7 Autonomic Nervous System (ANS)
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
What are the divisions of the autonomic nervous system (ANS)?
Sympathetic Nervous System
Parasympathetic Nervous System
Enteric Nervous System
What are the key characteristics of the ANS?
Involuntary
2 neuron relay with preganglionic neuron and postganglionic neuron
Maintains internal environment (homeostasis)
cardiac myocytes
glands
smooth muscles
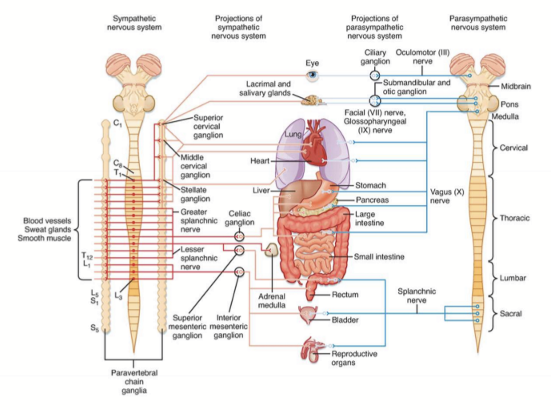
What parts of the ANS innervates organs and tissues?
Both SNS and PNS stimulate most organs/tissues, and stimulate opposite reactions/exhibit reciprocity
What is reciprocity?
When a tissue or organ is innervated by both SNS and PNS which stimulate opposite reactions
What does reciprocity create in the organ/tissue?
Constant tone, never “off”
For tissues that do not have dual innervation, how are they controled?
They are controlled based on increasing or decreasing stimulation
What are some organs that are only regulated by the SNS?
Adrenal medulla
Smooth muscle of blood vessels
Cardiac myocytes
(freeze and fawn are also controlled by SNS)
What does stimulation of SNS cause in the pupil?
Dilation/Mydriasis
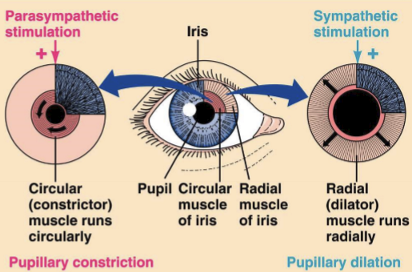
What does stimulation of PNS cause in the pupil?
Constriction/Miosis
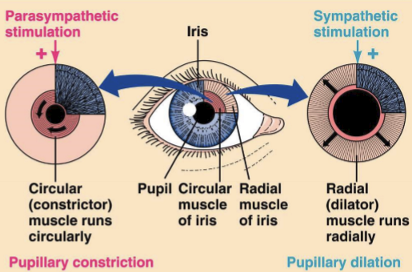
How do DFE (Dilated Fundus Examination) use the ANS to dilate the pupils?
Anticholinergic agents block PSN: Tropicamide, Atropine
Adrenergic Agonists stimulate SNS: Phenylephrine
Why is Tropicamide used over Phenylephrine?
Phenylephrine can cause in an increase in HR and BP and Tropicamide has less side effects
What system is only controlled by the SNS?
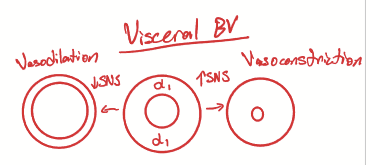
Smooth Vascular Muscles (SVM) as they only have adrenergic receptors, so no receptors for PNS
How does SNS regulate SVM?
With high SNS, the SMV vaso-constricts in viscera and vaso-dilates in skeletal muscles.
With low SNS, the SMV vaso-dilates in viscera and vaso-constricts in skeletal muscles
Overall, shifts blood to different organs and tissues
What adrenergic receptors do blood vessels on visceral organs have?
Alpha 1, causing vasoconstriction
What kind of adrenergic receptors do blood vessels for skeletal muscles have?
Beta 2 receptors, causing vasodilation
What nervous system controls the cardiac myocytes?
SNS ONLY, with an increase in SNS causing an increased in contraction strength
Where is the SNS located?
Thoracolumbar T1-L2
What are the components of the SNS?
Preganglionic neurons: short B fibers secreting ACh to bind to nAChR on postanglionic neuron
Postganglionic neuron: long C fibers secreting NorE
Target Tissues: Smooth muscles, glands, cardiac myocytes with alpha 1, 2 and beta 1, 2 receptors
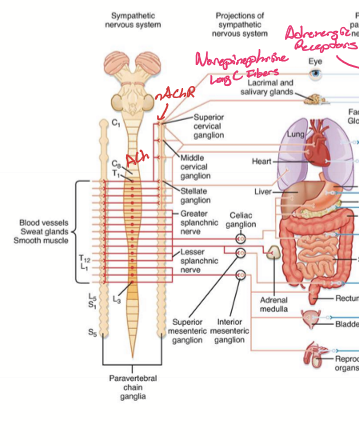
What is unique about sweat glands?
They can have short preganglionic neurons, long postganglionic neurons, and use M3 receptors on the sweat glands
Where are adrenergic sweat glands located?
Palms, soles, and forehead.
What is the postganglionic neuron equivalent in the adrenal medulla?
Chromaffin cells, secreting Epi into blood to bind to adrenergic receptors
What types of adrenergic receptors do epi prefer to bind to?
Beta 1 and 2, but will still bind to alpha 1 and 2.
Where is the PNS located?
CN: 3, 7, 9, 10, pregang cell bodies is CN Nuclei; Spinal Cord: S1-S3
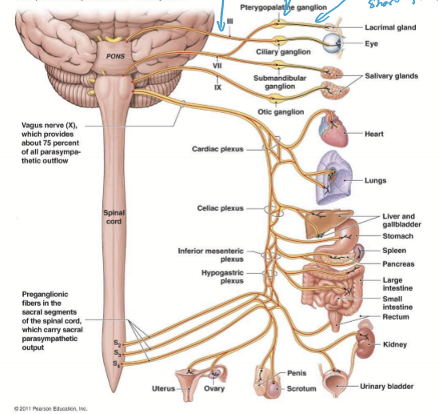
How is the PNS laid out?
Long preganglionic neurons: B fibers secreting ACh
Short postganglionic neuron: C fibers secreting ACh
Target tissues: smooth muscles, glands, cardiac muscles with Muscarinic receptors (M1-M6)
What are the shared characteristics between SNS and PNS?
2 neurons
Preganglionic neurons use B fibers and secrete ACh
ACh binds to nAChR on postganglionic neurons
Postgang neurons are C fibers
What is the differences between SNS and PNS?
Length of pre and post-gang fibers
Postgang for SNS secrete NorE, while PNS secrete ACh
SNS targets adrenergic receptors, PNS targets muscarinic receptors
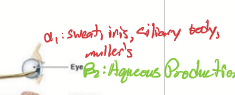
What are the functions of SNS stimulation to the eye?
Radial muscle for mydriasis/dilation
Muller’s mucles: lid
Sweat glands: adrenergic sweating
Stimulate development of iris color in infants
What is the pathway the SNS takes to get to the eye?
Central neuron from hypothalamus
Cell body in posterior hypothalamus
Descends ipsilateral through brainstem
Terminates at T1-T3 intermediolateral horn of Spinal cord
Synapses on pregang neuron
Preganglionic neuron
Exits through ventral root and enters sympathetic chain ganglia around apex of lung, common carotid, and breast lymph nodes
Postganglionic neuron
Cell body in superior cervical ganglion near bifurcation of common carotid
Axons travels on internal carotid artery near middle ear
Synapses and controls adrenergic receptors
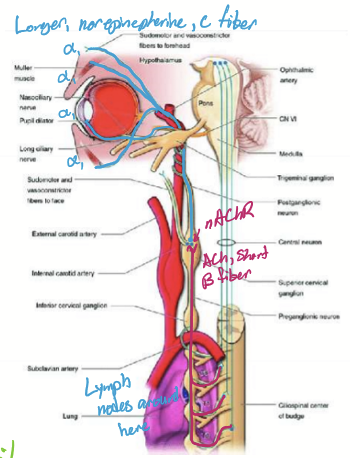
What is the sympathetic chain ganglion?
A structure that runs the length of the spine, part of the sympathetic nervous systemWhat does the superior cervical ganglion innervate?
What does the superior cervical ganglion innervate?
The head.
What does a change in SNS innervation do to visceral BV’s?
An increase in SNS causes vasoconstriction and a decrease causes vasodilation
Where are α1 adrenergic receptors located?
Radial muscle for mydriasis
Sweat (not axial)
Muller’s muscle
Vasoconstrictor
Where are α2 adrenergic receptors located?
Glands
inhibitory effect on α1

Where are β1 adrenergic receptors located?
Heart
Renal

Where can β2 receptors be found?
Aqueous humor production
Bronchodilatorz
What What does it mean if a therapeutic is direct or indirect?
A direct therapeutic means it directly affects a receptor. Indirect means that it has an effect on the production or degradation or release of a NT.
What are some sympathomimetics?
Epinephrine
Phenylephrine (alpha 1 specific) = 2.5%
Levodopa/ L-Dopa: A dopamine precursor
Cocaine: Blocks reuptake
MAOi and COMTi: Inhibit degradation
Hydroxyamphetamine: stimulates synaptic vesicle fusion
What are some sympatholytics therapeutics?
Non-specific blockers
Specific blockers
What can cause high SNS?
Stress
Temporary is normal
Chronic stress/trauma:
High levels of circulating cortisol: increases infection and leaky gut syndrome
Pheochromocytoma: tumor of adrenal medulla
High conc of circulating epi causes hypertensive retinopathy
What causes Low SNS?
Horner’s syndrome
What is horner’s syndrome caused by?
Disruption/lesion of sympathetic pathway to eye
What are the presentations of Horner’s syndrome?
Miosis
Ptosis
Anhidrosis
Heterochromia irides

What are some etiologies for Horner’s syndrome?
Damage to central neuron from stroke, trauma, demyelinating disease
Damage to pregang neuron from lung cancer (pancoast’s tumor) and metastatic breast cancer
Damage to postgang neuron from carotid aneurysm or dissection and carotid surgery (carotid endarterectomy)
Why are lesions to postgang neurons so significant?
Lesion in the postgang neurons can be due to Carotid aneurysms, carotid dissection, and carotid surgery.
What are the steps of SNS innervation of the radial muscle
SNS releases NorE → binds to alpha 1 receptors on radial muscle → mydriasis → NorE removed by reuptake
What happens to alpha 1 if there is damage to the SNS tract?
It is upregulated, causing a hypersensitivity from the denervation
What are the tests are ran for Horner’s Syndrome?
4% Cocaine: blocks reuptake; Normal = mydriasis; Horner’s = No Mydriasis
Apraclonidine (better test); Normal = slight miosis; Horner’s = Mydriasis
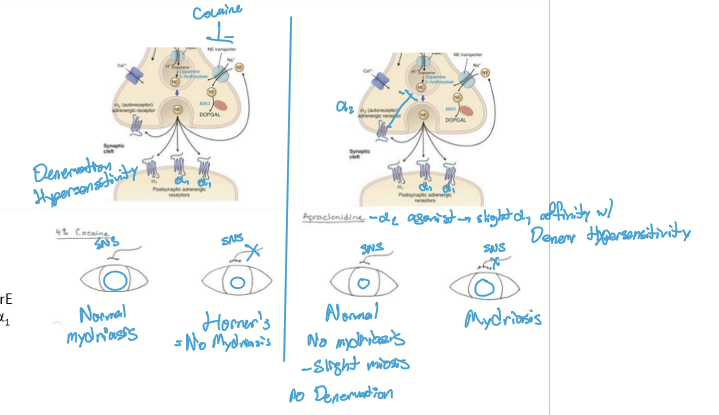
How does Apraclonidine work?
It stimulates both alpha 1 and 2 receptors. In a normal patient, apraclonidine will stimulate alpha 2 more, reducing the amount of stimulation alpha 1 receptors receive, causing a sight miosis in the eye. Due to the upregulation of alpha 1 receptors, the dilator muscle is hypersensitive and is stimulated by apraclonidine, causing a mydriasis overall.
What tests are used to determine if the lesion in horner’s is post vs preganglionic?
1% Hydroxamphetamine: Stimulates release of NT; post = no mydriasis since dead cells cannot release NT; Preganglionic lesion = mydriasis as cell is alive and still able to release NT
1% Phenylphrine: Tests for reuptake by stimulating alpha 1 receptors; post = mydriasis as no uptake can occur d/t dead cell; pregang lesion = no mydriasis as phenylephrine is removed by the postgang neuron
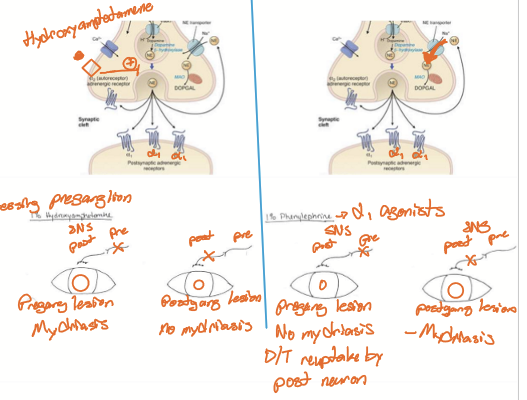
Which of the tests for Horner’s is considered fail-safe?
1% hydroxyamphetamine; bc if test fails, not concerned about compression of the pregang nerve from cancer
What is the pathway for Parasympathetic Innervation of the eye?
light stimulates RGC’s in eye
RGC’s synapes in the pretectal olivary nuclei and stimulate Edinger-Westphal nucleus bilaterally
Preganglionic Cholinergic neuron (long B fiber) in Edinger-Westphal nucleus projects on CN III
Synapes on Postganglionic neuron (B fiber) in Ciliary ganglion stimulating nAChR on postgang neuron
Short post (C fiber) neuron synapses on sphincter muscle
Releases ACh on M3 receptors causing BILATERAL MIOSIS
What type of muscarinic receptors does the eye and heart have? What makes them unique?
Eye has M3, causing miosis and lacrimation
Heart has M2, causing HR to slow down
What are cholinergic therapeutics?
Also called parasympathomimetic or M agonists; Pilocarpine is an example. It increases tear production