Environmental emergencies JCCC EMT (EMS 132)
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
63 Terms
what part ofthe brain controls temp? What are the tow types of sensors?
hypothalamus
–Central sensors
•On or near anterior hypothalamus
–Peripheral sensors
•In skin & mucous membranes
body response to cold vs heat
cold- increased metabolic rate/ shivering, vasoconstriction
heat-vasodilation, sweat, increased respiration, increased blood flow to skin
the different types of heat transfer (5 types)
convection- transfered through air or liquid
radiation- heat lost to atmosphere and other objects without touching them
respiration- heat lost through breathing
evaporation- sweat evaporates causing heat loss
conduction- transfer of heat from physical contact
a few examples of risk factors for hypothermia
drugs/poisons
extremes of age
medical conditions
measurement of severity of hypothermia
Mild: 32.1°–35°C/89.8°–95°F
Moderate: 28.1°–32°C/82.5°–89.7°F
Severe: 24°–28°C/75.2°–82.4°F
Profound: less than 24°C (75.2°F)
about every 4-5 degrees it gets worse
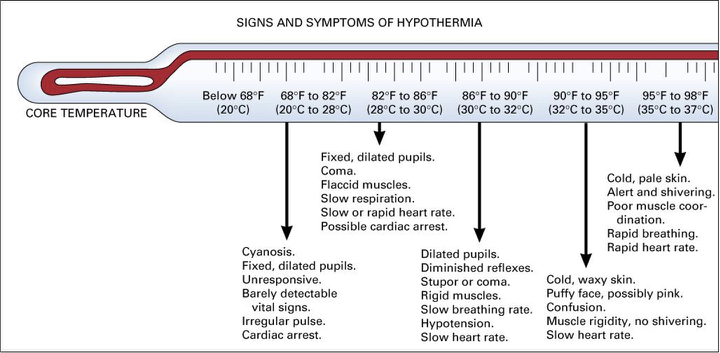
look at signs and symptoms
thermoregulation ability is lost when temperature drops below 95. Shivering usually stops around 90
s/s of hypothermia/how they progress
body tries to compensate then slows down
faster hr, rr, and shivering but then that all stops
AMS develops
skin goes from red to pale and waxy
pupils get dilated
how soon can death occur with hypothermia
2 hours
hypothermia happens ____ times faster in water
25-35
what is a local cold injury/what causes it.
–Local cold injury occurs when ice crystals form between the cells of the skin.
local cold injury risk factors
trauma, tight footwear, alcohol (a vasodilator), arteriosclerosis
external hypothermia
inadequate access to shelter
internal hypothermia
no heat in home
hypothermia assessment considerations
check pulse for 30-60 seconds carefully
move pt to warm enviornment early.
Get PMH for possible risk factors
look for signs of hypothermia and trauma
look for bradycardia, bradypnea, hypotension, poor perfusion, dilated pupils
hypothermia treatment
remove from cold enviornment
remove wet clothes
humidified and warmed (to max of 104-108) o2 if needed
warm food and drink if patient is able and awake
shivering is good
get a BGL
blankets
warmers/heat packs around core (no direct contact on skin)
hand pt carefully and keep them supine if possible (cut clothes off so you dont move arms) dont let them exert themselves
cardiac monitor on and AED ready
local cold injury s/s
numbness involving the affected body part
along with a "clumsy" feeling along with areas of blanched skin — later findings
include a "woody" sensation, decreased or loss of sensation, bruising or blister
formation, or a white and waxy appearance to affected tissue
hypothermia exp ?s
Attention to any associated injury or illness
Duration of cold exposure
Ambient temperature
Treatments initiated before EMS arrival
local cold injury treatment
avoid rewarming of extremities until definitive treatment
is possible.
If rewarming is feasible and refreezing can be prevented use
circulating warm water (37°–39°C/98.6°–102°F) to affected body
part, thaw injury completely. If warm water is not available, rewarm
frostbitten parts by contact with non-affected body surfaces. Do not
rub or cause physical trauma.
After rewarming, cover injured parts with loose sterile dressing.
keep doing CPR on hypothermic pt unless
Obvious fatal injuries (such as decapitation)
1.9.1.2 The patient exhibits signs of being frozen (such as ice formation in the airway)
1.9.1.3 Chest wall rigidity such that compressions are impossible
1.9.1.4 Danger to rescuers or rescuer exhaustion
1.9.1.5 Avalanche victims buried for 35 minutes or longer with airway obstruction by ice
or snow
note:
1.9.2 Fixed and dilated pupils, apparent rigor mortis, and dependent lividity may not be a contraindication for resuscitation in the severely hypothermic patient
hypothermia airway management considerations
In the absence of advanced airways, ventilate the patient at the same rate as a
normothermic patient
If the patient has an advanced airway, ventilate at half the rate recommended
for a normothermic patient to prevent hyperventilation. If EtCO2 is available,
ventilate to maintain normal EtCO2 levels (1:12 for adult and 1:4-6 for pediatric)
heat cramps
•Painful muscle spasms following strenuous activity in hot environment.
•Usually caused by electrolyte imbalance.
•Patient fully alert & sweaty with normal to warm skin temperature.
•Move to cool environment; replenish fluids.
heat exaustion
–Mild state of shock
•Pooling of blood in vessels below skin with increased vasodilation
•In extreme cases, organs are not well perfused.
•Prolonged – profuse fluid loss from sweating
heat exaustion s/s
–Mild to moderate perspiration
–Warm or cool skin temperature
–Skin color may be normal to pale
–Weakness, exhaustion, dizziness
–Nausea and vomiting
–Muscle cramps (usually in legs, abdomen)
–Rapid, weak pulse
–Rapid, shallow breathing
–Altered mental status (extreme cases)
temp greater than 100
heat stroke
–Body’s heat-regulating mechanisms breaks down & are unable to keep the body cool
–High body temperature damages brain cells.
–Temperature rises – inability to sweat
–Patient has altered mental status & may present with hot skin that is either dry or moist.\
the brain is cooking
heat stroke s/s
–Altered mental status
–Skin hot-to-touch
–Skin slightly moist-to-dry
–Rapid, shallow breathing
–Rapid pulse
–Weakness, exhaustion, dizziness
–Nausea & vomiting
–Convulsions
temp greater than 104
•
hyperthermia exp ?s
what were you doing
fluid intake
Diuretics?
how is heat exaustion indentified in compasrison to stroke
stroke is distinguished from heat exhaustion
by altered level of consciousness, seizures, or coma
stopping sweating
hyperthermia treatment
ABCs
get out of heat
remove clothing
if A&O give small sips of cool liquid
check BGL
cardiac monitor
if AMS or core temp of greater than 104
begin active cooling by:
1.4.2.7.1 Ice bath immersion provides the most rapid cooling mechanism
1.4.2.7.2 If ice bath immersion is not available, consider the following:
Tarp-assisted cooling with oscillation
1.4.2.7.2.2 1.4.2.7.2.3 Rotating ice water-soaked towels or sheets
Continually misting the exposed skin with tepid water while fanning
the victim
1.4.2.7.2.4 Truncal ice packs may be used, but are less effective than
evaporation
1.4.2.7.2.5 DO NOT apply wet cloths or wet clothing, as they may trap heat and
prevent evaporative cooling
if shivering occurs, call ALS for meds
keep doing active cooling until…
Cooling efforts should continue until the patient's temperature is less than
102.2°F (39°C) or, if continuous temperature monitoring is not available, until
the patient demonstrates improvement in mental status
drowning s/s
•Airway-patent? Obstructed? Fluids?
•Resp distress
•Resp Failure
•Cold to touch?
•Cyanotic?
Cardiac Arrest?
important s/s and concerns drowning
•Persistent cough
•Dyspnea/apnea
•AMS or LOC
•Vomiting
•Drug/ETOH
•Pertinent past medical hx
•Hypothermia
•Duration of CA/RA
•Age of patient
•Spinal Injury?
•Water temp
•Duration of submersion
mammalian diving reflex
•Drastically slows down metabolism and may prolong possibility of resuscitation
•Larynx spasms (inhibits breathing), slowed heart rate, vasoconstriction (except to heart and brain)
•The colder the water, the more pronounced the effects
does “secondary or dry drowning” really exist? if so what do we do
not exactly
it is possible that water enters the lungs and damages the alveoli. This can cause the alveoli to leak and cause non cardiogenic pulmonary edema (just like normal pulmonary edema). This can happen 12-48 hours later so its important to watch someone even if they are not showing symptoms.
pulmonary edema= CPAP
Barotrauma
(pressure-induced trauma)
•Dysbarism
a medical condition that results from changes to ambient pressure
Boyles law
Volume/pressure inversely related
if a diver takes a lungful of air while he is underwater, that air will expand in his lungs as he rises to the surface. If he holds his breath or ascends too rapidly (like a cork) the expanding air can rupture his lungs (air embolisms).
some gases become toxic or cause mental impairment when their partial pressure in the blood rises above a particular level.
•Henry’s Law
-- dissolving of gases (nitrogen) are faster at high pressures
•Ascent can cause bubbles in blood and tissue
•Charles Law
- gas will expand when heated
•Ascension can again cause trauma to airway structures and lungs
can also make bubbles
Barotrauma -- EENT and other considerations
•The “squeeze”-- pressure in cavities is too great, and eardrums or sinuses may rupture
•May see blood from ears/nose, pain to affected areas, dizziness/disorientation, & nausea (N/V)
pneumothorax
pneumomediastinum
Arterial Gas Embolism
•Ascend to rapidly causing trauma to alveoli & surrounding blood vessels which allows air to escape into circulation
•An “air clot” (air embolism)
S/S -- rapid onset of S/S of allergic reaction, deep pain in muscles, joints, tendons, distortion of senses, frothy blood in airway, coma, CA, behavioral changes
Decompression Sickness AKA ”the bends”
•Expansion of Nitrogen within tissues and joints
•Act as air emboli (air clots) and obstruct circulation
•Compress and stretch blood vessels and nerves
•Can mimic an allergic reaction
•May occur hours after a dive (versus air emboli that happens immediately upon ascent – if you are trying to delineate which is which)
diving exp ?s
•Where?
•Depths and how long?
•Rate of ascent
•Been on a plane?
•Air supply content?
•Work or problems underwater?
•Physical condition prior?
decomp sickness s/s
mild
Respiratory distress
•Pain
•Pruritis, skin bends (bruising or mottled skin)
•Skin rash
•Pain (severe) usually localized to abdomen, joints, tendons – makes patient bend over, hence “the bends”
•severe
S/S vary wildly
•Respiratory distress
•Nervous -- low back pain that progresses to paralysis, deafness, vertigo
•The “chokes”-- dyspnea, pain on inspiration, cough
•S/S of shock
care for drowning
ABCs
hypothermia treatment if needed
identify cause if possible
C-spine precautions if suspected
in water ventilations only if delayed extrication
Start CPR with 5 rescue breathes
care for diving incident
ABCs
treat other injuries
If air embolism suspected, place in left lateral recumbent position- helps trap air from traveling into cerebral circulation
Patients with symptoms suspicious for decompression illness, should be placed
on supplemental oxygen regardless of saturations to enhance washout of inert
gasses
transport to hyperbaric facility
Acute mountain sickness s/s
Headache plus one or more of the following: anorexia, nausea
or vomiting, fatigue or weakness, dizziness or lightheadedness or difficulty sleeping. (In
infants and young children, symptoms include pallor, fussiness, vomiting, decreased
appetite, poor sleep, decreased playfulness.) These symptoms must occur in the setting
of recent arrival to high altitude (generally considered greater than 5000 – 7000 feet)
High altitude pulmonary edema (HAPE): s/s
Progressive dyspnea, cough, hypoxia, and
weakness in high altitude environments (considered greater than 8000 feet). (In infants
and young children, symptoms again include pallor, fussiness, vomiting, decreased
appetite, poor sleep, decreased playfulness.) Patients may or may not exhibit new
symptoms if acute mountain sickness precedes symptoms of HAPE
High altitude cerebral edema (HACE):
Identified by mental status changes in patients with
symptoms of acute mountain sickness including altered mentation, ataxia, or stupor and
progressing to coma. Typically seen in high altitude environments (greater than 8000 feet)
altitude sickness treatment
ABCs
descend
pulmonary edema=CPAP
Acute mountain sickness
Ibuprofen or acetaminophen for pain
brown recluse- toxin type, s/s
•Bite injects a cytotoxin
•Cytotoxin -- toxic to cells
•Breaks down cell membranes leading to necrosis of the tissue
Not very painful when bite happens
may lead to amputation of bite area
•Not deadly
•Localized swelling (initially), tenderness
•Pale, mottled, cyanotic center w/possible blister formation
•Open sore & necrosis (2 - 8 hrs)

black widow- toxin type and s/s
•Inject a neurotoxin
•Neurotoxins affect the nervous system
•Black widow toxin causes affected nerve cells to dump neurotransmitters
•Very painful, but rarely deadly in healthy adults
•Painful bite
•Localized swelling initially
•Dizziness, sweating, N/V, rashes
cramping- abdomen, back, chest, shoulders
rigid abdomen
•Chest tightness, difficulty breathing, or abdominal pain (depending on bite site)
•Occur within 24 hours of bite & subside within 48 hours (usually)
•Antivenin exists – saved for those who are most at risk for adverse outcomes
Muscle pain****
spider bite care
monitor ABCs
clean wound with mild soap and water
cover with dry sterile dressing
cardiac monitor
BGL test
•Remove any watches / rings / constricting jewelry
keep them still- splint…
draw circle around swelling
take pic of spider if possible
the venomous snakes in kansas
cotton mouth
rattle snake
copperhead
rattle snake toxin
•Hemotoxic & neurotoxic:
•Hemotoxin -- break down blood & tissue causing necrosis & hemorrhaging, can also cause clotting issues
neuro- weakness, spasm, paralysis, etc
•Toxins affect blood & nervous system both at the bite site & systemically
•Patient age & size cause different effects (same with perpetrator)
copperhead toxin
hemotoxin
cottonmouth toxin
hemotoxin
snake bite care
ABCs
clean it
cover it
take pic of snake if possible
••Note time of bite
•Remove any constricting jewelry
•Keep patient calm
•Notify receiving facility immediately to ensure antivenin capabilities
•Rapid Transport to appropriate facility
draw circle around swelling
keep them still- splint…
what should you watch for with any bite or sting
anaphylaxis
marine stings
scrape of tentacles or carefully pull out tooth or barb
hot water immersion of effected part (113°F/45°C).
types of lightning strike
direct
contact-they were touching something that got struck
splash
ground current
body systems lightning strike can effect
cardiac
resp.
skin
nervous
musko.
care for lightning strike
ABCs
cspine
care for other trauma (fractures or burns)
drowning exp ?s
length of submersion
what lead up to it
alcohol involved?
Bee sting care
Remove stinger
Cool compress/not ice
clean it