacting with the antigen again, will cause ACD reactions
In the elicitation phase, the hapten/allergen will be presented to the memory T cell, causing an immune response
Langerhans
thought to be a subset of dendritic cells, but are now considered to be a specialized subset of tissue-resident macrophages
Sensitization Phase
n the body is exposed to the allergen for the first time, it gets “primed.”
Haptens are low-molecular-weight molecules found in contact allergens.
Sensitization - Haptens trigger an immune response when
haptens bind to skin protein carriers to become visible to the immune system
Hapten protein will recognize APCs within skin, like Langerhans and dermal dendritic cells
APC engulf and process the tagged haptens before migrating to lymph nodes nearby
In the lymph nodes, APCs will present hapten protein on surface to naive T cells, which will generate memory T cells that are hapten specific and watch for subsequent exposure
Elicitation Phase
Subsequent exposure of allergen triggers a local inflammatory response. Haptens from the invading allergen bind to skin protein carriers
APCs engulf, process and present primed T cells in the epidermis, dermis and near by lymph node
T cells will release inflammatory mediators, which will cause skin inflammation
Takes 48-72 hours from time of re-exposure for ACD to present. This is known as
latency period and shortens with subsequent exposures
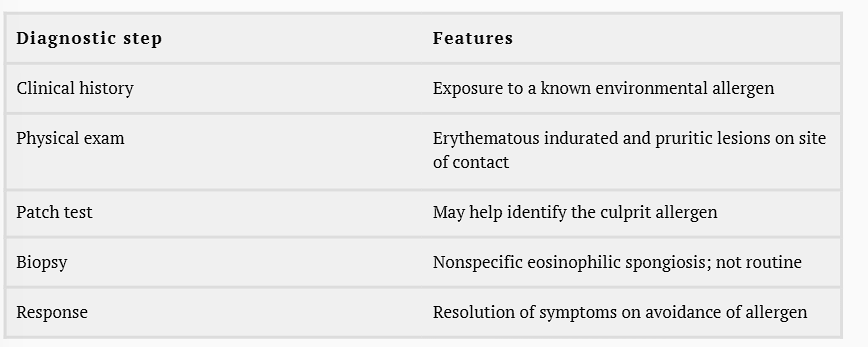
Diagnosis - 5 steps
Clinical history
Physical Exam
Patch test
Biopsy
Response
Management of ACD : Allergic dermatitis management is twofold
controlling the allergen and symptomatic treatment of skin inflammation.
Antigen control - identify trigger through pt history and a patch test - avoid the trigger or wear protective gear
Symptomatic treatment and chronic treatment
Symptomatic treatment of ACD lesions is with topical steroids. Systemic steroids may be considered if ACD is extensive.
If the disease is chronic or refractory to steroids, steroid-sparing immunosuppressants (eg, topical tacrolimus) or phototherapy may be used.
Examples of topical steroids include
Betamethasone, Fluticasone, Fluocinolone, Triamcinolone, and various Hydrocortisone preparations
ACD may be complicated by secondary bacterial infections or skin pigmentation change.
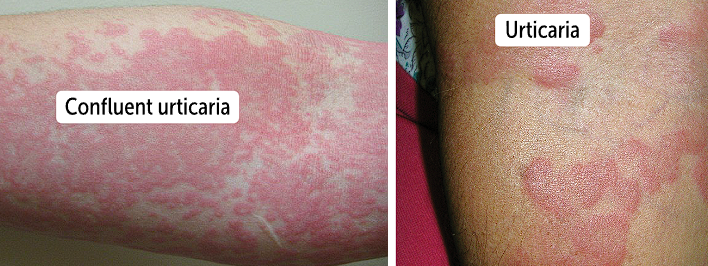
Urticaria
hives, is an allergic or skin condition that presents with intense itching, or pruritus.
Divided into acute (less than 6 weeks) and chronic (last more than 6 weeks)
Acute and chronic urticaria
effects children and adolescents while chronic urticaria affects adults
Clinical Presentation of urticaria
urticarial wheals appear as well-circumscribed, raised, erythematous plaques with areas of central pallor
Lesions are edematous and blanching
Lesions last about 24 hours and any part of body is impacted
From several mm to greater than 5 cm
Urticaria can be isolated, but can precede serious allergic reactions like anaphylaxis
Pathophysiology for acute urticaria, besides UPRTI, there are 3 major compounds that trigger urticaria
caused by allergic reaction mediated by IgE, which is usually caused by idiopathic causes, but also upper respiratory tract infections, medications, foods and infections
Infection with urticaria
Infection - bacteria and viral infections can be associated with acute urticaria
Common viruses are rotavirus and rhinovirus, hepatitis viruses, EBV, HSV
Bacteria such as Strep and Mycoplasma pneumoniae can also cause urticaria
Medication with urticaria
Most commonly associated medication is penicillin
Patients have urticarial reactions for up to 14 days after treatment with penicillin
Sulfonamides, muscle relaxants, diuretics and NSAIDS
Foods with urticaria
foods like peanuts, shellfish and milk, can cause acute urticaria symptoms
Acute urticaria is associated with
SLE, RA, Sjogren syndrome, celiac disease and autoimmune thyroid disease
Mechanisms for urticaria are due to ; degranulation process
specific IgE antibodies and mast cells, which are located in the dermis and are near bod surfaces
When IgE binds to mast cells, it will cause chemical release of mediators that cause allergy symptoms, such as histamine in a process called degranulation
IgE mediated pathway ; sensitization
Common way for mast cell degranulation, where bodies are exposed to new allergens, triggering B cells to release IgE in blood
IgE will bind to Fc-eR1 receptors on mast cell surface
This will sensitize the mast cells, which when re-exposed to the same allergen, will cross-link IgE proteins that are bound to mast cells
Will activate type 1 hypersensitivity
Non-IgE Mediated (Direct) Pathway
caused by C3a and C5a (anaphylatoxins) from the complement pathway, certain medications (eg, opiates and muscle relaxants), and foods (eg, tomatoes and strawberries) that can directly activate mast cells.
Common Final Pathway for mast cell degranulation
Symptoms show up quickly when activated mast cells release their preformed histamine, leukotriene C4, and prostaglandin D2 within their cytoplasm
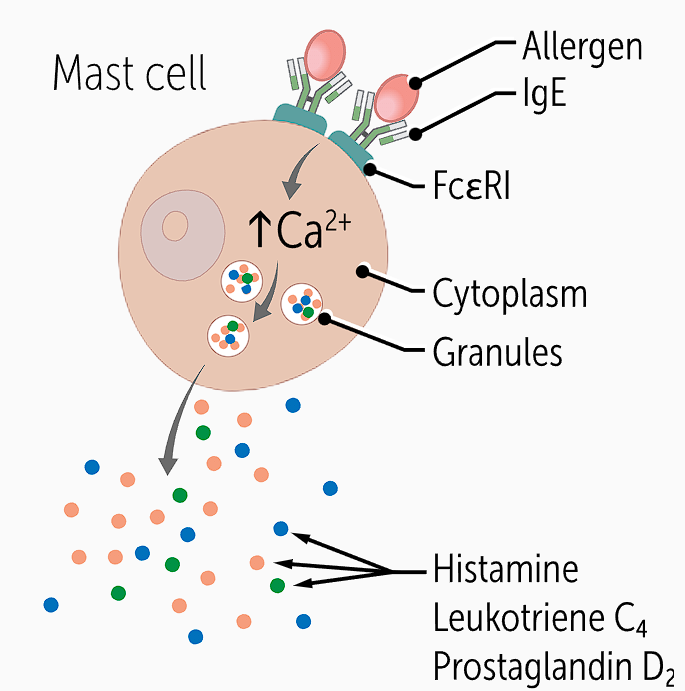
Histamine and prostaglandin cause (4)
vasodilation and thus redness; histamine and leukotrienes increase vascular permeability, leading to edema; and histamine also causes pruritus, leading to the itchy lesions
Acute urticaria diagnosis
history and physical examination of the characteristic skin lesions
differential may include atopic dermatitis (eczema), bullous pemphigoid and erythema multiforme
Atopic dermatitis (eczema)
a chronic inflammatory skin disorder characterized by dry skin and itchy rash, usually on flexor surfaces.
Skin thickens and fissures develop with time due to chronic itching.
Bullous pemphigoid
a bullous skin disorder that may be initially present with pruritic eczema-like or urticaria-like rash before the development of the classical tense skin bulla (blisters).
Patients with urticaria should be assessed for signs of/symptoms
a severe allergic reaction like anaphylaxis, and signs would include chest tightness or difficulty breathing, hoarse voice or throat tightness, nausea, vomiting, crampy abdominal pain and lightheadedness
Acute vs chronic urticaria
Diagnosis of acute urticaria can be made if characteristic skin lesions last less than 6 weeks, whereas lesions in chronic urticaria last more than 6 weeks
Skin prick test can identify allergens
Management - 2 steps
Control trigger and manage symptoms
Identify and remove the culprit trigger - if its a new medication or food, stop, if its an infection treat it and avoid other triggers
First line urticaria treatment is
H1 antihistamine therapy which will block histamine action on histamine receptors
newer second gen H1 blockers are preferred b/c there is less sedation, fewer anticholinergic adverse effects
Examples of firs gen (2) and second gen H1 blockers (2)
First gen - diphenhydramine and chlorpheniramine
Second gen - loratadine, cetirizine
Intramuscular H2 antihistamine therapy are used in emergent settings, drugs named
Ranitidine and famotidine
If antihistamine therapy fails, can use
short course of steroids
Prognosis of urticaria
Self limiting disease and will resolve in a few days
Most cases are isolated to the skin without systemic issue of anaphylaxis
Avoid cause and if idiopathic, increased chance of it causes chronic urticaria
Erythema multiforme (EM) and distinctive rash
acute inflammatory skin condition known for its distinctive rash resembling a target or bullseye
red rash with multiple morphology with a major and minor form based on severity
Prevalence of EM
Impacts people 20-30 y/o, prevalent among males than females
Clinical presentation of EM and typical size
target-like lesions on the skin which are initially round, erythematous papules which can be annular or targetoid papules
Will progresses to the target lesions which have dusky colored central area and erythematous base surrounded by a pale ring
Typical size is less than 3cm in diameter
EM major vs minor is based on
mucosal involvement
EM major will have cutaneous disease with severe mucosal involvement
EM minor will refer to cutaneous disease with mild or no mucosal involvement
Cutaneous lesions will manifest symmetrically on dorsal surface and then will spread toward the trunk

Other places that EM can have mucosal lesions
Conjunctiva (mucous membrane that lines eyelids), genitals and oral mucosa
Mucosal lesions in EM present with
erythema, erosions, or bullae

Half of EM cases are
idiopathic but other causes are due to infections and medications
Conjunctiva lesions can lead to
keratitis, scarring, and visual impairment, and genital lesions can cause painful urination
Keratitis can cause eye inflammation
Causes for EM
Half is idiopathic, other half is medication and bacteria that causes it
Infections include viral, fungal and bacteria
Most common microbe that causes EM is herpes simplex viruses
Mycoplasma pneumoniae infection has been linked to EM, especially in children
Important names for sulfa drugs to remember
sulfonamide antibiotics, such as Trimethoprim-Sulfamethoxazole.
Sulfasalazine (used for the treatment of arthritis) is also a sulfa drug
EM and hypersensitivity
type 4 hypersensitivity reaction due to the involvement of CD4+ T lymphocytes and CD8+ cytotoxic T lymphocytes.
Type 4 hypersensitivity response is also called a delayed hypersensitivity reaction because it usually takes at least 48 hours after exposure to an antigen for the tissue reaction to show up
Th1 cells will be sensitized to activate macrophages
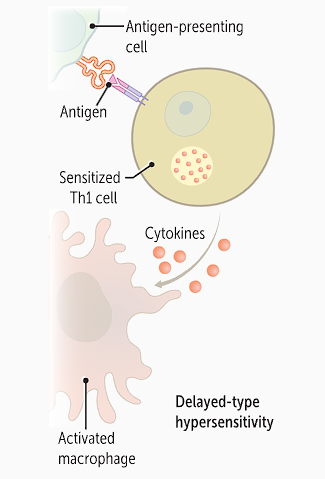
APCs will take up antigenic bacterial, viral or drug particle and
then present the antigens to CD4+ helper T cells. This activates CD4+ cells and they release interleukin 2 (IL-2), which differentiates T cells
Differentiated Th1 cells will then secre IFN-y and Th17 cells secrete IL-17 and IL-22
IFN-y, IL-17 and IL-22
IFN-γ activates macrophages, stimulating release of the cytokines tumor necrosis factor (TNF) and IL-1, causing inflammation.
IL-17 and IL-22 recruit neutrophils and monocytes to cause more damage
CD8 T cells mediated inflammation
involves killing antigen presenting cells when they take up antigens. These T cells are activated when their T-cell receptor binds APCs and release perforins, granzymes, and IFN-γ. These three cytokines cause cellular apoptosis and inflammation
perforins and granzymes work together to cause apoptosis while IFN-y will cause inflammation by activating macrophages and production of IL-1 and TNF-a for inflammation
Diagnosis of EM is made clinically based on history and physical examination.
Skin biopsy is not required unless the diagnosis is unclear
Hallmark sign is target lesions on skin on distal extrremities after known infection (HSV) or drug intake
EM major is diagnosed vs EM minor is diagnosed
EM major is diagnosed when the disease has 2 or more mucosal surfaces
There can be systemic issues like fever, fatigue and muscle aches
EM minor is diagnosed when one or no mucosal surfaces involved
Differential diagnosis with EM multiforme
Stevens-Johnson syndrome - which is a mucocutaneous reaction to drugs causing skin necrosis
SJS will have shows on truncal skin, with palness and tenderness at lesion site
Urticaria
Skin manifestations in SLE
Bullous disorders like pemphigus
The management of erythema multiforme is twofold: controlling the trigger and treating the disease
Find infection or trigger like new medication and treat the cause
Med management is determined based on severity of disease
Treat minor EM symptomatically, like
oral histamines for itchiness
Topical steroids for painful lesions
EM major needs intensive therapy with
systemic oral steroids in short courses
ocular involvement is vision threatening and needs immediate referral
EM rash is
self limiting, going away on its own
In rare cases, the patient will progress to chronic EM
A 25-year-old male presents to the clinic complaining of severe itchiness on both of his forearms. He reports that he just finished a 7-day course of penicillin for streptococcal pharyngitis. On examination of the skin, there are wheals with a central pink color and peripheral erythema of about 2 cm in diameter. The lesions are not painful and they blanch when pressed. Which of the following events is associated with the pathogenesis of these lesions?
Allergens bind to IgE that are attached to FcεRI receptors on mast cells.
Our immune system responds to allergens by recruiting Th2 cells, which releases IL-4, IL-5, and IL-13.
Recruitment of CD4+ Th1 cells that in turn releases IFN-γ.
Upregulation of E-cadherin on the CD34+ cells.
The correct answer is allergens bind to IgE that are attached to FcεRI receptors on mast cells (A). This activates mast cells and they release their preformed histamine, leukotriene C4, and prostaglandin D2. These vasoactive mediators lead to vasodilation and increase vascular permeability. This contributes to edema and the histamine causes pruritus. Our immune system responding to allergens by recruiting Th2 cells, which releases IL-4, IL-5, and IL-13 (B), is involved in the pathogenesis of atopic dermatitis. Recruitment of CD4+ Th1 cells that in turn releases IFN-γ (C) and upregulation of E-cadherin on the CD34+ cells (D) are part of the pathway for EM.
A patient with confirmed herpes simplex virus type 1 presents to the clinic with target-like lesions on the dorsum of his hands that are about 1 cm in diameter. He denies any other recent infections or use of any medications. What type of lymphocytes are involved in the pathogenesis of this condition?
B lymphocytes
Natural killer cells
Plasma cells
T lymphocytes
The correct answer is T lymphocytes (D). The clinical presentation describes erythema multiforme. They typically present with target-like lesions of <3 cm in diameter. It is strongly associated with herpes simplex virus infection. The pathogenesis involves a type 4 hypersensitivity, and this involves CD4+ T lymphocytes and CD8+ cytotoxic T lymphocytes. B lymphocytes (A) and plasma cells (C) are involved in type 1 hypersensitivity, as in urticaria. Natural killer cells (B) are a type of cytotoxic lymphocytes; however, they are not involved in the pathogenesis of erythema multiforme.
A 24-year-old male comes to the clinic with an itchy rash on his lower legs after returning from an expedition trip to Mexico that involved mountain climbing. The lesions are erythematous, indurated, and scaly. The patient had a similar rash a year ago. The physician reaches a diagnosis clinically and decided to treat him with topical steroids. What is the cause of this patient’s rash?
Type 1 hypersensitivity reaction
Type 2 hypersensitivity reaction
Type 3 hypersensitivity reaction
Type 4 hypersensitivity reaction
Nonimmune reaction
The correct answer is type 4 hypersensitivity reaction (D). This patient is most likely suffering from allergic contact dermatitis (ACD) due to exposure to poison ivy during his trip. ACD is caused by a type 4, delayed, cell-mediated, hypersensitivity reaction, which involves a sensitizing phase and an eliciting phase. Allergen haptens bind to skin protein carriers and trigger priming and subsequent activation of T cells on re-exposure. Type 1 hypersensitivity reaction (A) (eg, atopy, anaphylaxis) is mediated by preformed immunoglobulins. A type 2 hypersensitivity reaction (B) (eg, Goodpasture disease) is mediated by its antibodies. A type 3 hypersensitivity reaction (C) (eg, systemic lupus erythematosus) is mediated by immune complexes. A nonimmune reaction (E) (eg, phytophotodermatitis) occurs from exposure to toxins released from plants.