Chapter 7 : The Muscular System
1/178
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
179 Terms
Muscles
All muscles contract, or shorten; this causes the body, or substances in the body, to move.
3 types of muscles
skeletal, smooth, cardiac
-muscles cells are elongated and thin, so they're called muscle fibers.
Types of muscles
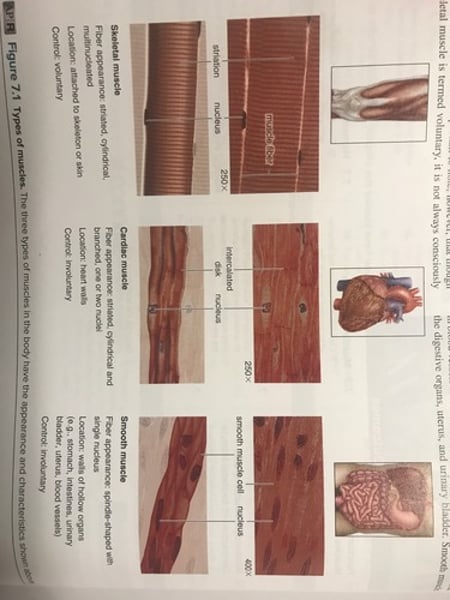
Skeletal muscles
-skeletal muscle fibers are cylindrical, multinucleated, and striated.
-attached to skeleton or skin. (Facial muscles)
-contraction is voluntary and controlled by the nervous system.
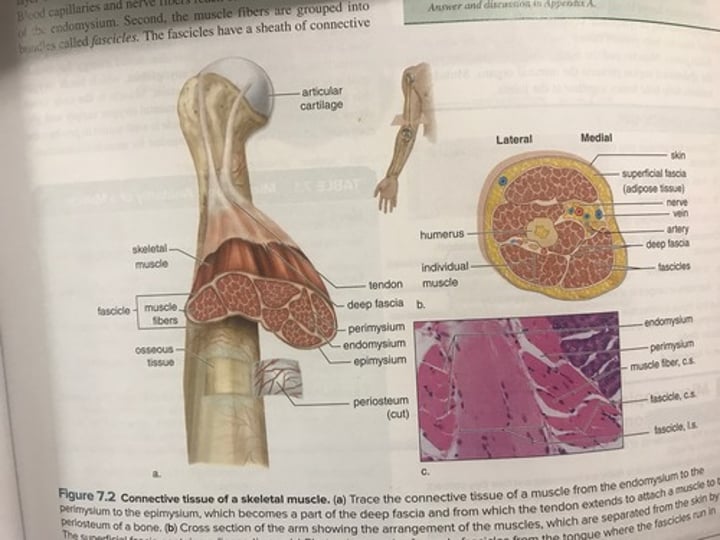
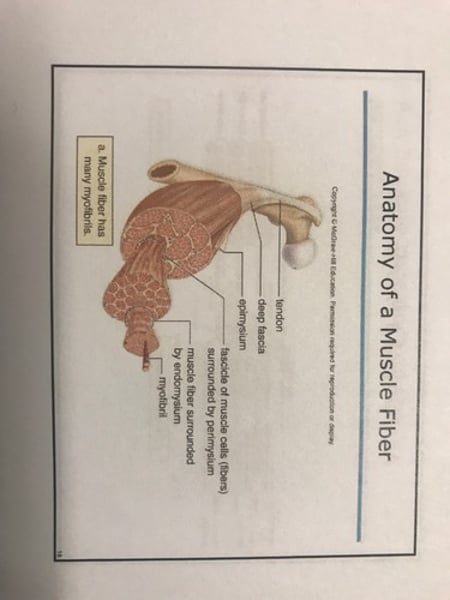
Connective tissue coverings of skeletal muscle
epimysium, perimysium, endomysium
Endomysium
-thin layer of areolar connective tissue.
-surrounds each skeletal muscle fiber.
Perimysium
surrounds bundles of muscle fibers (fascicles)
Epimysium
-layer that surrounds entire muscle.
-becomes part of the fascia (separated muscles from each other)
-collagen fibers extend from epimysium to form tendons that attach muscles to the periosteum of bone.
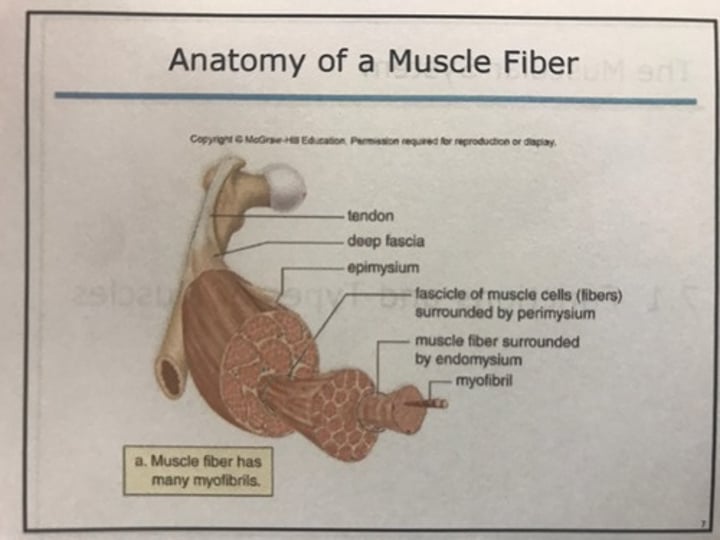
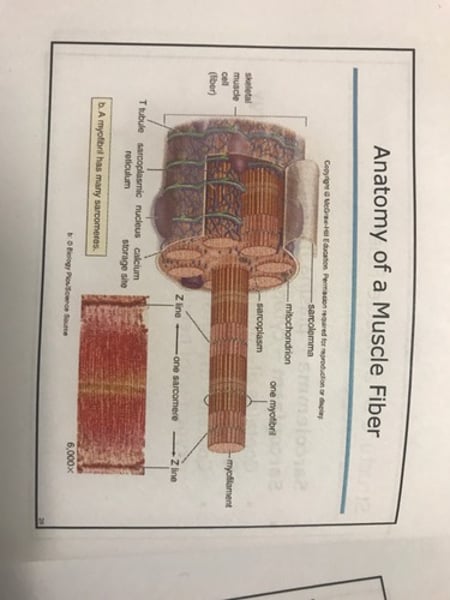
Anatomy of muscle fiber
Connective tissue of skeletal muscle
Functions of skeletal muscles
-support body to allow us to be upright.
-make bones and other body parts move.
-help maintain constant body temperature by generating heat. (Contraction generated heat - ATP)
-assists fluid movement in cardiovascular and lymphatic vessels.
-help protect bones & internal organs & stabilize joints.
Cardiac muscle
-forms heart wall
-fibers are uninucleated, striated & branched.
-fibers interlock at intercalated disks, which contain gap junctions to permit contractions to spread quickly throughout the heart.
-contraction is involuntary; does not require outside nervous stimulation.
-nerves do increase & decrease heart rate and strength of contraction depending on needs of body!
Smooth muscle
-located in walls of hollow organs.
-involuntary contraction.
-moves materials through organs and regulates blood flow.
-cylindrical cells with pointed ends (spindle shaped)
-each cells is uninucleated.
-no striations
-not easily fatigued.
Structure of muscle fiber
-sarcolemma : plasma membrane
-sarcoplasm: cytoplasm
-contains glycogen that provides energy for muscle contraction.
-contsins myoglobin, which binds oxygen until needed.
Muscle fiber
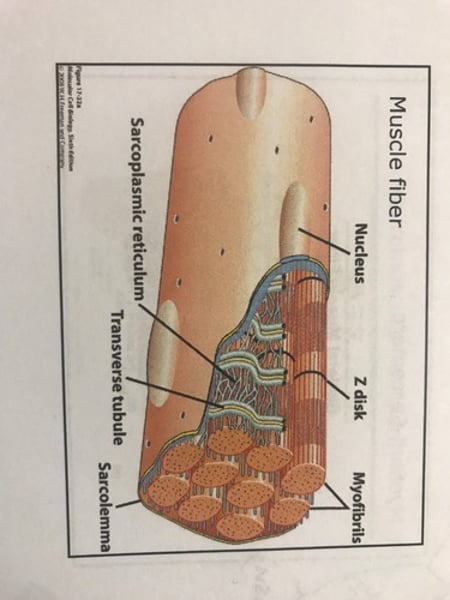
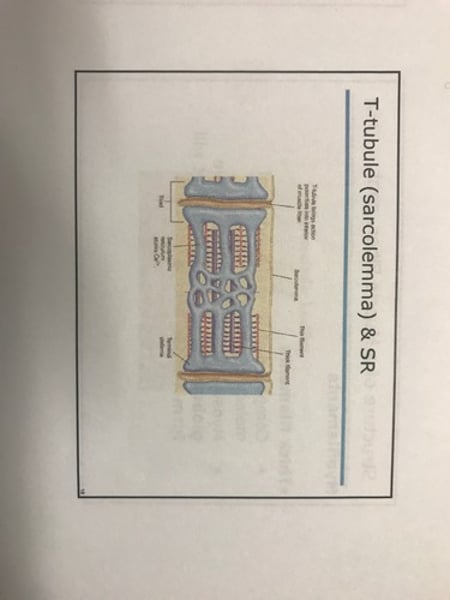
Sarcoplasmic reticulum (SR)
Smooth endoplasmic reticulum; stores calcium!
T (transverse) tubules
-Formed by the sarcolemma penetrating into the cell.
-Come into contact with expanded portions of the sarcoplasmic reticulum
T-Tubule (sarcolemma) & SR
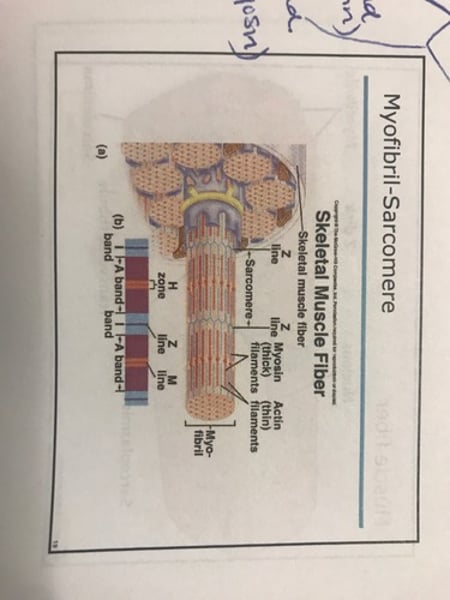
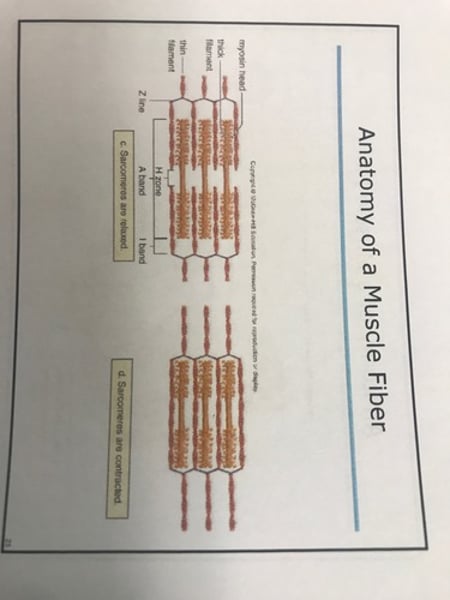
Myofibrils and Sarcomeres
-Myofibrils: cylindrical & run the length of the muscle fiber.
-myofibrils are composed of many sarcomeres:
-extend through 2 vertical z lines.
-contain 2 types of protein myofilaments (thick & thin filaments)
-I Band (light): contains only thin filaments.
-A Band (dark): in Center of sarcomere (contains thick & thin filaments)
-H Zone: in the center of the A band (has only thick filaments).
Anatomy of muscle fiber
Myofibril-Sarcomere
Anatomy of muscle fiber
Myofilaments
-Thick filaments:
-composed of several hundred molecules of myosin.
-myosin molecules end in a double globular head (a golf club) that will form a cross-bridge.
-Thin filaments:
-2 intertwining strands of actin.
-double strands of tropomyosin coil over each actin strand.
-Troponin occurs at intervals on the tropomyosin strand.
Anatomy of muscle fiber
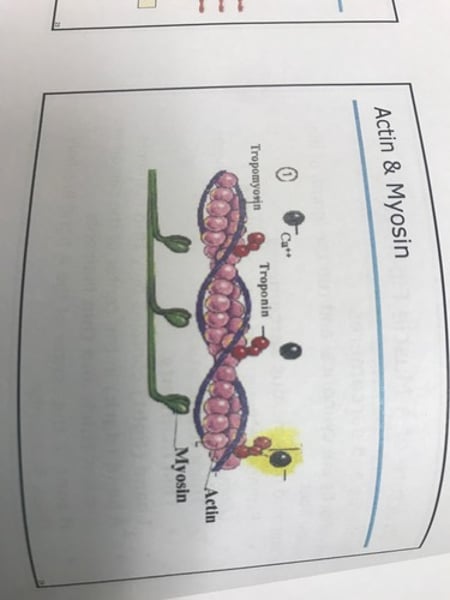
Actin & Myosin
Skeletal muscle contraction: the sliding filament theory
-skeletal muscle can only contract when stimulated by a type of neuron called a motor neuron.
-Motor Unit: one motor neuron and all of the muscle fibers it stimulates.
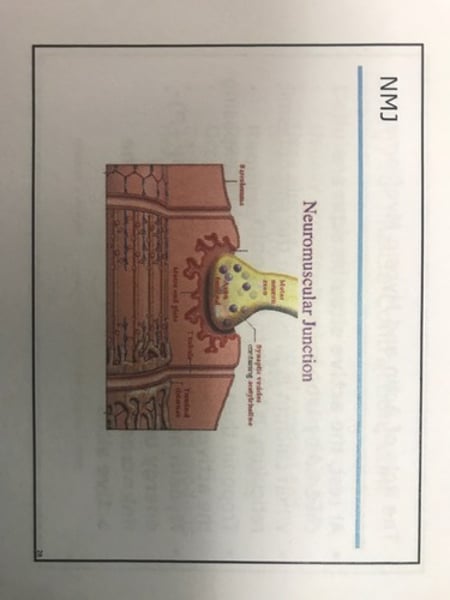
-Neuromuscular Junction (NMJ): the axon terminal of the motor neuron & the sarcolemma that the motor neuron stimulates; gap between the 2 cells is synaptic cleft.
-Acetylcholine (ACh): neurotransmitter used at neuromuscular junction; it is contained in synaptic vesicles in the axon terminal.
Neuromuscular Junction
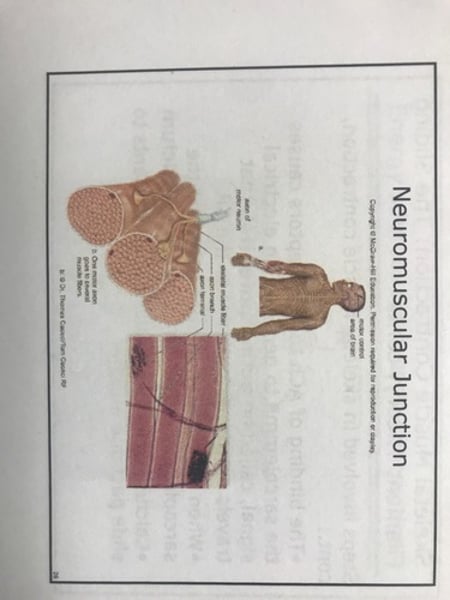
NMJ
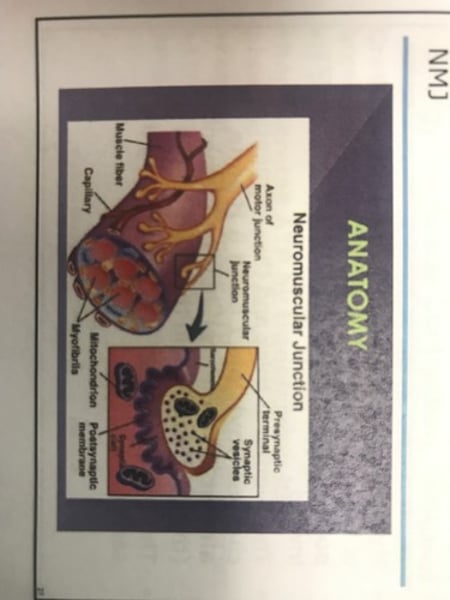
NMJ
Skeletal muscle contraction: sliding filament theory cont'd
Steps involved in skeletal muscle contraction
-nerve signal travels from the brain down the motor neuron, and arrives at the axon terminal.
-the synaptic vesicles release ACh; it diffuses across synaptic cleft.
-ACh bunds to receptors on sarcolemma.
Sliding filament theory cont'd
Steps in skeletal muscle contraction cont'd:
-binding of ACh to its receptors causes the sarcolemma to generate an electrical signal, called an action potential, that travels down the T tubules to the SR.
-when the action potential arrives at the sarcoplasmic reticulum, it releases calcium.
-Calcium from the SR allows The filaments to slide past one another.
Botulism toxin
-a protein produced by the bacterium Clostridium botulinum.
-works at the neuromuscular junction.
-paralyzed muscle by blocking the release of ACh from the motor neuron.
-no ACh means no muscle contraction; the paralysis of breathing muscles causes suffocation in victims.
-Botox is a diluted version; used therapeutically to treat migraines & cosmetically to reduce wrinkles.
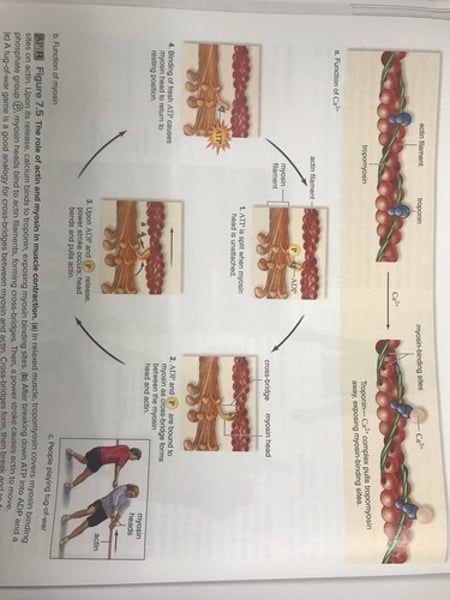
Role of actin & myosin filaments
-at rest, the active sites on actin are covered in tropomyosin.
-when calcium is present in the sarcoplasmic reticulum, it binds to troponin.
-troponin then moved tropomyosin, exposing the active sites on actin.
-Myosin heads break down ATP (ADP+P)- energy used to form a temporary link = cross-bridge with actin at active sites.
Role of actin & myosin filaments cont'd.
-Myosin heads then bend toward the C.E. yet of the sarcomere in an action called power stroke; they pull the actin filaments inward.
-the overlap of thick and thin filaments changes (invisible I band & H zone almost disappears) but the filaments (thick & thin) remain the same length.
-this cycles over and over, shortening the sarcomere.
Role of actin and myosin in muscle contraction
Role of actin & myosin filaments cont'd.
Relaxation of muscle:
-muscle contraction continues until nerve signal stops.
-when the nerve signal stops, the sarcoplasmic reticulum uses ATP to pump the calcium back into it.
-with no calcium bound to troponin, tropomyosin moves back into resting position, covering up the active sites on actin.
-Myosin heads detach from actin (ATP) and the sarcomere lengthens (muscle relaxes)
- rigor mortis - no ATP to relax muscles.
Energy for muscle contraction
-ATP stored in the muscle fiber only lasts a few seconds.
-muscles make new ATP in 3 ways:
1. Creatine phosphate breakdown.
2. Cellular respiration.
3. Fermentation.
Energy sources for muscle contraction
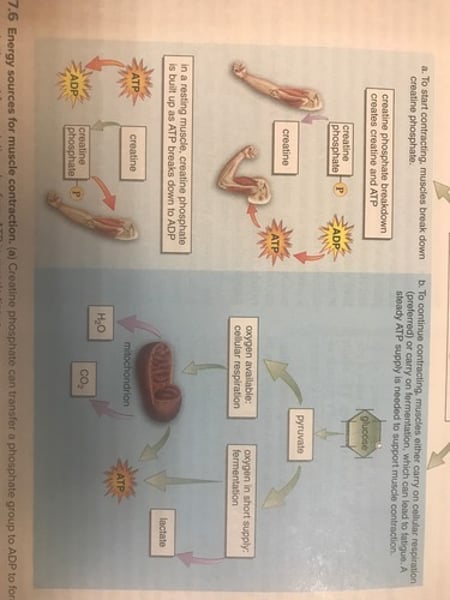
Creatine phosphate
(Stores energy-P)
Breakdown:
-anaerobic; does not require oxygen.
-regenerates ATP by transferring it's phosphate to ADP (recycle)
-fastest way to make ATP available to muscles.
-ATP produced this way only lasts about 8 seconds.
cellular respiration
-usually provides most of a muscles ATP.
-uses glucose from stored glycogen and fatty acids from stored fats.
-requires oxygen; myoglobin stored oxygen (red pigment)
-occurs in mitochondria.
-carbon dioxide and water are end products.
-Heat is a by-product.
Fermentation
-anaerobic process.
-occurs in sarcoplasm.
-produces ATP for short bursts of exercise.
-Glucose is broken down into pyruvate (pyruvic acid) and then to lactate (lactic acid).
Oxygen debt
Oxygen debt occurs when muscles use fermentation to supply ATP (not enough oxygen available to break down pyruvate).
-causes heavy breathing after exercise to replenish oxygen.
-requires replenishing creatine phosphate supplies and disposing of lactic acid.
-training causes the number of mitochondria to increase and a greater reliance on cellular respiration, so there is less oxygen debt.
Fatigue
Fatigue- when the muscle relaxes even though stimulation continues.
Reasons for fatigue
-ATP depleted.
-Accumulation of lactic acid in the sarcoplasm inhibits muscle function.
-ACh may become depleted.
-brain may signal a person to stop exercising.
Athletics & muscle contraction
-Size of muscles:
-atrophy: decrease in muscle size.
-hypertrophy: increase in muscle size.
-Slow twitch fibers (Type I fibers):
-tend to be aerobic.
-have more endurance.
-have many mitochondria.
-dark in color (red) because they contain myoglobin.
-highly resistant to fatigue.
-good for endurance activities (long running).
Athletics & muscle contraction cont'd.
Intermediate twitch fibers (Type IIa fibers):
-same features as slow twitch, but much faster.
-better blood supply.
-moderate strength for short periods of time (walking, jogging, or biking).
-called fast aerobic fibers.
-used in moderate activity.
Athletics & muscle contraction cont'd.
Fast twitch fibers (Type IIb fibers):
-tend to be anaerobic.
-designed for strength.
-light in color (white)
-have fewer mitochondria, little or no myoglobin, and fewer blood vessels.
-vulnerable to accumulation of lactic acid and can fatigue easily.
-good for short, explosions of energy (sprinting, weight lifting, pitching baseball).
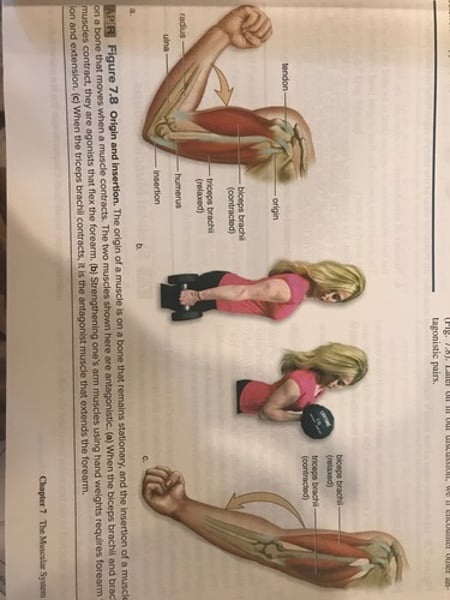
Origin
Attachment of a muscle to the bone that does not move(during movement of that particular muscle).
Insertion
attachment of a muscle on a bone that moves.
Prime mover
muscle that does most of the work in a movement (flex- brachialis)
Synergist
Muscle that assists a prime mover (biceps brachii)
Antagonist
Muscle that works against the muscle in question (triceps brachii)
origin and insertion
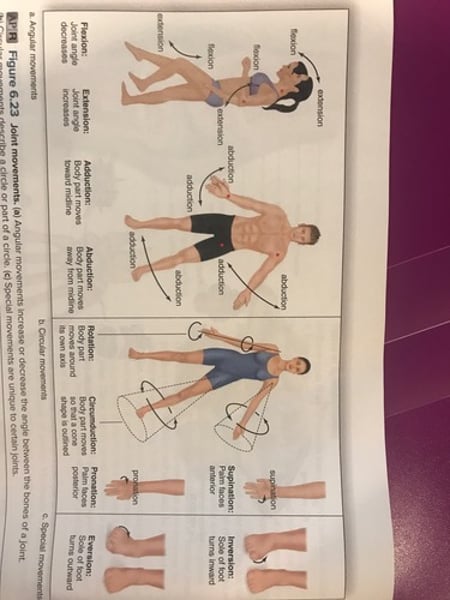
Joint movements
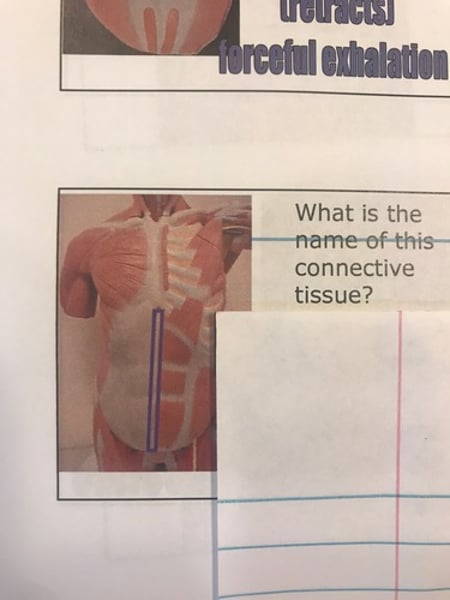
Fibrous connective tissue
Dense connective tissue - has thick bundles of collagen fibers.
-Dense regular connective tissue : has parallel fiber bundles found in
-Tendons: muscle to bone
-ligament : bone to bone
-aponeuroses : muscle to muscle.
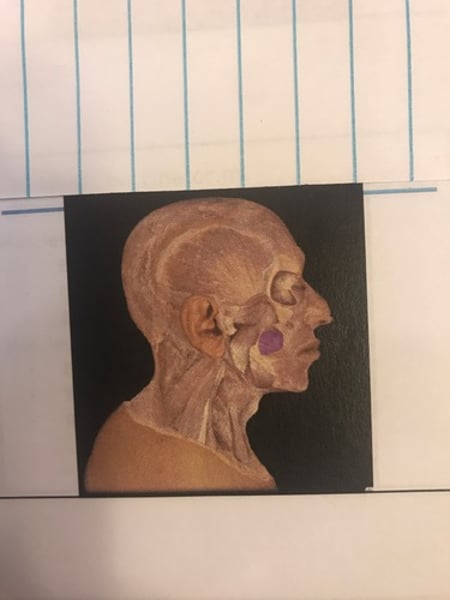
Temporomandibular joint
Joint of jaw (where mandible joins temporal bone).
Glenohumeral joint
Shoulder joint. (Where humerus fits into glenoid cavity of scapula)
Pubic symphysis
Fibrocartilage disk between left and right coxal bones. (Where they connect)
Sacroiliac joint
Where coxal bone joins the sacrum.
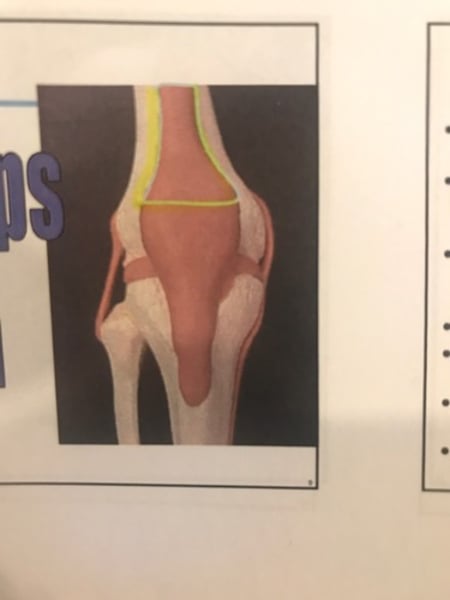
Tibiofemoral joint
Where tibia meets femur. (Knee joint)
Quadriceps tendon
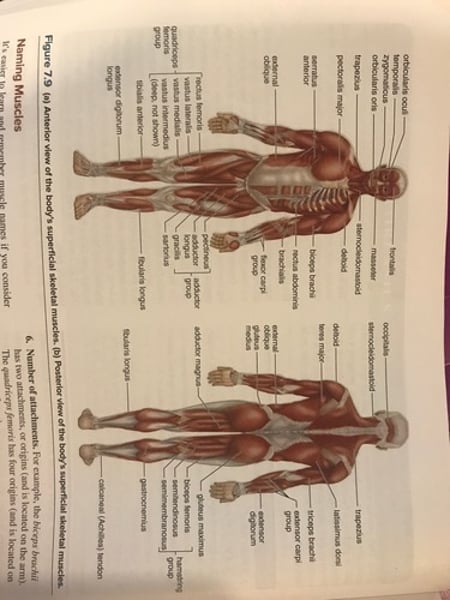
Naming muscles
-Size: Maximus, Medius, minimus, Longus (long), brevis (short), vastus (huge).
-Shape: deltoid (delta = triangle), trapezius (trapezoid), latissimus (wide), Teres (round).
-Directions of fibers : rectus (straight), orbicularis (circular), transverse (across), oblique (diagonal).
-Location: frontalis, Femoris, brachii.
-Attachment: origin & insertion (brachioradialis).
-Number of attachments: biceps, triceps, quadriceps.
-Action: flexor, extensor, adductor, levator (to lift)
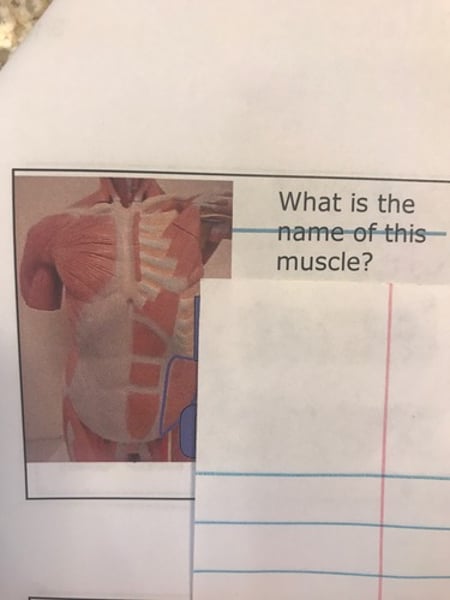
Superficial skeletal muscles
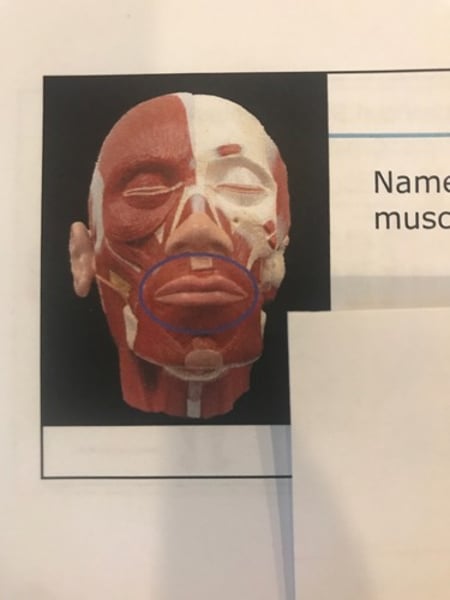
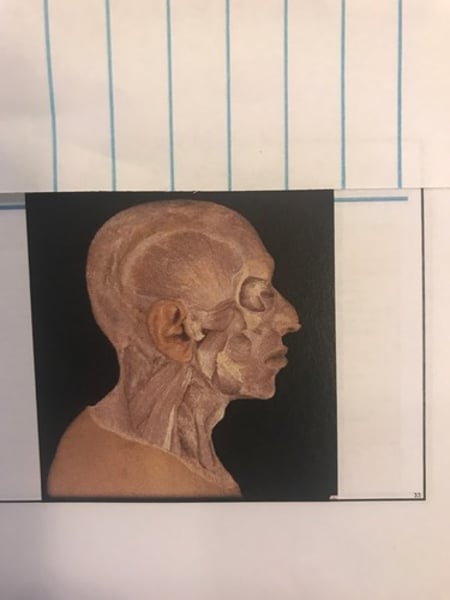
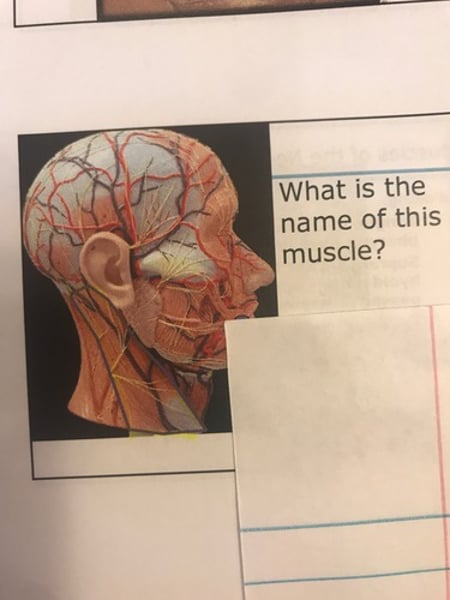
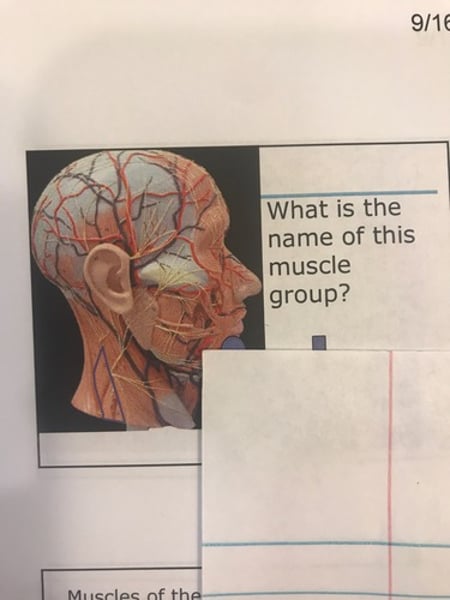
Muscles of the Head
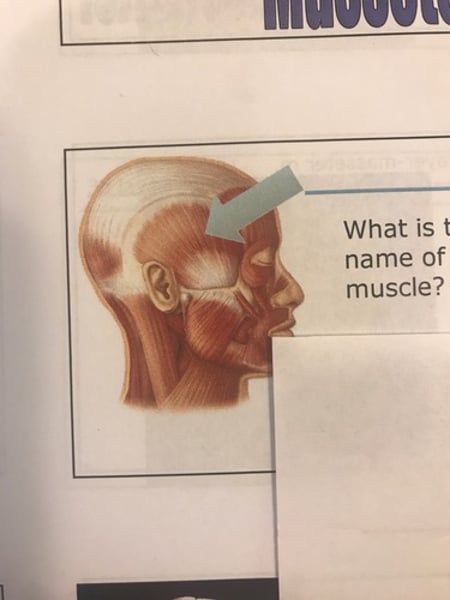
-Frontalis
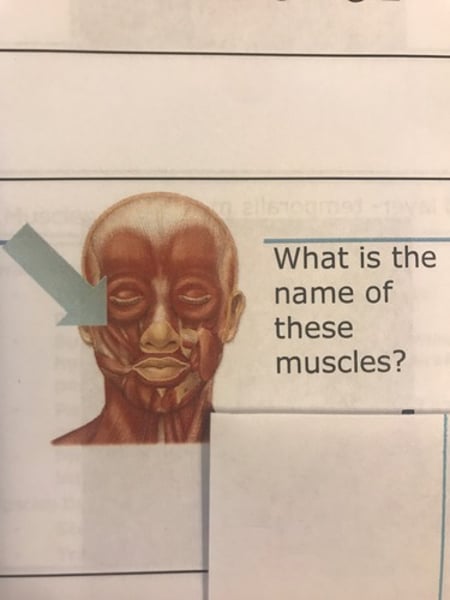
-Orbicularis Oculi (closes eye)
-orbicularis Oris (closes mouth)
-buccinatir
-Zygomaticus (cheekbone): smile
-levator Anguli oris.
-levator labii superioris.
-depressor anguli oris.
-depressor labii inferioris.
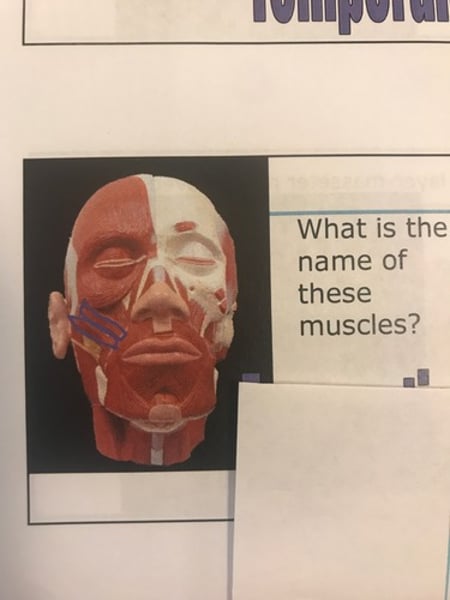
-masseter (elevates mandible) - chewing
-Temporalis (elevates mandible)
Muscles of mastication (synergistic)
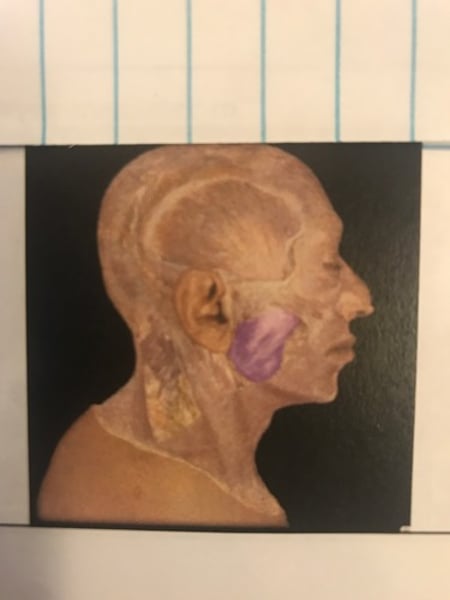
-masseter (elevates mandible) - chewing
-Temporalis (elevates mandible)
Muscles of head & neck
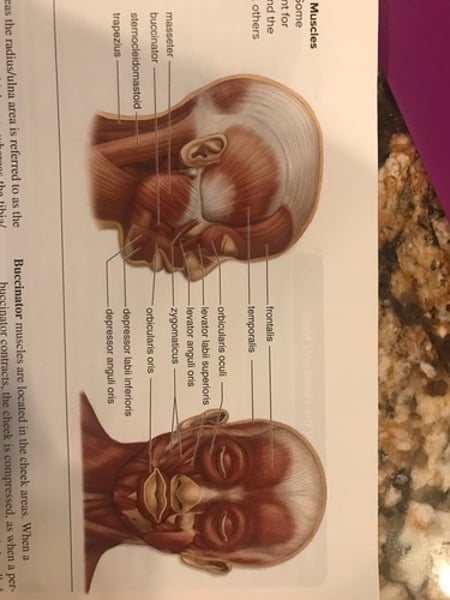
Frontalis
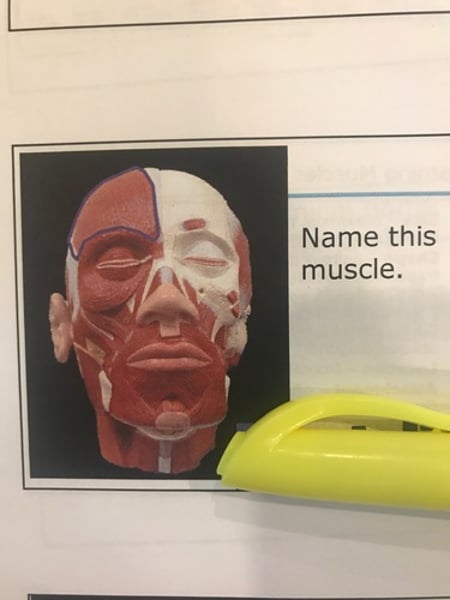
Orbicularis Oculi
closes eye
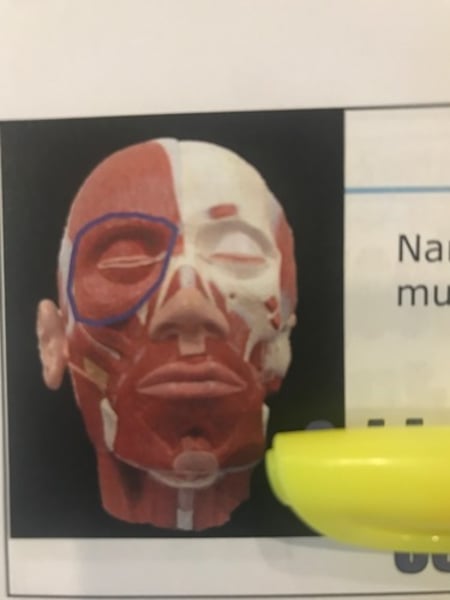
Orbicularis Oris
Closes mouth
Masseter
elevates mandible
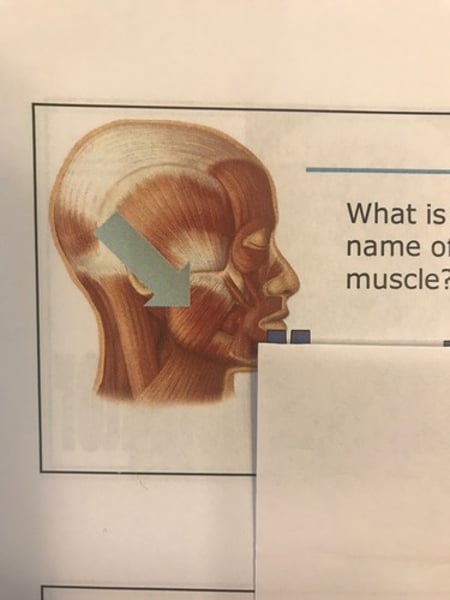
Temporalis
Zygomaticus
Zygomaticus
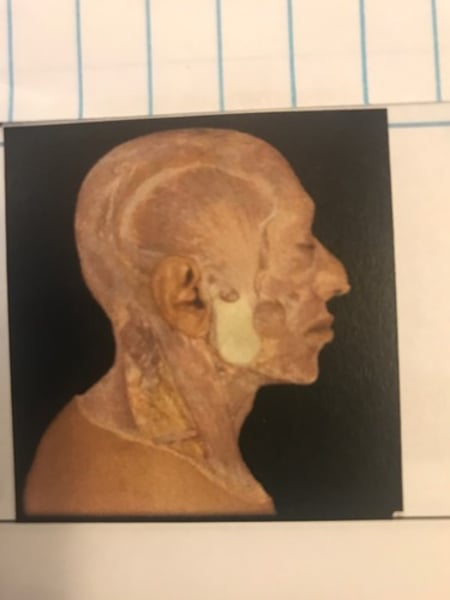
Buccinator
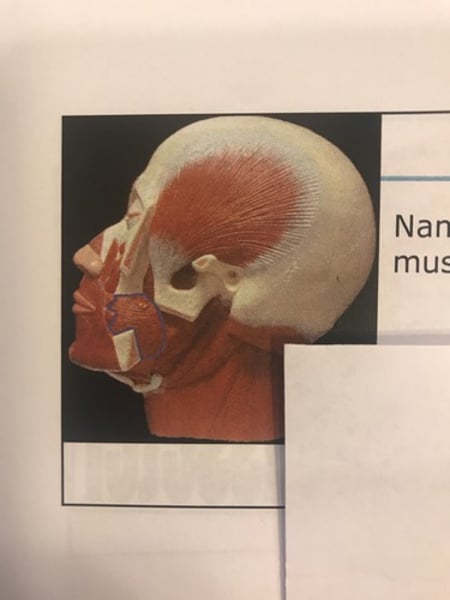
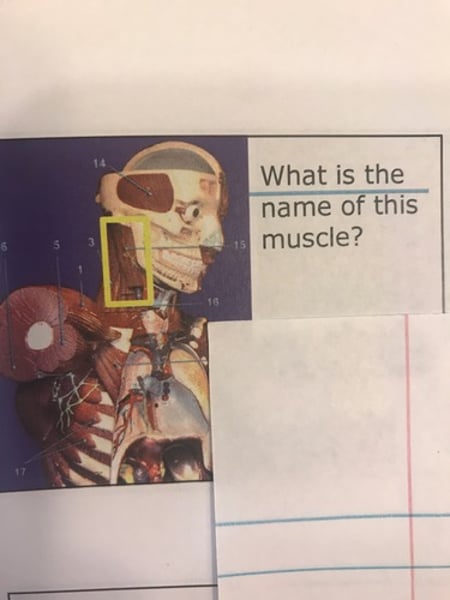
1st layer (Masseter)
1st layer (Zygomaticus)
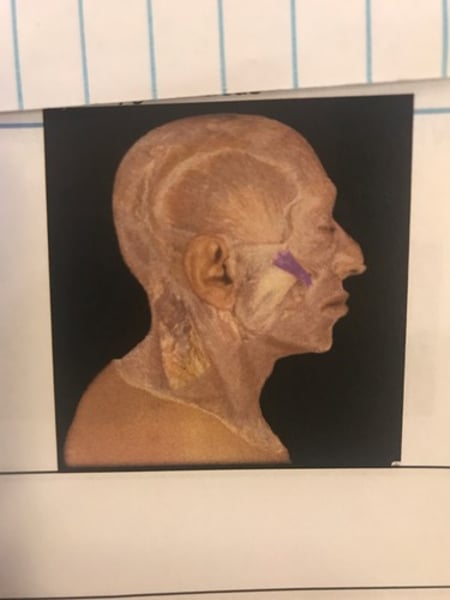
2nd layer (Masseter removed)
2nd layer (Temporalis)
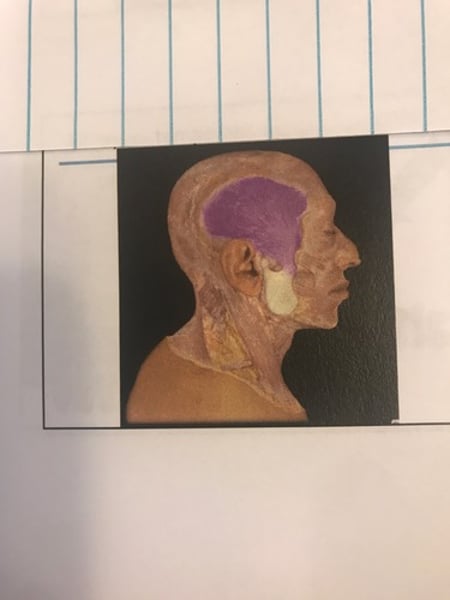
2nd layer (Zygomaticus)
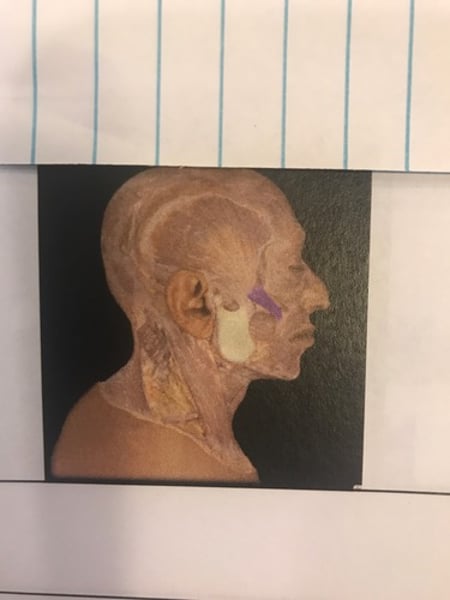
2nd layer (buccinators)
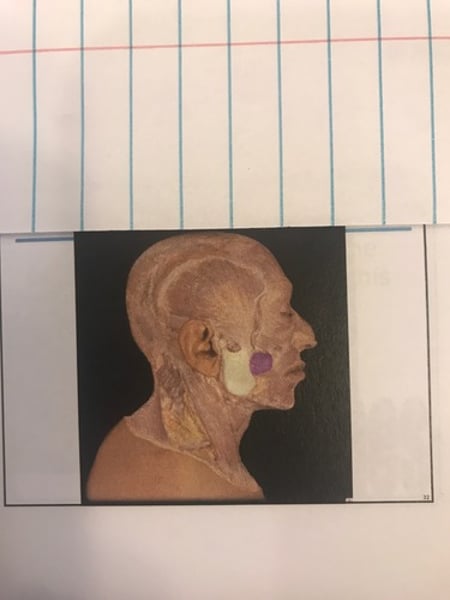
3rd layer (Mandible removed)
3rd layer (Buccinator)
Muscles of the neck
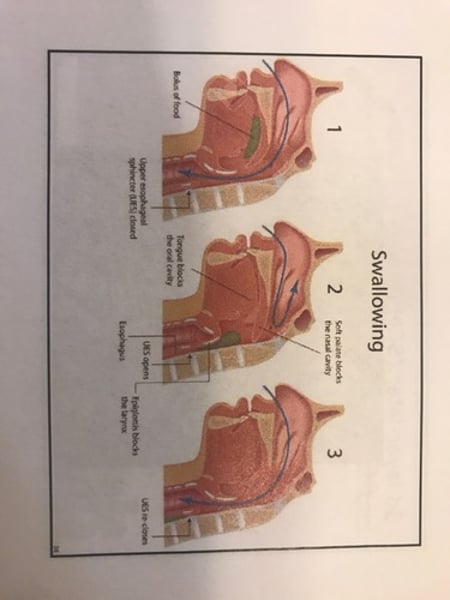
Swallowing:
-tongue & buccinators (move food to pharynx-back of throat)
-suprahyoid & infrahyoid muscles (move hyoid bone) - epiglottis close off respiratory passages -larynx.
-palatini muscles = soft palate close off nasal passages.
-pharyngeal constrictor muscles (push food into pharynx).
Muscles that move the head:
-sternoclenoidmastoid (flex & rotate)
-trapezius (extend)
Swallowing
1st layer (neck anter. - platysma intact)
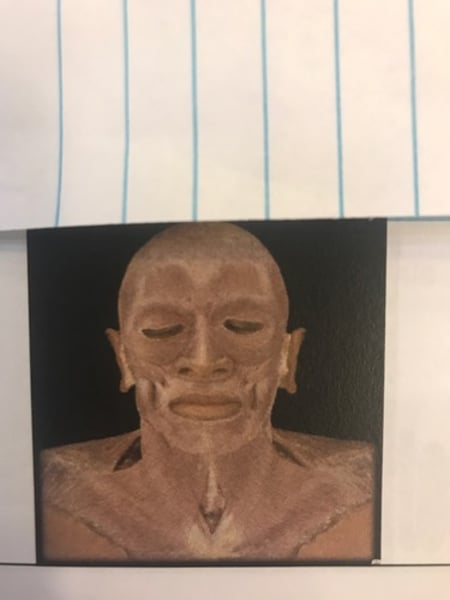
2nd layer- neck anter. (Platysma removed)
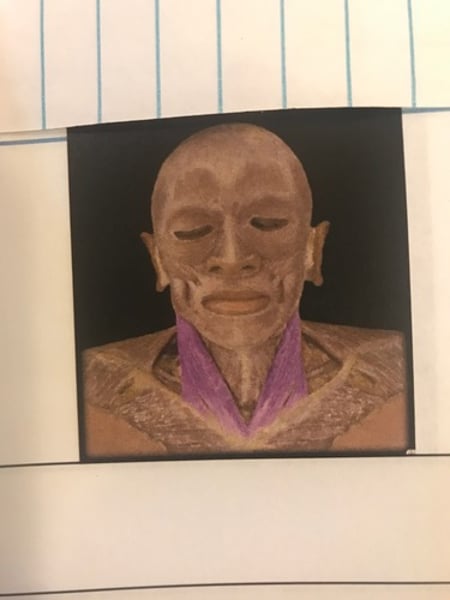
2nd layer - later (platysma removed)
3rd layer - anter (SCM removed) -scalenes muscle
3rd layer - later. (SCM removed) -scalene muscle.
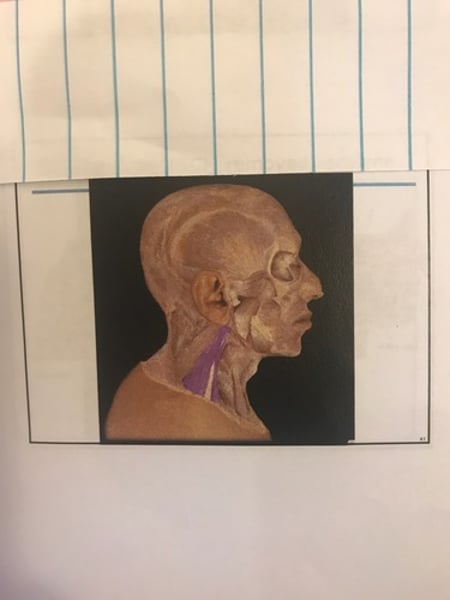
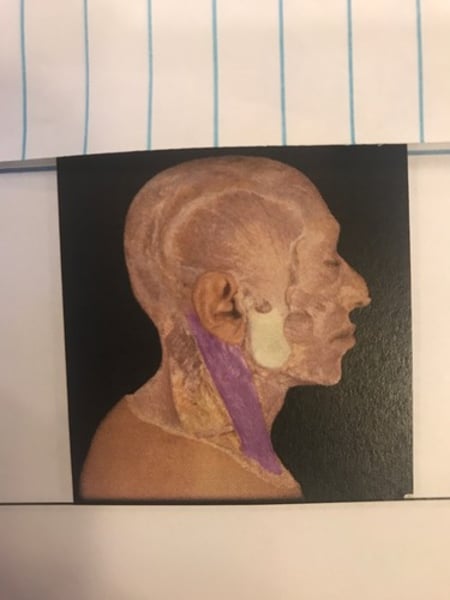
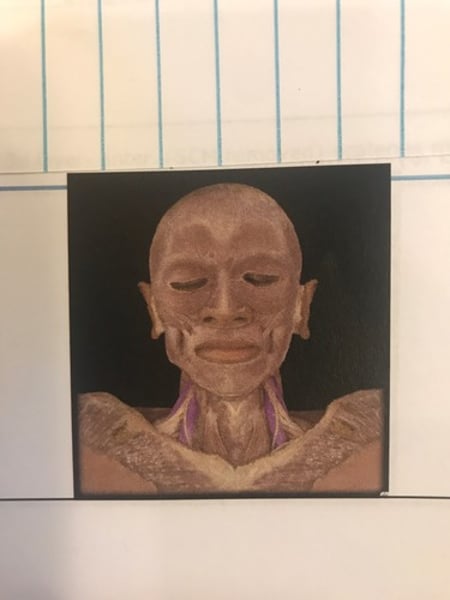
Sternocleidomastoid Muscle (SCM)
Sternocleidomastoid muscle (SCM)
Scalenes
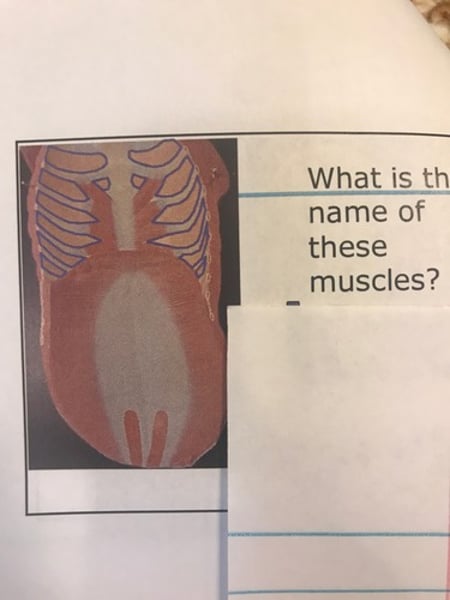
Muscles of the trunk
Thoracic wall:
-external intercostal muscles.
-diaphragm
-internal intercostal muscles.
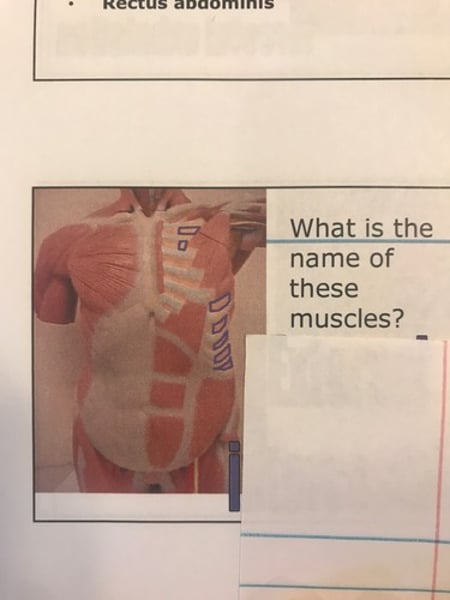
Abdominal wall:
-external & internal obliques.
-transverse abdominis.
-rectus abdominis.
Muscles of anterior shoulder & trunk.
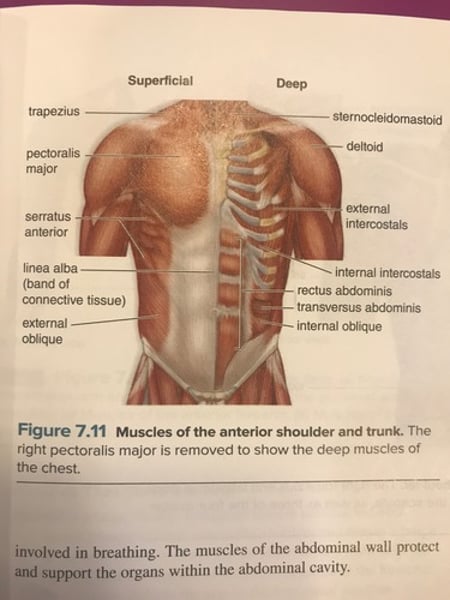
External intercostals
elevates rib cage
Internal intercostals
Depresses ribs, (retracts), forceful exhalation.
Muscles of the abdominal wall
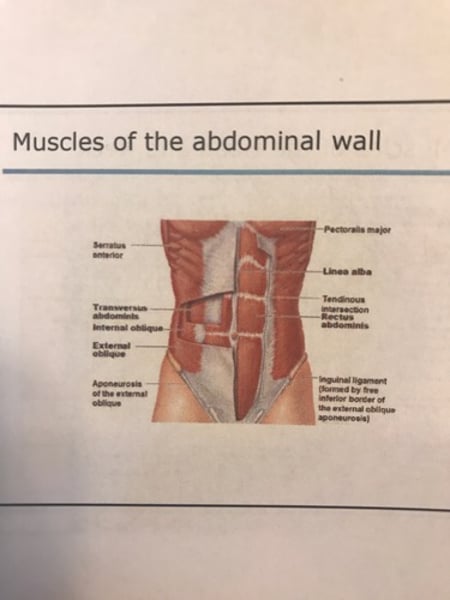
Linea alba
External obliques
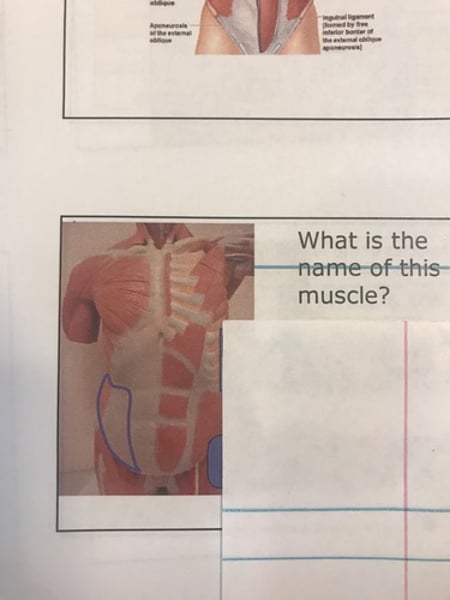
Internal obliques