Drug Actions and Drug Responses
1/207
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
208 Terms
What is pharmacokinetics the study of?
Drug movement throughout the body.
What is the process by which a drug is carried throughout the body to tissues and organs?
Distribution.
how drug is carried to the tissues
What is the process of chemically altering a drug, usually in the liver?
Metabolism.
enzymatically
What is the process of removing a drug from the body, often via kidneys/urine?
Excretion.
how we get the rest of that drug, the reminence and non active pieces out of the body
What term describes how long drug responses last and how they change over time?
Time course of drug responses.
Do drugs create new cellular functions?
No, drugs do not create new cellular functions.
it cannot make your body do something that it is not equipped to do
not going to all of a sudden make kidneys work like a pancrease
What do drugs alter in the body?
The rate of existing functions.
stimulate GI tract to move faster (laxitives)
What type of drug action involves stimulation? Give an example.
Stimulate → Example: Laxatives.
What type of drug action involves depression? Give examples.
Depress → Example: CNS drugs, sedatives.
What type of drug action involves replacement? Give examples.
Replace → Example: Insulin, other hormones.
What type of drug action involves destruction? Give examples.
Destroy → Example: Antibiotics, anticancer drugs.
killing cancer cells
What is the general principle of drug action in simple terms?
Drugs help the body help itself.
How do drugs cause action at the cellular level?
By forming chemical bonds with receptors.
they have to get attached to the cell somehow
How many main ways do drugs move through membranes?
Three ways.
What is one way drugs can move through membranes using small openings?
Channels or pores.
very few meds do this
drug would have to be very very small
What is one way drugs can move through membranes with the help of carriers?
Transport system.
very often
attach to something that carries it in
how oral drugs get in the system in GI tract
What protein can move drugs out of cells across membranes?
P-glycoprotein.
PGP
one of the really important proteins that help carry
What is the most common way drugs cross membranes?
Direct penetration of the membrane.
most membranes are primarily lipid base
so most meds that go through the membrane that way have to be lipid soluble
What is the definition of absorption in pharmacology?
Movement of a drug from its site of administration into the blood.
What does the rate of absorption determine?
How soon effects will begin.
slow to absorb means it takes a while for that drug to kick in
What does the amount of absorption help determine?
How intense the effects will be.
how much it is soluble
if i know a med doesnt absorb super well through a certain route, i have to dose knowing that i may need a higher dose to get the effect needed
What are the three main factors that affect drug absorption?
Drug solubility, drug ionization, and blood flow.
How does drug solubility affect absorption?
Drugs that are more soluble are absorbed more easily.
lipid soluble absorb and work faster
they dont need help to get through
more surface area=more of the medication absorbed
How does drug ionization affect absorption?
Non-ionized (uncharged) drugs are absorbed more readily than ionized (charged) drugs.
ionized absorb more poorly
non ionized are lipid soluble so they are easier absorbed
How does blood flow affect drug absorption?
Greater blood flow at the site of administration leads to faster absorption.
not good blood flow to gut means you will not absorb medication super well
IV drugs to someone without a pulse will go no where
What four aspects are considered when evaluating routes of drug administration?
Barriers to absorption, absorption pattern, advantages, disadvantages.
What are the barriers to absorption for intravenous (IV) drugs?
None — absorption is bypassed (goes directly into the bloodstream).
they are absorbed immediately and completely
What is the absorption pattern for IV drugs?
Instant and complete.
What are the advantages of IV administration?
rapid onset
precise control over drug levels- giving 3 units of insulin is exactly what they will get
allows use of large fluid volumes
can use drugs that would irritate tissues
What are the disadvantages of IV administration?
Risk of infection
Irreversible
expensive
inconvenient- you need an RN to do it
risk of fluid overload if using a lot of fluid
risk of embolism in IVs
What is the main barrier to absorption for IM drugs?
You need to make sure you have blood flow to that muscle
a pt with a crappy blood pressure is not getting flow to muscle
What is the absorption pattern for IM drugs?
Can be rapid or slow depending on drug solubility and blood flow to injection site.
What are the advantages of IM administration?
Good for poorly soluble drugs
Can be used for depot preparations (slow, sustained release)
can be good for pts who have hard time remembering to take med because it lasts a long time (?)
What are the disadvantages of IM administration?
Can hurt bad
inconvenient because you need nurse to do it
make sure pt is not on anti coagulants because you are worried about bleeding
What are the barriers to absorption for subcutaneous drugs?
There are no significant barriers; absorption is similar to IM.
still dependent on blood flow
How does the absorption pattern of subcutaneous drugs compare to IM?
Very similar to intramuscular (can be rapid or slow depending on solubility and blood flow).
What are advantages of subcutaneous administration?
Suitable for small volumes, relatively easy, can use for some depot preparations.
What are disadvantages of subcutaneous administration?
Pain, irritation, potential for tissue damage.
What are the main barriers to absorption for oral drugs?
Gastrointestinal lining, pH, presence of food, enzymatic degradation.
barrier to absorption is that it goes through liver before body so it may take time for it to hit
What is the absorption pattern for oral drugs?
Slower than parenteral routes; highly variable depending on drug and GI factors.
two drugs sometimes in the same class can absorb differently
if you have diarrhea you are going to get rid of it really fast
constipation means you will get more drug than needd
How do oral drugs move after absorption?
They enter the portal circulation and go through the liver (first-pass metabolism) before reaching systemic circulation.
first pass metabolism is because of blood flow in the into the splenic and empties into the liver and liver metabolizes and then pumps into system
EVERYTHING ORAL GOES THROUGH FIRST PASS
SUBLINGUAL, IV, SUBQ, RECTAL SUPPOSITORIES, AND BUCCAL DO NOT GO THROUGH FIRST PASS
anything that goes through GI tract goes through first pass
What are the advantages of oral administration?
easy
convenient
safe
suitable for self administration
reversible
What are the disadvantages of oral administration?
variable absorption
amount that gets inactivated
pt needs to be able to swallow
cause GI upset
What are common oral drug preparations?
Tablets, enteric-coated preparations, sustained-release preparations.
What is a key feature of enteric-coated oral preparations?
They resist dissolution in the stomach and dissolve in the intestine to prevent irritation or degradation.
What is the purpose of sustained-release oral preparations?
To release the drug slowly over time for prolonged effects and reduced dosing frequency.
cannot crush
What is a topical route of administration?
Application of drugs directly to the skin or mucous membranes for local effect.
What is a transdermal route of administration?
Drug is applied to the skin but absorbed into systemic circulation for systemic effects.
patches
What is an inhaled route of administration?
Drug is breathed into the lungs for local or systemic effect.
breathing treatment
What is a rectal route of administration?
Drug is inserted into the rectum for local or systemic effect; useful if oral is not possible.
What is a vaginal route of administration?
Drug is inserted into the vagina for local treatment.
What is direct injection as a route of administration?
Injection of drugs directly into a body cavity, tissue, or organ for localized effect.
nerve blocks, anesthetics, joint injections
What factors affect drug distribution in the body?
Local blood flow, competition for binding sites, hypoalbuminemia, and tissue binding.
How does local blood flow affect drug distribution?
Areas with higher blood flow receive drugs more quickly; poorly perfused tissues receive them more slowly.
is there a tumor blocking binding
What is meant by competition for binding sites in drug distribution?
Drugs can compete for protein binding sites (like albumin), affecting how much free drug is available to act.
certain binding sites may have multiple drugs that cab bind to so there is competition
How does hypoalbuminemia affect drug distribution?
Low albumin levels increase the amount of free drug, which can intensify effects or toxicity.
if not a lot of protein for drugs to bind to, they wont get distributed well
What is tissue binding in drug distribution?
Some drugs bind to specific tissues, which can serve as a reservoir and affect duration and intensity of drug action.
are they able to bind to tissues like bones, teeth, etc
What is the blood-brain barrier (BBB)?
Tight junctions between the cells that form the walls of most capillaries in the central nervous system.
on purpose so that not everything can pass through there
How must drugs pass to cross the blood-brain barrier?
They must pass through the cells of the capillary wall.
What types of drugs can cross the blood-brain barrier effectively?
Drugs that are lipid soluble or that have a specific transport system.
they have to have something to get past that
babies dont have BBB until 12 months
Do the membranes of the placenta completely block drug passage?
things cross back and forth
anything given to mom is assumed to be given to the baby
How is drug movement across the placenta determined?
In the same way as it is for other membranes (depending on lipid solubility, transport systems, and ionization).
What are the risks of drug transfer across the placenta?
Birth defects, low birth weight, physical anomalies, alterations in mental aptitude, and risk of drug dependency if mother uses opioids.
What can happen if a mother habitually uses opioids during pregnancy?
The baby can be born drug-dependent.
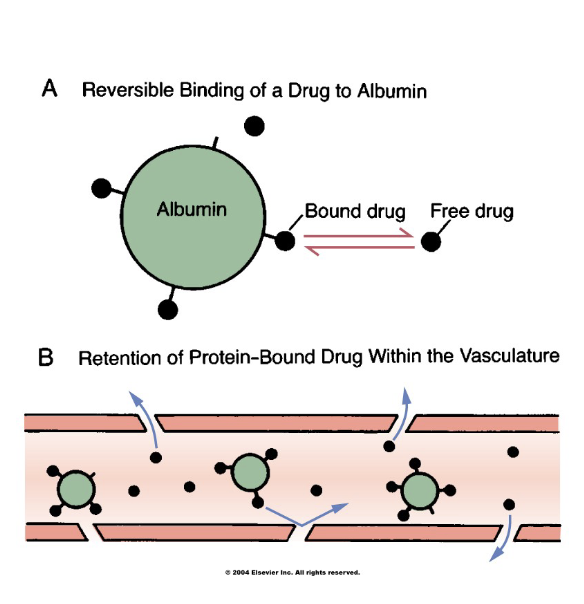
What is protein binding in pharmacology?
The reversible formation of bonds between drugs and proteins in the body.
that is what carries them through body and gets them where they need to go
Which protein is most abundant and important for drug binding?
Plasma albumin.
always in the blood stream
What is a key characteristic of plasma albumin?
It is a large molecule that always remains in the bloodstream.
How does protein binding affect drugs?
It affects drug distribution by controlling how much free (active) drug is available.
warfarin and albumin have a very high affinity for each other (90% bound)
if more albumin is bound, it stays in blood stream for a while and takes a while to get out
albumin bounding affects half lives
until drug hits the receptor, effects do not happen
more drug free floating in blood stream means more liekly to see bad side effects
Why must some drugs enter cells?
To reach their site of action or to undergo metabolism and excretion.
that pill needs to get exactly to cells to make it happen
Do all drugs need to cross the cell membrane to produce effects?
No, many drugs act by binding with receptors on the external surface of the cell membrane.
most are hitting to receptor sites
How do drugs that bind to cell surface receptors differ from those that enter cells?
They do not need to cross the cell membrane to produce their effects.
How do drugs interact with receptors?
Like a lock and key – the drug and receptor must have compatible shapes.
What is an agonist?
A drug that has affinity for a receptor and efficacy, meaning it can activate the receptor to produce a response.
it is going to turn that cell on and make it do the thing its supposed to do
What is an antagonist?
A drug that has affinity for a receptor but no efficacy, meaning it binds but does not activate the receptor.
it binds just doesnt work
beta blocker- blocks the receptor to begin with
What is drug metabolism (biotransformation)?
The process of decreasing the amount of active drug in the body, usually by chemical inactivation.
How are drugs chemically inactivated during metabolism?
hey are converted into more water-soluble compounds or metabolites.
so it can be fully absorbed for excretion
What is the major site of drug metabolism?
The liver.
for most drugs
most medications, issue if lover doesnt work well bc raises risk for toxicity
What are other sites where metabolism can occur?
Lung, kidney, and small intestine.
Which enzyme system is responsible for most drug metabolism?
Cytochrome P450 isoenzymes.
Which drugs can be metabolized?
Only free/unbound drugs (not protein-bound).
drugs have to be unbound from albumin
What is one therapeutic consequence of drug metabolism related to the kidneys?
Accelerated renal drug excretion.
i also gave a whole bunch of lasiks, i am going to excrete out that medication factor
How can metabolism affect drug activity?
It can cause drug inactivation or increased therapeutic action (because of slow or altered metabolism)
What is the effect of metabolism on prodrugs?
It can activate prodrugs into their active forms.
has to change into something else to work
How can metabolism affect drug toxicity?
It can increase or decrease toxicity depending on the drug and metabolites.
Can metabolism ever decrease toxicity?
Yes, metabolism can convert some drugs into less toxic forms, reducing adverse effects.
What are some special considerations that affect drug metabolism?
Age, induction of drug-metabolizing enzymes, first-pass effect, nutritional status, and competition among drugs.
How does age affect drug metabolism?
Infants and older adults often metabolize drugs more slowly due to immature or declining liver function.
What is induction of drug-metabolizing enzymes?
When drugs stimulate liver enzymes, speeding up the metabolism of themselves or other drugs.
What is the first-pass effect?
The liver metabolizes some drugs extensively after oral administration before they reach systemic circulation, reducing their bioavailability.
makes it take a second
How does nutritional status affect drug metabolism?
Poor nutrition can reduce enzyme function, slowing drug metabolism.
low protein, nothing to bind to
What is meant by competition among drugs in metabolism?
Multiple drugs metabolized by the same enzymes can compete, affecting their levels and effects.
What is the first-pass effect?
Drugs absorbed orally (PO) pass through the liver before reaching systemic circulation, where many can be metabolized and inactivated.
How can the first-pass effect affect drug response?
It can make oral drug effects negligible if a large portion is metabolized before reaching circulation.
nitroglycerine
How can the first-pass effect contribute to drug-drug interactions, tolerance, or toxicity?
Some drugs can stimulate liver enzymes, altering the metabolism of themselves or other drugs.
ALL PO DRUGS TO THROUGH FIRST PASS
ALL PO DRUGS TO THROUGH FIRST PASS
if giving sublingual, it does not go though first pass
What is hepatic biotransformation?
The liver’s metabolism of drugs, which can vary based on genetics (e.g., “rapid” vs “slow” acetylators).
Which routes of administration bypass the first-pass effect?
Intramuscular (IM), intravenous (IV), buccal, sublingual (SL), and inhaled (MDI) routes.
What is drug excretion?
The removal of drugs and their metabolites from the body.
Through which routes can drugs and metabolites exit the body?
Urine, sweat, saliva, breast milk, or expired air (for MDI)
What is the primary route of drug excretion?
Renal (through the kidneys and urine).