myocardial Ischaemia
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
47 Terms
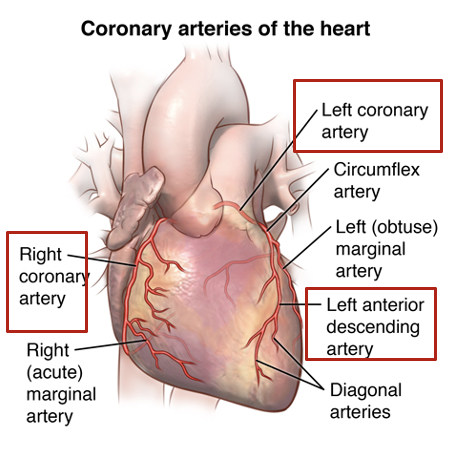
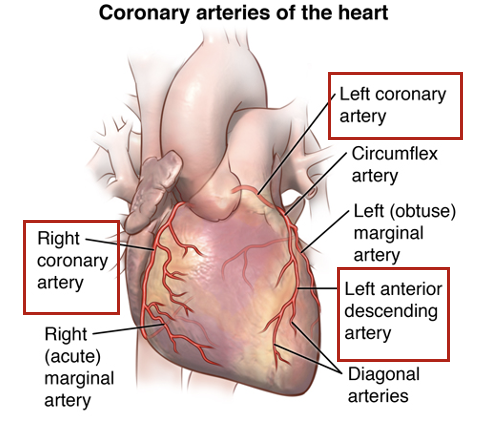
what is coronary artery disease
reduced blood flow of coronary arteries
most common cause is atherosclerosis → build up of fatty plaques in the coronary artery walls
what happens when fatty plaque deposists in the coronary arteries (atherosclerosis) → add on gizmo
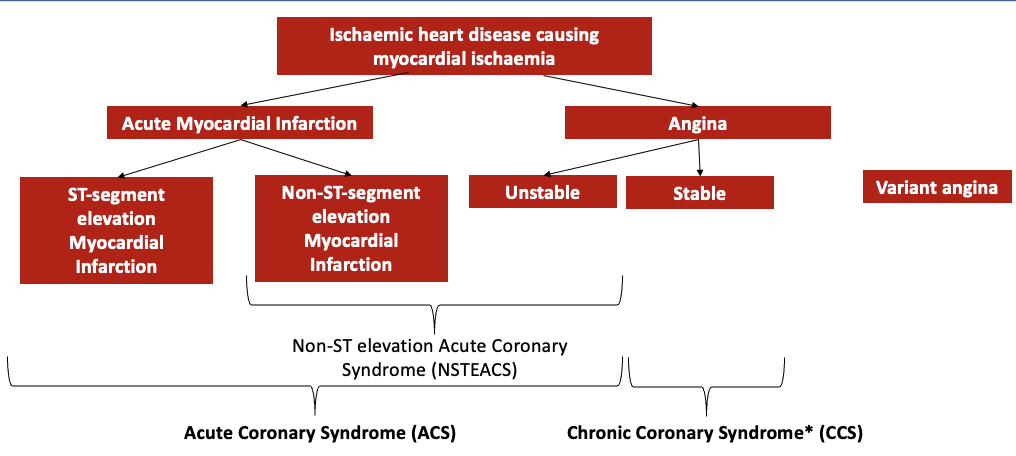
become narrowed → restricts blood supply to heart resulting in Non-ST elevation Acute Coronary Syndrome (NSTEACS)
NSTEACS are divided into
chronic coronary syndrome
acute coronary syndrome
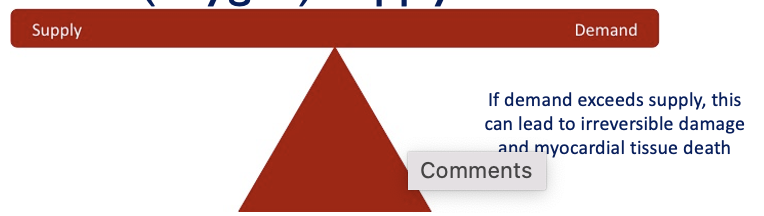
what is myocardial ischaemia
when myocardial cells don’t receive enough blood (oxygen)
there is an imbalance between myocardial blood (oxygen) supply and demand
if demand exceeds supply → irreversible damage and myocardial tissue death
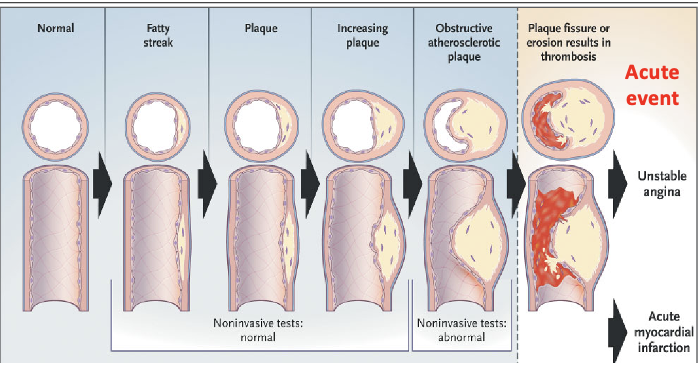
what is atherosclerosis
when fatty deposits build up in the arteries, which causes them to narrow
stages from normal to progressive coronary artery disease
Damage to artery wall (caused by smoking, diabetes, hypertension etc) → inflammation and build up of fatty plaques (atheroma) in walls of coronary arteries
If the plaque ruptures → platelet activation, aggregation and thrombus formation
thrombus can break loose and travel to other part of body (embolus)
coronary artery disease when atherosclerosis occurs leads to…
ischaemic heart disease (coronary artery disease, and is divided into
chronic coronary syndromes (CCS) → people are ‘stable’, symptoms are controlled/asymptomatic
acute coronary syndromes (ACS) → people are not stable, symptomatic due to sudden reduction in blood flow to heart
what are the disease consequences of ischaemic heart disease causing myocardial ischaemia
how to distinguish between clinical symptoms of myocardial ischaemia
ECG → ST elevation, ST depression, T wave inversion
troponin T/ troponin I → protein released from cardiac cells when damaged
what is stable angina slide 11
crushing sensation in the chest caused by they have narrow blood vessel and reduced blood flow to the heart (ischaemic pain)
chest pain, tightness, indigestion type pain
Associated with effort (exercise, cold, excitement) à demand exceeds supply
Relieved by rest or medications
Short lived
predictable and reproducible
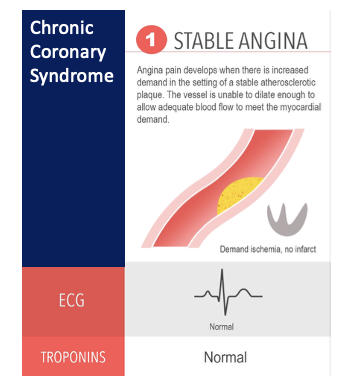
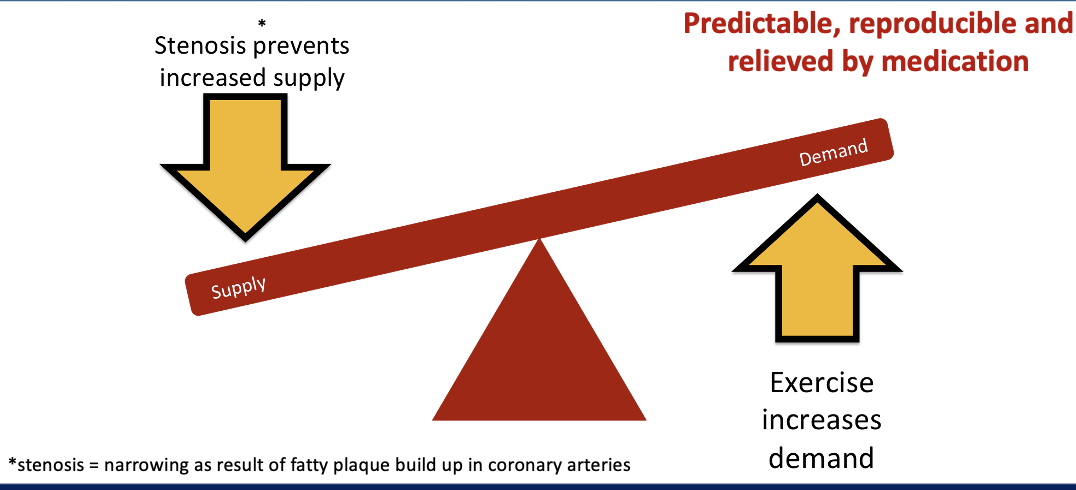
how is supply and demand affected in stable angina
only really a problem when in high demand for oxygen, but supply is really low
can occur during intense exercise and stress
stenosis → narrowing as a result of fatty plaque build up in coronary arteries
stenosis prevents increased supply
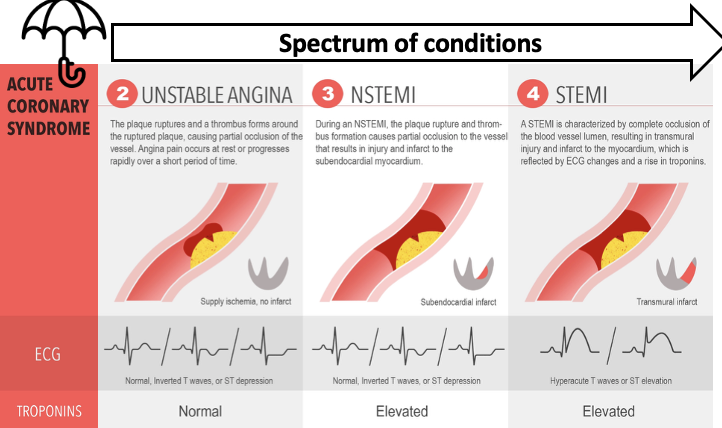
what is acute coronary syndrome and the different spectrum of conditions
describes a spectrum of clinical syndromes including
unstable angina → normal, inverted T waves (ST depression), troponins are normal
non-ST elevation myocardial infarction (NSTEMI) → normal, inverted T waves (ST depression), roponins are elevated
ST elevation myocardial infarction (STEMI) → hyperacute T waves (ST elevation), troponins are elevated
caused by thrombosis, leading to acute occlusion of a coronary artery , presenting as the spectrum of clinical syndromes
what are the symptoms of acute coronary syndrome
Severe pain – chest, jaw, neck, back
Breathlessness
Nausea and vomiting
Light-headedness
Sweating
can be unpredictable and acute in onset
For some people the first major sign is cardiac arrest
how does myocardial infarction develop
proceeds in ‘wavefront’ from subendocardium to subepicardium
Eventually transmural infarct is produced (24 hours), and cell death occurs by coagulation necrosis
Further changes take place over days and weeks
Neutrophils enter the infarct → scar tissue is developed (granulation)
Ventricular remodelling → ventricles change in size, shape, and function in response to damage or disease
what are the complications of myocardial infarction
heart failure
arrhythmias
ventricular ectopic beats
ventricular tachycardia
ventricular fibrillation
supraventricular tachycardia
heart block
intracardiac thrombus
cardiac rupture
pericarditis
how is ischaemic heart disease diagnosed and investigated
coronary angiography (invasive) → catheter passed up to heart and coronary arteries, dye is injected and X-rays are taken
imaging → via CT coronary angiogram, cardiac MRI, echocardiogram
electrocardiogram (ECG) → distinguishes between NSTEACS/STEMI
clinical history → symptom assessment
troponin blood test → detects sign of damage to heart cells
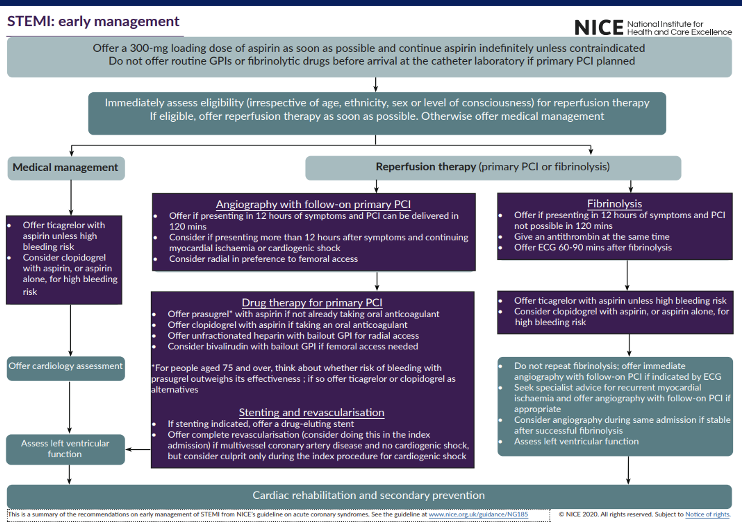
how is acute ST elevation myocardial infarction (STEMI) managed
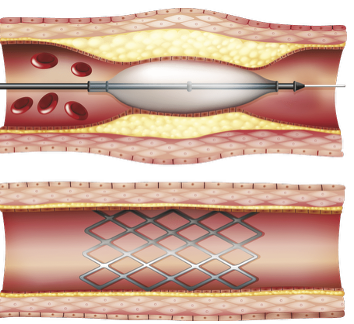
primary percutaneous coronary intervention (PPCI)
an emergency procedure that rapidly opens blocked coronary artery with a balloon and implants a stent to restore blood flow
usual first line approach if accessible within specified timeframe from onset symptoms
thrombolyis
using a "clot-busting" drug to dissolve blood clots, restoring blood flow
usual approach if PPCI can’t be achieved within specified timeframe from onset of symptoms
medical management
no intervention
decision of risk vs benefit
what is Percutaneous Coronary Intervention (PCI)
balloon inserted to widen vessel and stent deployed
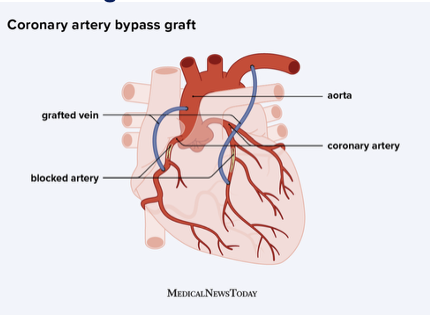
what is coronary artery bypass graft (CABG)
open heart surgery where vessel removed from another part of body and grafted to either side of the blockage to divert blood flow
what is thrombolysis
dissolution of a blood clot
Allows reperfusion of ischaemic region
Limits infarction size and reduces complications
Can be used within 12 hours after infarction
Complications include bleeding (haemorrhagic stroke)
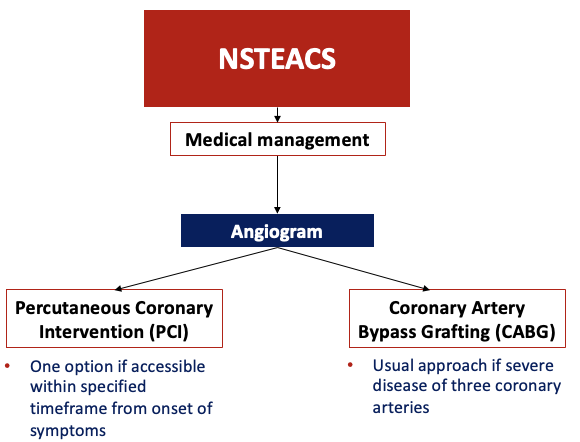
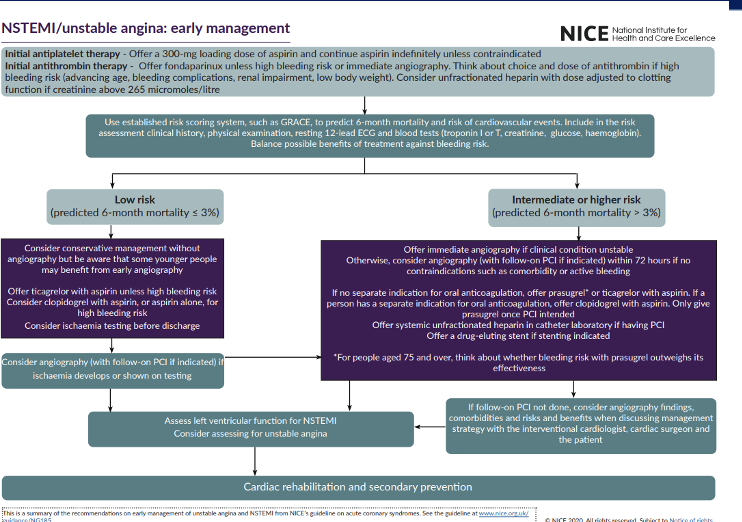
what is the management of Non-ST-Segment Elevation Acute Coronary Syndrome (NSTEACS)
medical management → angiogram test leads to two options
percutaneous coronary intervention → if accessible within specified time frame from onset of symptoms
coronary artery bypass grafting (CABG) → usual approach if severe disease of three coronary arteries
what are the types of acute coronary syndrome
Type 1: Caused by plaque rupture – most commonly seen
Type 2: Oxygen supply-demand imbalance without atherosclerosis
Type 3: Sudden death with MI Symptoms
Type 4: MI associated with stenting
Type 5: MI associated with bypass grafts
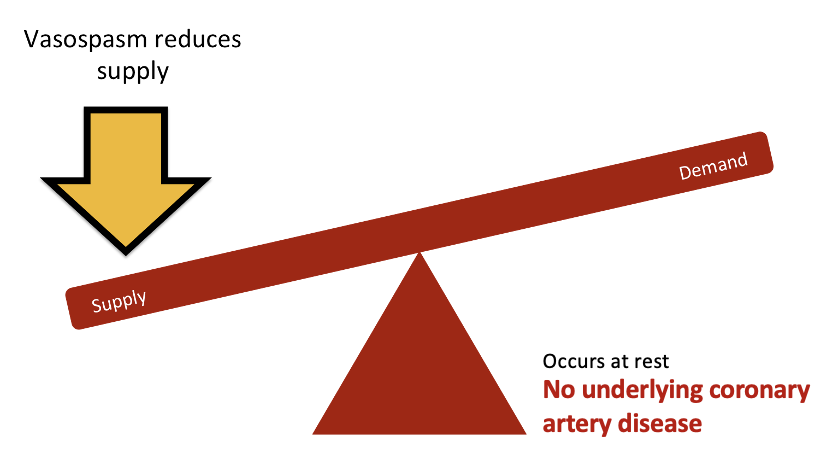
what is variant angina (prinzmetal/coronary artery spasm)
vasospasms reduces supply
occurs at rest
there is no underlying coronary artery disease
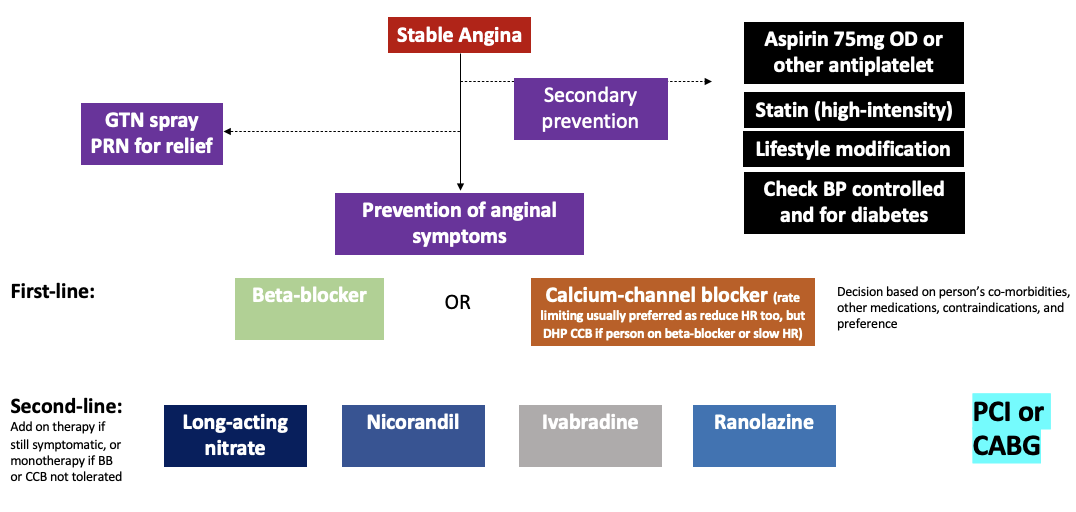
what is the treatment for stable angina
anti anginal medicines
reduce heart rate (in order to reduce demand and cardiac work)
beta blockers
ivabradine
rate limiting calcium chanel blockers
widen narrowed coronary arteries
Coronary artery dilation improves blood flow to heart
Vein dilation decreases preload, reducing cardiac work, lowers blood pressure
nitrates
calcium channel blockers
nicorandil
ranolazine
what are beta blockers
examples
bisoprolol
atenolol
mechanism
Beta-selective adrenoceptor blocking agent → blocks action of adrenaline and noradrenaline on heart → reduces heart rate and the hearts demand for oxygen
Dose adjusted to resting heart rate of 60 bpm (provided blood pressure ok) or maximum target dose
No preference on which betablocker (licenced)
Also lowers BP
can’t be used for patients with asthma
what are rate-limiting calcium channel blockers
examples
verapamil
diltiazem (rate-limiting)
mechanism
Calcium channel blockers with both cardiac and vascular effects
Reduce heart rate and therefore oxygen demand of the heart
Reduce force of heart contraction (negative inotropic effect)
Vasodilation
Will also lower BP
Avoid use with betablockers
what are dihydropyridine calcium channel blockers
examples
amlodipine
felodipine
mechanism
Calcium channel blockers with predominantly vascular effects (vasodilation)
don’t affect rate
can be used with beta blockers
Vasodilation
Coronary artery dilation improves blood flow to heart
vein dilation decreases preload, reducing cardiac work
what are nitrates
examples
glyceryl trinitrate (GTN)
isosorbide mononitrate (ISMN), isosorbide dinitrate
mechanism
vasodilation via the release of nitric oxide (NO)
Endogenous production of NO is impaired by coronary artery disease, nitrates provide an exogenous source of NO
Side effects – some related to vasodilation eg reduced blood pressure, lightheadedness, headaches
how does vasodilation via the release of nitric oxide occur (use of nitrates)
Organic nitrates are metabolised to release NO
NO activates soluble guanylate cyclase (sGC)
sGC forms cyclic guanosine monophosphate (cGMP) from guanosine triphosphate (GTP)
cGMP activates Protein Kinase G (PKG)
PKG dephosphorylates myosin light chains and promotes sequestration of intracellular Ca2+
Vascular smooth muscle is relaxed
what are the forms of nitrates for angina
GTN sublingual spray or tablets
for Acute angina attacks
Quick onset and short time of action
ISMN tablets –taken daily.
Intravenous
Chronic nitrate use produces tolerance → timing of doses is important
Reasons for nitrate tolerance are not entirely known but likely to involve a physiologic compensation of having high levels of nitric oxygen.
what is ivabradine
a pacemaker current inhibitor
mechanism
Blocks the pacemaker sodium and potassium currents (If or ‘funny current’) that go through the hyperpolarization-activated cyclic nucleotide-gated (HCN) channels in the heart that controls depolarization of the sinoatrial node reducing heart rate and therefore oxygen demand of the heart
Doesn’t lower BP
Sinus rhythm
May cause visual disturbance due to retinal If
what is nicorandil
a vasodilator drug
mechanism
Combined NO donor and activator of K+ channels
NO release leads elevation in cGMP and activation of K+ channels
Effect is hyperpolarisation (K+ leaves cells) with coronary artery vasodilation and improved blood flow
Side effect: ulceration → formation of a break in the skin or a mucous membrane, leading to a sore where tissue has broken down and disintegrate
what is ranolazine
for chronic angina
Mechanism not fully understood:
Reduces the work of the heart by reducing the late sodium current in the cardiac action potential
Effect is a reduction in calcium entry which reduces wall tension and improves blood flow via the coronary arteries.
Reduce ionic imbalances that can occur in ischaemia
Marketed as no change in HR or BP
Drug interactions eg carbamazepine, clarithromycin, phenytoin
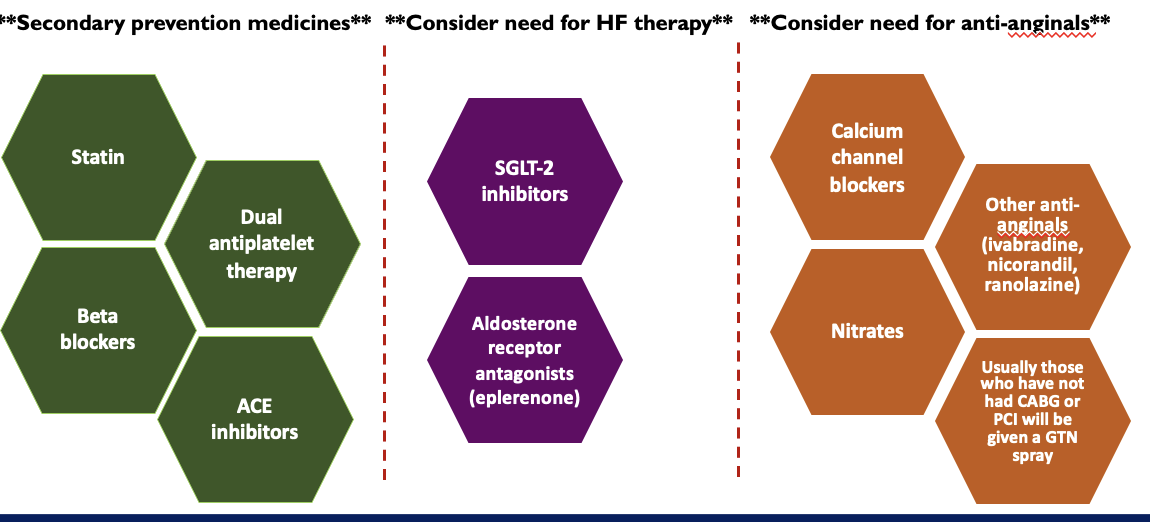
summary of treatment guidelines for anti anginals
what is the initial management for acute coronary syndromes (STEMI, NSTEMI, unstable angina)
Medications to prevent further platelet aggregation → aspirin/ clopidogrel/ ticagrelor (loading doses)
Medicines to treat the pain → morphine is a vasodilator and reduces preload, and to a lesser extent afterload)
If ongoing chest pain then can give nitrates (usually GTN sublingual)
If low oxygen saturations and breathless → can be given oxygen
If nauseous → give antiemetic
what is the treatment for ST-elevation myocardial infarction (STEMI)
Primary PCI or Thrombolysis → Antithrombin, glycoprotein IIb/IIIa antagonists
If not suitable then manage as for NSTEACS
what is the treatment for NSETEMI/Unstable angina (NSTEACS)
antithrombin therapy → fondaparinux SC 2.5mg daily
summary of early management of STEMI
summary of early management treatment of NSETEMI/Unstable angina
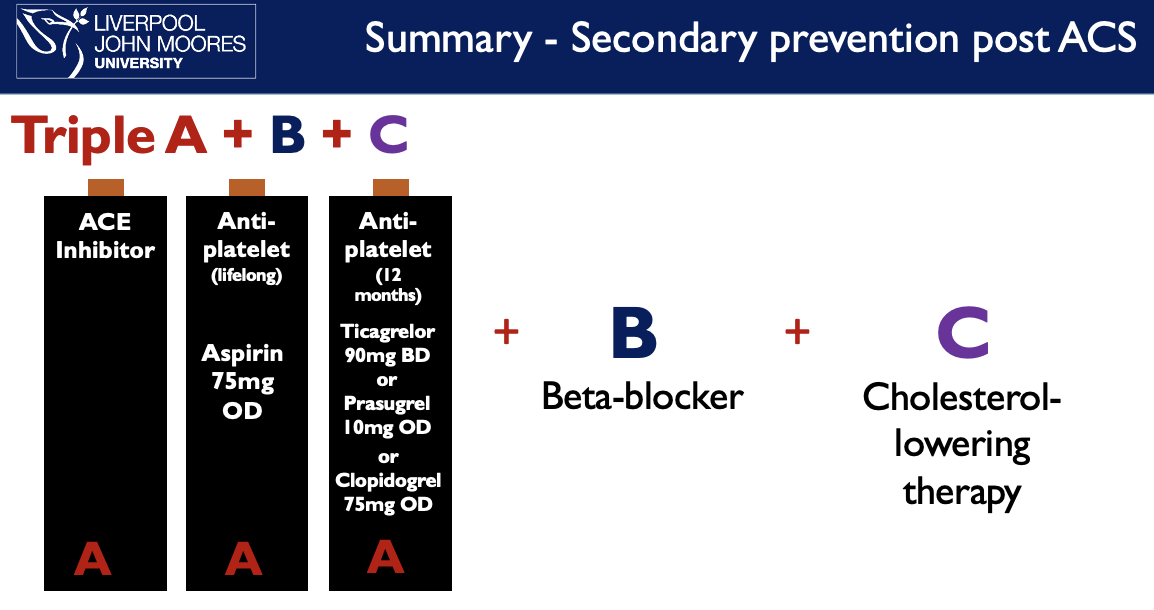
what is the secondary prevention after acute coronary syndrome
antiplatelets
ACE inhibitors
betablockers
statins
how are antiplatelets as secondary prevention after ACS
Reduce platelet aggregation in ACS
Dual antiplatelets for12 months following ACS or PCI then review (usually reduce to single antiplatelet)
Bleeding risks with dual antiplatelets
To reduce the risk → co-prescribe PPIs for those at high risk on antiplatelets
Interaction between clopidogrel and omeprazole/esomeprazole MHRA alert → shouldn’t be co-prescribed
how are ACE inhibitors used as secondary prevention after ACS
cardioprotective (preservation of the heart)
Reduce afterload , improve ejection fraction, may improve endothelial function, limit remodelling and infarct expansion
Reduce mortality
need to titrate doses
mechanism on different lecture
how are betablockers used as secondary prevention after ACS
Cardioprotective ((preservation of the heart))
Reduce heart rate, prevent overworking of heart
Reduce myocardial oxygen demand (prevent angina)
Reduce incidence of arrythmias
Some beneficial in reduced left ventricular dysfunction (see HF lectures)
Reduce mortality
need to titrate doses
how are statins used as secondary prevention after ACS
High intensity
e.g. Atorvastatin 80mg daily
Effects additional to cholesterol lowering
Can have effects on inflammation, thrombogenesis and the blood vessels
Reduce mortality and further events
Some side effects include rhabdomyolysis, liver effects , MHRA → rare myasthenia gravis
(mechanism of action in other lecture)
summary of medical management for secondary prevention
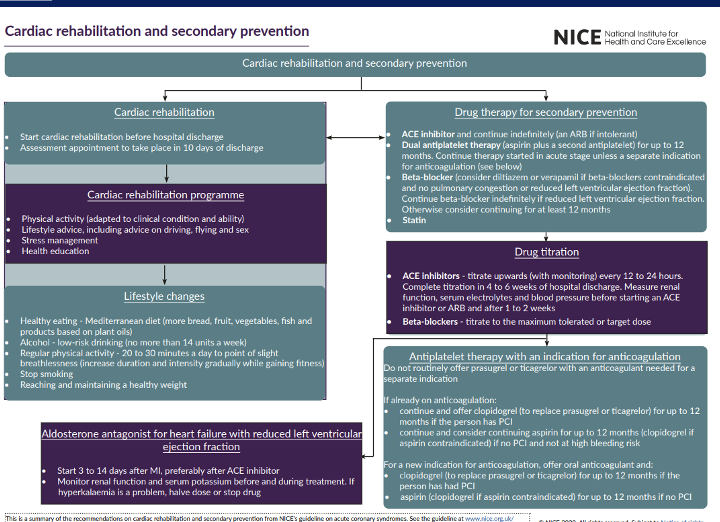
summary of cardiac rehabilitation and secondary prevention (NICE)
what is triple A + B + C for secodnary prevention