Nutrition 29 | Nutrition for Liver Disease and Gallstones
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
What is fatty liver?
It's a buildup of fat in the liver due to imbalance between fat made by the liver and fat used/exported.

What happens to excess fat in the liver?
It’s packaged into VLDLs and sent into the bloodstream.
What are common causes of fatty liver?
Metabolic defects/insulin resistance
Excess alcohol intake
Drug use
What are the consequences of fatty liver?
May be asymptomatic
Can lead to inflammation, liver enlargement, fatigue
In severe cases, cirrhosis, liver failure, or cancer
What lab findings suggest fatty liver?
Elevated liver enzymes (ALT, AST), and elevated triglycerides, cholesterol, and insulin.
How is fatty liver treated?
Remove the cause (e.g., stop alcohol, manage diabetes)
Weight loss and physical activity
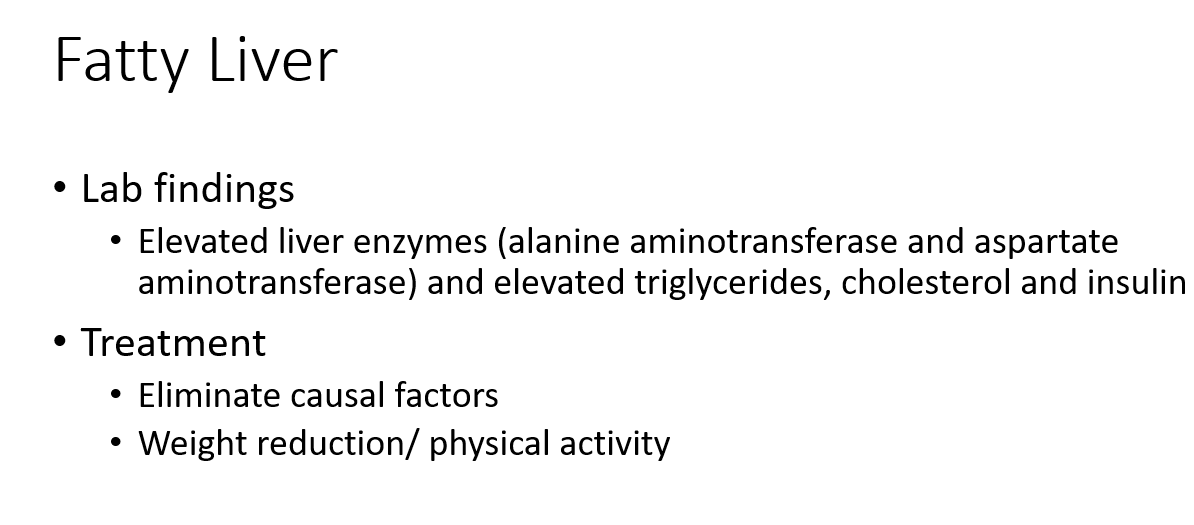
What is hepatitis?
Hepatitis is liver inflammation caused by damage to liver tissue.
What are the main causes of hepatitis?
Infections with specific viruses:
Hepatitis A: fecal-oral transmission
Hepatitis B: bloodborne, sexual transmission, mother to infant in childbirth
Hepatitis C: bloodborne (no vaccine)
Excessive alcohol intake
Drug and toxin exposure
Fatty liver disease
Autoimmune disease
What symptoms are associated with hepatitis?
Fatigue, nausea, anorexia, pain in liver, jaundice, elevated liver enzymes
Varies by cause and severity
May be asymptomatic in mild cases
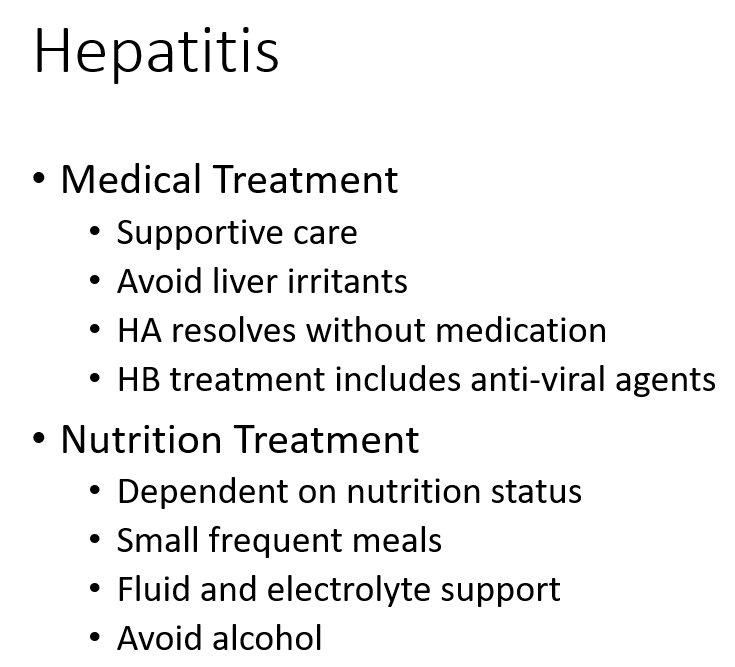
What is the medical treatment for hepatitis?
Supportive care
Avoid liver irritants
Hepatitis A (HA): typically resolves without medication
Hepatitis B (HB): may require anti-viral agents
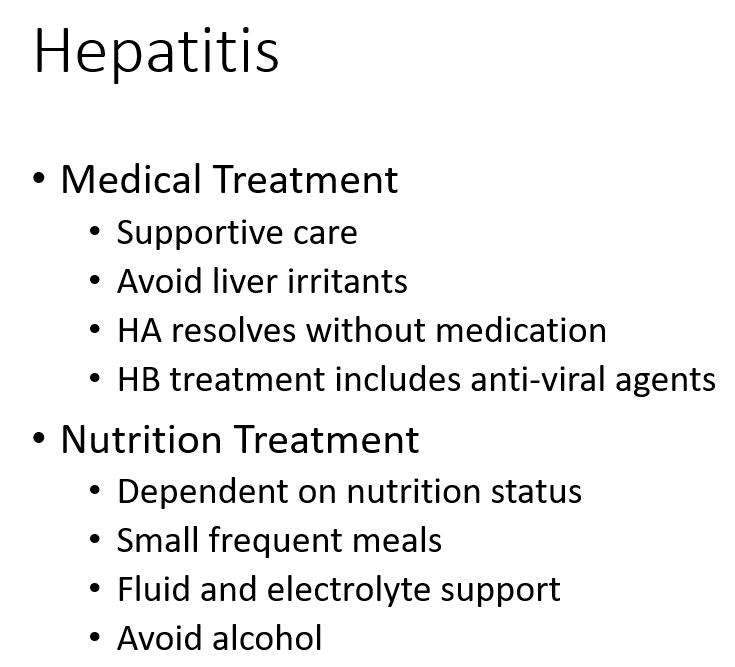
What nutrition treatment is recommended for hepatitis?
Based on nutritional status
Small frequent meals
Fluid and electrolyte support
Avoid alcohol
What are the major causes of cirrhosis?
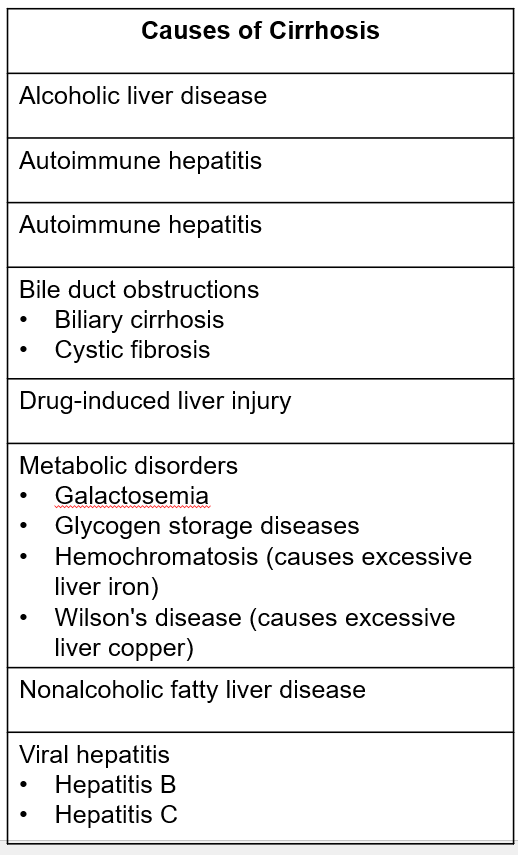
What is cirrhosis?
Cirrhosis is an advanced stage of liver disease marked by extensive scarring that leads to impaired liver function and potentially liver failure.
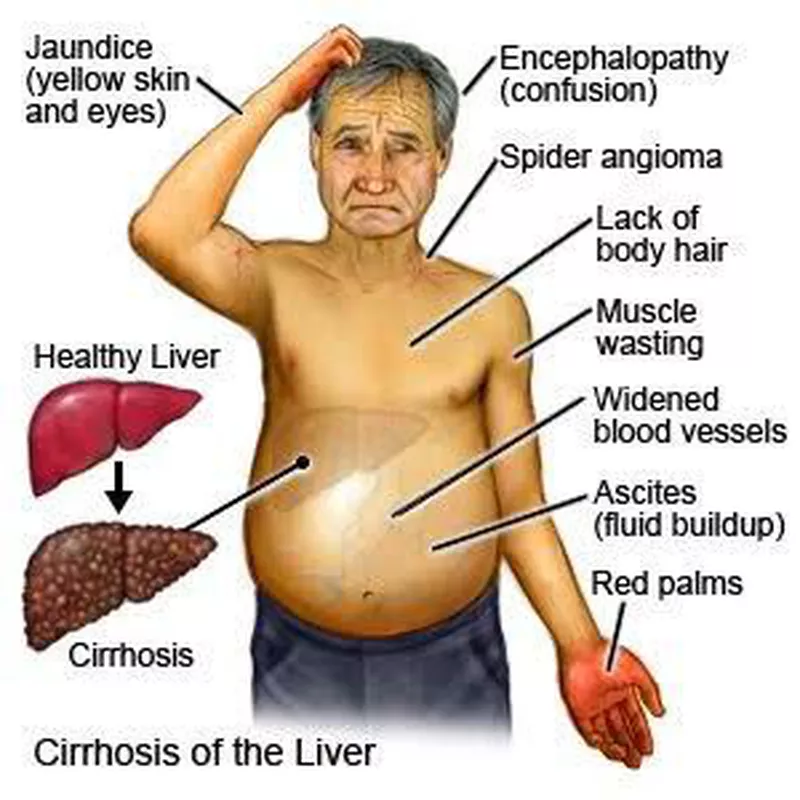
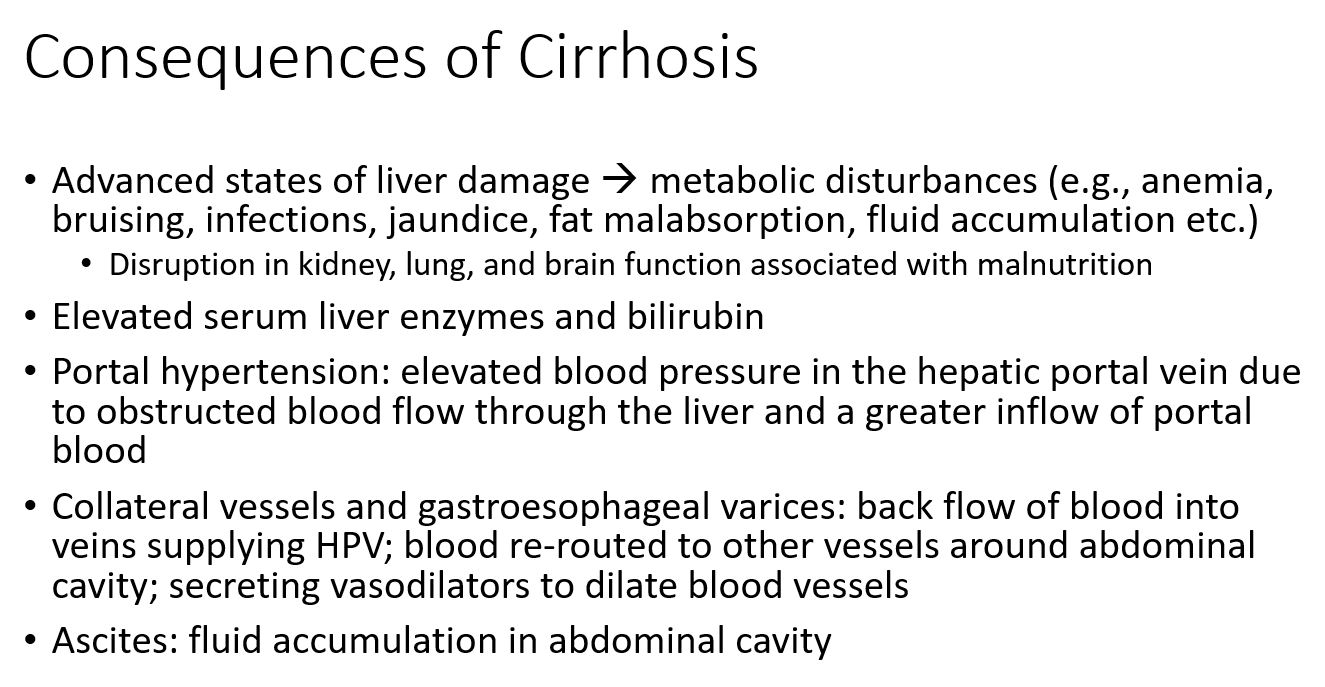
What are the complications of cirrhosis?
Metabolic issues like anemia, bruising, jaundice, poor fat absorption, infections, and fluid buildup.
Organ dysfunction in the kidneys, lungs, and brain due to malnutrition.
Elevated liver enzymes and bilirubin levels (signs of liver stress).
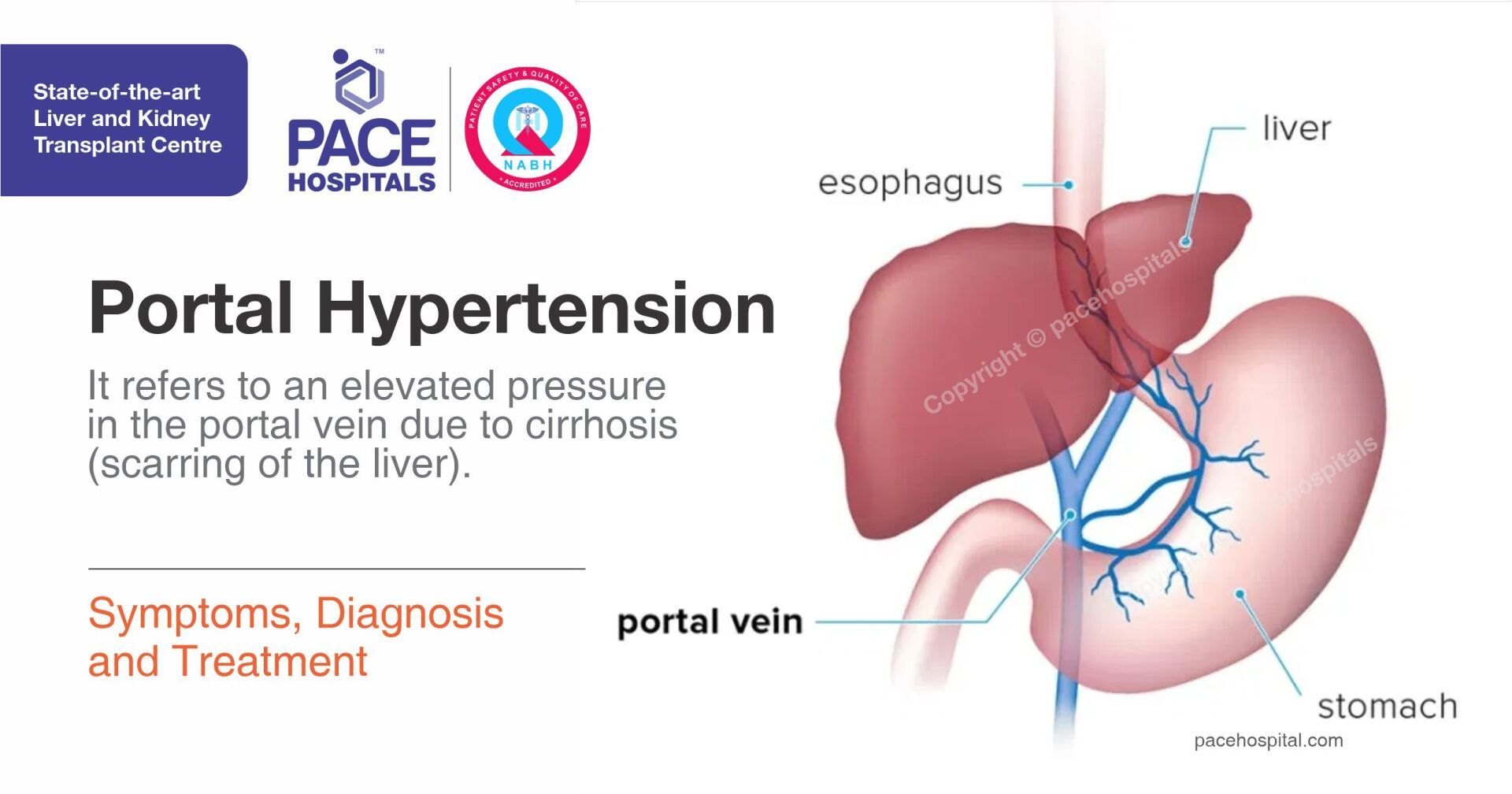
Portal hypertension: high pressure in the vein to the liver from blocked blood flow.
Varices: enlarged veins in the abdomen or esophagus that can rupture and bleed.
Ascites: fluid buildup in the belly.
These occur because the liver is scarred and can't function properly anymore.
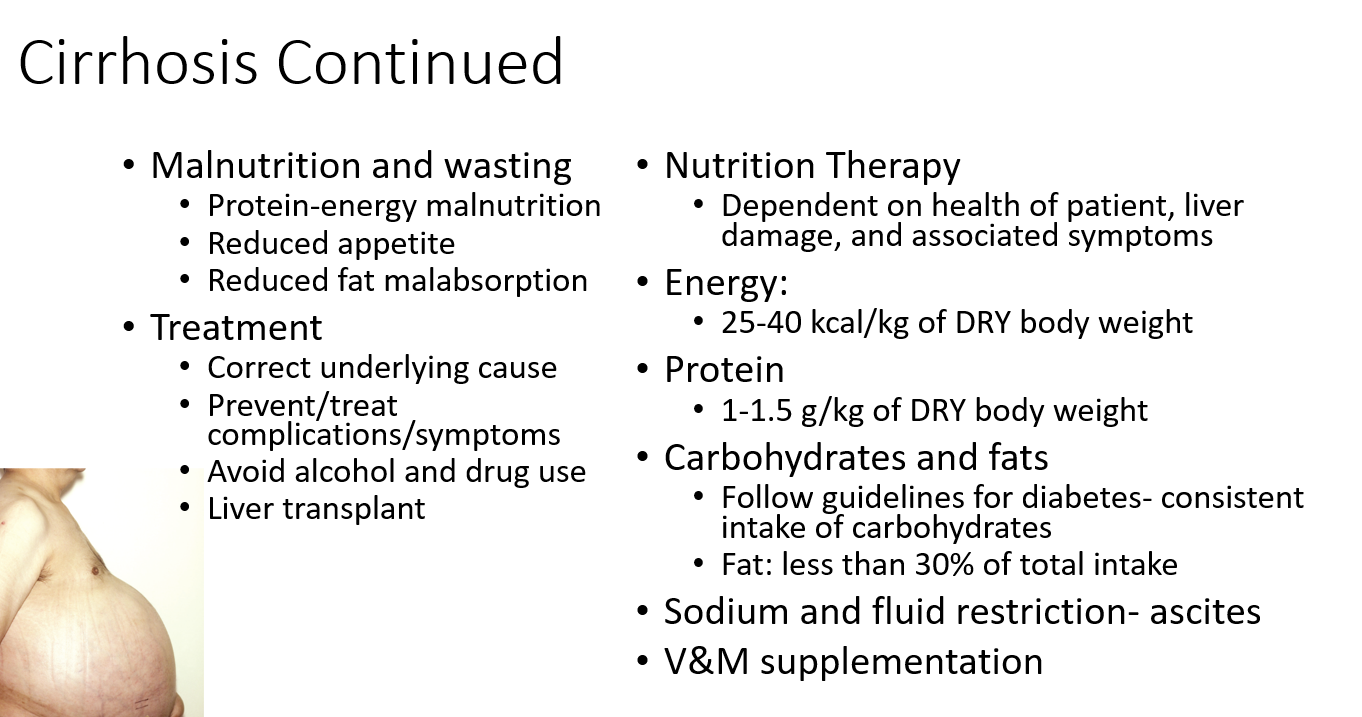
What causes malnutrition in cirrhosis?
Poor appetite
Fat malabsorption
Protein-energy malnutrition (loss of muscle and fat)
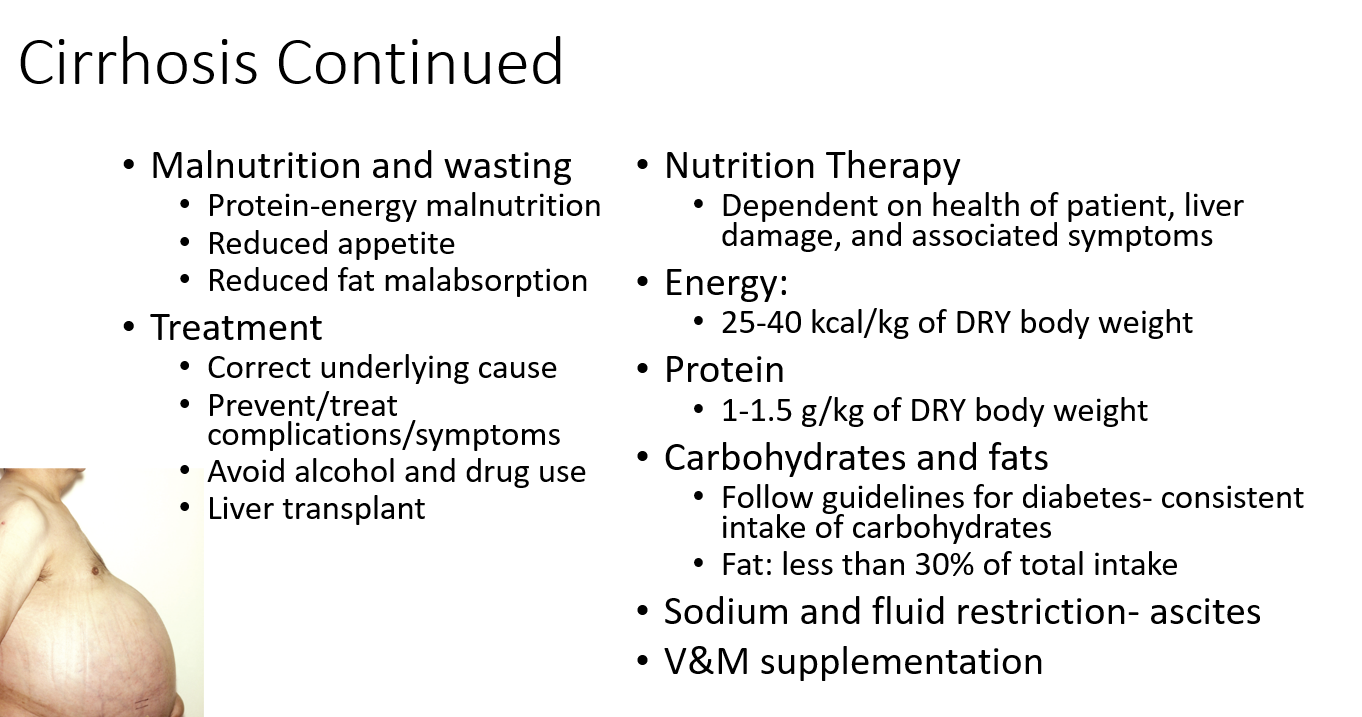
What is the general treatment for cirrhosis?
Fixing the root cause
Managing complications
Avoiding alcohol and drugs
Liver transplant if needed
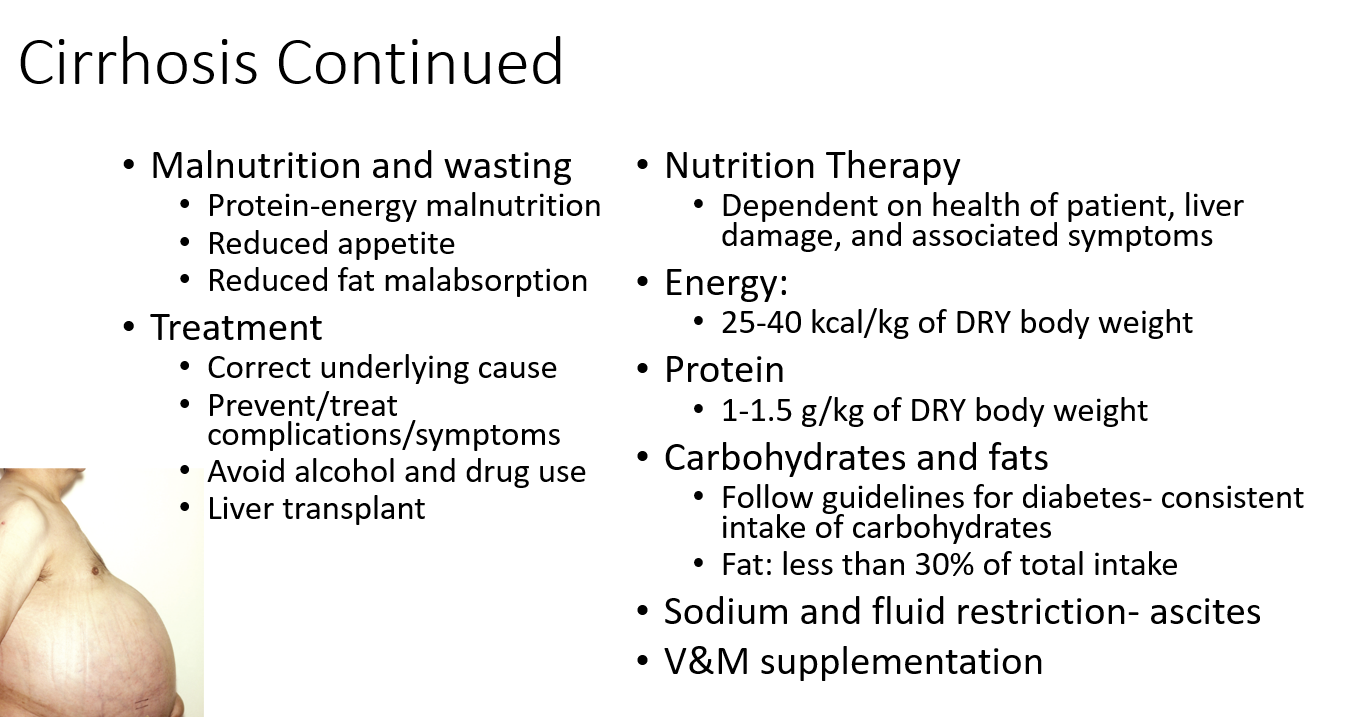
What is the nutrition therapy for cirrhosis?
Calories: Provide enough energy based on the person’s needs and body size
Protein: Include a moderate amount to support healing and prevent muscle loss
Carbohydrates: Keep intake steady throughout the day, similar to diabetes management
Fat: Limit fat to a smaller portion of the total diet
Sodium & Fluids: Restrict both if there’s fluid buildup in the belly (ascites)
Vitamins & Minerals: Supplement if the person isn’t getting enough through food
How does blood flow change in cirrhosis?
Scarring blocks normal blood flow through the liver, increasing pressure in the portal vein (called portal hypertension).
What causes reduced nutrient intake in cirrhosis?
Abdominal discomfort, nausea, vomiting
Early fullness from ascites
Taste changes, anorexia
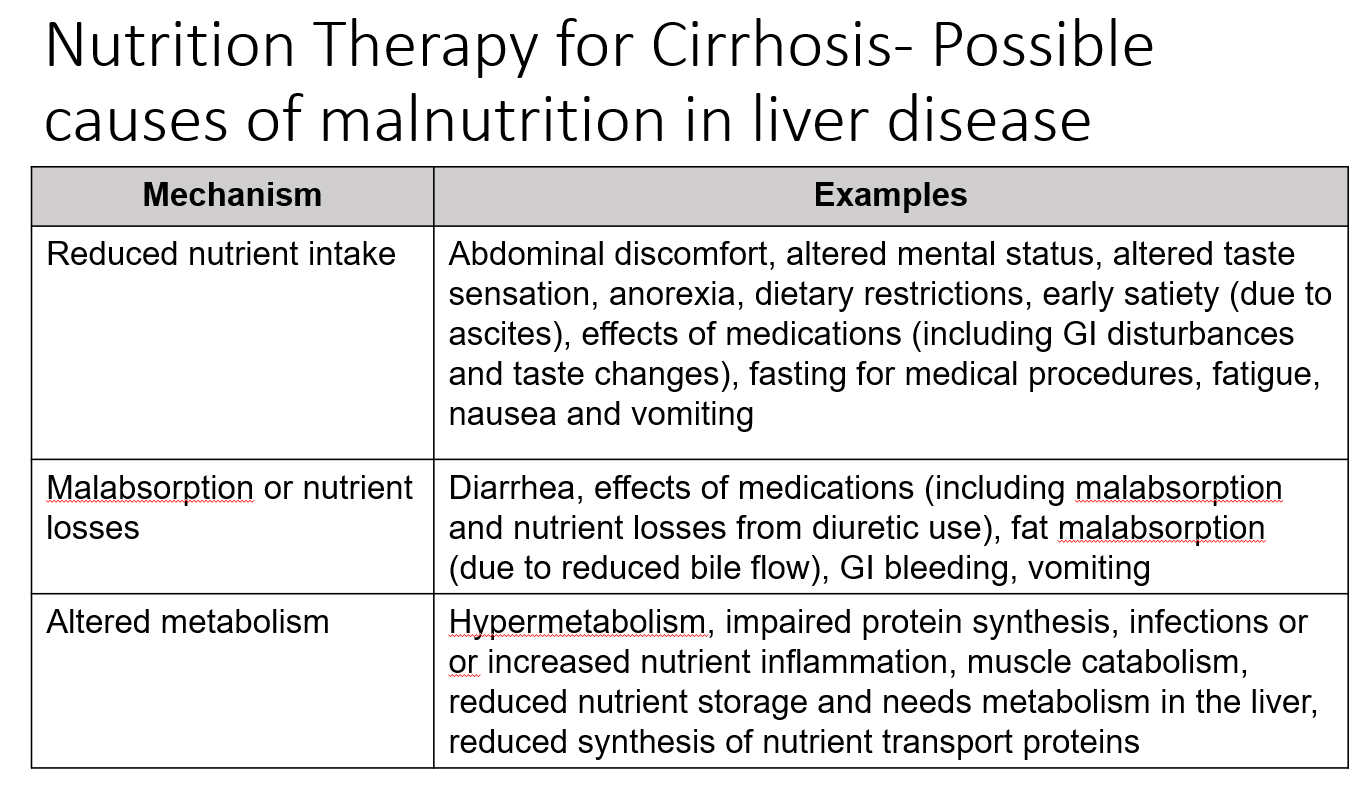
How does malabsorption lead to malnutrition in cirrhosis?
Diarrhea
GI bleeding
Vomiting
Fat malabsorption (↓ bile flow)
Medication side effects
How does altered metabolism contribute to malnutrition?
Hypermetabolism
Increased inflammation or infections
Poor protein synthesis
Muscle breakdown
Reduced storage or transport of nutrients in liver
When is a liver transplant necessary and how is patient priority determined?
They are needed in liver failure, often due to chronic hepatitis C or alcoholic liver disease.
Priority on the transplant waiting list is based on illness severity.
Why is nutrition status important in liver transplant patients?
Poor nutrition status can complicate surgery. It's essential to check for and correct malnutrition before transplantation.
What are the main concerns after a liver transplant?
Immunosuppressive drugs (risk of rejection and infection)
GI side effects
Need for increased protein and energy for proper healing
What are gallstones?
Solid stones formed in the gallbladder from crystalline deposits of cholesterol and/or bilirubin.
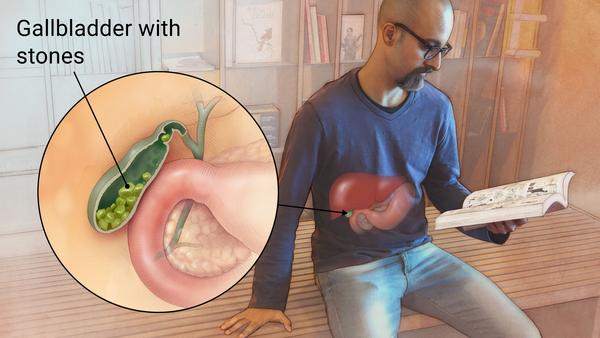
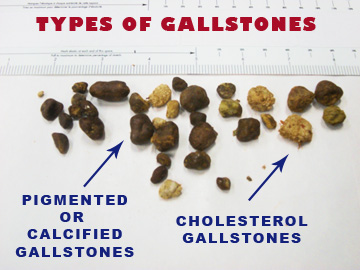
What are the two main types of gallstones?
Cholesterol gallstones (90%): Form when bile becomes too concentrated, creating sludge; range from pea- to golf ball-size.
Pigment gallstones: Made from bilirubin salts, linked to infections or RBC breakdown; usually soft and crushable.
What are the complications of gallstones?
Most are asymptomatic (75–80%).
If bile duct is blocked, pain becomes steady and severe.
Inflamed or swollen gallbladder
Gallbladder rupture
What are key risk factors for cholesterol gallstones?
Aging: bile composition changes, stones don’t dissolve easily
Pregnancy:
Estrogen ↑ bile cholesterol
Progesterone ↓ gallbladder motility
Obesity: ↑ cholesterol production = more in bile
Female gender: higher estrogen
Ethnicity:
Highest risk: Native Americans
Lowest: African Americans, Asians
What is the surgical treatment for gallstones?
Cholecystectomy (removal of the gallbladder) is the main surgical option.
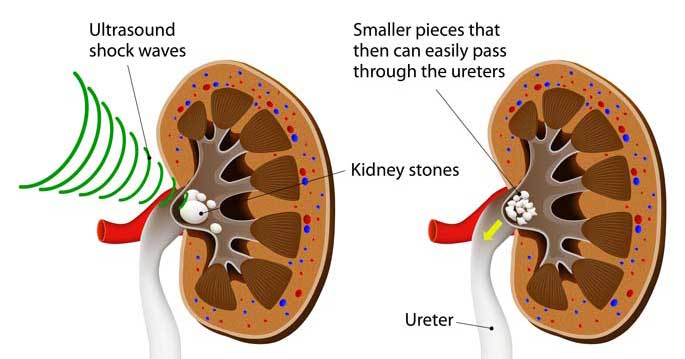
What are the non-surgical treatments for gallstones?
Used for small cholesterol stones.
Drug therapy helps lower cholesterol levels in bile.
Shock-wave lithotripsy uses sound waves to break up gallstones.