Revisesed - Chapter 19 Flashcards: The Peripheral Endocrine Glands: Adrenal Gland
1/162
Earn XP
Description and Tags
Pages 672 - 685, 666-671, 701 - 713
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
163 Terms
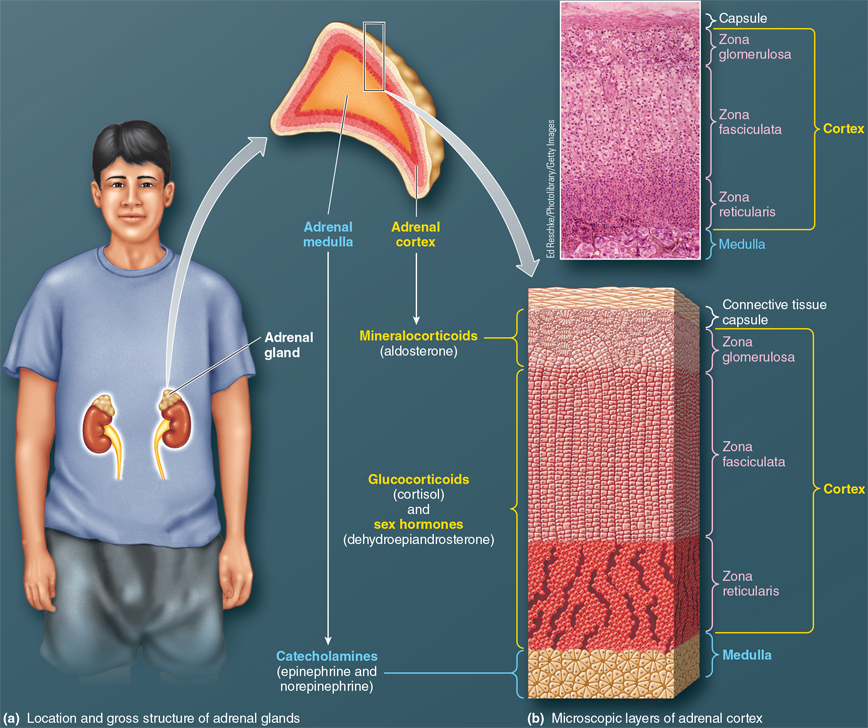
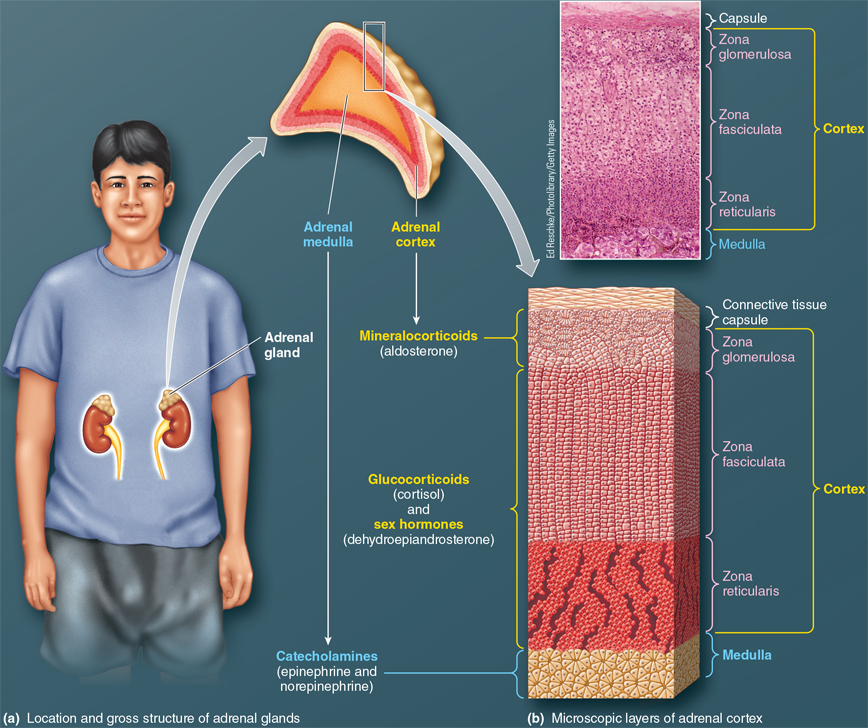
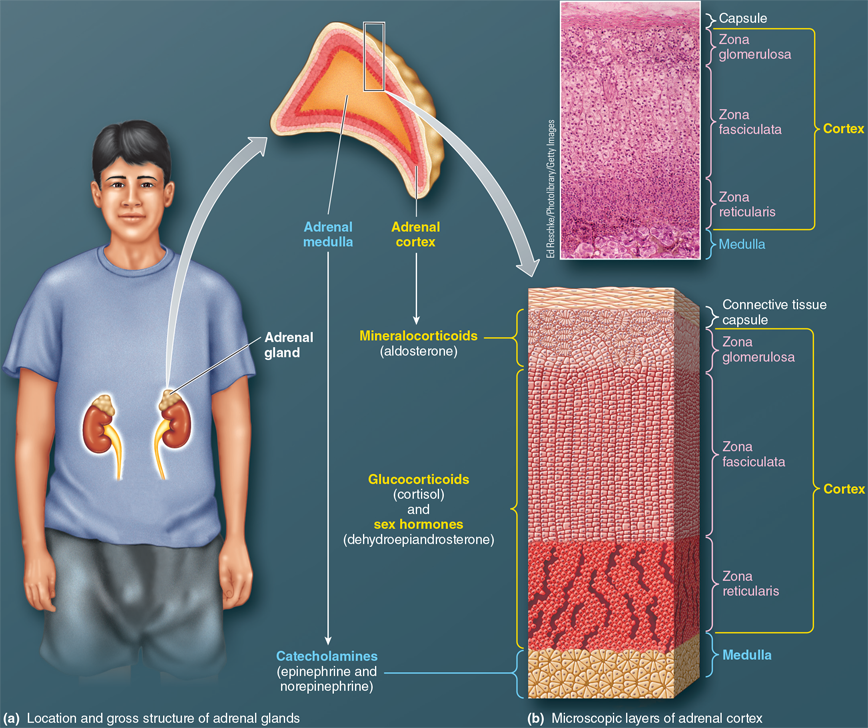
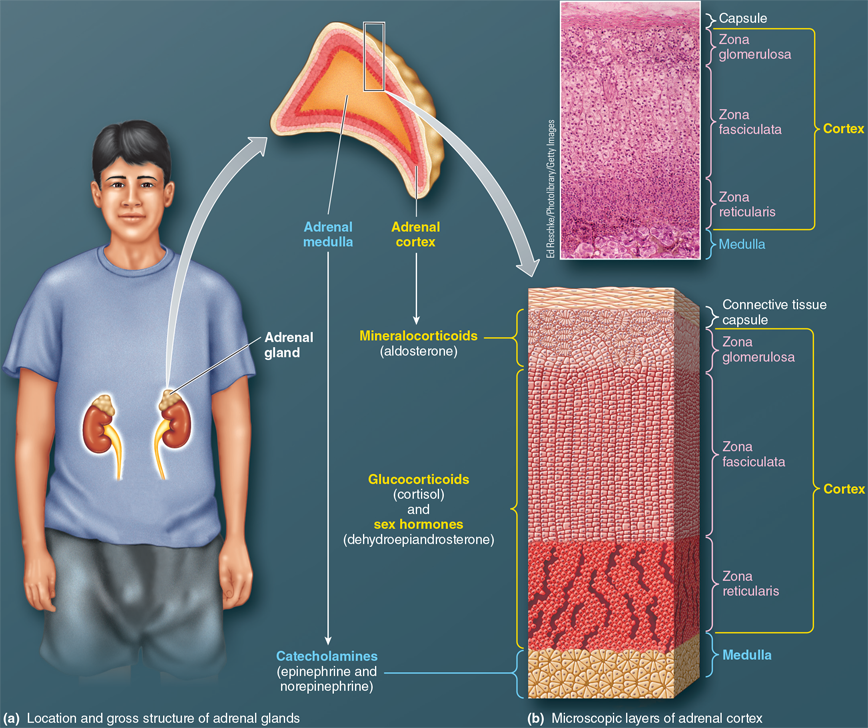
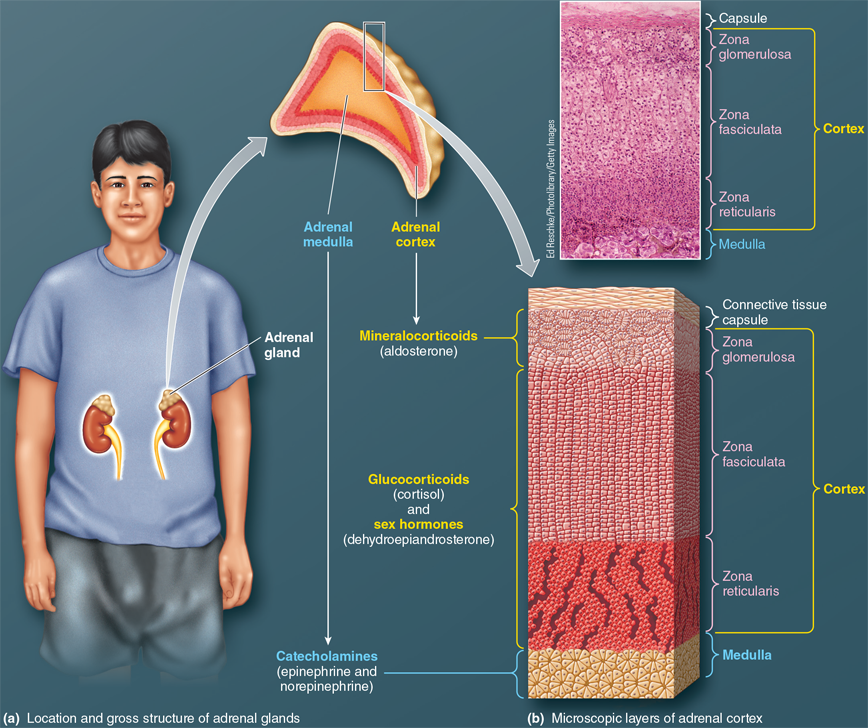
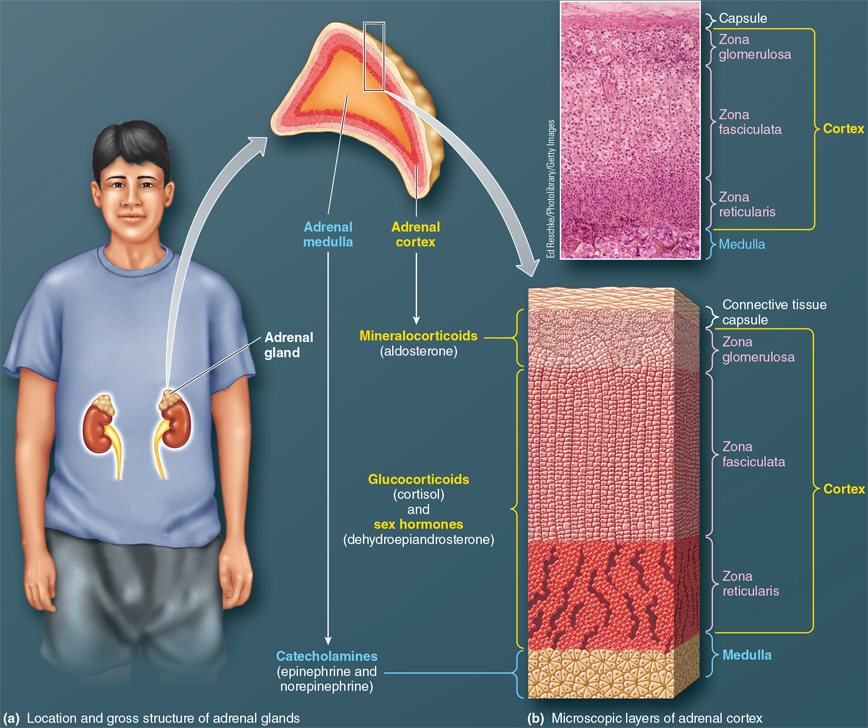
Where is the location of the adrenal glands?
They are embedded above each kidney in a capsule of fat.
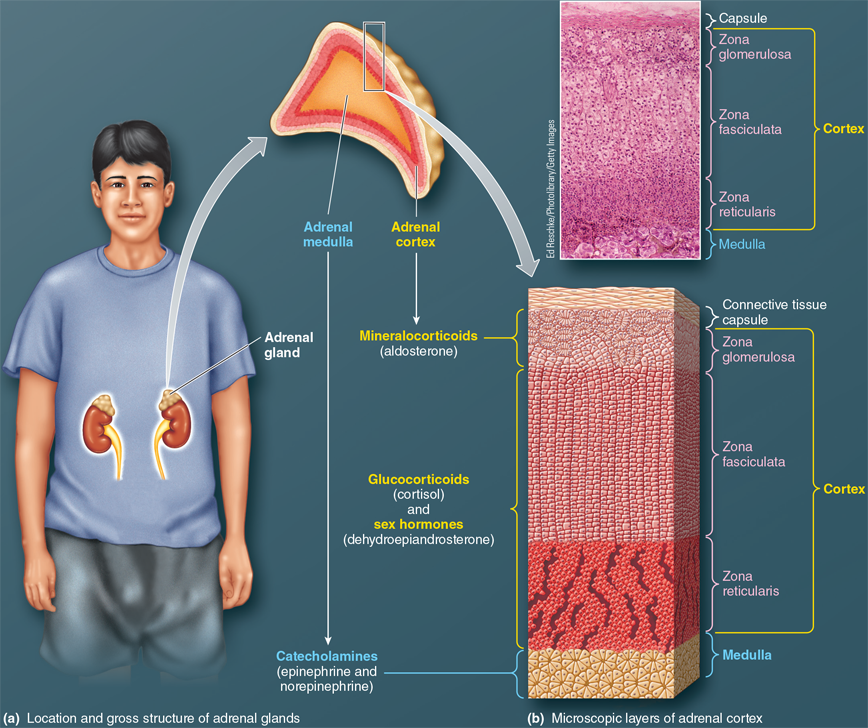
What are the two endocrine glands in the adrenal gland, and how are they structured?
The adrenal cortex forms the outer layer, while the adrenal medulla is the inner portion
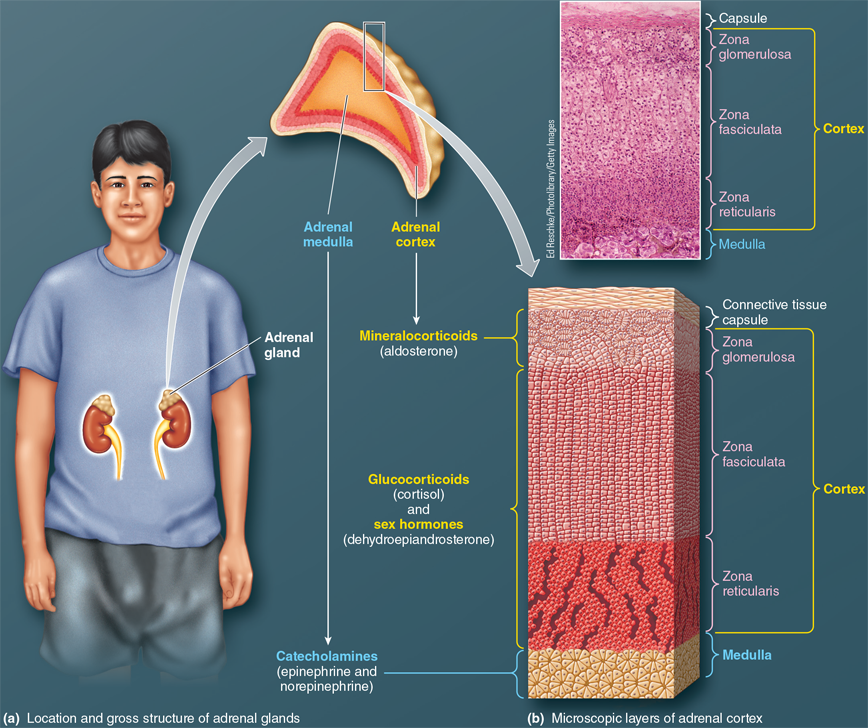
What types of hormones does the adrenal cortex secrete?
The adrenal cortex secretes a variety of steroid hormones, including glucocorticoids, mineralocorticoids, and androgens.
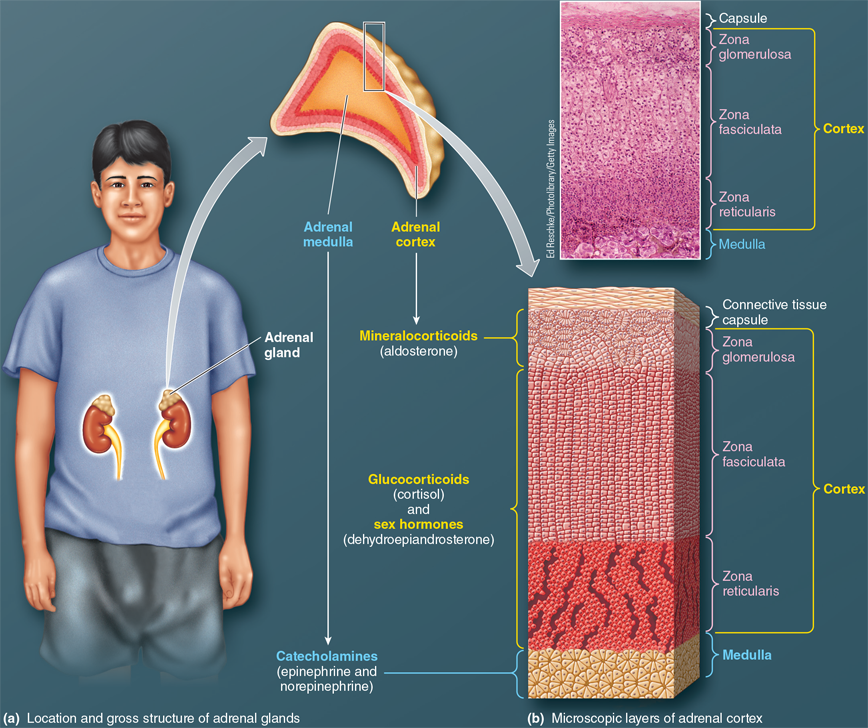
What type of hormones does the adrenal medulla secrete?
The adrenal medulla secretes catecholamines, such as epinephrine and norepinephrine.
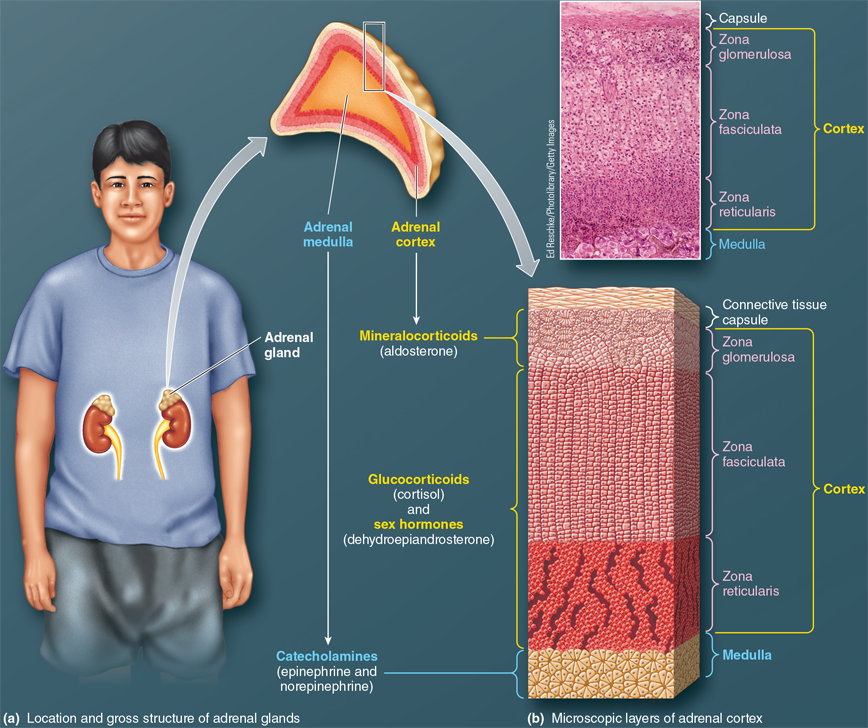
What are the 3 Different layers of the adrenal cortex?
Zona golmerulosa (outer layer)
Zona faciculata (middle layer)
Zona reticularis (inner layer)
What are adrenal cortex hormones derived from?
cholesterol
What is the primary function of mineralocorticoids (e.g., aldosterone)?
like aldosterone, regulate electrolyte balance, specifically Na⁺ (sodium) and K⁺ (potassium) balance.
What is the main role of glucocorticoids (e.g., cortisol)?
Like cortisol, regulate glucose metabolism, and also affect protein and lipid metabolism and help the body adapt to stress.
What is the most important adrenocortical sex hormone, and what type of hormone is it?
The most important adrenocortical sex hormone is dehydroepiandrosterone (DHEA), an androgen (a "male" sex hormone)
Where is aldosterone produced in the adrenal cortex?
Aldosterone is produced exclusively in the zona glomerulosa of the adrenal cortex
In which part of the adrenal cortex is cortisol primarily synthesized?
Cortisol is primarily synthesized in the zona fasciculata, one of the inner layers of the adrenal cortex.
Can other tissues outside the adrenal cortex produce mineralocorticoids or glucocorticoids?
No, only the adrenal cortex can produce mineralocorticoids and glucocorticoids.
Where are adrenal sex hormones produced, and how does this compare to their production in the gonads?
Adrenal sex hormones are produced in the zona fasciculata and zona reticularis of the adrenal cortex, but they are produced in far greater abundance in the gonads (testes in males and ovaries in females).
What happens to adrenocortical hormones once they are synthesized?
Adrenocortical hormones are lipophilic, so they diffuse through the plasma membrane of steroidogenic cells into the blood and must bind to plasma proteins to travel in the bloodstream.
What are adrenocortical hormones?
Adrenocortical hormones are steroid hormones produced by the adrenal cortex, including mineralocorticoids (e.g., aldosterone), glucocorticoids (e.g., cortisol), and sex hormones (e.g., dehydroepiandrosterone).
What are steroidogenic cells?
Steroidogenic cells are specialized cells in the adrenal cortex that synthesize and secrete steroid hormones, including those classified as adrenocortical hormones.
What type of neurons make up the adrenal medulla?
The adrenal medulla consists of modified sympathetic postganglionic neurons known as chromaffin cells.
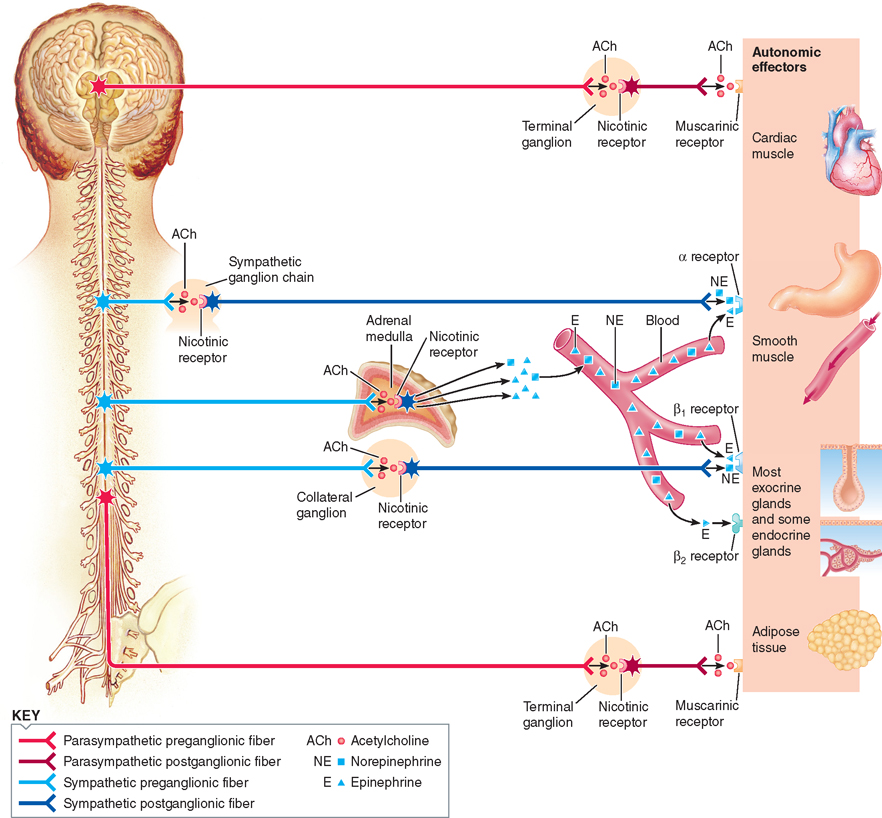
How does the adrenal medulla function as part of the sympathetic nervous system?
The adrenal medulla is a modified part of the sympathetic nervous system and releases hormones directly into the blood, bypassing the typical pathway of terminating on effector organs.
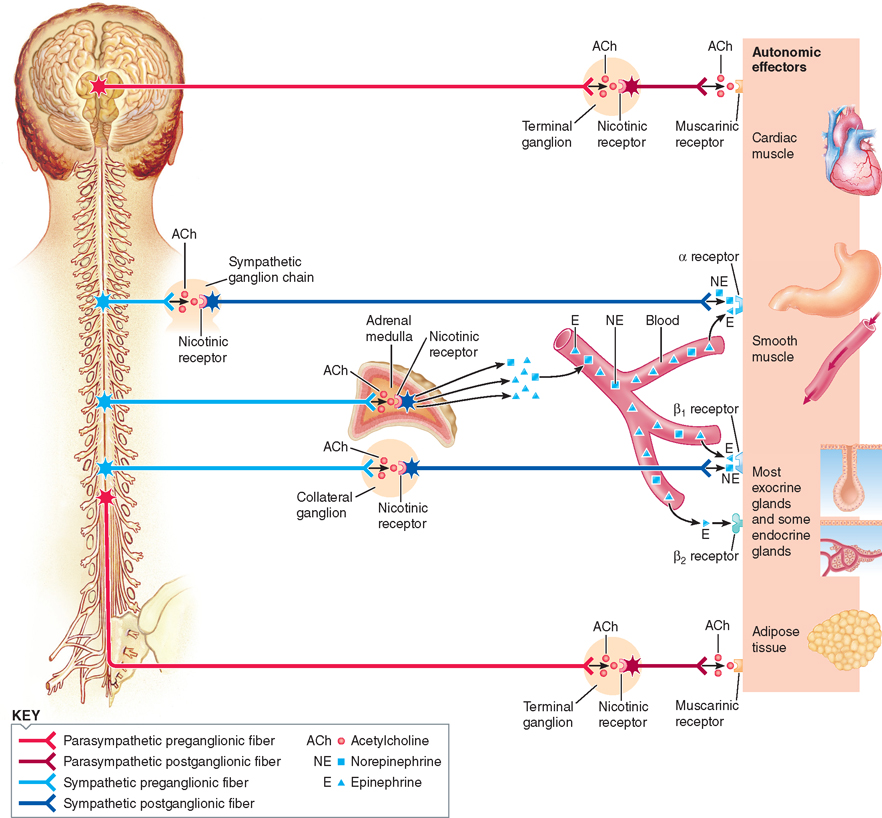
What hormones are released by the adrenal medulla, and what is their primary output?
The adrenal medulla releases norepinephrine and epinephrine, with epinephrine accounting for 80% of the total catecholamine output.
What protects catecholamines from being destroyed during storage?
Catecholamines (primarily epinephrine and norepinephrine) are stored in chromaffin granules, which protect them from being destroyed by cytosolic enzymes.
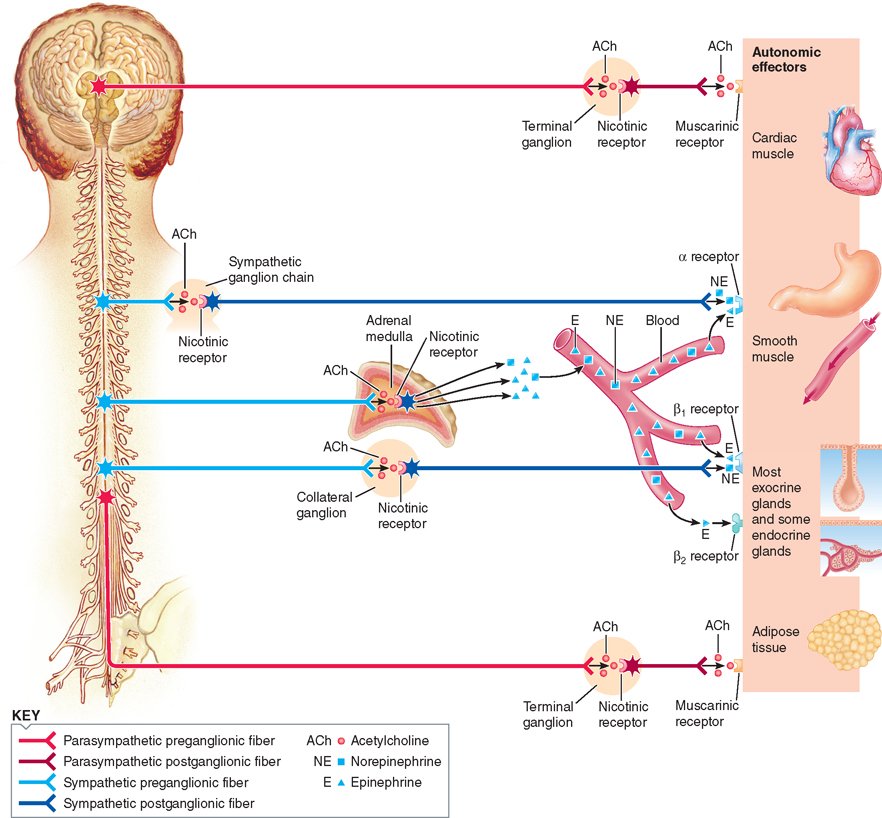
How do the production locations of epinephrine and norepinephrine differ?
Epinephrine is produced exclusively by the adrenal medulla, while the bulk of norepinephrine is produced by sympathetic postganglionic fibers.
What are the major effects of mineralocorticoids?
Mineralocorticoids primarily affect Na+ and K+ balance and are crucial for maintaining blood pressure homeostasis.
Where does aldosterone mainly work in the body?
Aldosterone mainly works in the kidneys, where it helps the body keep Na+ (salt) and get rid of K+ (potassium) when making urine.
How does aldosterone affect ECF volume and blood pressure?
Aldosterone promotes Na+ retention, which induces osmotic retention of water, expanding the ECF volume (including plasma volume) and playing an important role in long-term regulation of blood pressure.
What happens without aldosterone?
Without aldosterone, a person rapidly dies from circulatory shock due to excessive Na+-holding water loss, which causes a marked fall in plasma volume.
Does ACTH from the anterior pituitary regulate aldosterone secretion?
No, ACTH promotes secretion of cortisol, not aldosterone. Regulation of aldosterone secretion is independent of the anterior pituitary.
What are the primary metabolic effects of cortisol?
Cortisol increases blood glucose by stimulating gluconeogenesis, inhibits glucose use by many tissues (except the brain), promotes protein degradation, and facilitates lipolysis (fat breakdown).
How does cortisol help maintain blood glucose levels?
Cortisol stimulates gluconeogenesis in the liver, converting non-carbohydrates (like amino acids) into glucose, helping maintain blood glucose levels between meals.
What is the role of cortisol in the brain's glucose supply?
Cortisol ensures that glucose is available for the brain by inhibiting glucose uptake by other tissues, making it a priority for brain function.
How does cortisol affect protein and fat stores?
Cortisol increases protein degradation (mainly in muscles) and stimulates lipolysis, breaking down fats and releasing fatty acids for energy use.
What is the role of cortisol in vasoconstriction?
Cortisol has a permissive role, meaning it must be present in sufficient amounts to allow catecholamines (like epinephrine) to induce vasoconstriction during stress.
How does cortisol help with adaptation to stress?
Cortisol mobilizes glucose, amino acids, and fatty acids during stress, providing essential fuel for the brain and supporting tissue repair during injury.
What are the anti-inflammatory effects of cortisol?
Cortisol suppresses inflammation by inhibiting neutrophil migration, blocking cytokine production, and reducing immune responses like antibody production.
How do synthetic glucocorticoids differ from natural cortisol?
Synthetic glucocorticoids are designed to maximize anti-inflammatory effects while minimizing metabolic effects, useful in treating conditions like rheumatoid arthritis and allergies.
What are some side effects of long-term glucocorticoid use?
Prolonged use can lead to infections, gastric ulcers, high blood pressure, bone thinning, and menstrual irregularities.
Why is prolonged glucocorticoid use dangerous for the adrenal cortex?
Prolonged use of glucocorticoids suppresses the hypothalamus-pituitary-adrenal axis, which can lead to adrenal atrophy—a condition where the adrenal cortex shrinks and loses its ability to produce cortisol naturally, possibly resulting in permanent damage.
What sex hormones does the adrenal cortex secrete in both sexes?
The adrenal cortex secretes small amounts of both androgens (male sex hormones) and estrogens (female sex hormones) in both males and females.
What is the primary androgen secreted by the adrenal cortex?
The main androgen secreted by the adrenal cortex is dehydroepiandrosterone (DHEA), which is weaker than testosterone but physiologically important in females.
How do adrenal androgens compare in males and females?
In males, adrenal androgens like DHEA are overpowered by testosterone from the testes, whereas in females, DHEA plays a key role in pubic hair growth, pubertal growth spurt, and sex drive.
What controls adrenal androgen secretion?
ACTH from the anterior pituitary controls the secretion of adrenal androgens like DHEA, which often parallels cortisol secretion.
What happens to DHEA levels as a person ages?
DHEA secretion peaks between the ages of 25 and 30, then gradually declines, reaching less than 15% of its peak level by the age of 60.
What is the relationship between epinephrine and norepinephrine in the body?
Epinephrine and norepinephrine exert similar effects in many tissues, with epinephrine generally reinforcing sympathetic nervous activity.
What makes epinephrine and norepinephrine distinctive.
their different affinities for different receptor types
What role do epinephrine and norepinephrine play in stress responses?
They support peak physical exertion during stressful situations by increasing cardiac output and blood pressure, helping to prepare the body for fight-or-flight.
How does epinephrine affect blood flow during stress?
Epinephrine causes vasoconstriction to increase blood pressure and redirects blood to vital organs like the heart and skeletal muscles through vasodilation.
What is one respiratory effect of epinephrine?
Epinephrine dilates the respiratory airways, reducing resistance and making it easier to move air in and out of the lungs.
How does epinephrine affect the digestive and urinary systems during fight-or-flight?
Epinephrine reduces digestive activity and inhibits bladder emptying, as these processes are temporarily put on hold during stress.
What are the metabolic effects of epinephrine?
Epinephrine increases blood glucose by stimulating gluconeogenesis and glycogenolysis in the liver and muscles. It also promotes the breakdown of fat (lipolysis) to raise blood fatty acid levels.
How does epinephrine affect insulin and glucagon?
Epinephrine inhibits insulin secretion, reducing glucose uptake, and stimulates glucagon secretion to further increase blood glucose levels.
Why is epinephrine’s metabolic effect important in fight-or-flight situations?
It provides extra fuel (glucose and fatty acids) for muscle work and ensures adequate energy for the brain during the crisis.
How does epinephrine impact the body’s overall metabolic rate?
Epinephrine increases the metabolic rate, enhancing energy production in tissues like the heart, respiratory muscles, and liver.
What effect does epinephrine have on the central nervous system (CNS)?
Epinephrine promotes arousal and increased alertness, helping quick thinking and response in emergency situations.
What are some other physical effects of epinephrine during stress?
Epinephrine causes sweating to release extra heat from muscle activity and dilates pupils for improved vision in a threatening situation.
What triggers the release of epinephrine from the adrenal medulla?
Epinephrine is released only through sympathetic stimulation of the adrenal medulla, usually in response to fear or stress.
What is hypercortisolism, and what condition is it associated with?
Hypercortisolism is the excessive secretion of cortisol, associated with Cushing's Syndrome.
What are the possible causes of excessive cortisol secretion in Cushing's Syndrome?
: Causes include overstimulation of the adrenal cortex by excessive CRH or ACTH, adrenal tumors secreting cortisol independently of ACTH, and ACTH-secreting tumors located outside the pituitary.
What are the prominent symptoms of Cushing's Syndrome?
ymptoms include hyperglycemia, glucosuria, muscle weakness, abnormal fat distribution (e.g., "buffalo hump" and "moon face"), thin skin, easy bruisability, and poor wound healing
What effects does excess cortisol have on glucose and protein metabolism?
Excess cortisol leads to increased gluconeogenesis, resulting in high blood glucose levels and protein breakdown, causing muscle loss and weakness.
What is the cause of aldosterone hypersecretion, and what condition is it referred to?
Aldosterone hypersecretion can be caused by an adrenal tumor (primary hyperaldosteronism, Conn’s syndrome) or high activity of the renin-angiotensin-aldosterone system (RAAS) due to chronic arterial blood flow reduction to the kidneys (secondary hyperaldosteronism).
What are the symptoms of aldosterone hypersecretion?
Symptoms include hypernatremia (excess sodium retention), hypokalemia (potassium depletion), and hypertension (high blood pressure).
What is hypo-cortisol's, and what condition does it refer to?
Hypo-cortisol's is the inadequate secretion of cortisol, referred to as Addison's Disease.
What is the most common cause of primary adrenal insufficiency (Addison’s Disease)?
The most common cause is autoimmune destruction of the adrenal cortex, leading to the deficiency of both aldosterone and cortisol.
What are the symptoms associated with Addison's Disease?
Symptoms include hyperkalemia (potassium retention), hyponatremia (sodium depletion), hypotension (low blood pressure), poor stress response, hypoglycemia, and hyperpigmentation of the skin.
What is the relationship between ACTH and skin pigmentation in Addison's Disease?
n Addison’s Disease, low cortisol levels lead to elevated ACTH levels, which can bind to α-MSH receptors in the skin, causing hyperpigmentation.
How does adrenal androgen hypersecretion manifest in adults and children?
In adult females, it can cause hirsutism and cessation of menstruation; in newborn females, it may result in male-type external genitalia; in prepubertal boys, it causes precocious pseudopuberty.
What is the underlying enzymatic defect in adrenogenital syndrome?
It is often caused by a deficiency of an enzyme essential for cortisol synthesis, leading to excess production of androgens and insufficient cortisol levels.
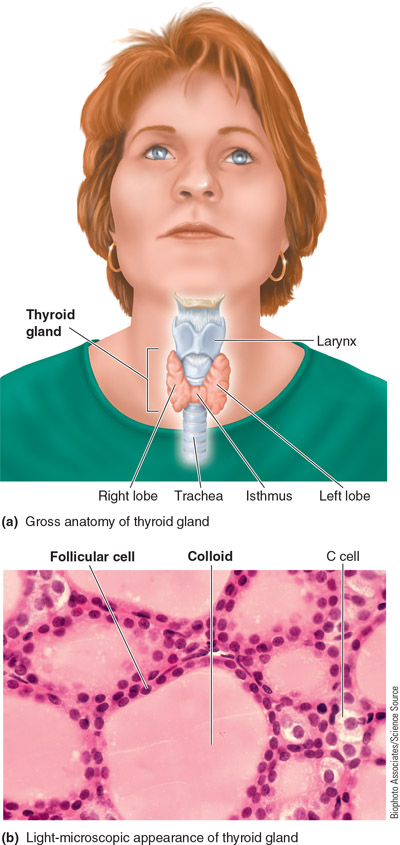
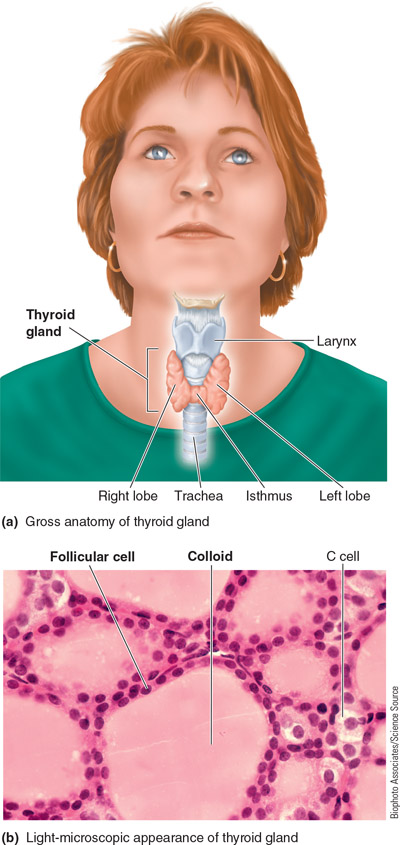
What is the thyroid gland and where is it located?
It consist of two lobes of endocrine tissue joined in the middle by narrow tissue glands, the isthmus, creating a bow tie shape. it is located lying in the neck over the trachea.
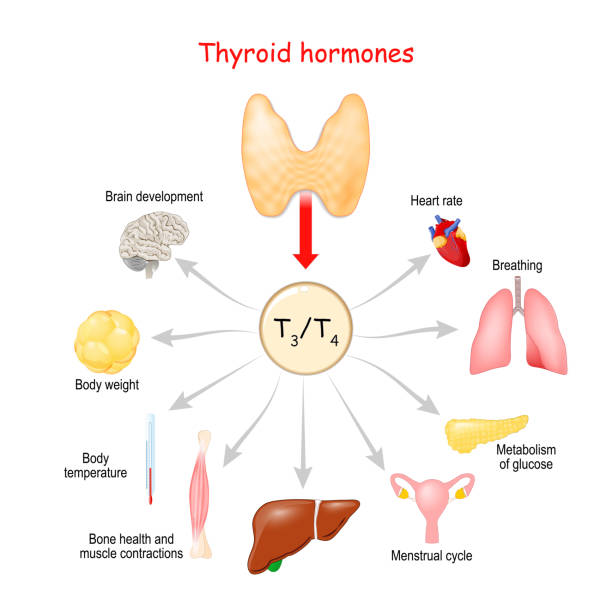
What does the thyroid gland do?
it secretes the hormones thyroxine and tri-iodothyronine, which regulates the overall basal metabolic rate, and calcitonin, which contributes to control of calcium balance.
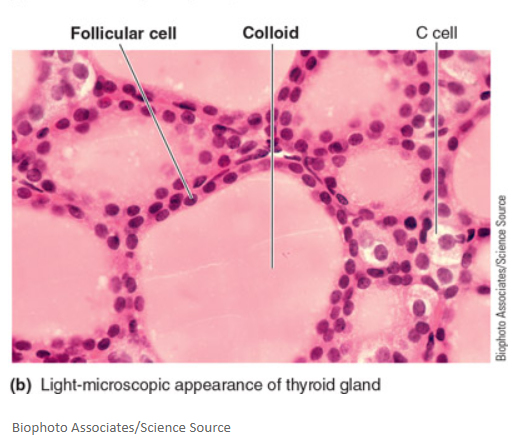
What are follicular cells?
These are the major thyroid secretory cells and can arrange into a hollow sphere called a follicle
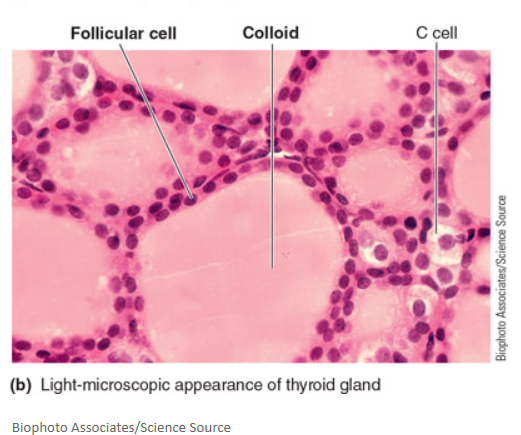
What is a colloid?
Colloid is a viscous substance found within the lumen of thyroid follicles, serving as an extracellular storage site for thyroid hormones until they are needed by the body.
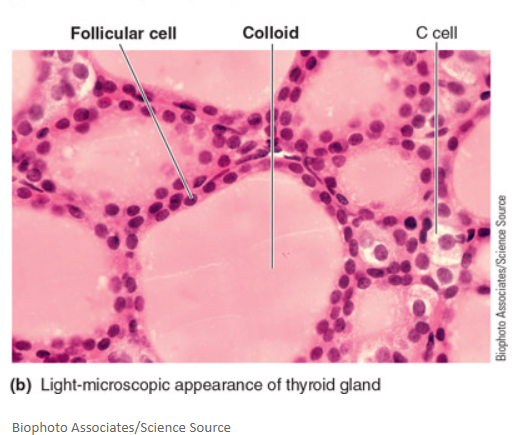
What is a follicle?
A follicle is a hollow, spherical structure in the thyroid gland formed by a single layer of follicular cells that surrounds an inner lumen filled with colloid. It serves as a functional unit for storing thyroid hormones.
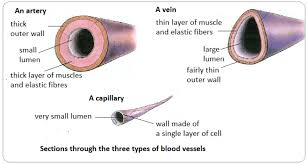
What is a lumen?
Lumen refers to the inner open space or cavity of a tubular structure, such as a follicle or blood vessel, through which substances can pass or be contained. In the context of the thyroid gland, the lumen is the cavity within a follicle that holds colloid.
What are the thyroid hormones?
these are produced in the follicular cells, derived from amino acid tyrosine, known as tetraiodothyronine and tri-iodothyronine. These are important regulators in overall basal metabolic rate.
What are the basic ingredients for thyroid hormone?
tyrosine and iodine
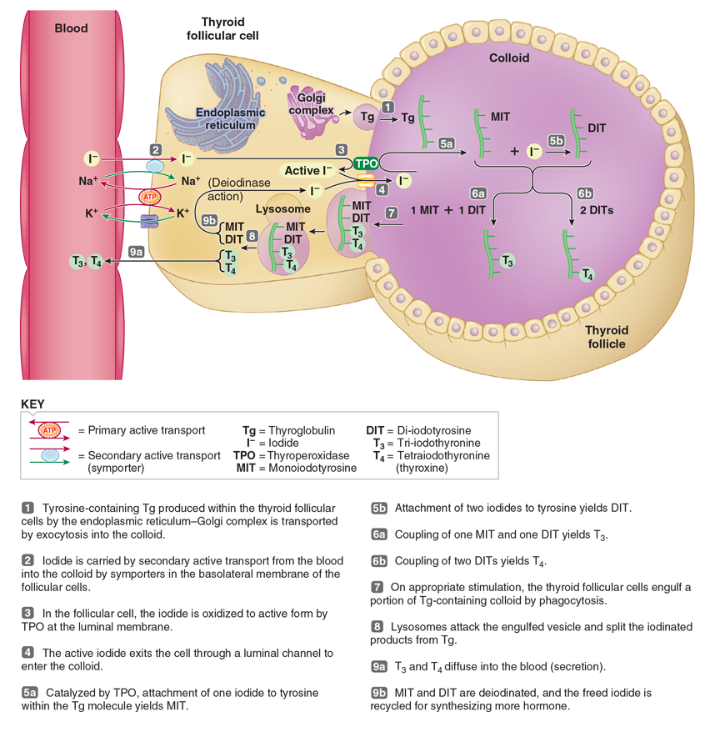
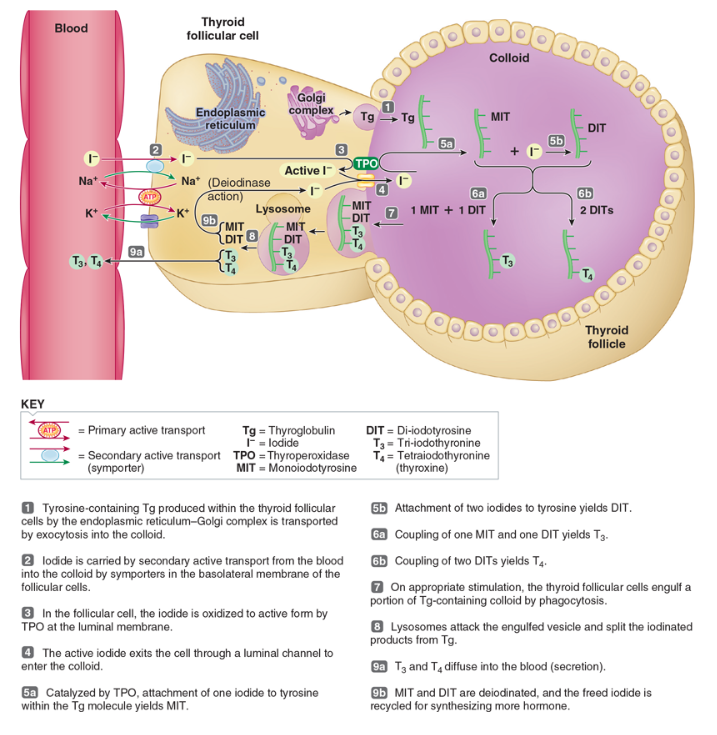
What is the process of thyroid hormone biosynthesis, and what are its key components?
Thyroid hormone biosynthesis involves the uptake of the amino acid tyrosine and iodide from the blood by follicular cells in the thyroid gland. Tyrosine is synthesized in sufficient amounts by the body, while dietary iodine must be reduced to iodide before absorption. The iodide is then transported into the follicular cells via the iodide trap, where it is oxidized to "active" iodide by the enzyme thyroperoxidase (TPO) at the luminal membrane.
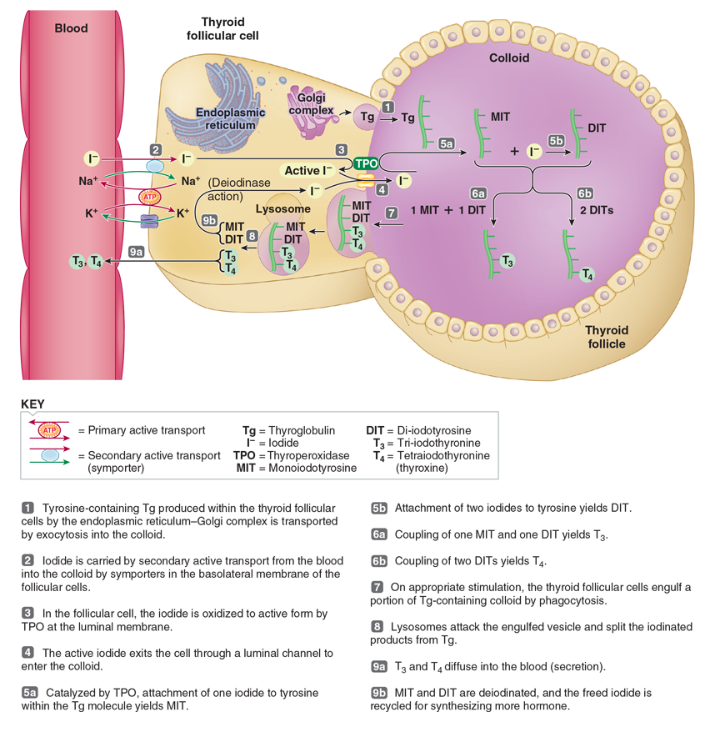
How is thyroglobulin formed, and what role does it play in thyroid hormone synthesis?
Thyroglobulin is a large protein produced by the endoplasmic reticulum-Golgi complex of follicular cells. As it is synthesized, tyrosine becomes incorporated into thyroglobulin. Once produced, this tyrosine-containing thyroglobulin is secreted into the colloid via exocytosis, where it serves as a precursor for thyroid hormone synthesis. Within the colloid, iodide is attached to tyrosine residues in thyroglobulin, forming monoiodotyrosine (MIT) and diiodotyrosine (DIT).
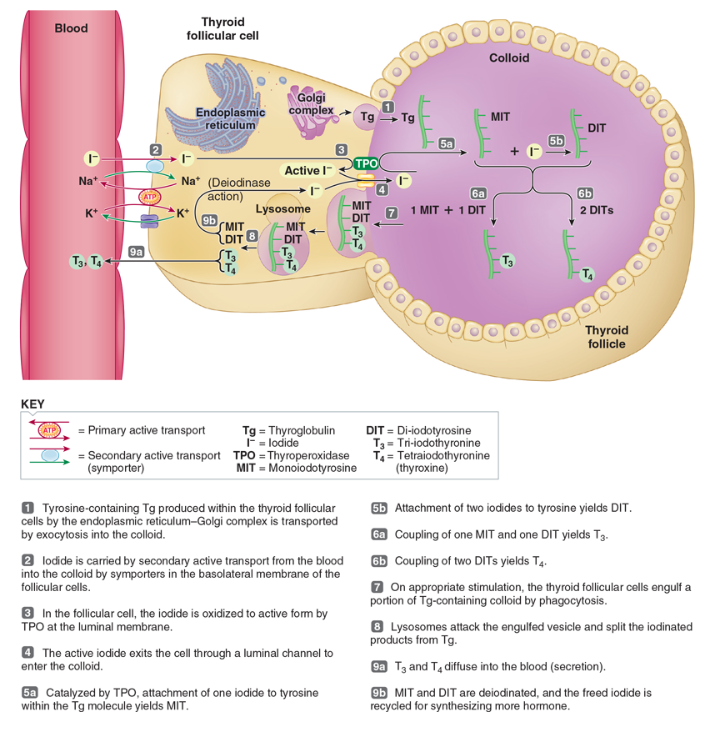
What is the coupling process in thyroid hormone synthesis, and how are hormones stored?
The coupling process occurs within the thyroglobulin molecule, where MIT and DIT combine to form the active thyroid hormones T3 (tri-iodothyronine) and T4 (thyroxine). T3 is formed by coupling one MIT with one DIT, while two DIT molecules yield T4. These hormones remain attached to thyroglobulin in the colloid, where they are stored until needed, providing a reserve that can last for several months.
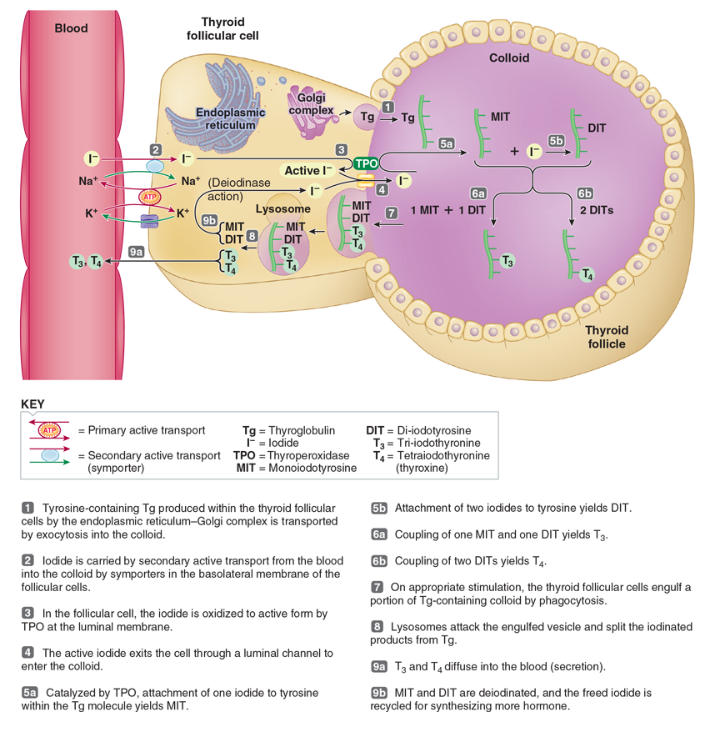
Describe the mechanism of thyroid hormone secretion from the thyroid gland.
To secrete thyroid hormones, follicular cells phagocytize the colloid containing thyroglobulin-hormone complexes. The internalized colloid droplets merge with lysosomes, where enzymes break down thyroglobulin, releasing T3 and T4. These lipophilic hormones then diffuse across the cell membranes of the follicular cells into the bloodstream, while the inactive forms, MIT and DIT, are recycled within the cells.
How are T3 and T4 transported in the bloodstream, and what is their biological significance?
Once released into the bloodstream, T3 and T4 quickly bind to plasma proteins, primarily thyroxine-binding globulin, with less than 0.1% of T4 and less than 1% of T3 remaining unbound and biologically active. T4 is secreted in greater amounts (about 90%) but is converted to the more potent T3 outside the thyroid gland, primarily in the liver and kidneys. T3 is the major active form of thyroid hormone at the cellular level, regulating metabolism and influencing various physiological processes.
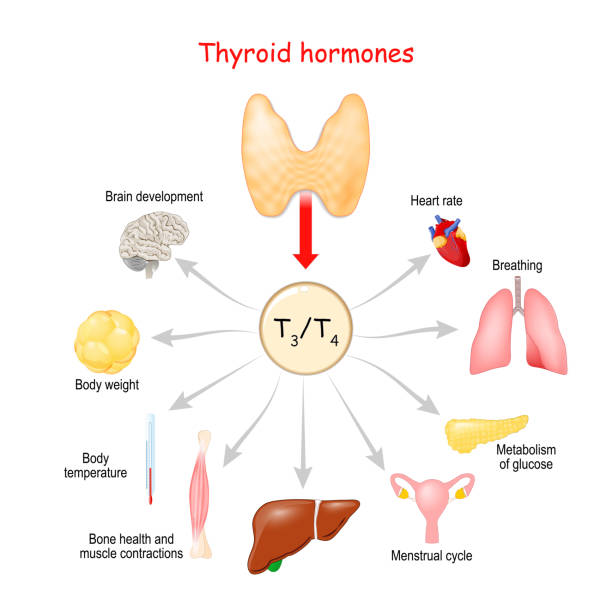
How does thyroid hormones affect the body?
It can affect every tissue in the body by crossing the plasma membrane and binds with intracellular receptors of DNA. this binding alters the transcription of specific mRNA and this synthesis new proteins or enzymes.
why is the thyroid hormone actions considered “sluggish”?
the response to increase thyroid hormone is detectable after several hours and its maximal is not for several days.
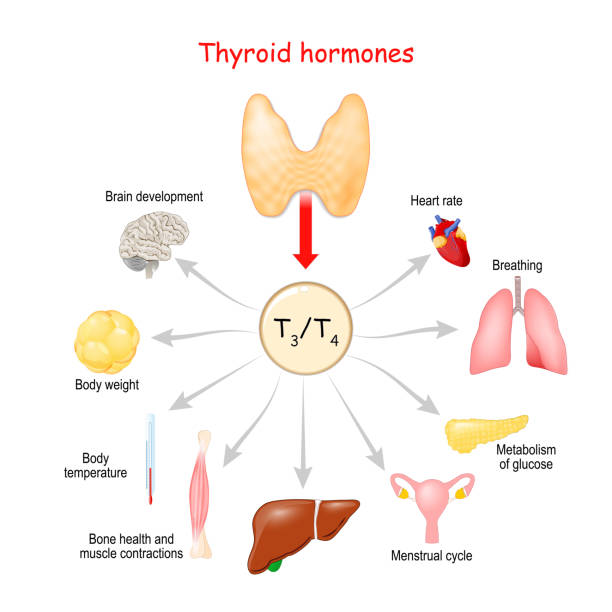
How does thyroid hormone influence metabolic rate and heat production in the body?
Thyroid hormone significantly increases the body's basal metabolic rate (BMR), which refers to the rate of oxygen consumption and energy expenditure while at rest. It is the primary regulator of BMR, enhancing metabolic activity. This increased metabolic activity leads to a calorigenic effect, meaning it produces more heat as a byproduct of higher energy expenditure, contributing to overall body temperature regulation.
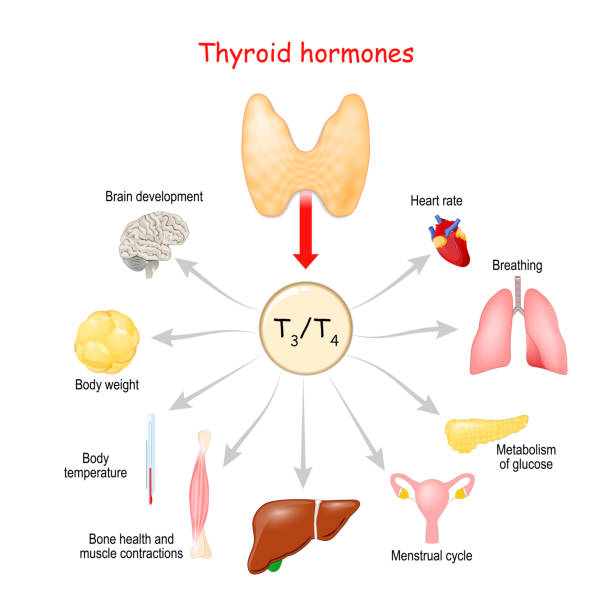
how does the thyroid hormone affect the cardiovascular system?
Increases heart rate and force of contraction, and increasing the heart response to catecholamines.
How does thyroid hormone affect growth?
Thyroid hormone is essential for normal growth as it stimulates the secretion of growth hormone (GH) and increases insulin-like growth factor I (IGF-I) production in the liver, promoting tissue growth and bone development.
What role does thyroid hormone play in the development of the nervous system?
Thyroid hormone is crucial for the normal development of the central nervous system (CNS). Its deficiency from birth can hinder nervous system development.
Why is thyroid hormone important for adults?
In adults, thyroid hormone is essential for maintaining normal central nervous system (CNS) activity, supporting overall neurological function.
What is the sympathomimetic effect of thyroid hormone?
Thyroid hormone mimics sympathetic nervous system actions by increasing target-cell receptors for catecholamines (epinephrine and norepinephrine), enhancing their effects.
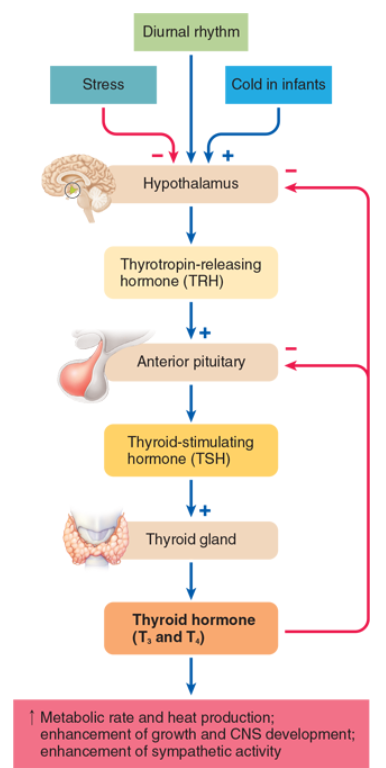
What is Thyroid stimulating hormone?
an anterior pituitary hormone that stimulates secretion of thyroid hormone and promotes growth of the thyroid gland.
What happens if there is no thyroid stimulating hormone (TSH)?
the thyroid atrophies (decreases in size) and secretes its hormones at a very low rate.
What happens if there in excess thyroid stimulating hormone (TSH)?
the thyroid it undergoes hypertrophy (increases the size of each follicular cell) and hyperplasia (increases the number of follicular cells) in response
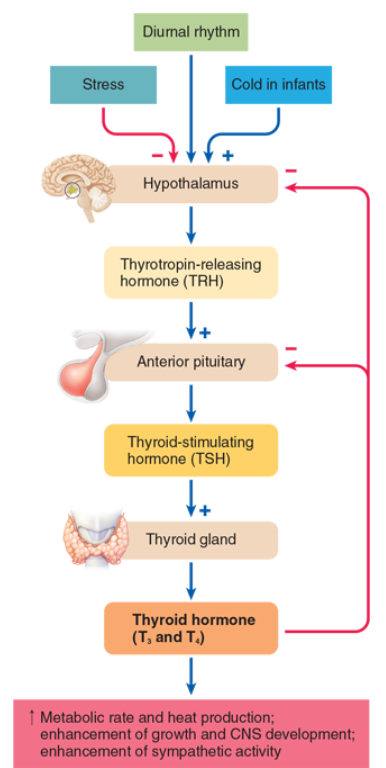
What role does thyrotropin-releasing hormone (TRH) play in TSH secretion?
TRH stimulates the anterior pituitary to secrete thyroid-stimulating hormone (TSH) in a tropic manner, activating thyroid hormone production.
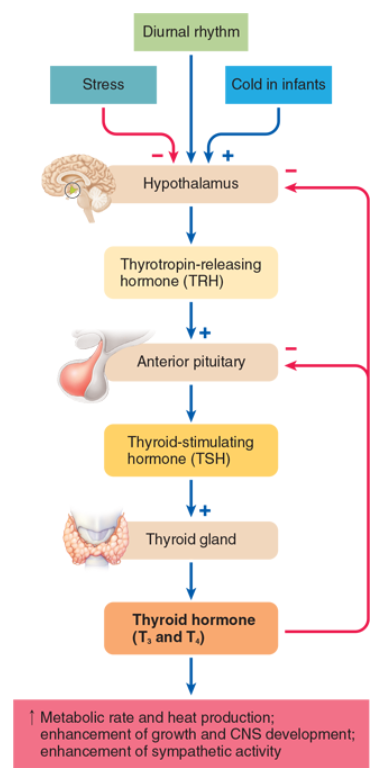
How does thyroid hormone regulate TSH secretion?
Thyroid hormone inhibits TSH secretion from the anterior pituitary and hypothalamus through negative feedback, helping to maintain stable thyroid hormone levels.
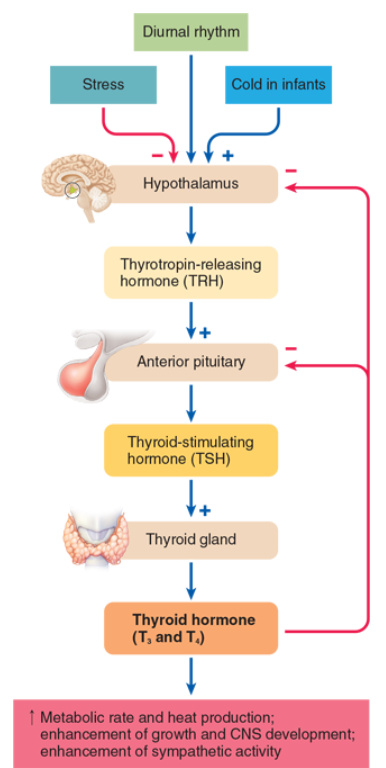
What is the function of the negative feedback loop between thyroid hormone and TSH?
The negative feedback loop regulates free thyroid hormone levels daily, while the hypothalamus mediates long-term adjustments in hormone secretion.
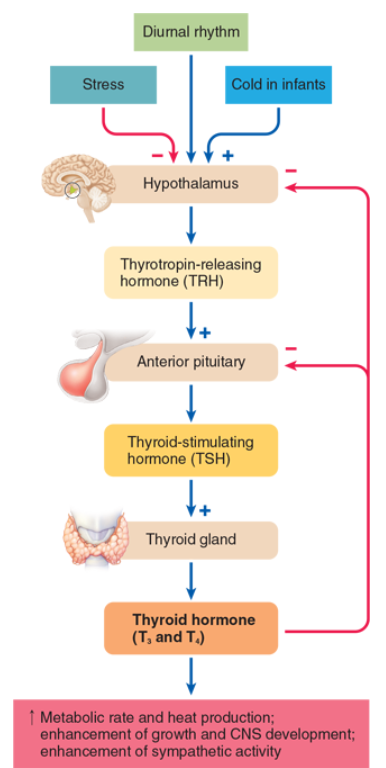
What effect does cold exposure have on TRH secretion in newborns?
Cold exposure increases TRH, TSH, and thyroid hormone secretion in newborns to help maintain body temperature during the transition from the mother’s warmth to cooler air.
What types of stress affect TSH and thyroid hormone secretion?
Physical stress, starvation, and infection inhibit TSH and thyroid hormone secretion, likely through neural influences on the hypothalamus. The adaptive significance of this inhibition is unclear.
What is hypothyroidism?
the deficiency of thyroid hormone secretion
What is hyperthyroidism?
the excess of thyroid hormone secretion
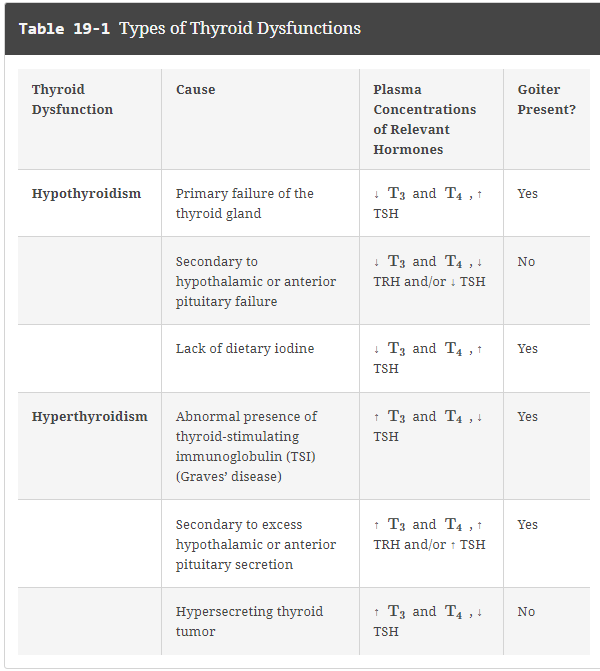
What can cause hypothyroidism ?
Primary failure of the thyroid gland
deficiency of TRH and/ or TSH hormone
inadequate dietary iodine
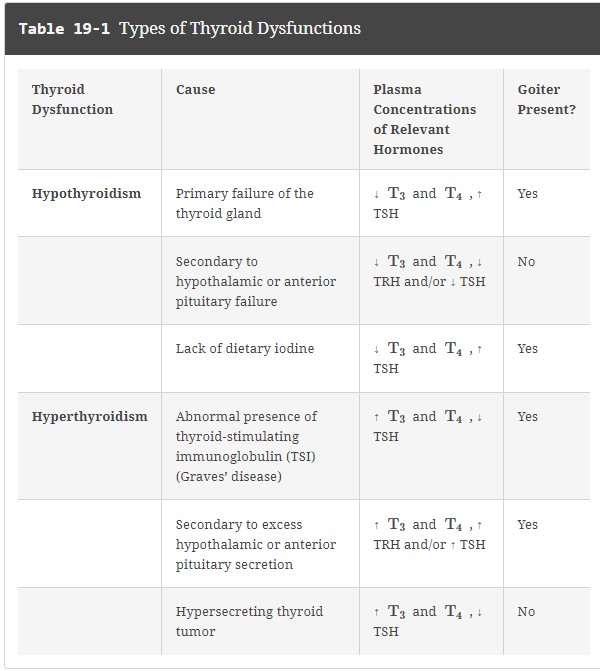
What are the symptoms of hypothyroidism?
had a reduce basal metabolic rate
displays poor tolerance of cold
has a tendency to gain excessive weight
Easily fatigued
slow reflexes such as slow speech and poor memory
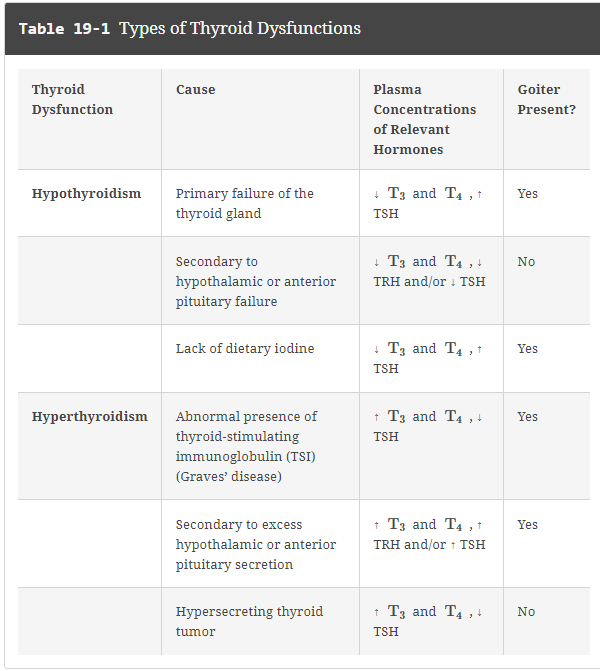
What can cause hyperthyroidism?
Grave disease
excess TRH or TSH
Thyroid tumor