Urology
1/177
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
178 Terms
Up to 65% of filtered sodium and water is reabsorbed in:
the proximal convoluted tubule
Which of the following are used as crude indicators of GFR:
BUN
Creatinine
SDMA
All of the above
All of the above.
A 4 y/o MC DSH is presented to you with a 12 hour history of straining to urinate without producing urine. PE reveals a large, turgid bladder. Lab work shows a creatinine of 12 mg/dL. Which of the following is most likely for this patient?
Normal, non-azotemic patient
Pre-renal azotemia
Renal azotemia
Post-renal azotemia
Post-renal azotemia
Renal Blood supply starting at renal artery
Renal artery → interlobar arteries → arcuate arteries → interlobular arteries → afferent arterioles → glomerulus → efferent arterioles
What is the functional unit of the kidney?
The Nephron
Functions of the kidney
Excretion of metabolic waste products
Regulation of water and electrolyte balance
Regulation of acid-base balance
Regulation of erythrocyte production
Activation of vitamin D
Secretion, metabolism, and excretion of hormones
List the factors that contribute to GFR
Forces favoring filtration
Glomerular hydrostatic pressure PG = 60
Bowman’s capsule colloid osmotic pressure 𝝿B = 0
Forces Opposing Filtration
Bowman’s capsule hydrostatic pressure PB = 18
Glomerular capillary colloid osmotic pressure 𝝿G = 32
Net filtration pressure = 60 - 18 - 32 = +10mmHg
Describe RAAS
Decrease in arterial pressure leads to a decrease in glomerular hydrostatic pressure (↓GFR) → decreased NaCl at the macula densa. This triggers the release of rennin, which converts Angiotensinogen to Angiotensin I. ACE then converts Angiotensin I to Angiotensin II.
Effects of Angiotensin II
Increased Sympathetic Activity
Tubular Na+ Cl- reabsorption and K+ excretion. H2O retention
Aldosterone secretion from adrenal cortex (water retention)
Arteriolar vasoconstriction. Increase in blood pressure
ADH secretion from the pituitary glands = collecting duct H2O absorption
Causes of a low BUN
Decreased protein intake or protein anabolism (young animals)
Increased excretion of BUN (ex. DM, Cushing’s) = PU/PD
Decreased production (ex. Liver disease, urea cycle defect)
Causes of a high BUN
Increased protein catabolism (ex. Fever, burns, steroids, starvation, exercise)
Increased protein ingestion (ex. GI bleed, high protein diet)
Decreased GFR (ex. azotemia)
Causes of low creatinine
Decreased muscle mass, cachexia
Increased GFR
Causes of high creatinine
Normally higher in greyhounds
Decreased GFR (azotemia)
Pre-renal azotemia
Decreased blood flow to the kidneys
Causes
Hypovolemia
Cardiac Disease
Renal vasoconstriction
Clinical evidence of dehydration of hypovolemia - UA shows concentrated sample
Renal Azotemia
Results from decreased GFR when there is loss of >75% renal mass
Causes
Primary renal disease
Secondary injury (ischemia, obstruction, etc.)
Generally accompanied by loss of urine concentration ability, electrolyte changes, and signs of clinical illness
Postrenal Azotemia
Results from obstruction or rupture of the urinary outflow tracts
Causes
Urolithiasis
Bladder rupture
Marked hyperkalemia is common, may see evidence of uroabdomen.
How do we use SDMA to determine GFR?
Produced by all nucleated cells at a constant rate
Excreted primarily by the kidneys, and is not reabsorbed by the renal tubules or influenced by non-renal factors
Considered a more sensitive early marker for declining GFR in dogs and cats
Normal USG range for dog and cat
Dog: 1.015-1.045
Adequate >1.030
Cats: 1.035-1.060
Adequate >1.040
What is isosthenuria?
Kidney cannot concentrate OR dilute (1.008-1.012)
What is hyposthenuria?
Kidney can dilute but cannot concentrate (<1.008)
Understand pathophysiology mechanisms of AKI in cows/horses
Acute Kidney Injury is caused by an abrupt reduction in glomerular filtration rate - leads to azotemia, fluid/electrolyte/acid-base disturbances.
Defined as acute increase in serum creatinine of 0.3mg/dl or greater
If sustained → Acute Kidney Failure
Three Major Categories
Pre-Renal
Renal
Post-Renal
Describe vasomotor nephropathy in bovine/equine
persistent causes of pre-renal hypoperfusion
ischemic tubular injury > necrosis
Sepsis/systemic inflammation
decreased renal perfusion
release of cytokines, vasopressors altering afferent/efferent pressure balance.
Thrombotic disorders
Which drugs can cause toxic nephropathy in bovine/equine
Aminoglycosides, oxytetracycline
NSAIDs
Imidocarb
Which pigments can cause toxic nephropathy in cows/horses?
Hemoglobin
Myoglobin
Which plants can cause toxic nephropathy in cows/horses?
Sorghum, oxalate, oak
How do aminoglycosides cause toxic nephropathy?
Nephrotoxicity associate with high trough levels not high peak
Proximal tubule intracellular accumulation = cellular death
Urinalysis: proteinuria, cylindruria, enzymuria, and hematuria
Renal failure can develop even after drug withdrawal
How do NSAIDs cause toxic nephropathy?
Inhibition of PGE2 and PGI2 synthesis => inability to regulate renal blood flow
Medullary crest or papillary necrosis
Urinalysis: Hematuria (early stage)
Ultrasound: Renal medullary rim sign
How do oxytetracycline cause toxic nephropathy?
inhibition of tubular cells oxidative enzymes
hydropic degeneration
necrosis
Propylene glycol (vehicle) may decrease renal blood flow
How does salt poisoning cause ARF?
hyperfiltration - leading to increased glomerular pressure
What is the toxic part of oak, that causes ARF in heifers?
Tannic and gallic acids
How does pigweed cause ARF?
Oxalates + calcium ions = insoluble crystals > tubular blockage and necrosis
Pathophysiology of post-renal failure in cows/horses?
Retrograde increase in tubular hydrostatic pressure
Glomerular mesangial cell contraction
vasoconstriction of the afferent arteriole
Leads to: decreased glomerular blood flow, decreased GFR, tubular damage
Renal pelvis enlargement, loss of medullary tissue, hydronephrosis, atrophy.
In horses, what creatinine is defined as azotemia? Bovine?
>1.5 mg/dL horses
>0.9mg/dL bovine
What electrolyte abnormalities do we see in cows with ARF?
Significantly low Chloride
Significantly high Phosphorus
Low Sodium
High Magnesium
What is normal equine/bovine urine production?
15-30ml/kg/day
Describe glomerulonephritis in bovids. Etiology and pathophysiology.
Etiology
Antigen-antibody complexes deposition in the glomeruli
specific antibodies against glomerular basement membranes
Associated with infection: Abscesses, mastitis, liver fluke infestation, metritis, BVD
Leads to → increased permeability of the glomerular barrier, severe proteinuria, progressive renal failure, hypoalbuminemia, weight loss, ventral edema.
How do you diagnose glomerulonephritis?
Renal biopsy - hypercellularity of the glomerular tufts (proliferative GN) or thickening of the glomerular barrier (membranous GN)
What is Nephrotic Calf Syndrome?
A type of glomerulonephritis associated with hyperimmune serum administration
bottle jaw and generalized edema, tricavitary effusion
Anemia, Azotemia, Hypoalbuminemia
Enlarged kidney
Urinalysis: proteinuria, isosthenuria, granular or hyaline casts, RBCs, WBCs
What is pyelonephritis in the bovid?
Ascending infection from lower urinary tract
E.coli or Corynebacterium renale
Acute/Subacute or chronic
Describe the difference between acute/subacute and chronic pyelonephritis in the bovid.
Acute/subacute
Fever > 103.5
Anorexia
Sudden drop in milk production
Colic
Urinary Obstruction (blood clots)
Stranguria, polyuria, arched stance
Hematuria
Chronic
Weight loss
Poor hair coat
Anorexia
Poor milk production
Diarrhea
Polyuria
Anemia
Stranguria
What is the pathophysiology of amyloidosis in the bovid?
Extracellular deposition of amyloid in kidney, intestine, liver, adrenal gland, spleen
Pathophysiology -
primary = immune-mediated or metabolic storage disease
secondary = associated with chronic infections (most commonly systemic AA type amyloid)
What are the clinical findings of amyloidosis in the bovid?
diarrhea, edema, weight loss, enlarged kidneys, hypercoagulation (urinary losses of antithrombin III), nephrotic syndrome
Diagnosis and prognosis of amyloidosis?
Dx: renal biopsy
Prognosis: fatal, no treatments exist
What is enzootic hematuria?
Pathophysiology - progressive noninfectious cystitis with tissue metaplasia of the bladder mucosa
chronic exposure to non-toxic levels of bracken fern toxins ± bovine papilloma viruses (BPV2)
Clinical signs - severe hematuria, stranguria, and anemia, urethral obstruction from blood clots bladder wall thickening, bladder neoplasm.
Dx: presumptive based on multiple animals affected in same pasture, r/o infectious
Treatment/prognosis - remove bracken fern. Hematuria will resolve if exposure is discontinued before development of bladder tumor
Know pathophysiologic mechanisms of chronic renal failure in horses
Progressive loss of renal function
Loss of urinary concentrating ability
Retention of nitrogenous and other metabolic end products
Alterations in electrolyte and acid-base status
Dysfunction of several hormone systems
Uremia - multiple organ dysfunction
Common causes of acute renal failure in horses
Infectious causes
Pyelonephritis
Secondary to lower UTI
Stranguria, dysuria, dermatitis
Culture, colony count, sensitivity
Gram negative bacteria, streptococcus spp.
Leptospira interrogans
Serovar Pomona
Vasculitis and endotheliitis >>> interstitial nephritis
Sporadic in adult horses
Outbreak of fever and ARF in young horses
Clinical signs
Fever (anorexia, depression, hematuria)
Urine analysis - pyuria w/o bacteriuria
Enlarged kidneys on U/S
Diagnosis
PCR on urine - second voided sample after furosemide
Treatment
Antibiotics
Beta lactams
Fluoroquinolones
Fluid therapy
Prevention
Vaccination - killed, whole cell bacterin
Prognosis = good
ARF - acute glomerulopathies
Purpura hemorrhagica horses
Streptococcus equi equi
May cause hematuria and proteinuria but very rarely ARF
Actinobacillus equuli foals - bacteremia to kidneys
Common causes of chronic renal failure in horses
Developmental = renal agenesis, renal hypoplasia, renal dysplasia, and polycystic kidney disease
Primary glomerular disease = weight loss and pitting edema
Primary tubulo-interstitial disease = weight loss w/o edema
causes
Chronic/irreversible nephrotoxic or vasomotor causes
Chronic pyelonephritis - most common in mares
chronic/intermittent obstruction
Renal dysplasia
Mechanisms of incontinence in horses
Cystitis and chronic urethritis
Irritation of stretch receptors in the bladder wall
Stimulation of stretch receptors in parasympathetic afferents
Stimulation of detrusor contractions
Pollakuria
Ectopic ureter - more common in fillies
Urethral injury
Post obstruction
Post foaling mares
Cystolithiasis
Bladder paralysis
“Lower Motor Neuron” bladder = loss of anal sphincter tone, tail paralysis, perineal hypoalgesia, hindlimb weakness
Polyneuritis (cauda equina neuritis)
Lumbo-sacral trauma
EHV-1 myeloencephalitis
Atonic and distended bladder with relaxed urethral muscles, continuous incontinence (vs UMN dysfunction - intermittent)
Chronic distension of the bladder -> accumulation of calcium carbonate crystals -> Sabulous urolithiasis/cystitis
Stretching of the detrusor muscle, inability to contract
Loss of sphincter function
Incontinence
Causes of hematuria in horses
Urolithiasis
UTI
Polypoid cystitis
Urethritis
Neoplasia
Idiopathic renal hematuria
Idiopathic hemorrhagic cystitis
NSAIDs - induced ulcerative cystitis
Urethral rents
How do you differentiate psychogenic PU/PD from diabetes insidious in horses?
Measure serum electrolytes esp. Sodium - DI cases may have hypernatremia
Check ACTH and signs of Cushing’s disease
Any recent environmental, social changes
Water deprivation test - 24 hours or until 5% dehydration or modified water deprivation test (over 5-7 days)
ADH (40-80 IU/ 500kg) administration (to diagnose central DI)
List common urinary disorders in foals.
Spurious hypercreatininemia
Elevated creatinine at birth associated with placental dysfunction and neonatal encephalopathy but usually no renal injury
Azotemia -
Creatinine 3.2-8mg/dl
BUN increased, but not as much as creatinine
Decline 50% in 24 hours, normal 2-3 days with or without fluids
Electrolytes usually normal
AKI/ARF
Hydroureter syndrome
Incomplete obstruction of urine flow causing ARF
Signs
Hydroureters, hydronephrosis, severe hyponatremia, encephalopathy
Etiology unknown but may be related to dysfunction of the ureterovesical valves
Treatment frustrating.
Congenital defects (renal agenesis/dysplasia, polycystic kidney, ectopic ureters)
What are the most common causes of acute renal failure in horses, and what is the management?
Most common causes:
Hemodynamic or nephrotoxic insults
Management: correction fluid deficits, treatment of the underlying causes
Prognosis of acute renal failure in horses
High recovery rate in horses ~70% IF:
Primary disease quickly treated
Toxins removed
Horse not oliguric
Clinical findings of tubulo-interstitial CRF in horses? Diagnosis?
Clinical signs - Weight loss, PU/PD, anorexia, dental tartar, colic, occasionally fever and/or incontinence
Laboratory findings - minimal proteinuria, normal or increased serum protein, hyponatremia and hypochloremia, occasional hypercalcemia, isosthenuria
Diagnosis - clinical signs, laboratory findings, ultrasound, biopsy
Ultrasound - often small kidneys, increased echogenicity, stones sometimes
Sabulous Cystitis in horses
Causes
Clinical signs
Treatment
Sabulous Cystitis
Causes
Bladder paralysis
Neurologic disease or musculoskeletal problems that prevent the normal posturing for urination
Clinical signs: incontinence
Affected horses may not present for months to years after onset of the problem
Treatment
Urine evacuation
Bladder lavage (repeated)
Bethanechol - parasympathomimetic drug, to stimulate the muscarinic receptors in the detrusor muscle.
Causes of stranguria in foals
“Dummy bladder”
Aspect of neonatal encephalopathy syndrome
Ruptured bladder
Urachal abscess
“Neurogenic bladder”
Newborn colts
Stranguria without obstruction or urinary tract rupture
Part of neonatal encephalopathy syndrome
Treatment
Indwelling catheter
Phenoxybenzamine - 5mg PO q12h
(a-adrenergic antagonist used to reduce urethral hypertonus)
Diagnosis and treatment of a ruptured bladder.
Diagnosis
Common in foals, post-partum mare, gelding with urethral obstruction
Stranguria, abdominal distention
Ultrasound
Bloodwork
Hyponatremia/chloremia, hyperkalemia
Azotemia
Peritoneal tap
Treatment
A medical emergency
Improve respiratory function
correct electrolyte, acid-base abnormalities
Hyperkalemia
Hyponatremia
Acute (<3 days) - do not raise serum [Na+] by >1-2 mEq/L/h
Chronic - do NOT raise serum [Na+] by >0.5-1.0 mEq/L/h
Peritoneal drain
Which of the following antibiotics is nephrotoxic?
fluoroquinolones
penicillins/beta-lactams
Aminoglycosides
Macrolides
Aminoglycosides
You diagnose a patient with AKI whose blood pressure is 220/110 and has several pinpoint retinal hemorrhages. How would you address the patient’s hypertension?
reduce the patient’s fluid rate
administer amlodipine and monitor blood pressure to optimize dosing to effect
administer ace inhibitor alone
recheck BP in 24 hours before intervening.
Administer amlodipine and monitor blood pressure to optimize dosing to effect
Which of the following drugs has the added benefit of affecting PPAR-gamma and has dramatically improved proteinuria in our experience at Cornell?
Benazepril
Telmisartan
Losaran
Enalapril
Telmisartan
Which of the following is NOT part of the general strategies for the medical management of urolithiasis?
Decreasing urine volume
increasing the solubility of crystalloids
increasing crystallization inhibitors
decreasing the concentration of calculogenic crystalloids
Decreasing urine volume (you want to increase urine volume)
You document persistent proteinuria in one of your canine patients. The urine protein:creatinine (UPC) ratio is 8.2 with an inactive sediment. Their USG has recently been as high as 1.032. Which of the following best describes the likely source of proteinuria?
pre-renal
renal, glomerular
renal, tubular
post-renal
renal, glomerular
Which of the following would be the most radio-opaque urolith?
cystine
urate
xanthine
calcium oxalate
Calcium oxalate
A 6-year-old female spayed Labrador retriever presents for stranguria and hematuria. You determine she has a urinary tract infection and radio-opaque cystic calculi. What diet would you consider to attempt dissolution?
Hill’s s/d
You diagnose a cat with Stage 1 CKD that has significant periodontal disease. In planning a dental procedure, which of the following is the LEAST important consideration to minimize the progression of your patient’s renal disease?
monitoring blood pressure and avoiding hypotension under anesthesia
avoiding NSAID for post-op pain management
minimizing extractions
providing appropriate fluid therapy to optimize peri-procedure hydration
minimizing extractions
What is the most common histologic lesion associated with chronic kidney disease in dogs and cats?
lymphoma
glomerulonephropathy
amyloidosis
chronic tubulointerstitial nephritis
Chronic tubulointersitial nephritis
A 9-year-old male castrated mixed breed dog presents for annual examination and vaccines. The client reports he is doing well and is very active and went swimming this morning. His PE is unremarkable. You recommend a CBC, Chemistry, and UA to screen for emerging diseases as he ages. His 4Dx is negative. He has a 3+ protein with a USG of 1.028 and no other lab abnormalities. What do you recommend next?
start ace inhibitor
abdominal and thoracic imaging
recheck a first-morning urine sample on a day after minimal activity
referral to an internist
recheck a first-morning urine sample on a day after minimal activity (swimming can lead to pre-renal proteinuria)
On average, SDMA blood concentrations are increased with what percentage loss of kidney function?
45%
Decreased cardiac output falls under which etiology of acute kidney injury?
intra-renal
pre-renal
post-renal
pre-renal
Which of the following is NOT a suitable treatment for urethral sphincter mechanism incompetence (USMI)?
Prazosin
Estriol (incurin)
Urethral bulking
PPA (Proin)
Prazosin
Patients with ectopic ureters may also present with which of the following conditions:
UTI
Paramesonephric septal remnant
Renal hypoplasia
All of the above
All of the above
Treatment options for Detrusor Urethral Dyssynergy (DUD) include:
Tamsulosin
Prazosin
Castration
All of the above
All of the above
What are the indications for a nephrectomy?
Irreparable trauma
Persistent hydronephrosis
Renal/perirenal masses
Persistent infection
Kidney donor
Postoperative considerations of a nephrectomy?
Fluids
Maintain renal perfusion and prevent clots in urinary tract
Monitor for azotemia
Monitor blood pressure
Avoid renal toxins
NSAIDs, Abx, dyes
indications for ureteral surgery
Ureteral obstructions
Calculi (Most common)
Stricture
Spay ligations
Neoplasia (rare - but can crawl up from bladder - TCC)
Ureteral ectopia necessitating reimplantation (extramural type) or laser ablation (intramural type)
Kidney transplantation
Normal Ureteral diameter in dogs and cats is:
0.4mm cats
Approx: 3mm in dogs
Surgical intervention of choice for chronic stone formers:
Ureteral stenting!!
Preferred over ureterotomy (creation of a stoma in the ureter) as this is associated with many complications.
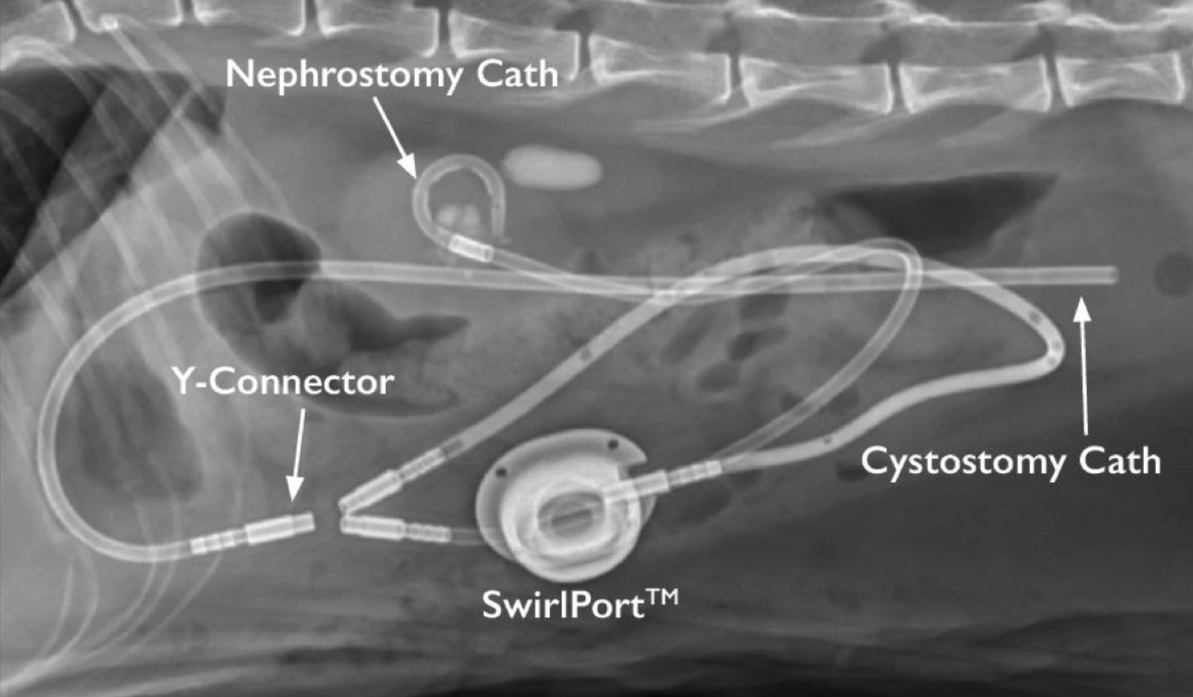
What is SUBS and why would you perform this?
Subcutaneous ureteral bypass system
Indications
ureteral strictures, calculi, trauma, neoplasia
ureteral stent reaction or intolerance.
Most often performed on cats! There is a high SUB calcification rate seen in canine patients, requiring a device exchange. Stents in cats are hard to place, so this was invented.
What is the appropriate procedure for ureteral obstructions in dogs?
ureteral stent
What is the most common cause for ureteral obstruction in dogs and cats?
ureterolithiasis
Indications for ureteral reimplantation in dog
Ureteral trauma
Distal ureteral obstruction
Extramural ectopic ureters
How do you surgically treat an extramural ectopic ureter?
Ureteroneocystostomy
How do you surgically treat an intramural ectopic ureter?
cystoscopic laser treatment
You COULD go a neoureterostomy, but this method is associated with less ureteral trauma and stricture. It is minimally invasive.
Cystotomies are most commonly performed for ______.
the removal of cystic calculi
True/false: antibiotics change culture results in dogs undergoing cystotomy.
false = treat them with antibiotics!!!!
Should you approach the bladder dorsally or ventrally during a cystotomy?
Ventral cystotomy
Veterinarians are nervous about ventral cystotomys due to pressure on the bladder, however this is not something that we see problems with
Going ventrally allows you to avoid the ureters
What samples should you collect during a cystolithotomy
Collect stones for stone analysis and culture
Collect bladder mucosa for culture
Do NOT waste client money on a pre-op urine culture
What is the holding layer of the bladder?
submucosa
Healing ability of the bladder? Which suture would you use?
full thickness defects regain 100% of normal tissue strength in 14-21 days.
Use absorbable or delayed absorbable monocryl
Postoperative management after a cystotomy
Always take postoperative imaging
In studies 14-20% of cases had stones left behind
Intravenous balanced electrolyte solution for 12-24h
Inform owner that cystotomy offers temporary relief and medical management may be necessary to prevent recurrence
Hematuria and small blood clots can be expected for 4-5 days postop.
UROKINASE produced by the endothelium
Most common bladder cancer in dogs and cats. Treatment?
transitional cell carcinoma.
Treat with a partial cystectomy - be careful of seeding/exfoliating.
check for metastasis first.
Prognosis of dog diagnosed with TCC
This is a very aggressive neoplasm
Most dogs die from urethral obstruction
Urethral stents
Permanent cystotomy catheter
Surgery alone 3-6 mo median survival
Chemotherapy
Piroxicam 6m median survival
COX2 inhibition
70% initial response rate
Mitoxantrone and piroxicam: 11m median survival.
Cats with FLUTD present with a small/large urinary bladder on PE
SMALL!
FLUTD is usually seen in
males or females
indoor or outdoor
Males
Indoor
self-limiting disease
What factors contribute to FLUTD?
Stress/lifestyle
inflammation
Crystalluria (stones)
Diet H2O
Urethral Plug
Genetics
Infection (uncommon)
3 main causes
Feline Interstitial (idiopathic) cystitis - FIC: most common
Urethral plugs (crystals, cells, mucus, debris)
Urolithiasis
True/false: bacterial cystitis is uncommon in cats <10years.
true
What are the indications that FLUTD is caused by bacterial infection?
Uncommon cause <10years
Female more likely
Recent urinary procedures
Urethral catheterization
Perineal urethrostomy
Urolithiasis
Systemic disease
How do you treat FLUTD?
Multimodal treatment
Pain, stress, DIET, water intake
NOT antibiotics! NOT NSAIDs! Steroids…probably not
Environmental modification/enrichment
Anxiolytics
gabapentin
Amitriptyline
Fluoxetine
Analgesics
buprenorphine
fentanyl
gabapentin
Alpha-1 Antagonist (smooth muscle relaxation)
prazosin
phenoxybenzamine
Client Education is key
self limiting but recurrent condition
Acid base and electrolyte derangements caused by urethral obstruction.
metabolic acidosis
uremic acids
Hyperlactatemia caused by hypoperfusions
Respiratory acidosis
hypoventilation
Hyperkalemia
decreased renal excretion
shifting from IC > EC due to acidosis
cardiac implications
Hypocalcemia
unclear pathophysiology
cardiac implications